Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.15 n.4 Pretoria Dec. 2023
http://dx.doi.org/10.7196/AJHPE.2023.v15i4.326
RESEARCH
Education about planetary health and sustainable healthcare: A national audit of health professions education curricula in South Africa
J H IrlamI; A DreyerII; G FiliesIII; L GovenderIV; N JacobV; J JayakumarVI; C L LokotolaVII; R NaidooVIII; S ReidIX; H-A RotherX
IMSc (Climate Change and Development), MPhil (Epidemiology) ; Primary Health Care Directorate, Department of Family, Community and Emergency Care, Faculty of Health Sciences, University of Cape Town, South Africa
IIBA, Adv Dip Adult Ed, MPH (Health Promotion); Division of Rural Health, Department of Family Medicine and Primary Care, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIBSc (OT), MPhil Health ScEd, PhD; Interprofessional Education Unit, Faculty of Community and Health Sciences, University of the Western Cape, Cape Town, South Africa
IVMB ChB, PG Dip (HPE), MPhil (HPE); Division of Anatomical Pathology, Faculty of Health Sciences, University of Cape Town, South Africa
VMB ChB, FCPHM (SA), MMed (Public Health Medicine); School of Public Health, Faculty of Health Sciences, University of Cape Town, South Africa
VIPhD (Clinical Sciences and Immunology), PG Dip (Educational Technology); Department of Pathology, Faculty of Health Sciences, University of Cape Town, South Africa
VIIMPH, PhD (Public Health); Division of Family Medicine and Primary Care, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VIIIMB ChB, DOH, MPH (Occupational Medicine), PhD (Industrial Health); Discipline of Occupational and Environmental Health, College of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IXMB ChB, PhD; Primary Health Care Directorate, Department of Family, Community and Emergency Care, Faculty of Health Sciences, University of Cape Town, South Africa
XPhD (Environmental Sociology) Division of Environmental Health, School of Public Health, Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
BACKGROUND. Climate change and environmental degradation have severe public health impacts. Education about planetary health (PH) and sustainable healthcare (SH), or the interdependence of health and healthcare and planetary ecosystems, is developing globally to enable health professionals to protect public health from these threats, and to build sustainable healthcare systems.
OBJECTIVE. To assess the status of PH and SH in health professions education in South African (SA) faculties of health sciences as a foundation for future work.
METHODS. Educators at all 24 SA faculties of health sciences were surveyed regarding undergraduate and postgraduate faculty courses with PH- and SH-related learning objectives and outcomes, learning activities and assessments. Pivot tables were constructed to analyse their responses.
RESULTS. Forty-one responses were received, representing 9 health professions from 15 of 24 faculties of health sciences in SA (62.5%). More than half (53.7%) were unaware of any courses with PH and SH content at their faculties. Nineteen respondents from 11 faculties reported 44 courses and provided data on 18 non-duplicate courses. Learning activities included advising patients about environmental and health co-benefits of their lifestyle choices (33.3%); written assignments (38.9%); oral presentations (55.6%); and community-based research (38.9%). Nine courses (50%) reported PH- and SH-related assessments, most commonly oral presentations (88.9%); reflective essays (77.8%); multiple-choice or short assessment questions (55.6%); and research outputs (55.6%).
CONCLUSION. Education about PH and SH is starting to develop in SA faculties, although with a limited variety of learning activities and assessments. This study provides a useful baseline for curriculum development and assessment of progress.
Climate change has been widely recognised as a major and growing threat to global health in the 21st century, which is amplifying environmental risks to health.[1,2] Educating current and future health professionals to protect health from climate change, to promote behaviour to mitigate and adapt to a changing climate, and to work for the environmental sustainability of health services, is therefore increasingly important.[3] Advocacy on climate change is recognised as a duty of health professionals, especially given their proximity to those most vulnerable to climate-health impacts, their expertise and experience in treating such impacts, their influence in promoting more sustainable healthcare (SH), and the high levels of public trust placed in them.[4]
SH aims to provide high-quality healthcare, without compromising the ability of the healthcare system to meet future health needs. Promoting health and the timeous delivery of quality healthcare benefits patients and the ecosystems on which their health depends.[5] Education for sustainable healthcare (ESH) has been defined as the organisation of health professions education to develop knowledge, skills and attitudes about the interdependence of health and healthcare and planetary ecosystems.[6,7] This includes the effects of rapid climate and environmental changes on health, and conversely, the impacts of healthcare systems on the environment. There is growing international practice and research about integrating sustainability into various educational contexts and health professions education curricula that need to be adapted appropriately for local settings.[8-12] The Consensus Statement on Planetary Health and Education for Sustainable Healthcare,[13] developed by the Association for Medical Education in Europe (AMEE), is an important milestone in the field. It describes the knowledge, skills and values required to practise SH, and has proposed learning objectives, activities and assessments to promote multidisciplinary learning. ESH mainstreams, as a cross-cutting curricular theme, the concept of planetary health (PH), which encompasses the health and wellbeing of human civilisation and the state of the natural systems on which it depends.[14]
With the wide-ranging social and health impacts of global climate change and environmental degradation, the concept of environmental accountability has emerged as an aspect of the social accountability of health educational institutions. It recognises that institutional policies and practices that reduce environmental impact, and educating graduates to promote PH and SH, are ways in which educational institutions can address public health needs in a rapidly changing environment.[15-17] The World Health Organization (WHO) COP26 Special Report on Climate Change and Health[18] has urged that health workers be trained to help build low-carbon and climate-resilient healthcare systems. The WHO-Civil Society Working Group to Advance Action on Health and Climate Change has called on health education stakeholders to incorporate climate change into curricula for preparing health professionals 'to recognise and address the health risks and impacts of climate change and to ensure functioning healthcare systems in a climate-changed future'.[19] An ESH curriculum for the UK[20] was published by the UK Medical Schools Council in 2022 in support of the Outcomes for Graduates framework of the General Medical Council (GMC),[21] which requires application of the principles of population health and SH.
Common barriers to integrating ESH include perceptions that existing curricula are overloaded; poor integration, alignment and assessment of current content on environmental sustainability; and faculty leaders, educators and students who doubt the relevance and worth of ESH, or fail to see what health professionals can do, especially in the face of more apparently urgent 'downstream' health challenges.[5,6] Common enablers of integration include strong institutional leadership; increasing public awareness of climate and environmental crises, creating greater interest among educators and students; sharing of case studies and learning resources; and opportunities for change that arise from periodic curriculum reviews.[5,6] Partnerships between educators and students, supported by international collaboration, have been critical for the successful integration of PH and SH into health professions curricula in other settings.[22,23]
Southern Africa is highly vulnerable to environmental and climate risks to health, such as malnutrition and trauma arising from destructive extreme weather events.[24-26] South Africa (SA) has therefore adopted climate change policies and plans to build capacity in climate change awareness and adaptation.[27,28] Progress on including environmental accountability in health professions education in SA has been slow, despite calls to do so.[29] It should therefore be a priority for enabling future health professionals to identify and appropriately treat climate-sensitive conditions, to promote healthy behaviour and to advocate for sustainable healthcare systems.
However, the status of PH and SH in health professions education in SA faculties of health sciences is uncertain. The Education for Sustainable Healthcare Special Interest Group (ESH SIG) of the Southern African Association of Health Educationalists (SAAHE) was established in July 2021 to promote education regarding PH and SH in SA and southern Africa. This article describes a national audit in late 2021 of PH and SH in health professions education in faculties of health sciences in SA to provide a foundation for future work of the ESH SIG and others.
Methods
Design
The audit is a cross-sectional survey and the first of three phases of a mixed methods study design for the development of SA health professionals as advocates for PH and SH.
Study population and sampling
The study population comprised educators at all 24 SA faculties of health sciences. They were surveyed using a form based on the AMEE Consensus, which achieved broad consensus on a set of proposed learning objectives, activities and assessments.'131 The audit was endorsed by the national board of SAAHE and piloted on members of the ESH SIG executive, which helped to improve the clarity of the survey form. The invitation to participate in the audit was then shared widely with educators at all SA faculties of health sciences via SAAHE and several other networks (Box 1). The 2021 COP26 Special Report on Climate Change and Health'181 was referenced in communications to highlight the topicality of the study and to encourage timeous responses.
Data collection and analysis
The survey questions pertained to all undergraduate and postgraduate faculty courses that contained content regarding PH and SH, which were defined as the interdependence of health and healthcare and planetary ecosystems[13] (Supplementary File: https://www.samedical.org/file/2089). Respondents were asked to report on PH- and SH-related course learning objectives and outcomes, learning activities and formative or summative assessments, using checklists derived from the AMEE Consensus,'131 with provision for any further responses. They were requested to separately email course learning outcomes (defined as the specific questions that the convener wants the course to raise) and course learning objectives (i.e. specific, measurable knowledge and skills that the student should gain) for thematic analysis. Survey data were captured via Google Forms and responses were viewed in Google Sheets Excel pivot tables, constructed by JI, to analyse the frequency of key variables in the responses.
Ethical approval
Ethical approval was obtained in August 2021 from the Research Ethics Committee, Faculty of Health Sciences, University of Cape Town (UCT) (ref. no. HREC 358/2021).
Results
Forty-one responses were received from educators, representing 9 of the 17 professions (Box 2) registered with the Health Professions Council of SA (HPCSA) and the SA Nursing Council (SANC). All were included in the analysis. The most common professions that responded were medical practitioners (n=13; 31.7% of sample) and environmental health practitioners (EHP) (n=5; 12.2%). Fifteen of the 24 faculties of health sciences in SA were represented in the sample (62.5%), 8 faculties more than once, but by different departments and courses. The faculties of UCT and the University of Pretoria had the most representatives, with 8 and 7 respondents, respectively. The respondents were nearly evenly split between the ranks of professor, associate professor, senior lecturer and lecturer. They most often described their occupations as undergraduate or postgraduate educators in environmental health or SH, and less often as researchers, health promoters or as engaging directly with communities (Supplementary Table 1: https://www.samedical.org/file/2089).
Their reporting of faculty courses with PH and SH content ranged from no courses (n=22; 53.7% of respondents) to >4 courses (n=4; 9.8%). Overall, 44 courses were reported by 19 respondents from 11 faculties. Data were provided for 21 of the courses, but as 3 of these courses were duplicate reports by 2 respondents at the same faculties, their responses were combined to provide data on 18 unique courses at 11 faculties.
Eight of these were undergraduate courses, 7 were postgraduate courses, and 3 were offered to both undergraduates and postgraduates in different disciplines. Three of the 8 undergraduate courses (29.4%) were offered exclusively within MB ChB programmes, 2 exclusively to EHPs (25%), 1 to physiotherapists only, and the remaining 2 (25%) to several disciplines. Of the 7 postgraduate courses reported, 5 were Master in Public Health (MPH) programmes, 1 an MMed (Community Health) programme and 1 a Postgraduate Diploma in Occupational Health. The existence of PH- and SH-related course learning outcomes was reported for 15 courses (83.3%) and learning objectives for 17 (94.4%) of the 18 courses (Supplementary Table 2: https://www.samedical.org/file/2089).
The response to the request for emailed detail on the learning outcomes and objectives elicited only a few responses; therefore, no meaningful qualitative analysis was possible.
Learning activities
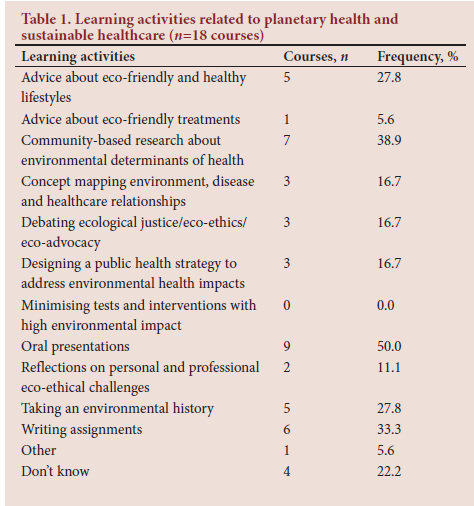
Over all 18 courses, the average reported frequency of the 11 learning activities proposed by the AMEE Consensus was 4 (22.2%) per course, ranging from 0 to 9 activities. The most frequent learning activities related to PH and SH were oral presentations on such topics (n=9; 50.0%); community-based research about key environmental determinants of health (n=7; 38.9%); written assignments (n=7; 38.9%); and advice to real or role-played patients about the environmental and health co-benefits of their lifestyle choices (n=5 courses; 27.8%). The following learning activities were each employed by 3 of the 18 courses (16.7%): designing a public health strategy to address environmental health impacts; concept mapping the relationships between the environment, disease and healthcare; and debating issues of ecological justice, eco-ethics and eco-advocacy by health professionals (Table 1). The 10 courses that included a postgraduate offering had twice the average number of forms of learning activities than the 8 undergraduate courses (Supplementary Table 2: https://www.samedical.org/file/2089).
Assessments
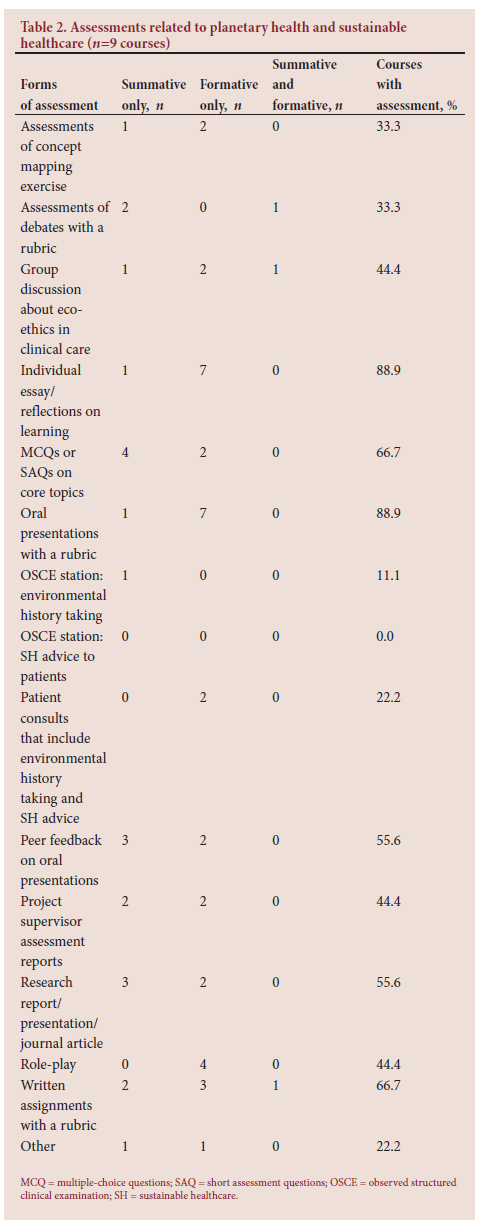
Nine of the 18 courses (50.0%) reported formative and/or summative assessments of PH and SH content (Supplementary Table 3: https://www.samedical.org/file/2089). The most common types of assessments were essays or individual reflections on learning (n=8; 88.9%); oral presentations with a rubric (n=8; 88.9%); written assignments (n=6; 66.7%); and multiple-choice or short assessment questions (MCQs/SAQs) (n=6; 66.7%). Environmental history taking and advice about sustainable and healthy lifestyles at observed structured clinical examination (OSCE) stations (n=1; 11.1%), and advice regarding sustainable and healthy lifestyles at OSCEs, were reported least often. Overall, more formative (n=36) than summative types of assessment (n=22) were reported (Table 2).
Discussion
The responses received related to 18 undergraduate and postgraduate courses. Overall, the quantity and variety of course learning activities and assessments regarding PH and SH were limited compared with those proposed by the AMEE Consensus,[13] especially at the undergraduate level. More traditional forms of learning and assessment predominated, such as oral presentations, writing assignments and MCQs/SAQs. More innovative forms suggested by the AMEE Consensus that were seldom reported include reflecting on and debating sustainability and eco-ethical challenges; investigating viable eco-friendly alternatives to tests and treatments with high environmental impacts; and environmental history taking and advice about sustainable and healthy lifestyles in OSCEs and during real or role-played patient consultations. These appear to be significant missed opportunities to test the application of knowledge in the psychomotor and affective domains, given how important these skills and values are for health professionals in promoting sustainability in clinical care and patient self-care. More authentic approaches that allow for multiple assessments of progress and for individual creativity are needed to foster such skills and values.[13]
Communicating sustainability values so that patients, their families and clinical colleagues understand how care for the environment is essential for health and wellbeing, is recognised in the UK curriculum for ESH as an important competency of professionalism and leadership for change.[20] Students should therefore learn how to take an environmental history from their patients and have conversations about their climate-health risks, as well as co-beneficial opportunities for personal and public health by means of eco-friendly lifestyle choices about energy, transport, food and waste disposal. Such conversations could also promote available sustainable alternatives to excessive medicalisation, investigation and treatment, while respecting the priorities and socioeconomic circumstances of the patient. Hence, general practitioners may have particularly good opportunities to empower patients and promote low-carbon alternatives, which are key principles of sustainable clinical practice.'30,311 However, such 'social prescribing' of non-medical options can also be readily practised by other disciplines, and may be especially effective in well-functioning health teams with a deep understanding of the determinants of health in their communities. The multidisciplinary student profile of many of the courses also provides a good opportunity for learning approaches to health and healthcare from a variety of health professionals.
Common examples of social prescribing include exercise and mindfulness classes; recreational and food gardening; active commuting on foot or by bicycle; and minimising, recycling and composting waste.[20] Involving students in such activities for communities that they serve can be a powerful learning experience. Students' learning should include the population-based community-orientated primary care (COPC) approach that can help to identify interventions to reduce climate vulnerabilities, to empower communities' responses to climate emergencies and to address specific environmental determinants of health. It should also include learning about the prevailing public health challenges and potential interventions to develop greater resilience to environmental and climate risks to health and healthcare, such as flooding, high temperatures, poor waste management, displacement, migration and the changing epidemiology of diseases.[32] Interventions to mitigate the considerable climate and environmental impacts of health facilities, and their leadership implications for health professionals and facility managers, should also be examined, using guidelines and local case studies from projects such as the Global Green and Healthy Hospitals (GGHH) initiative.[33]
Sustainability issues can be readily linked to existing topics in many specialties and build on students' prior knowledge of climate and environmental change. Discussions of current extreme weather events reported in the media, such as floods, droughts, heatwaves and wildfires that heavily impact health and healthcare services, could include the vital role of health professionals in climate mitigation, healthcare adaptation, and disaster preparedness and response. Integrating such discussions with lectures, self-directed learning and hands-on learning about clinical skills and case management, both longitudinally throughout the years of study and collaboratively across the disciplines, could deepen learning in a well-constructed curriculum. A systems thinking approach is therefore important for broadening the focus from managing the patient within a healthcare setting, to addressing the social and environmental determinants of health and disease.[20]
Similar barriers and enablers for integrating PH and SH as reported in the literature are likely in SA health professions education curricula; therefore, a strong case needs to be made. Determining the perceptions of national educators about the importance of PH and SH in the unique SA context, and what they think key learning objectives, activities and assessments should be, will help to build this case. A companion article'341 describes the subsequent Delphi panel phase of the mixed methods study to assess the relevance and applicability to SA of the learning objectives, activities and assessments proposed by the AMEE Consensus.
Study limitations
Despite extensive efforts to disseminate the survey across multiple networks of educators, the 41 responses received from 15 faculties are a limited representation of health professions and academic ranks at faculties of health sciences in SA. Regular follow-up and reminders by the principal investigator helped to boost the survey response rate at a time when academic year-end pressures and COVID-19-related academic disruptions were a major barrier. Data collection of longer duration - earlier in the year -may have yielded a larger and more representative response rate. The limited response may also reflect a disinclination to respond due to low awareness and understanding of the concepts of PH and SH, and perceptions of minimal relevance, as there are few courses with such content. The requested details on course learning outcomes and objectives are missing owing to a very low follow-up response rate, as explained above. Finally, further detail about learning activities and assessments was not requested to limit the burden of data collection on respondents and hence to achieve a higher overall response rate.
Conclusion
As far as we are aware, this is the first systematic attempt to survey education regarding PH and SH in health professions education in SA. We found that such education is starting to develop in SA health sciences faculties, albeit with a limited variety of learning activities and assessments of PH and SH content. Further research using deeper qualitative approaches would be helpful to address the study limitations.
Respondents recognised the growing importance and relevance of PH and SH to health professions education and practice, particularly in a country such as SA that is highly vulnerable to the health and social impacts of climate change and environmental degradation. Further work is therefore required in curriculum development in SA faculties of health sciences, enabled by strong institutional leadership, faculty staff and student involvement, sharing of ESH resources and continual monitoring and evaluation of progress. As such work is central to the mission of the ESH SIG of SAAHE, this audit provides a helpful baseline for the group's future activities, as well as informing the subsequent phases of the mixed methods study (a national Delphi panel; and a case study of the Faculty of Health Sciences, UCT).
Declaration. None.
Acknowledgements. Executive members of the Education for Sustainable Healthcare (ESH) Special Interest Group, Southern African Association of Health Educationalists (SAAHE); Ms Abigail Dreyer, Division of Rural Health, Department of Family Medicine, University of the Witwatersrand; Dr Tladi Ledibane, Department of Community Medicine, Sefako Makgatho University; Dr Gérard Filies, Interprofessional Education Unit (IPEU), University of the Western Cape; Prof. Poovendhree Reddy, Department of Community Health Studies, Durban University of Technology.
Author contributions. All authors complied with the International Committee of Medical Journal Editors' rules of authorship. JI conceptualised the study, designed the survey, collected and analysed the data, and prepared all drafts of the article. H-AR and SR commented on the study protocol and the audit tool. The other coauthors contributed data, assisted with sharing the audit in their institutions, and provided comment on two drafts of the article.
Funding. None.
Conflicts of interest. None.
References
1. Costello A, Abbas M, Allen A, et al. Managing the health effects of climate change. Lancet 2009;373(9676):1693-1733. https://doi.org/10.1016/S0140-6736(09)60935-1 [ Links ]
2. Watts N, Amann M, Ayeb-Karlsson S, et al. Countdown on health and climate change: From 25 years of inaction to a global transformation for public health. Lancet 2018;391(10120):581-630. https://doi.org/10.1016/S0140-6736(17)32464-9 [ Links ]
3. Walpole SC, Mortimer F, Inman A, et al Exploring emerging learning needs: A UK-wide consultation on environmental sustainability learning objectives for medical education. Int J Med Educ 2015;6:191-200. https://doiorg/10.5116/ijme.5643.62cd [ Links ]
4. Macpherson CC, Wynia M. Should health professionals speak up to reduce the health risks of climate change; AMA J Ethics 2017;19(12):1202-1210. https://doi.org/10.1001/journalofethics.2017.19.12.msoc1-1712 [ Links ]
5. Tun S. Fulfilling a new obligation: Teaching and learning of sustainable healthcare in the medical education curriculum. Med Teach 2019;41(10):1168-1177. https://doi.org/10.1080/0142159X.2019.1623870 [ Links ]
6. Walpole S, Vyas A, Maxwell J, et al. Building an environmentally accountable medical curriculum through international collaboration. Med Teach 2017;39(10):1040-1050. https://doi.org/10.1080/0142159X.2017.1342031 [ Links ]
7. Centre for Sustainable Healthcare. Education for sustainable healthcare network. 2020. https://networks.sustainablehealthcare.org.uk/network/education-sustainable-healthcare (accessed 14 October 2022). [ Links ]
8. Madden DL, McLean M, Brennan M, et al. Why use indicators to measure and monitor the inclusion of climate change and environmental sustainability in health professions education; Med Teach 2020;42(10):1119-1122. https://doi.org/10.1080/0142159x.2020.1795106 [ Links ]
9. Shea B, Knowlton K, Shaman J. Assessment of climate-health curricula at international health professions schools. JAMA Netw Open 2020;3(5):e206609. https://doi.org/10.1001/jamanetworkopen.2020.6609 [ Links ]
10. Walpole SC, Pearson D, Coad J, et al. What do tomorrow's doctors need to learn about ecosystems? BEME Guide No. 36. Med Teach 2015;10:1-15. https://doi.org/10.3109/0142159X.2015.1112897 [ Links ]
11. Walpole SC, Barna S, Richardson J, et al. Sustainable healthcare education: Integrating planetary health into clinical education. Lancet Planetary Health 2019;3(1):e6-e7. https://doi.org/10.1016/S2542-5196(18)30246-8 [ Links ]
12. Barna S, Maric F, Simons J, et al. Education for the Anthropocene: Planetary health, sustainable health care, and the health workforce. Med Teach 2020;42(10):1091-1096. https://doi.org/10.1080/0142159X.2020.1798914 [ Links ]
13. Shaw E, Walpole S, McLean M, et al. AMEE consensus statement: Planetary health and education for sustainable healthcare. Med Teach 2021;43(3):272-286. https://doi.org/10.1080/0142159X.2020.1860207 [ Links ]
14. Whitmee S, Haines A, Beyrer C, et al. Safeguarding human health in the Anthropocene epoch: Report of the Rockefeller Foundation-Lancet Commission on planetary health. Lancet 2015;386(10007):1973-2028. https://doi.org/10.1016/S0140-6736(15)60901-1 [ Links ]
15. Boelen C, Pearson D, Kaufman A, et al. Producing a socially accountable medical school. AMEE Guide No. 109. Med Teach 2016;38(11):1078-1091. https://doi.org/10.1016/S0140-6736(15)60901-1 [ Links ]
16. Pearson D, Walpole S, Barna S. Challenges to professionalism: Social accountability and global environmental change. Med Teach 2015;37(9):825-830. https://doi.org/10.3109/0142159x.2015.1044955 [ Links ]
17. McLean M, Gibbs T. Addressing code red for humans and the planet: We are in this together. Med Teach 2022;44(5):462-465. https://doi.org/10.1080/0142159X.2022.2040733 [ Links ]
18. World Health Organization. COP26 special report on climate change and health: The health argument for climate action. 2021. https://www.who.int/publications/i/item/cop26-special-report (accessed 14 October 2022). [ Links ]
19. World Health Organization Civil Society Working Group to Advance Action on Health and Climate Change. A all for strengthening climate change education for all health professionals: An open letter to universities and all education stakeholders. https://climateandhealthalliance.org/wp-content/uploads/2022/06/Curriculum-letter.pdf (accessed 14 October 2022). [ Links ]
20. Tun S, Martin T. Education for Sustainable Healthcare. A Curriculum for the UK. London: Medical Schools Council, 2022. https://www.medschools.ac.uk/media/2949/educattion-for-sustainable-healthcare_a-curriculum-for-the-uk_20220506.pdf (accessed 14 October 2022). [ Links ]
21. General Medical Council. Outcomes for Graduates. London: GMC, 2018. https://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates (accessed 14 October 2022). [ Links ]
22. Tun S, Wellbery C, Teherani A. Faculty development and partnership with students to integrate sustainable healthcare into health professions education. Med Teach 2020;42(10):1112-1118. https://doi.org/10.1080/0142159x.2020.1796950 [ Links ]
23. Musaeus P, Wellbery C, Walpole S, et al. E-collaborating for environmentally sustainable health curricula. In: Azeiteiro U, Filho WL, Aires L, eds. Climate Literacy and Innovations in Climate Change Education. Climate Change Management. Berlin: Springer, 2018. [ Links ]
24. Davis-Reddy CL, Vincent K. Climate Risk and Vulnerability: A Handbook for Southern Africa. 2nd ed. Pretoria: Council for Scientific and Industrial Research, 2017. [ Links ]
25. Chersich MF, Wright CY, Venter F, et al Impacts of climate change on health and wellbeing in South Africa. Int J Environ Public Health 2018;15(9):1884. https://doi.org/10.3390/ijerph15091884 [ Links ]
26. Godsmark CN, Irlam J, van der Merwe F, et al. Priority focus areas for a sub-national response to climate change and health: A South African provincial case study. Environ Int 2019;122:31-51. https://doi.org/10.1016/j.envint.2018.11.035 [ Links ]
27. Department of Environment Forestry and Fisheries. National Climate Change Adaptation Strategy. Pretoria:DEFF, 2019. [ Links ]
28. National Department of Health. National Climate Change and Health Adaptation Plan 2020 - 2024. Pretoria: NDoH, 2019. [ Links ]
29. Academy of Science of South Africa (ASSAf). Reconceptualising health professions education in South Africa. 2018. http://research.assaf.org.za/handle/20.500.11911/95 (accessed 14 October 2022). [ Links ]
30. Gandhi V, Al-Hadithy N, Göpfert A, et al Integrating sustainability into postgraduate medical education. Future Healthc J 2020;7(2):102-104. https://doi.org/10.7861/fhj.2020-0042 [ Links ]
31. Mortimer F. The sustainable physician. Clin Med 2010;10(2):110. [ Links ]
32. Lokotola CL, Mash R, Naidoo K, et al. Climate change and primary health care in Africa: A scoping review. J Climate Change Health 2023;11:100229. https://doi.org/10.1016/j.joclim.2023.100229 [ Links ]
33. Global Green and Healthy Hospitals. Case studies. https://greenhospitals.org/case-studies (accessed 20 April 2023). [ Links ]
34. Irlam J, S Reid, H-A Rother. Education about planetary health and sustainable healthcare: A national Delphi panel assessment of the AMEE Consensus for health professions education in South Africa. Afr J Health Professions Educ 2024;16(1):e327. [ Links ]
 Correspondence:
Correspondence:
J H Irlam
james.irlam@uct.ac.za
Accepted 19 July 2023














