Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
African Journal of Health Professions Education
versión On-line ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.15 no.2 Pretoria jun. 2023
http://dx.doi.org/10.7196/AJHPE.2023.v15i2.1683
RESEARCH
The operational approach to and challenges of high-technology clinical simulation in South Africa
R van WykI; M LabuschagneIII; G JoubertII
IPhD (HPE), BComm (IT); Clinical Simulation and Skills Unit, School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIBA, MSc; Department of Biostatistics, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIMB ChB, MMed (Ophth), PhD (HPE); Clinical Simulation and Skills Unit, School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Research has been published on the application of high-technology clinical simulation as a training tool in South Africa (SA). However, little has been published on the operational approach taken and challenges faced when establishing and running a high-technology clinical simulation facility
OBJECTIVE: To ascertain the current operational approach taken and challenges faced regarding high-technology clinical simulation by SA simulation facilities
METHODS: A quantitative descriptive study with an online questionnaire survey was conducted with representatives of simulation facilities at SA public health professions training institutions where high-technology simulation is used. The questionnaire consisted of sections dealing with the characteristics of and challenges faced by the facilities and the following operational aspects: management, funding, staffing and staff development, curriculum integration, physical environment and research
RESULTS: Forty-two institutions were approached and 23 (54.8%) participated. Simulation was used at 16 (69.6%) of these institutions, representing 17 facilities, with 14 (82.4%) using high-technology simulation. Nine (64.3%) of the 14 simulation facilities were custom built. Four (28.6%) facilities had dedicated technical staff. The participating simulation facilities acquired their funding mainly through institutional budget allocations (78.6%) and government education grants (78.6%). The number of students using high-technology simulation facilities was the highest among the fifth-year (median 195) and sixth-year (median 21) students
CONCLUSION: Large student groups and a lack of trained simulation staff are some of the challenges being faced by high-technology simulation facilities in SA. Recommendations and guidelines should be established to ensure effective integration and alleviation of all operational aspects and challenges
High-technology simulation refers to using a high-technology simulator(s) during a simulation experience.[1] These simulators are computerised and program-controlled by someone external to the learner.[2] High-technology simulators include human patient simulators,[3] a flat-screen simulation that is not a manikin but a program running on a personal computer (PC) and a smartphone or tablet to train students how to use didactic information.[4] Recent developments include augmented reality where a digital overlay over real-world objects is created,[5] and virtual reality where a headset is used to create a digital environment and a scenario where students can interact with the virtual procedure. Laparoscopic surgery and endoscopic trainers are used extensively for training and deliberate practise of procedures. Students' ability and progress are automatically monitored and feedback is provided by the software.[6] For the purpose of this study the term 'high technology' was used instead of high fidelity, as the latter means a higher level of realism. The dimensions involved in fidelity are the physical, psychological and social factors, the culture of the group and the participants' mode of thinking.[4]
Research has been published on the application of high-technology clinical simulation as a training tool for specific clinical scenarios in South Africa (SA).[7-10] However, little has been reported on the operational approach taken and challenges faced when creating and running a high-technology clinical simulation facility in SA. Swart et al.[7] stated that financial constraints to obtain simulators and a lack of dedicated simulation technicians, trained educators and time for simulation activities are the major barriers to simulation implementation. The importance of using simulation to expand the teaching platform as SA student numbers increase, was the focus of the research reported by Labuschagne et al[11] Phillips[12] concluded that the high human and financial investment of a simulation facility in SA should mandate effective use of the facility.
Due to the specific SA training platform, case mix (tuberculosis, HIV, non-communicable diseases, such as diabetes, hypertension and cardiovascular conditions) and resources (limited access to simulation facilities and expensive equipment),[8] the local operational challenges may differ from those established in developed countries.
According to Calzada,[13] healthcare simulation is currently experiencing an international rise in usage. Apart from the actual simulators, operational subsystems are needed for best practices to achieve optimum operational functioning in high-technology simulation. Several authors identify these additional subsystems as management, funding, staffing and staff development, curriculum integration, physical environment considerations and research outputs.[14-16]
The objective of the current study was to establish the operational approach taken and challenges faced regarding high-technology clinical simulation by simulation facilities at accredited SA public health professions training institutions.
Methods
Design
A quantitative descriptive study was performed. A deductive research approach was followed, as it tested the existing theory[17] of high-technology simulation against how it is experienced in SA facilities.
Sampling and participants
The target population comprised representatives of simulation facilities at SA public health professions training institutions where high-technology simulation is used. Only institutions that have accredited professional programmes (the South African Nursing Council, the Health Professions Council of South Africa and the South African Pharmacy Council) were included; private institutions were excluded. An institution could have more than one simulation facility. Each institution identified was approached to ascertain how many simulation facilities they have. Using the contact details obtained from the relevant council's website, the listed representative of the institution was contacted to determine whether simulation is part of the training platform at a specific institution and who the contact person for the simulation facility is. The identified contact person was requested to complete the questionnaire used to collect information. The Clinical Skills and Simulation Unit, Faculty of Health Sciences, University of the Free State (UFS), Bloemfontein, SA, was excluded from the study owing to the first (RvW) and second (ML) authors' affiliation to the facility.
Data collection
An online questionnaire survey was conducted by the first author (RvW). It was developed using the Education Survey Automation Suite (EvaSys), available at www.surveys.ufs.ac.za and hosted by UFS. The URL of the questionnaire was sent to participants by email. The questionnaire was divided into eight sections. The first section recorded demographic data. The following sections included the six operational subsystems: management aspects, funding, staffing and staff development, curriculum integration, physical environment and research. These operational subsystems were derived from Palaganas et al.,[14] Labuschagne[15] and Kyle and Murray.[16] The final section focused on the challenges faced by the units and was divided into initial challenges faced when the unit was established and the day-to-day challenges. The layout of the questionnaire was created according to the best practices and visual design proposed by Artino et al.[18] Using both national and international literature contributed to validity during the literature review, which served as a guide for the development and content of the questionnaire.
Pilot study
A pilot study was conducted with representatives of two facilities that use simulation as a teaching tool. Feedback on the design, clarity and correctness of the questionnaire by the two representatives was obtained telephonically. The pilot study, together with the fact that a questionnaire survey is a structured research instrument, enhanced the reliability. The responses from the pilot study were used in the main study, as no changes to the questions or methodology were required.
Data analysis
The data were collected and collated into a blinded Microsoft Excel, version 16.0 (Microsoft Corp., USA) sheet by the first author (RvW). The data were analysed by the Department of Biostatistics, UFS, in terms of frequencies and percentages. Answers to open-ended questions were coded into themes by the first author (RvW), followed by quantitative analysis.[19] The use of open-ended questions coded into themes also increased validity, as these were based on the participants' responses rather than themes created beforehand by the researcher.
Ethical considerations
Approval for the research project was obtained from the Health Sciences Research Ethics Committee (HSREC), UFS (ref. no. HSREC 115/2017). Permission from the dean of the Faculty of Health Sciences and the vice-rector, Research, UFS, was obtained for the project. Permission to conduct the survey with the relevant simulation facility representative was requested from the various health professions training institutions in the target population. In most cases (n=10), approval from the relevant dean or department head was sufficient to complete the questionnaire, while others had an institutional or faculty ethics committee or a research gatekeeper committee that had to approve participation. An information letter and an informed consent form to be signed were sent to representatives by email.
Results
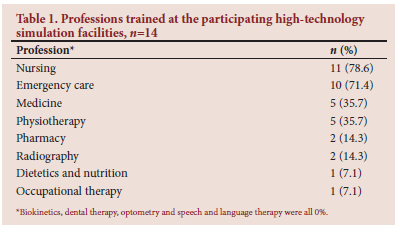
A total of 128 representatives from 12 health professions, representing 42 institutions, were contacted. These institutions were classified into three categories: universities (n=23), nursing colleges (n=12) and emergency care colleges (n=7). Replies were received from 27 (64.3%) institutions, but 4 (that indicated that they use simulation) did not complete the survey, leaving 23 (54.8%) participating institutions. These 23 institutions consisted of 19 (82.6%) universities, 2 (16.7%) nursing colleges and 2 (28.6%) emergency care colleges. Seven (30.4%) of the 23 participating institutions indicated that no simulation was used. These 7 institutions comprised 5 (26.3% of respondents) universities and 2 (100% of respondents) nursing colleges. Simulation was used at 16 (69.6%) of the participating 23 institutions - 14 universities and 2 emergency care colleges. The 16 institutions represented 17 simulation facilities, as one of the universities had two separate participating facilities. High-technology simulation is used in the participating facilities (n=14) across 8 professions (Table 1), with nursing and emergency care being the most commonly represented professions. Ten (71.4%) of the facilities serve more than one profession.
Fourteen of the participants indicated that high-technology simulation was used at the facility they represented (each from a different institution). Reasons listed for no high-technology simulation (n=3) was that no funds were available (n=2) and that there was no need for high-technology simulation in the curriculum (n=1). Only 4 (28.6%) of the 14 (28.6%) facilities were stand-alone facilities with their own management systems in place, whereas 10 (71.4%) were situated in a clinical department.
With regard to the most prevalent documentation used by the facilities, 10 (71.4%) used student feedback forms, while 9 (64.3%) had a financial plan and 9 (64.3%) had policy documents in place. Documents that were used the least were strength, weaknesses, opportunities and threats (SWOT) analyses, which were performed by only 3 (31.4%) facilities. Performance indicator documents were used by 4 (28.6%) and only 5 (35.7%) facilities had needs analysis documents.
The median number of full-time employees at a stand-alone simulation facility was 5 (range 1 - 9) and where a simulation facility was part of another department, a median of 2 (range 0 - 13) full-time staff was allocated for simulation. Three respondents indicated that in some instances, multiple roles were covered by the same staff member, whereas in 2 cases, facilities made use of staff (content specialists) on an ad hoc basis to assist with simulations.
Four (28.6%) facilities had dedicated technical staff. Of the facilities surveyed, 46.2% indicated that they had no back-up plan in place if a staff member was absent on the day of a simulation. The other 53.9% attempted to ensure that all staff members were involved in the planning phase so that another staff member could cover certain aspects when someone was absent.
The participating simulation facilities mainly acquired their funding through institutional budget allocations (78.6%) and government education grants (78.6%). Fifty percent of the facilities also received funds through government health grants. These institutional and government funding streams were related to the day-to-day teaching and learning activities of the institutions' students. Other sources of income were external (nongovernment funding, also referred to as third-stream income) and were mainly generated through certification training courses (35.7%) and other training provided to external clients (57.1%).
During the survey, 78.6% of the participating facilities stated that they used a financial steering committee, and the same number had a procurement policy in place.
Nine (64.3%) of the simulation facilities were custom built, while the other 5 used pre-existing spaces allocated to them. Twelve (85.7%) of the surveyed facilities had dedicated rooms available for simulations, but only 3 (21.4%) had separate, dedicated debriefing areas. Regarding the latter, only 50.0% of the facilities had spaces that could be used for debriefing (3 had dedicated debriefing rooms, and the remaining 4 used multipurpose spaces).
With regard to audio-visual equipment, 11 (78.6%) facilities used it to stream or record some or all of the high-technology experiences in the facility. In 10 (71.4%) facilities, these were recorded for later viewing, and 4 (28.6%) facilities also had the capabilities to stream the simulations to observers in a separate room. Eight (57.1%) of the facilities had control/observation rooms. Six (75%) used rooms that were separate from the areas where the simulation experience took place.
The highest frequencies of high-technology simulation usage were among third-year (9 facilities), fourth-year (8 facilities) and postgraduate (8 facilities) students. The number of students using high-technology simulation facilities was highest among the fifth-year (median 195) and sixth-year (median 21) students. While almost all (92.9%) of the facilities used high-technology simulation for teaching and learning activities, only 50% used it for summative assessment, and 57.1% used it for formative assessment.
In the facilities with research outputs (6 of 14; 42.9%), the involvement of the simulation staff was mainly as postgraduate examiners or postgraduate study leaders (5 each). In 4 facilities, research outputs were via the publication of research articles in journals, and in 3 instances, by postgraduate students using high-technology simulation equipment for research. Five of 6 (83.3%) facilities were producing research outputs pertaining to a health profession discipline using high-technology simulation, with the research focusing on simulation or high-technology simulation.
Four (28.6%) of 14 respondents were involved in their respective facility's initial establishment. Each of these respondents (n=4) were requested to list up to 5 specific challenges (open-ended question) they had experienced with the initial set-up of the facility. These 5 aspects were ranked (most important = 5; least important = 1) and combined into themes.
All 4 (100%) respondents pointed out that finding an appropriate space, infrastructure issues and layout had been a challenge during the initial setup (ranked 4; range 1 - 5). Three (75%) respondents indicated that technical difficulty with PCs (ranked 4; range 3 - 5) and budget constraints (ranked 2; range 1 - 3) had been challenging.
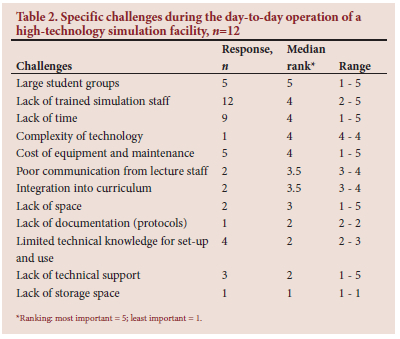
Similarly, each respondent was asked to list up to 5 specific challenges (open-ended question) experienced with the day-to-day running of the facility. These aspects were ranked (most important = 5; least important = 1). The aspects were combined into themes and are reported in Table 2. Two respondents did not complete the question.
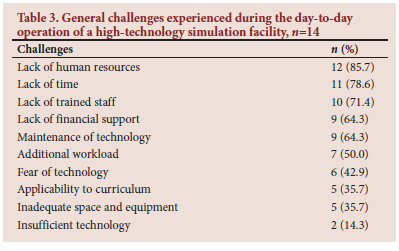
Other general challenges experienced were given as a list to select from and were not ranked. During the initial set-up of the facilities (n=4), lack of trained staff (n=4; 100%) and lack of human resources (n=3; 75.0%) had been the most prevalent challenges.
General challenges faced by facilities during the day-to-day running (n=14) are listed in Table 3. Respondents were asked what approach (if any) they took to alleviate the day-to-day challenges. Six indicated that they were planning and budgeting for additional simulation training for staff, including technical training for using high-technology manikins correctly and effectively, as well as for general maintenance. One respondent indicated that they planned training in collaboration with other simulation facilities to share knowledge. Three respondents indicated that they needed more physical space, of which one had successfully motivated for additional space based on the facility's usage statistics.
Two respondents indicated that they worked closely with discipline-specific staff and lecturers (from other departments) to help create the scenarios well in advance to avoid rushing it later. These 'subject matter experts' also helped to run the scenario in the simulation facility. Three of the facilities motivated for additional dedicated staff on an annual basis to try to alleviate the staff shortage. One mentioned that in these motivations, they also requested additional time in the students' schedule to use simulation.
Two respondents commented on the challenges of high-technology simulation. One referred to the expensive equipment. The other said that learning objectives should be defined clearly and that high-technology could be distracting ('nice to play with but not always the best teaching tool'), and that medium-fidelity equipment might often achieve the same teaching and learning goals.
Discussion
The response rate differed between the three categories of institutions included in the study. The low response rate from emergency care colleges (28.6%) and the high participation rate of universities (82.6%) skewed the data in favour of the universities, which was a study limitation. With 2 nursing colleges indicating that they did not use any simulation and the other 10 not responding, nursing colleges possibly do not use simulation and are excluded from the discussion. Numbers did not allow for the comparison of different types of facilities.
Management aspects
Considering the documentation in place at participating SA facilities, only 35.7% had conducted a formal needs analysis. A needs analysis is crucial to set goals and strategies,[20] and should also be the starting point for any management decisions. Furthermore, the needs analysis should be reviewed periodically to adapt to changing needs and the environment.
The use of a SWOT analysis should be an ongoing process[21] over the lifetime of a facility. However, only 21.4% of facilities had conducted a SWOT analysis.
Staffing and staff development
A lack of trained staff and human resources was a challenge for facilities during the initial set-up and also during day-to-day operations. Four participating facilities had dedicated technical simulation staff while the other 10 had none (without specifying how this gap was bridged). The lack of dedicated technical simulation staff might place more pressure on the educational staff to prepare and run potentially complex simulations. Koh and Dong[22] stated that the development of competent simulation technicians, with scope for further professional development, is essential for uninterrupted and successful simulation operations.
According to Andreatta,[23] simulation facilities, irrespective of size, need at least three staff roles, which include executive administration, educational assistance and technical operations. Staff and educators who are unavailable, sick or late could also be a barrier to effective simulation.[24]
To ensure effective multi-tasking by individuals in some areas, it is important to equip them with the correct resources in terms of training and development.
This was especially relevant in light of COVID-19 protocols,[25,26] when some staff members were not able to be on site. It is important to make sure that all staff members have a basic overview and understanding of all topics of simulation, especially of high-technology simulation and its complexities. This approach would ensure that staff with different designations could stand in for each other when a staff member is not available.
Funding
High-technology simulation facilities can be expensive to start and run, as equipment, maintenance of equipment and staff costs might be high.[13] Funding is a critical element to run a successful high-technology simulation facility.[27]
Because financial control is such an important factor in achieving sustainable success, it is advisable that a financial steering committee should be in place for a simulation facility, especially with the relatively higher costs involved in high-technology simulation modalities.[13,27-30]
Third-stream income was mostly generated through providing continued professional development (CPD) activities to external clients, although other options for external funding are once-off corporate sponsorships and research funding. An advantage of third-stream income could be higher income through well-attended courses, especially when these are well marketed and advertised and the facility has an established reputation.[13] Disadvantages of external funding could be a lack of focus on the institution's core mission.[31]
Physical environment
Contextual fidelity plays an important role in the students' experience of simulation. Therefore, the environment must resemble their actual workplace as closely as possible. This setting must also include resources such as consumables, patient documentation and medical equipment required for the specific simulation experience.'3- The SA facilities that participated in the survey indicated that infrastructure and finding appropriate spaces (layout) were challenges. The majority used dedicated observation/control rooms, and footage of the simulation can be recorded or streamed to an observation area.
When planning a room that will be used for high-technology simulation, it is important to keep increasing technical complexities in mind.[32] One should be mindful of the electrical systems in place, i.e. where high-technology simulation equipment will be installed. There is no one-size-fits-all approach as far as infrastructure is concerned. Flexibility is key, and the use of spaces depends on the needs analysis for the simulation activities, available options and available funds to adapt existing structures.[30]
Curriculum integration
The effective integration of simulation into the curriculum, which consists of the simulation experience and debriefing, can also lead to better training of professional attributes in a safe environment. These attributes include, among others, interprofessional collaboration, professionalism, communication and leadership.[11] One has to ensure that the students' theoretical knowledge is at a point where it will be beneficial to move forward with skills and/or simulation. The learning outcomes should be analysed and a decision should be made whether skills training will be required.
From the data collected, it seems that the participating SA facilities have integrated high-technology simulation correctly from a curriculum scaffolding and assessment point of view.
Research
Using simulation for research can be broadly divided into two categories, i.e. research about simulation education, and using simulation and simulators to perform research on health concepts, interventions and equipment.[33] Research can also be conducted to secure additional income for a facility through research grants.[34] Many high-technology simulators record data while they are used, which could easily be obtained for quantitative analyses on various topics and interventions. It is important to make sure that staff are trained in research methodology, specifically while using simulation. In the participating SA facilities, most of the research conducted was in the form of postgraduate studies focusing on simulation education. Research outputs are an important component of any tertiary education institution, but to achieve this in a busy simulation facility can be challenging. A strategy to consider is to combine existing teaching and learning activities into a research project.
Challenges
When considering high-technology simulation, operational challenges and obstacles might cause staff members to question the use of high technology in clinical simulation. These challenges include a lack of time, fear of technology, lack of human resources, inadequate space and equipment, lack of trained staff (computer literacy), lack of financial support, insufficient technology, lack of maintenance of technology, additional workload and lack of applicability to the curriculum.[35,36]
Conclusion
Institutional budget allocation and government education grants are the major sources of income for high-technology simulation at the participating institutions. With regard to staffing allocation, it was indicated that multiple roles are covered by the same staff members (multi-tasking). Some standalone facilities use staff on an ad hoc basis to assist with simulations. Large student groups, insufficient time for simulation activities and a lack of trained simulation staff are some of the most frequent challenges being faced by high-technology simulation facilities in SA. Integration of high-technology simulation into a curriculum should follow accepted educational principles and should contribute to achieve the relevant educational outcomes. When training topics are considered for high-technology simulation, it is important to not only focus on the teaching and learning philosophies of such simulation, but also on behind-the-scenes and more practical aspects of making sure that high-technology simulation is used optimally. Potential research outputs should be explored and could even add to generating income for a facility.
Changes in one aspect could influence other aspects and effective integration of the different aspects would enhance high-technology clinical simulation in SA. Recommendations and guidelines should be established to ensure effective integration of all aspects of high-technology clinical simulation. This is essential to alleviate or overcome operational challenges and secure longterm sustainability of high-technology clinical simulation in SA.
Declaration. The research for this study was done in partial fulfilment of the requirements for RvW's PhD (HPE) degree at the University of the Free State.
Acknowledgements. We thank the participants of the simulation facilities who participated in the study, the Health and Welfare Sector Education and Training Authority (HWSETA) for funding and Dr Daleen Struwig, medical writer/editor, for technical and editorial preparation of the manuscript.
Author contributions. RvW and ML conceptualised the study, GJ provided methodological input. RvW collected the data and GJ analysed the data. RvW drafted the manuscript, which all authors reviewed and edited.
Funding. Health and Welfare Sector Education and Training Authority (HWSETA).
Conflicts of interest. None.
References
1. Ostergaard D, Dieckmann P. Simulation-based medical education. In: Dent JA, Harden RM, eds. A Practical Guide for Medical Teachers. 4th ed Edinburgh: Elsevier 2013:207-214. [ Links ]
2. Huang YM, Rice J, Spain AE, Palagas JC. Terms of reference. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer, 2015:xxi-xxxiv [ Links ]
3. Milkins L, Moore C, Spiteri J. Simulation Based Education: Professional Entry Student Education and Training. Gladesville: Health Education and Training Institute (HETI), 2014. https://www.voced.edu.au/content/ngv%3A77832 (accessed 8 June 2022). [ Links ]
4. Lioce L, Lopreiato J, Downing D, et al. and the Terminology and Concepts Working Group. Healthcare Simulation Dictionary. 2nd ed. Rockville, MD: Agency for Healthcare Research and Quality, 2020. https://doi.org/10.23970/simulationv2 [ Links ]
5. CAE Healthcare. Limitless learning. https://caehealthcare.com/hololens (accessed 28 June 2022). [ Links ]
6. Surgical Science. LapSim® - your first choice for laparoscopy training. https://surgicalscience.com/systems/lapsim/ (accessed 28 June 2022). [ Links ]
7. Swart R, Duys R, Hauser ND. SASS: South African Simulation Survey - a review of simulation-based education. South Afr J Anaesth Analg 2019;25(4):12-20. https://doi.org/10.36303/SAJAA.2019.25.42191 [ Links ]
8. Labuschagne MJ. The role of simulation training in ophthalmology. Cont Med Educ 2013;31(4):157-159. [ Links ]
9. Botma Y. Nursing students' perceptions on how immersive simulation promotes theory-practice integration. Int J Afr Nurs Sci 2014;1:1-5. [ Links ]
10. Nel N, Stellenberg EL. Nursing students' perception of simulation as clinical teaching method in the Cape Town Metropole, South Africa. Afr J Health Professions Educ 2015;7(2):176-179. https://doi.org/10.7196/AJHPE.363 [ Links ]
11. Labuschagne MJ, Nel MM, Nel PPC, van Zyl GJ. Recommendations for the establishment of a clinical simulation unit to train South African medical students. Afr J Health Professions Educ 2014;6(2):138-142. https://doi.org/10.7196/ajhpe.345 [ Links ]
12. Phillips M. Starting a high-fidelity simulation laboratory: Pearls and perils. World Crit Care Nurs 2014;9(2):55. [ Links ]
13. Calzada JA. Where's the money, sources of revenue. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer 2015:268-282. [ Links ]
14. Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer, 2015:6-7. [ Links ]
15. Labuschagne MJ. Clinical simulation to enhance undergraduate medical education and training at the University of the Free State. PhD thesis. Bloemfontein: University of the Free State, 2012. https://scholar.ufs.ac.za/handle/11660/1096 (accessed 28 June 2022). [ Links ]
16. Kyle RR Jr Murray WB. Clinical Simulation: Operations, Engineering and Management. Burlington: Elsevier, 2008. [ Links ]
17. Trafford V, Lesham S. Stepping Stones to Achieving Your Doctorate. Berkshire: Open University Press, 2010. [ Links ]
18. Artino AR Jr, la Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research: AMEE Guide No. 87. Med Teach 2014;(36):463-474. https://doi.org/10.3109/0142159X.2014.889814 [ Links ]
19. Mouton J. How to Succeed in Your Master's and Doctoral Studies: A South African Guide and Resource Book. Pretoria: Van Schaik, 2001. [ Links ]
20. Kim S, Hewitt W, Buis JA, Ross BK. Creating the infrastructure for a successful simulation program. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer, 2015:66-89. [ Links ]
21. Johnson GL, Augustson JL. Writing and implementing a strategic plan. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer 2015:364-376. [ Links ]
22. Koh BLS, Dong C. From routine to leadership: Extending the role of simulation technicians in Southeast Asia. In: Nestel D, Kelly M, Jolly B, Watson M, eds. Healthcare Simulation Education: Evidence, Theory and Practice. Oxford: Wiley Blackwell, 2018:190-194. [ Links ]
23. Andreatta P. Simulation center personnel. In: Crawford SB, Baily LW, Monks SM, eds. Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice. Switzerland: Springer Nature, 2019:47-58. [ Links ]
24. Canales C, Huang YM. Expecting the unexpected: Contingency planning for healthcare simulation. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer, 2015:582-591. [ Links ]
25. Clinical Simulation Unit (CSU). Operations Plan for COVID-19 Infection Control Measures in the Clinical Simulation and Skills Unit (CSSU), Francois Retief Building UFS. Bloemfontein: University of the Free State, 2020. [ Links ]
26. Arandjelovic A, Arandjelovic K, Dwyer K, Shaw C. COVID-19: Considerations for medical education during a pandemic 'version 1-. MedEdPublish, 2020;9(1):87. https://doi.org/10.15694/mep.2020.000087.1 [ Links ]
27. Bar-on M, Yucha CB, Kinsey J. Funding a collaborative simulation centre: First step in interprofessional education. Clin Simulation Nurs 2013;9(11):e531-e534. https://doi.org/10.1016/j.ecns.2013.04.014 [ Links ]
28. Barrott J, Sunderland AB, Micklin JP, Smith MM. Designing effective simulation activities. In: Forrest K, McKimm J, Edgar S, eds. Essential Simulation in Clinical Education. Oxford: Wiley Blackwell, 2013:168-195. [ Links ]
29. CAE Healthcare. Proposal guidance for institutions seeking educational grants for human patient simulation. 2013. https://caehealthcare.com/media/files/CAE-Grant-Proposal-Guidance-for-Institutions.pdf (accessed 28 June 2022). [ Links ]
30. Sekandarpoor F, Luevano ER, Crawford SB. Infrastructure and simulation center design. In: Crawford SB, Baily LW, Monks SM, eds. Comprehensive Healthcare Simulation: Operations, Technology, and Innovative Practice. Switzerland: Springer, 2019:111-146. [ Links ]
31. Denning SM, Jewett Johnson CM, Johnson D, Loen M, Patow C, Brannen CK. Partners in simulation: Public academic-private health care collaboration. In: Kyle RR Jr, Murray WB, eds. Clinical Simulation: Operations, Engineering and Management. Amsterdam: Elsevier, 2008:335-344. [ Links ]
32. Seropian MA, Alinier G, Hssain I, et al. Building a simulation center: Key design strategies and considerations. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer, 2015:434-454. [ Links ]
33. Gaba DM. Simulation: More than another tool in the toolbox. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer, 2015:4-16. [ Links ]
34. Kahol K. Securing funding for simulation research. In: Levin AI, DeMaria S Jr, Schwartz AD, Sim A, eds. The Comprehensive Textbook of Healthcare Simulation. New York: Springer, 2013:633-640. [ Links ]
35. Kim S, Hewitt W, Buis JA, Ross BK. Creating the infrastructure for a successful simulation program. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer, 2015:66-89. [ Links ]
36. Johnson GL, Augustson JL. Writing and implementing a strategic plan. In: Palaganas JC, Maxworthy JC, Epps CA, Mancini ME, eds. Defining Excellence in Simulation Programs. Philadelphia: Wolters Kluwer 2015:364-376. [ Links ]
 Correspondence:
Correspondence:
R van Wyk
vanwykr3@ufs.ac.za
Accepted 16 November 2022














