Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.14 n.4 Pretoria Dec. 2022
http://dx.doi.org/10.7196/AJHPE.2022.v14i4.1592
RESEARCH
Supporting undergraduate research capacity development: A process evaluation of an Undergraduate Research Office at a South African Faculty of Medicine and Health Sciences
D L MaraisI; N C Gey van PittiusII
IPhD; Research Development and Support Division, Stellenbosch University, Cape Town, South Africa
IIPhDDean s Division, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND. University-based research capacity development (RCD) mechanisms tend to focus on staff and postgraduate students, with few structures targeted at undergraduate students. Support for undergraduate research must be tailored to the unique requirements of research at this level, while maintaining links with relevant structures in both the RCD and teaching and learning domains.
OBJECTIVE. To conduct a process evaluation of the Undergraduate Research Office (URO) in the Faculty of Medicine and Health Sciences at Stellenbosch University, South Africa, using RCD and characteristics of excellence in undergraduate research criteria as benchmarks.
METHODS. A process evaluation of URO's first 6 years was conducted using a logic model of URO's inputs, activities, and outputs. Through a retrospective document review, a descriptive analysis of URO's inputs and activities (narrative) and URO's outputs (statistical) was conducted.
RESULTS. Following a description of inputs and activities, results present URO's outputs as a measure of the uptake of these activities. From 2015 to 2020, 259 undergraduate research projects were completed. Research consultations, workshops and undergraduate presentations at the faculty's Annual Academic Day have more than doubled since URO's inception. The Undergraduate Research Ethics Committee has reviewed 243 ethics applications since 2015, with a 1 - 2-week turnaround time. A total of 134 funding applications worth ZAR705 986 have been awarded for research project, conference presentation and publication costs.
CONCLUSION. Results show the potential impact of a formal undergraduate research support entity on the undergraduate research outputs of a Faculty of Medicine and Health Sciences. This article highlights elements for success for formal undergraduate research support, and identifies gaps going forward.
The value of building capacity to conduct research to address health challenges in low- and middle-income countries is well recognised.[1-3] Various strategies have been implemented, including formal research training at higher education (HE) institutions[4,5] and research-focused degrees.[6] In parallel, the importance of evidence-based healthcare (EBHC), as endorsed by the Health Professions Council of South Africa (HPCSA), has seen the integration of EBHC teaching in medical/health science faculties.[7-9] In addition to the system- and patient-level benefits of a research-skilled health workforce, individual-level benefits include critical thinking and problem-solving.[10-13] This article focuses on the development of research capacity in undergraduate health sciences students.
Teaching on EBHC - how to use research - has generally become an integral part of undergraduate medical and health science curricula.[14] Teaching undergraduate students how to do research, including their own research projects, takes several forms.[13,15] Research teaching may be structured into the curriculum as a stand-alone course/module, possibly involving compulsory research projects. Elsewhere, research is extracurricular, either as an elective course/programme or as experiential learning opportunities. The likelihood of students taking up these extracurricular opportunities depends on a research-enabling environment, including awareness-raising about its value and opportunities for doing research. A third approach involves hybrid models that integrate components of structured teaching and elective training and/or experience. Enhancing student engagement in research depends on research-supportive staff, programmes, and environments.[16]Previous research has identified enablers of undergraduate research, which we have classified into three categories: enabling environment; training and resources; and awareness, opportunity, and recognition (see Table 1, columns 1 and 2).[16] Each element might apply to specific programmes or to a faculty as a whole.
HE institutions have diverse responses to the challenges of fostering a research culture and developing research capacity among staff/students.[28-30] Typically, this is co-ordinated through some form of research management and/or institution-wide/faculty-based support structure, incorporating various components. Table 1 (column 3) also shows components of research development interventions, identified by Cooke et al.[31] in a scoping review of research capacity literature. Research-capacity development (RCD) is often seen as a means to an end - increasing research outputs/impact -rather than an end in itself.[32] For undergraduate students, however, the process of learning about and gaining research skills is arguably more important than the 'end' (output).
Nevertheless, building only individual research skills may not be sustainable; RCD should be embedded in research support structures[33,34] established in a favourable institutional environment.[28,35] The existence of an RCD office signals the intentions of management to support research, and is critical for fostering a culture conducive to research and innovation.[36] Other elements of RCD success include commitment/support from all levels of leadership and management, building relationships and buy-in from staff, and staffing the RCD office with highly qualified professionals who can straddle professional, academic, and service-oriented domains.'[30,37-39]
University-based RCD mechanisms tend to focus on staff and postgraduate research support,[37,40] with few structures/activities targeted at undergraduate students. With both curricular and extracurricular activities, and the focus on enhancing research-related capacity, undergraduate-level research-supportive strategies cut across two core HE functions: research, and teaching and learning. Support for undergraduate research must therefore be tailored to the unique requirements of research at this level, while maintaining links with relevant structures and processes in both the research and teaching/learning domains. Drawing on international experience, the Council on Undergraduate Research (CUR) identified best practices for fostering undergraduate research,[41] adapted and summarised for relevance to this article in Table 1 (columns 4 and 5). Notably, these characteristics of excellence in undergraduate research (COEUR) combine elements of RCD mechanisms outlined above (e.g. administrative support; funding), while highlighting links to teaching/learning domains (e.g. curriculum; assessment activities).
In this article we document the process of setting up and operationalising a central support structure for undergraduate research, and evaluate this against RCD and COEUR best practices. Process evaluations of the internal processes that facilitate effective research are rare, despite this being one of the main functions of university research management structures.[33] This is a gap this article aims to address.
Process evaluation
A logic model depicts how a programme theoretically works to benefit its participants, and is thus a useful framework for programme evaluation.[42] It demonstrates the links between a programme's inputs (resources), activities (what the programme does with the inputs), outputs (direct products of the activities, also called units of service), and outcomes (the benefits or changes that result).[42-44] Savaya and Waysman[44] also recommend that logic models start with a situational needs analysis. Process evaluations document the process of a programme's implementation to determine whether programme activities have been implemented as intended, and resulted in particular outputs.[45,46] While outcome evaluations assess the effectiveness of a programme in producing change, process evaluations focus on the first three columns of the logic model: inputs, activities, and outputs.[45,46] Formative process evaluations are useful in fine-tuning programmes and keeping them on track.'471 To develop our process evaluation plan, we followed the six steps proposed by Linnan and Steckler[47] and Saunders et al,[48] applying these to the relevant components of our logic model, shown in Fig. 1.
In programme evaluation, benchmarks can be used either as a baseline or as aspirational targets against which a programme can be compared.[42] Attending to the importance of theory in informing an evaluation framework,[43,48] we employed the latter conceptualisation of benchmarks - drawing on the best practices in RCD and undergraduate research presented in Table 1. The 'programme' in this article is conceptualised as the research support service that URO provides to Faculty of Medicine and Health Sciences (FMHS) undergraduate students. Our aim was to conduct a process evaluation of URO's first 6 years, with two objectives: (i) to describe URO's inputs and activities; and (ii) to assess the associated outputs as a measure of how the implementation of activities aligned with identified best practice benchmarks. In the next two sections, we describe the situation analysis, inputs and activities (steps 1, 2 and 5 of the process evaluation). In the methods section we present the final process evaluation plan, focusing on URO's outputs in the analysis and results (process evaluation steps 3, 4 and 6).
Context: Target population and needs
In SA, learning how to conduct research is a compulsory component of health sciences training programmes through dedicated research methods modules (human nutrition, nursing and midwifery, occupational therapy, physiotherapy, and speech-language and hearing therapy), as mandated by the HPCSA. Research is an elective option in the undergraduate medical curriculum (MB ChB), although the HPCSA increasingly emphasises the necessity of research training, with a compulsory research assignment for postgraduate medical curricula. SA universities have incorporated research in these programmes in different ways.[22,24-26,49] At Stellenbosch University (SU)'s FMHS, health sciences students conduct primary and secondary research in groups during their third and fourth years as part of the research modules, while MB ChB students may complete an individual research project during their 6-year undergraduate degree, although there is no structured research teaching in the curriculum. EBHC has also been incorporated into health sciences and medical curricula at the faculty.[7,8,14]
These curricular/extracurricular undergraduate research activities take place within the broader institutional context of the research-intensive SU, and a FMHS that aims to address major health challenges facing the African continent. The central Division for Research Development provides institution-wide support/oversight for research at SU, while the faculty's Research Development and Support Division (RDSD) supports specific FMHS research activities. The RDSD comprises the Tygerberg Doctoral Office, Research Capacity Development and Funding Office (staff and postgraduate students), Health Research Ethics Office and Grants Management Office, and in 2020 the Registrar Research Support Office was established. Until 2015, undergraduate research ethics applications were submitted along with staff and postgraduate student applications to the Health Research Ethics Committee (HREC), and there was no dedicated funding available for undergraduate research.
URO was established in 2015 following the Vice Dean of Research and Internationalisation's commitment to supporting undergraduate research, and advocacy for co-ordinated research support by the special interest group (SIG) for undergraduate research. The SIG conducted research into enablers and constraints of undergraduate research,[16] with the URO head now leading the research team interviewing staff and students from all programmes. This supplemented URO's needs assessment during its first year, which involved meeting key stakeholders (staff/students) to create a map of FMHS undergraduate research activities and challenges. This process was critical in learning how URO could support structured (health sciences) and elective (medical) research programmes and in obtaining buy-in from environments/staff involved in undergraduate research.
The URO head also conducted desktop research on and networked with undergraduate research support at all other medical faculties in SA to benchmark how research was - or was not - incorporated into medical curricula. Based on this situational analysis, URO focused on three core functions (research capacity-building; ethics review; funding) and two support functions (co-ordination/oversight; awareness-raising/showcasing). To the best of our knowledge, URO is the first and currently only central structure dedicated to supporting undergraduate research at a faculty of medicine and health sciences in SA.
Inputs and activities
In Table 2, we present URO's inputs and activities mapped onto the evaluation framework benchmarks.
Inputs
Inputs are conceptualised as the resources invested to establish and enable URO to perform its planned activities. In describing URO's context and characteristics here, we are addressing process evaluation steps 1 and 4 (Fig. 1). URO was established as a fully fledged
office within the RDSD, aligning with COEUR's recommended structure of a central support office for undergraduate research (Table 2, 3rd column). URO is organisationally and operationally linked to the faculty's RDSD; office space and equipment were made available in the RDSD, and the URO head reports directly to the Vice Dean. The URO head was appointed to establish and manage the office through funding from the SU Rural Medical Education Partnership Initiative, with FMHS commitment to permanently fund this post. The appointed head is a qualified health professional, with Masters-level training on appointment, and experience in health research, project and grant management and research ethics training. The post built in time for continued professional development, which the head has used to complete her PhD and engage in ongoing academic and research work.
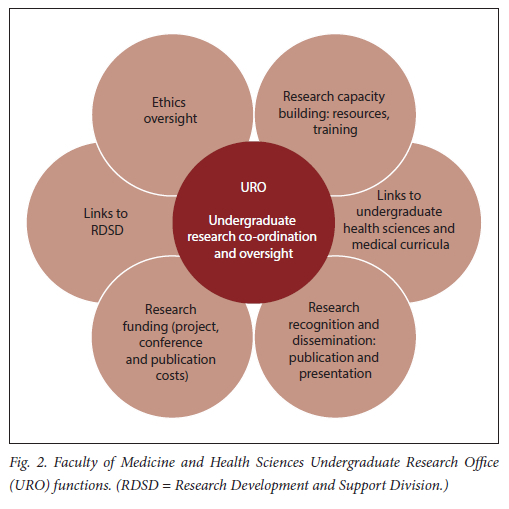
URO's mandate is to co-ordinate, support and grow undergraduate research at the FMHS through its core and support functions (Fig. 2). Thus URO incorporates several RCD components while creating links with medical and health sciences academic programmes.
Activities
Activities are conceptualised as the services that URO provides to fulfil its mandate. In describing these activities below, we address process evaluation step 2. The SIG was formalised into the Undergraduate Research Committee (URC), co-chaired by the Vice Dean and URO head with representation from all undergraduate research programmes and student body, to act as a co-ordination mechanism and facilitate communication between key stakeholders. Initially meeting quarterly, URC was restructured in 2018 into an oversight/steering committee, meeting annually. The URO head meets regularly with other RDSD office heads around operations of the RDSD as a research support unit, and with the Vice Dean to ensure alignment with URO's strategic objectives and performance indicators. She also serves on Subcommittee C of the Research Committee of Senate, the faculty's research committee, to ensure links with the broader research culture.
All health research involving human participants in SA requires approval from a HREC. To streamline and fast-track ethics approval of undergraduate research, the Undergraduate Research Ethics Committee (UREC) was established in October 2015 as a subcommittee of the two HRECs overseeing research ethics in the FMHS. Terms of reference and standard operating procedures (SoPs) for UREC were integrated into HREC SoPs and approved by SU's Senate Research Ethics Committee. UREC comprises a chair, vice-chair and members representing undergraduate research environments. The URO head serves as UREC co-ordinator and is a full committee member (reviewer). UREC reviews minimal-risk undergraduate and Honours-level research via expedited review procedures. URO also established an ethics consultation service for students submitting ethics applications, and created resources, available through URO's website, to guide students on ethical and regulatory aspects of research.
The Undergraduate Research Fund was created to facilitate compulsory research and incentivise elective research. A commitment of funding was secured from the FMHS's Subcommittee C towards three sub-funds: Undergraduate Research Project Fund (ZAR5 000 per award), Undergraduate Conference Presentation Fund (ZAR10 000 per award) and Undergraduate Publication Incentive Fund (ZAR10 000 per award). Application forms, regulations and procedures were set up, and calls for applications initiated in 2015.
The development of URO's website was critical as the mechanism for offering its services and resources. Generic research-related resources were created, alongside tailor-made resources addressing specific requirements of different programmes and their student researchers. In addition to the guidance documents and videos on the website, a one-on-one consultation service was offered to all undergraduate student researchers. A workshop programme was offered to health sciences programmes, addressing topics such as literature searching and referencing, academic writing and research ethics. These workshops supplemented the taught research courses in these programmes. The URO head has also been co-leading the team developing a new compulsory MB ChB research module. The URO head attended and gave MB ChB lectures to raise awareness around research opportunities for MB ChB students. New resources were added to the 'Roadmap to Research' resource page each year as gaps were identified. URO's website and social media pages also served an important awareness-raising function, showcasing student research experiences and achievements, while the FMHS Undergraduate Research Society was an important link to the student community. As a member of the Annual Academic Day (AAD) committee, URO's head ensures that undergraduate student research is well represented at this showcase of FMHS research.
Methods
In the evaluation logic model, outputs are the direct products of a programme's activities, usually measured in terms of volume of work accomplished.'42 Having described URO's inputs and activities, step 3 in the process evaluation is to develop a list of process evaluation questions, guided by evaluation components (benchmarks) and focusing on outputs. Step 4 is to identify the methods that will be used to answer these questions (i.e. the data sources and analysis). URO's context and resources have already been described (step 5); the final process evaluation plan (step 6) is presented in Table 3.
Table 3 shows the data sources that were drawn on to address the process evaluation questions and the time points of data collection. In this descriptive evaluation study, a retrospective document review was conducted during 2020. Where indicated in the last column, a narrative description has been presented under 'inputs and activities' above in relation to some of the proposed questions. Descriptive statistics were used to analyse the remaining outputs (volume of work). As no human participant data were collected, ethics approval was not required.
Results
In this section, results from the analysis of the outputs of URO's activities are presented.
Enabling environment
A narrative description of the first three evaluation components (faculty commitment, administrative support and strategic plans) in Table 3 has been provided in 'inputs and activities' above.
Research oversight (ethics review)
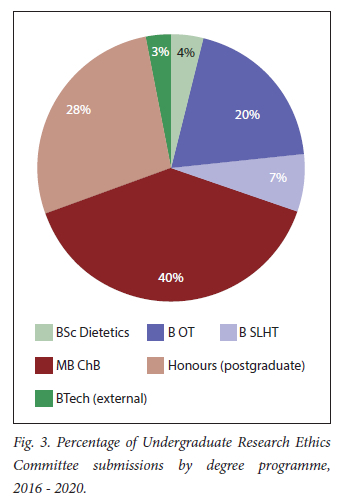
The establishment of UREC has been described above. Since its first review cycle in October 2015, UREC has reviewed 243 undergraduate and Honours ethics applications: 2016 (includes October 2015 applications): 44; 2017: 55; 2018: 39; 2019: 53; and 2020: 52. Fig. 3 shows the percentage of UREC applications received per degree programme. The majority came from MB ChB (40%), Honours (28%) and occupational therapy (20%) students. Physiotherapy students conduct systematic reviews (no ethics review); dietetics students usually participate in a larger departmental research project with a single ethics application.
Apart from June (vacation), there are two UREC submission deadlines per month from January to October; November deadlines were added in 2020. The largest number of applications are received towards the beginning (13%), middle (15%) and end (16%) of each year.
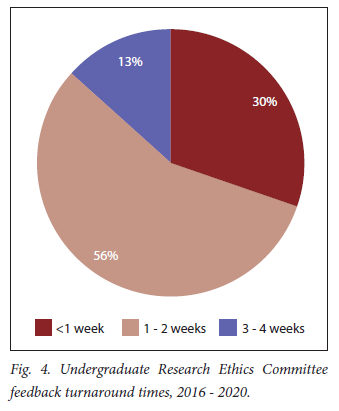
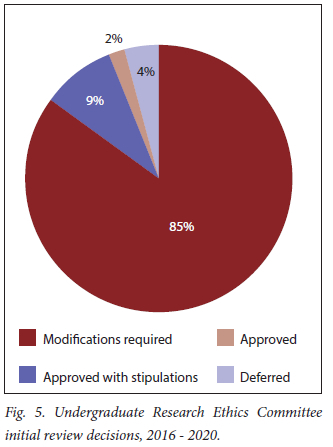
As shown in Figs 4 and 5, most review decisions were communicated to applicants within 2 weeks of submission (86%); the most frequent review decision was 'modifications required' (85%).
Funding
The creation of the Undergraduate Research Fund has been described above. Two calls for the Undergraduate Research Project Fund are published annually; 87 applications have been funded, for a total amount of ZAR316 280 between 2015 and 2020. The breakdown of awards by department/division is shown in Fig. 6. The majority of awards were made to occupational therapy students (44%), followed by MB ChB (32%) and dietetics (16%) students.
Training and resources
URO's research capacity-building activities from 2015 to 2020 are summarised in Table 4. The number of consultations (n=383) and workshops (n=54) have more than doubled since URO's inception, remaining relatively consistent during the 2020 COVID-19 lockdown when URO's services were offered virtually. Online resources (n=37) have continued to be added to the URO website in response to needs identified during consultations/workshops.
From 2015 to 2020, 259 undergraduate research projects were completed: 180 in groups (health sciences) and 79 individually (MB ChB) (see Fig. 7). Health sciences research projects have remained relatively consistent; research has been a structured part of their fourth-year programmes for many years. MB ChB research projects have increased slightly. However, the average number of MB ChB elective research projects has more than doubled since 2015, from a total of 25 and annual average of 5 projects between 2010 and 2014 to a total of 79 and average of 13 projects annually from 2015 to 2020.
Awareness, opportunity, and recognition
Undergraduate presentations at the FMHS AAD, a yearly showcase for FMHS research, doubled from 2015 to 2019 (n=122, Fig. 8). In 2020, AAD was held virtually and only poster presentations were accepted from staff/students. The majority of AAD presentations across the 6 years were by MB ChB students (48%). In 2020, SU was invited to participate in the International Conference of Undergraduate Research, where 16 FMHS undergraduate researchers presented. At least 34 publications have resulted from undergraduate research since URO was established. Students' research achievements (presentations, publications) are showcased on URO's website and social media pages. This celebrates and incentivises student research and provides a useful resource to encourage and stimulate further student research.
Between 2016 and 2019, 30 Undergraduate Conference Presentation Fund awards (total ZAR224 706) have been made (see Fig. 9). Most awards were made to MB ChB students (70%) followed by B Speech-Language and Hearing Therapy students (20%). Due to COVID-19 lockdowns, no conference presentation applications were accepted in 2020.
Seventeen Undergraduate Publication Incentive Fund awards (total ZAR165 000) were made between 2015 and 2020 (Fig. 10). Most awards were made to MB ChB (59%) and physiotherapy students (35%).
Discussion
This process evaluation has demonstrated how URO's inputs and activities incorporate several elements common to both RCD mechanisms and interventions recommended by COEUR to provide integrated support for undergraduate research in the FMHS. As outputs are the direct products of activities, assessing these has provided a measure of how well URO's core functions have been operationalised. Based on this process evaluation, this discussion highlights critical elements for success in the context of the RCD and undergraduate research literature, particularly the best practices identified by COEUR[41] - i.e. what worked, and why. We then identify gaps to be addressed going forward.
Although RCD is often conceptualised as a means to an end (i.e. high-quality research influencing policy/practice), Cooke[50] asserts that RCD evaluation should 'capture changes in both the "ends" but also the "means": it should measure the ultimate goals but also measure the steps and mechanisms to achieve them'. In undergraduate research, an institution's research enterprise can be harnessed to support student learning,[43] such that RCD may impact both process and outcome in support of curricular/ extracurricular research activities. Cooke et al[32] identified which circumstances best allow RCD interventions to achieve success, that is, the social change that RCD triggers across multiple contexts. These mechanisms, classified as either symbolic or functional, provide a useful framework for discussing what worked in operationalising URO's objectives and producing its outputs.
URO, as an RCD intervention, holds what Cooke et al.[32] refer to as symbolic value. As such, URO serves several important functions, including signalling the importance of undergraduate research through various aspects, as discussed above, indicating management's commitment to fostering an undergraduate research culture in the FMHS. As a central office providing administrative support for undergraduate research, URO also aligns with COEUR best practices.[41] In recognising and showcasing undergraduate student researchers' achievements, another COEUR best practice, URO also has a twofold symbolic function: an observable endorsement of the value of undergraduate research, and a means of making students visible as research-active individuals, thereby fostering a sense of belonging in the broader research culture.[51]-
The symbolic value of staff/students being able to perceive the observable difference made by URO's activities is linked to the importance of RCD interventions securing the engagement/ commitment of stakeholders and beneficiaries.[32]
This was a critical component in URO's early years, when efforts were focused on needs assessment and relationship-building to secure buy-in to proposed objectives and activities. This was particularly important in environments with established teaching and research support, where the perceived form of support required differed from the form it ultimately took (i.e. URO). It was essential to determine how URO could support existing programmes, in addition to filling gaps where such programmes did not exist. We believe that as URO worked to develop resources and training, raise awareness about research opportunities, facilitate ethics review, mobilise funding, and showcase undergraduate research, the value of the office became evident over time. This, in turn, secured the ongoing engagement of staff/students and also fortuitously implemented several COEUR best practices.[41]
A third way in which RCD interventions may be effective is by acting as a catalyst for releasing potential research energies from within individuals and organisations.[32] This aligns with Trostle's assertion that 'to support research implies funding studies, but to support research capacity implies funding the multiple prerequisites to performing research.'[52] By creating comprehensive resources and providing training in research, URO served as a catalyst for releasing research energies in compulsory research programmes and to spark research potential in programmes where research was optional. More significantly, URO created enabling conditions for conducting research, through the establishment of UREC to streamline ethics review, and the Undergraduate Research Fund to fund undergraduate research. Unnecessarily onerous ethics approval processes[24,25] and lack of funding[18,26] are significant obstacles to undergraduate research. Several actions, outlined above, ensured that streamlined undergraduate research ethics review was efficient and sustainable. URO also added resources and training in health research ethics, such that ethics review can function as a learning experience for undergraduates.[53,54]
While URO has achieved many of the COEUR best practices, others require more focus going forward. Particularly, undergraduate research requires significant time investment from supervisors, but incentivising supervisory support and protecting faculty time for research supervision[41] have not received adequate attention. The value of building a community of student scholars and champions for undergraduate research[41] was realised partly through the Tygerberg Undergraduate Research Society. However, it has faced challenges in continuity and sustainability, and URO can contribute here. Several FMHS environments offer Honours degree programmes (a postgraduate degree that follows completion of a bachelor's degree, i.e. fourth year), providing structured teaching and supervision in research. However, we have found that Honours students, as novice researchers, often fall through the gaps in terms of tailor-made resources and training. To address this, we are exploring extending URO's capacity-development and funding services to Honours students, who typically are at the same level in terms of research experience as fourth-year health sciences and medical students.
Several undergraduate programmes are currently undergoing curriculum renewal, including the MB ChB programme, where research will become compulsory. This has created an opportunity to review and align resources across different programmes, including sharing best practices and, where possible, teaching resources, in undergraduate research. This streamlining may in turn catalyse an increase in high-quality research outputs from undergraduate research. It will require URO to continue to be adaptive to student and programmatic needs, as well as the changing higher education landscape, particularly the move towards hybrid learning accelerated by the COVID-19 pandemic. In response to resulting restrictions, URO created additional guidance documents and new virtual support mechanisms for undergraduate student researchers. In addition, discussions around intercalated degrees for senior medical students would necessitate research capacity to be in place early on. It is hoped that the lessons learned in this office will serve as a useful guide for our newly established Registrar Research Support Office in the RDSD, as well as for similar structures supporting undergraduate research in SA and beyond.
Conclusion
The results of this process evaluation demonstrate the potential impact on undergraduate research of a formal support entity in a FMHS. Using RCD and COEUR benchmarks we have highlighted how creating an enabling environment, training and resources, and awareness, opportunity and recognition, can facilitate undergraduate research capacity development, and recommend this as a model to other institutions wanting to support and grow undergraduate research. We emphasise the importance of committed leadership and staff, relationship building and buy-in, and targeting ethics review and funding mechanisms.
Declaration. None.
Acknowledgements. The authors would like to acknowledge the many staff and students at the Faculty of Medicine and Health Sciences who have been pivotal to the success of this Undergraduate Research Office. We also thank Mrs Viv O'Neill for editing and proofreading this manuscript.
Author contributions. DLM: Conducted process evaluation, co-conceptualised and drafted manuscript, produced results, figures, and tables. NCGvP: Contributed to process evaluation benchmarks, co-conceptualised manuscript, wrote pieces of manuscript, reviewed and edited manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Lansang MA, Dennis R. Building capacity in health research in the developing world. Bull World Health Org 2004;82(10):764-770. [ Links ]
2. Whitworth JA, Kokwaro G, Kinyanjui S, et al Strengthening capacity for health research in Africa. Lancet 2008;372(9649):1590-1593. https://doiorg/10.1016/S0140-6736(08)61660-8 [ Links ]
3. IJsselmuiden C, Marais DL, Becerra-Posada F, Ghannem H. Africa's neglected area of human resources for health research - the way forward. S Afr Med J 2012;102(4):228-233. http://www.samj.org.za/index.php/samj/article/view/5377/4011 (accessed 18 November 2022). [ Links ]
4. Lalloo UG, Bobat RA, Pillay S, Wassenaar D. A strategy for developing future academic leaders for South Africa in a resource-constrained environment. Acad Med 2014;89(Suppl 8):S55-S59. https://doi.org/10.1097/acm.0000000000000354 [ Links ]
5. Singh RJ. Challenges and successes of research capacity building at a rural South African university. S Afr J High Educ 2015;29(3):183-200. https://hdl.handle.net/10520/EJC176228 (accessed 18 November 2022). [ Links ]
6. Katz AA, Futter M, Mayosi BM. The intercalated BSc (Med) Honours/MB ChB and integrated MB ChB/PhD tracks at the University of Cape Town: Models for a national medical student research training programme. S Afr Med J 2014;104(2):111-113. https://doi.org/10.7196/samj.7639 [ Links ]
7. Rohwer A, Willems B, Young T. Taking stock of evidence-based healthcare in the undergraduate medical curriculum at Stellenbosch University: Combining a review of curriculum documents and input from recent graduates. Afr J Health Professions Educ 2015;7(1):98-104. https://doi.org/10.7196/AJHPE.501 [ Links ]
8. Schoonees A, Rohwer A, Young T. Evaluating evidence-based health care teaching and learning in the undergraduate human nutrition; occupational therapy; physiotherapy; and speech, language and hearing therapy programs at a sub-Saharan African academic institution. PLoS One 2017;12(2):1-18. https://doi.org/10.1371/journal.pone.0172199 [ Links ]
9. Young T, Rohwer A, Van Schalkwyk S, Volmink J, Clarke M. Patience, persistence and pragmatism: Experiences and lessons learnt from the implementation of clinically integrated teaching and learning of evidence-based health care. A qualitative study. PLoS One 2015;10(6):1-19. https://doi.org/10.1371/journal.pone.0131121 [ Links ]
10. Laidlaw A, Aiton J, Struthers J, Guild S. Developing research skills in medical students: AMEE Guide No. 69. Med Teach 2012;34(9):754-771. https://doi.org/10.3109/0142159x.2012.704438 [ Links ]
11. Maggio LA, Tannery NH, Chen HC, Ten Cate O, O'Brien B. Evidence-based medicine training in undergraduate medical education. Acad Med 2013 Jul;88(7):1022-8. http://journals.lww.com/00001888-201307000-00036 (accessed 24 March 2021). [ Links ]
12. Zee M, de Boer M, Jaarsma ADC. Acquiring evidence-based medicine and research skills in the undergraduate medical curriculum: Three different didactical formats compared. Perspect Med Educ 2014;3(5):357-370. https://link.springer.com/article/10.1007/s40037-014-0143-y (accessed 24 March 2021). [ Links ]
13. Amgad M, Tsui MMK, Liptrott SJ, Shash E. Medical student research: An integrated mixed-methods systematic review and meta-analysis. PLoS One 2015;10(6):1-31. https://doi.org/10.1371/journal.pone.0127470 [ Links ]
14. Young T, Rohwer A, Volmink J, Clarke M. What are the effects of teaching evidence-based health care (EBHC)? Overview of systematic reviews. PLoS One 2014;9(1):e86706. https://doi.org/10.1371/journal.pone.0086706 [ Links ]
15. Earley MA. A synthesis of the literature on research methods education. Teach High Educ 2014;19(3):242-253. https://doi.org/10.1080/13562517.2013.860105 [ Links ]
16. Marais DL, Kotlowitz J, Willems B, Barsdorf NW, Van Schalkwyk S. Perceived enablers and constraints of motivation to conduct undergraduate research in a Faculty of Medicine and Health Sciences: What role does choice play? PLoS One 2019;14(3):1-23. https://doi.org/10.1371/journal.pone.0212873 [ Links ]
17. Riley SC, Morton J, Ray DC, et al. An integrated model for developing research skills in an undergraduate medical curriculum: appraisal of an approach using student selected components. Perspect Med Educ 2013;2:230-247. https://doi.org/10.1007/s40037-013-0079-7 [ Links ]
18. Pugsley L, Dornan T. Using a sledgehammer to crack a nut: Clinical ethics review and medical education research projects. Med Educ 2007;41(8):726-728. https://doi.org/10.1111/j.1365-2923.2007.02805.x [ Links ]
19. Robinson L, Drewery S, Ellershaw J, Smith J, Whittle S, Murdoch-Eaton D. Research governance: Impeding both research and teaching? A survey of impact on undergraduate research opportunities. Med Educ 2007;41(8):729-736. https://doi.org/10.1111/j.1365-2923.2007.02776.x [ Links ]
20. Funston G, Piper RJ, Connell C, Foden P, Young AMH, O'Neill P. Medical student perceptions of research and research-orientated careers: An international questionnaire study. Med Teach. 2016;38(10):1041-1048. https://doi.org/10.3109/0142159x.2016.1150981 [ Links ]
21. Zier K, Stagnaro-Green A. A multifaceted program to encourage medical students' research. Acad Med. 2001;76(7):743-747. https://doi.org/10.1097/00001888-200107000-00021 [ Links ]
22. Mahomed S, Ross A, Van Wyk JM. Training and assessing undergraduate medical students' research: Learning, engagement and experiences of students and staff. Afr J Prim Heal Care Fam Med 2021;13(1):a2559. https://doi.org/10.4102/%0Aphcfm.v13i1.2559 [ Links ]
23. McLean AL, Saunders C, Velu PP, Iredale J, Hor K, Russell CD. Twelve tips for teachers to encourage student engagement in academic medicine. Med Teach 2013;35(7):549-554. https://doi.org/10.3109/0142159x.2013.775412 [ Links ]
24. Burger M, Louw QA. Integrating evidence-based principles into the undergraduate physiotherapy research methodology curriculum: Reflections on a new approach. Afr J Heal Professions Educ 2014;6(2):198. http://www.ajhpe.org.za/index.php/ajhpe/article/view/516 (accessed 26 April 2016). [ Links ]
25. Nel D, Burman RJ, Hoffman R, Randera-Rees S. The attitudes of medical students to research. S Afr Med J 2014;104(1):32-36. https://doi.org/10.7196/samj.7058 [ Links ]
26. Knight SE, Van Wyk JM, Mahomed S. Teaching research: a programme to develop research capacity in undergraduate medical students at the University of KwaZulu-Natal, South Africa. BMC Med Educ 2016;16(61): PMC4754994. https://doi.org/10.1186/s12909-016-0567-7 [ Links ]
27. Murdoch-Eaton D, Drewery S, Elton S, et al. What do medical students understand by research and research skills? Identifying research opportunities within undergraduate projects. Med Teach 2010;32(3):e152-160. https://doi.org/10.3109/01421591003657493 [ Links ]
28. Bosch A, Taylor J. A proposed frameworkof institutional research development phases. J High Educ Policy Manag 2011;33(5):443-457. https://doi.oig/10.1080/1360080X.2011.585742 [ Links ]
29. Stackhouse J, Day R. Global and regional practices in university research management: Emerging trends. Int J Technol Manag Sustain Dev 2005;4(3):189-205. https://doi.org/10.1386/ijtm.4.3.189/1 [ Links ]
30. Hong Nguyen TL, Meek VL. Key considerations in organizing and structuring university research. The Journal of Research Administration 2015; 46(10):41-62. [ Links ]
31. Cooke J, Booth A, Nancarrow S, Wilkinson A, Askew D. Re : Cap - A Scoping Review to Identify the Evidence-Base for Research Capacity Development in Health and Social Care. Sheffield, University of Sheffield, 2006. [ Links ]
32. Cooke J, Gardois P, Booth A. Uncovering the mechanisms of research capacity development in health and social care: A realist synthesis. Heal Res Policy Syst 2018;16(93):1-22. https://doi.org/10.1186/s12961-018-0363-4 [ Links ]
33. Kirkland J, Ajai-Ajagbe P. Research management in African universities: from awareness raising to developing structures. London: Association of Commonwealth Universities, 2013. [ Links ]
34. Mashaah MT, Hakim J, Naik Y, Gomo E. Strengthening research governance for sustainable research: Experiences from three Zimbabwean universities. Acad Med 2014;89:69-72. https://doi.org/10.1097%2FACM.0000000000000348 [ Links ]
35. Kirkland J. Research management: A global profession? Perspectives 2009;13(2):33-36. https://doi.org/10.1080/13603100902805383 [ Links ]
36. Lues L, Lategan L. Research development at a South African university of technology: A case study. South African J High Educ 2006;20(3):108-121. https://doi.org/10.4314/sajhe.v20i3.25589 [ Links ]
37. Johnson B, June CW, Drennan R. Research Management: A Handbook for Southern African Research Management Offices. Pretoria: SARIMA, 2018. [ Links ]
38. Matus J, Walker A, Mickan S. Research capacity building frameworks for allied health professionals - a systematic review. BMC Health Serv Res 2018;18(716):1-11. https://doi.org/10.1186/s12913-018-3518-7 [ Links ]
39. Snyder DC, Brouwer RN, Ennis CL, et al. Retooling institutional support infrastructure for clinical research. Contemp Clin Trials 2016;48:139-145. https://doi.org/10.1016/j.cct.2016.04.010 [ Links ]
40. Dison A. Research capacity development of individuals at three South African university research centres. PhD thesis. Cape Town: University of the Western Cape, 2015. [ Links ]
41. Rowlett RS, Blockus L, Larson S. Characteristics of excellence in undergraduate research (COEUR). In: Hensel N, editor. Characteristics of Excellence in Undergraduate Research (COEUR). Washington: Council on Undergraduate Research, 2012:2-19. https://www.cur.org/assets/1/23/COEUR_final.pdf (accessed 22 December 2020). [ Links ]
42. United Way of America. Measuring program outcomes: A practical approach. Evaluation Reflection 47. 1996. https://digitalcommons.unomaha.edu/slceeval/47 (accessed 10 December 2021). [ Links ]
43. Cooksy LJ, Gill P, Kelly PA. The program logic model as an integrative framework for a multimethod evaluation. Eval Program Plann 2001;24(2):119-128. https://doi.org/10.1016/S0149-7189(01)00003-9 [ Links ]
44. Savaya R, Waysman M. The logic model: A tool for incorporating theory in development and evaluation of programs. Adm Soc Work 2005;29(2):85-103. https://doi.org/10.1300/J147v29n02_06 [ Links ]
45. TSNE MissionWorks. Process evaluation vs. outcome evaluation. In: Evaluation Best Practices Executive Directors Guide. Boston: TSNE Mission Works; 2018:10-13. https://www.tsne.org/blog/process-evaluation-vs-outcome-evaluation (accessed 29 October 2021). [ Links ]
46. Stuart K, Maynard L, Rouncefield C. Types of evaluation. In: Rouncefield C, Stuart, K, Maynard, L, editors. Evaluation Practice for Projects with Young People: A Guide to Creative Research. London: SAGE Publications,2017:59-78. [ Links ]
47. Linnan L, Steckler A. Process evaluation for public health interventions and research: An overview. In: Steckler A, Linnan L, editors. Process Evaluation for Public Health Interventions and Research. San Francisco: Wiley/Jossey-Bass, 2002:1-23. [ Links ]
48. Saunders RP, Evans MH, Joshi P. Developing a process-evaluation plan for assessing health promotion program implementation: Ahow-to guide. Health Promot Pract 2005;6(2):134-147. https://doi.org/10.1177/1524839904273387 [ Links ]
49. Bovijn J, Kajee N, Esterhuizen TM, Van Schalkwyk SC. Research involvement among undergraduate health sciences students: A cross-sectional study. BMC Med Educ 2017;17(1):1-10. https://doi.org/10.1186/s12909-017-1025-x [ Links ]
50. Cooke J. A framework to evaluate research capacity building in health care. BMC Fam Pract 2005;6(44):1-11. https://doi.org/10.1186/1471-2296-6-44 [ Links ]
51. Hansen J, Calvert B. Developing a research culture in the undergraduate curriculum. Act Learn High Educ 2007;8(2):105-116. https://doi.org/10.1177%2F1469787407077984 [ Links ]
52. Trostle J. Research capacity building in international health: Definitions, evaluations and strategies for success. Soc Sci Med 1992;35(11):1321-1324. https://doi.org/10.1016/0277-9536(92)90035-o [ Links ]
53. Bowater L, Wilkinson M. Twelve tips to teaching (legal and ethical aspects of) research ethics/responsible conduct of research. Med Teach 2012;34(2):108-115. https://doi.org/10.3109/0142159x.2011.588738 [ Links ]
54. Edwards SJL. Student projects in medicine: A lesson in science and ethics. Account Res 2009;16(6):285-306. https://doi.org/10.1080/08989620903328451 [ Links ]
 Correspondence:
Correspondence:
D L Marais
debbiem@sun.ac.za
Accepted 4 May 2022.














