Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
African Journal of Health Professions Education
versión On-line ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.14 no.4 Pretoria dic. 2022
http://dx.doi.org/10.7196/AJHPE.2022.v14i4.1568
RESEARCH
High-fidelity simulation: A practice model for nurse educators at a South African private higher education institution
E PowellI; B ScroobyII; A van GraanI
IPhD; School of Nursing, Faculty of Health Sciences, North-West University, Potchefstroom campus, South Africa
IIPhD, MCur, BCur ; School of Nursing, Faculty of Health Sciences, North-West University, Potchefstroom campus, South Africa
ABSTRACT
BACKGROUND. The clinical skills development of student nurses is one of many challenges facing nursing education owing to a lack of available clinical placements and learning opportunities. Simulation training as an optional teaching-learning method creates an environment where clinical skills are developed and students are prepared for the nursing profession. The successful implementation of high-fidelity simulation (HFS) strategies as part of the nursing curricula requires nurse educators to have knowledge and skills. At the South African private higher education institution (SAPHEI) where the research for this study was done, it became evident that nurse educators do not have the required knowledge, skills or support to implement HFS. The absence of evidence in the literature of a practice model for a SAPHEI to facilitate the implementation of HFS reveals a gap in the practice base of nursing education.
OBJECTIVE. To develop a practice model for nurse educators at a SAPHEI to facilitate the implementation of HFS.
METHODS. The researcher used a theory-generative research design. The study was conducted in two phases, with two steps in each phase, to address four objectives in all.
RESULTS. Phase 1 identified and described the main and related concepts. A resulting conceptual framework was used for the development of the practice model. Phase 2 addressed the relational meaning of the main and related concepts, as well as the construction of the practice model through theory synthesis.
CONCLUSION. The main aim of this research study was to develop a practice model for nurse educators at a SAPHEI to facilitate the implementation of HFS as part of the clinical skills development of student nurses. The practice model offers a schematic outline that represents HFS as a teaching-learning method. The importance of the outline lies therein that it specifies the context and situations in which the model is useful.
The main objective of nursing education is to guide student nurses towards clinical competence.[1,2] Student nurses need clinical exposure to gain experience and confidence to perform clinical tasks. In the private sector, clinical exposure has proven to be a challenge due to insufficient clinical placements and learning opportunities. A contributing factor is a decrease in patient bed occupation rates due to the increased cost of healthcare. The challenge experienced with clinical exposure and limited learning opportunities contributes to student nurses' lack of confidence when performing clinical tasks, consequently creating an 'unsafe' environment for them and for the patient.[1,2]
Nurse educators have explored different ways to help student nurses become competent practitioners. Simulation training (an active, collaborative learning method) was added to the traditional models of learning in an attempt to enhance cognitive learning and improve clinical skills towards competence[3] as learning shifts away from passive, receptive and content driven, to active and dynamic and requires reflexivity.[4] Clinical simulation training has been proven to improve the development of clinical competence and confidence among student nurses,[1] who can practise clinical skills in a safe environment.[5] High-fidelity simulation (HFS) training (the use of high-technology, life-like programmed manikins that breathe, talk, blink and have heart and bowel sounds) allows student nurses to learn through graded experience rather than 'practising on' potentially distressed and vulnerable patients in reallife consultations.['6]
However, the successful implementation of HFS strategies as part of the nursing curricula requires nurse educators to have knowledge and skills. [7] At the SAPHEI that participated in the research study, simulation training is used in addition to clinical exposure to enhance student nurses' clinical competence and confidence. The implementation of HFS at the SAPHEI has been a challenge owing to nurse educators' lack of the required knowledge, skills or support.[8] Nurse educators have either not been exposed to or have limited experience with HFS.[9] Therefore, there is a need for a practice model for nurse educators at the SAPHEI. Taking into consideration the wide range of beliefs, cultural differences, limited resources and different levels of awareness among nurse educators at the SAPHEI,[9] the researcher, with the assistance of a librarian, searched for a practice model to facilitate the implementation of HFS at a SAPHEI. The absence of literature evidence of an existing practice model reveals a gap in the practice base of nursing education specific to the SAPHEI. To fill the gap, the main objective of this research was to develop a practice model for nurse educators at a SAPHEI to facilitate the implementation of HFS as part of the clinical skills development of student nurses. The practice model offers a schematic outline that represents HFS as a teaching-learning method at a SAPHEI, which sets it apart from existing HFS models, as it specifies the context and situations for which the model is useful.
This article describes the development of the practice model for nurse educators at the participating SAPHEI.
Methods
A theory-generative research design was adopted,[10,11] which included two distinct data collection phases.
Phase 1 identified and described the main and related concepts, culminating in a conceptual framework[10] that was later used for the development of the practice model. Phase 2 addressed the relational meaning of the main and related concepts, as well as the construction of the practice model through theory synthesis (Fig. 1).
Data collection
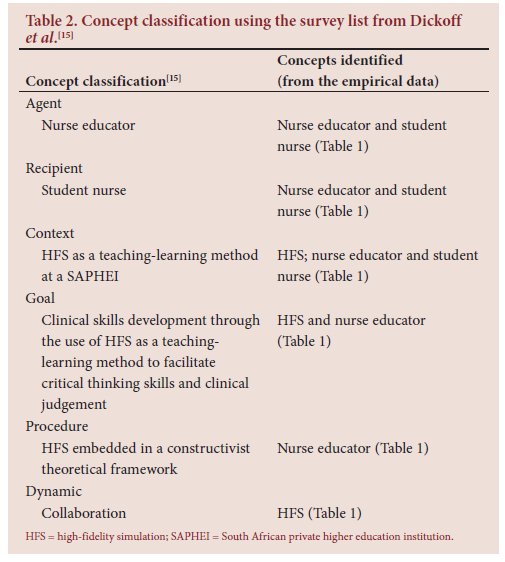
Mouton and Marais]12] explain that concepts can be structured into certain types of statements, which should then be arranged according to regulative interests or orientations to form a conceptual framework that can be presented as a model. The conceptual framework was developed from concepts identified (Table 1) from empirical data (phase 1), concept classification and an in-depth literature review. The empirical data were gathered as part of a mixed-method research study where the following objectives were investigated and described: (i) nurse educators' current use and experiences with HFS as part of the nursing programmes at a SAPHEI;[8] and (ii) nurse educators' views of HFS as an educational approach in nursing programmes.[9] The steps followed to develop the conceptual framework were: (i) selecting and defining concepts from empirical data; (ii) developing statements relating the concepts; (iii) expressing the statements hierarchically; and (iv) developing a conceptual map that expresses the framework.[13,14] For the development of a conceptual framework, the population included all the selected main and related concepts (Table 2) that had been identified from the empirical data obtained during phase 1, step 1, and purposively sampled in the form of literature searches. All available national and international sources of data were used as population during the construction of the relational meaning of main and related concepts. The sample consisted of conclusion statements. During the model construction phase (phase 2, step 2), the conclusion statements from the results obtained from the construction of relational meaning of main and related concepts (phase 2, step 1) were used as the sample.
Data analysis
The researcher used all the data gathered from phase 1, as well as an in-depth literature control, to develop and describe the conceptual framework. This framework was developed through statement synthesis by identifying and defining concepts with proposed relationships. After the completion of the statement synthesis, a practice model was developed through theory synthesis. Theory synthesis refers to the development and organisation of empirical data to develop a model describing the relationships that may exist among concepts.[15] The description and evaluation of the practice model (Table 3, levels 3 and 4) are not discussed in this article. Table 3 indicates the application of the levels of practice theory by Dickoff et al.[15]
Rigour
Inductive and deductive strategies are the main reasoning strategies used during theory development and construction.'141 In an inductive argument, supportive evidence can lead to highly probable conclusions, thus lending gradual supporting statements to the conclusions.'121 Deduction occurs when a specific conclusion is inferred from general premises or principles. It proceeds from the general to the specific. True premises necessarily lead to true conclusions;[12] therefore, the truth of the conclusion is already either implicitly or explicitly contained in the truth of the premises. Induction and deduction strategies were used sequentially to arrive at an adequate theoretical formulation.[14] The researcher used these two strategies interdependently to help understand the concepts identified during the research study.
Ethical approval
Ethical approval for the study was obtained from the Research Health Science Ethics Committee of North-West University (ref. no. NWU-00011- 18-A1) and the SAPHEI. During phases 1 and 2 of the research, participants gave voluntary written informed consent to participate in the study and they could withdraw at any time. All collected data were transcribed and saved on a password-protected external hard drive. Confidentiality was maintained by coding of data to ensure anonymity.
Results
The method used to identify the key concepts and sub-concepts was justified from the literature,[12,14] primarily the article by Hsieh and Shannon.[16] The key concepts and sub-concepts emerged from the empirical research performed during phase 1 of the study (Table 1). An in-depth review was done to ensure consistency and congruency while identifying concepts. In the finalised list of key concepts and subconcepts that had been identified, the focus was on the qualitative features of the concepts - not the number of main and related concepts. In this way the consistency of the central idea that linked the identified concepts was ensured (Table 1).[13]
The researcher relied on the work of Dickoff et al.[15]for the classification of the concepts identified in Table 3. Theory is born in practice, refined in research and applied to practice.[15] The concepts were therefore explained within the context of the applicable practice setting to achieve the aim of this research study. The following three components formed an essential part of the practice model: (i) specific goal content as the aim of the activity; (ii) prescriptions for an activity to realise the goal content; and (iii) a survey list to classify the activities or elements involved in achieving the goal content.[15] The survey list used the following 6 modified questions their features (Table 2):[15] (i) agent: who or what performs the activity?; (ii) recipient: who or what benefits from the activity?; (iii) context: in what context is the activity performed?; (iv) target/goal (terminus): what is the targeted outcome of the activity?; (v) procedure: what is the procedure, protocol or technique of the activity?; and (vi) dynamics: what is the energy source for the activity?
Table 2 illustrates the use of deductive logic from concept identification to concept classification using the modified survey list of Dickoff et al[15]
Table 4 summarises the statements concluded from the conceptual framework that led to the practice model (Fig. 2).
Relational statements are central to model development, as they state an association between two or more concepts during the process of constructing a scientific body of knowledge. [14] The construction process of the relational statements started with identified, examined and analysed major concepts. Relational linkages between these concepts were determined through a process of deductive reasoning.[14] The relational statements were assessed against empirical support,[14] and were developed from the empirical conclusion statements by means of deductive reasoning. This process was aimed at the interpretation of associations between the major concepts, as follows:
• The nurse educator, as a facilitator of clinical skills development in student nurses, should possess certain characteristics and skills: knowledgeability, clinical competence, effective facilitation, being organised, sharing information/interacting and collaborating, compassion and respect, patience and co-operation, supportiveness and an ability to instil confidence, dynamism and enthusiasm, fairness and being non-judgemental, having a sense of humour, admitting mistakes and limitations, and flexibility. They should acknowledge the uniqueness of each student nurse to ensure an effective teaching-learning environment that will facilitate the clinical competence of student nurses by the integration of theory into practice and promoting clinical judgement.
• The student nurse as an adult learner should demonstrate emotional intelligence, self-directed learning, experience, learning readiness and learning orientation, which leads to being task orientated and problem directed. They should approach learning intentionally, be self-motivated, be active participants of their own learning and acquire meaning and understanding through reflection and continuous collaboration with the nurse educator and peer group to gain clinical competency through the use of HFS as a teaching-learning method.
• The nurse educator should prepare student nurses for clinical practice as part of the student's curriculum by creating a safe and conducive environment for clinical skills development through the use of HFS as a teaching-learning method and continuous collaboration with the student nurse towards clinical competence.
• HFS as a teaching-learning method and collaboration between the nurse educator and student nurse should support the development of clinical skills towards clinical competence.
• The nurse educator and student nurse should strive towards the development of clinical skills by implementing HFS as a teaching-learning method. HFS, embedded in a constructivist theoretical framework, enhances clinical skills development towards clinical competence if and when applied by a skilled facilitator. This statement is only true if the facilitator uses the correct equipment and resources and when there is proper planning using teaching-learning methods that lead to theory-practice integration and the development of clinical skills, critical thinking and clinical judgement.
• Collaboration should encircle the model to show that it is a continuous and interactive process between the nurse educator and student nurse to ensure safe and comprehensive patient care by applying HFS as a teaching-learning method to develop clinical skills towards clinical competence.
Discussion
In this research study the nurse educator was a qualified registered nurse with an additional qualification in nursing education that supports clinical and theoretical teaching-learning methods. Continuous, lifelong learning is important for nurse educators to improve their knowledge and understanding, not exclusively focused on their clinical discipline and theoretical modules but including facilitation skills and teaching-learning methods.
Student nurses referred to in this study were pre-registered diploma students studying towards a qualification in the nursing profession. They are from a range of backgrounds, with differences in education, language, religion, socioeconomic circumstances, culture, ethnicity, value systems and many more. They are adult learners entering a new demanding profession.
The context of this research study is HFS as a teaching-learning method at a SAPHEI. The goal is to expose student nurses to clinical skills through the use of HFS as a teaching-learning method to facilitate critical thinking and clinical judgement.
Collaboration is a dynamic process. The nurse educator and student nurse work together to reach a common goal (clinical competence). The nurse educator interacts with the student nurse and the HFS environment to facilitate teaching-learning to enhance clinical competence. HFS allows the student nurse to use their existing knowledge during a simulated training experience to build on their previous knowledge in developing new knowledge and experiences.
Conclusion
The main aim of this research study was to develop a practice model for nurse educators at a SAPHEI to facilitate the implementation of HFS in clinical skills development of student nurses. The purpose of the development of this practice model was to provide a schematic outline that represents HFS as a teaching-learning method, which is important as it specifies the context and situations in which the model is useful. The context is a SAPHEI offering nursing education programmes for undergraduate student nurses.
The nurse educator forms the core attribute of the practice model, as they act as a facilitator for the HFS teaching-learning method through which the student nurse can, by active participation and collaboration, develop their clinical skills. The nurse educator (with their own set of characteristics) interacts with the student nurse (with their own set of characteristics) through HFS, which is embedded in a constructivist theoretical framework. The nurse educator and student nurse strive towards the development of clinical skills by implementing HFS as a teaching-learning method. Collaboration encircles the model to show that it is a continuous and interactive process.
The structure of the model gives an overall shape to all the conceptual relationships within it, illustrating the relationships within the model. There is an identifiable relationship between the individual and the setting that is portrayed as the environment of the model. All the structural elements of the model therefore have to be depicted in a way that determines the strength, direction and quality of the model, which shows the concepts and relational statements.
The credibility of the practice model can only be determined after it has been evaluated. To evaluate the practice model, it must be implemented at a SAPHEI, but due to the COVID-19 pandemic, it could not be done.
Research flowing from this study will evaluate the proposed practice model after implementation of changes if deemed necessary.
Study limitations
This study was conducted at one SAPHEI, limiting the findings to a single institution.
Declaration. The research for this study was done in partial fulfilment of the requirements for EP's PhD degree at the University ofNorth-West, Potchefstroom. It is the third of three articles published as a requirement for the completion of EP's PhD degree.
Acknowledgements. We acknowledge the financial and material support for language editing and publication fees from our affiliated university.
Author contributions. EP collected the data, conducted the data analysis and developed the HFS practice model as part of her doctoral thesis. EP also wrote this article. BS and AvG, as EP's promotor and co-promotor, respectively, reviewed and revised the article. BS finalised the article.
Funding. North-West University gave financial support in the form of a postgraduate bursary.
Conflicts of interest. None.
References
1. Agea JLD, Nicolas AM, Méndez JAG, Martinez MGA, Costa CL. Improving simulation performance through self-learning methodology in simulated environments (MAES©). Nurse Educ Today 2019;76:62-67. https://doi.org/10.1016/j.nedt.2019.01.020 [ Links ]
2. Häggström M, Bäckström B, Vestlin I, Hallin K, Segevall C, Kristiansen L. Overcoming reluctance towards high fidelity simulation - a mutual challenge for nursing students and faculty teachers. Glob J Health Sci 2017;9(7):127-137. https://doi.org/10.5539/gjhs.v9n7p127 [ Links ]
3. Nehring WM, Lashley FR. Nursing simulation: A review of the past 40 years. Simul Gaming 2016;40(4):528-552. https://doi.org/10.1177%2F1046878109332282 [ Links ]
4. Berragan L. Simulation: An effective pedagogical approach for nursing? Nurse Educ Today 2011;31:660-663. https://doi.org/10.1016/j.nedt.2011.01.019 [ Links ]
5. Harper M, Eales-Reynolds L, Markham C. Transforming simulation in clinical education: Is pre-placement hybrid learning valuable to healthcare students? J Contemp Med Educ 2013;1(1):15-24. https://doi.org/10.5455/jcme.20121129051301 [ Links ]
6. Nestel D, Bearman M. Simulated Patient Methodology: Theory, Evidence and Practice. Chichester: Wiley Blackwell, 2015. [ Links ]
7. Paige JB, Morin KH. Using Q-methodology to reveal nurse educators' perspectives about simulation design. Clin Simul Nurs 2015;11(1):11-19. https://doi.org/10.1016/j.ecns.2014.09.010 [ Links ]
8. Powell E, Scrooby B, van Graan A. Nurse educators' use and experiences with high-fidelity simulation in nursing programmes at a South African private higher education institution. Int J Afr Nurs Sci 2020;13:1-6. https://doi.org/10.1016/j.ijans.2020.100227 [ Links ]
9. Powell E, Scrooby B, van Graan A. Nurse educators' views on implementation and use of high-fidelity simulation in nursing programmes. Afr J Health Professions Educ 2020;12(4):215-219. https://doi.org/10.7196/AJHPE.2020.V12I4.1411 [ Links ]
10. Creswell JW. Educational Research: Planning, Conducting and Evaluating Quantitative and Qualitative Research. 4th ed. Edinburgh: Pearson, 2018. [ Links ]
11. Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. 2nd ed. Los Angeles: SAGE, 2011. [ Links ]
12. Mouton J, Marais HC. Basic Concepts in the Methodology of the Social Sciences. Pretoria: Human Sciences Research Council, 1996. [ Links ]
13. Chinn PL, Kramer MK. Integrated Theory and Knowledge Development in Nursing. 8th ed. St Louis: Elsevier, 2011. [ Links ]
14. Walker LO, Avant KC. Strategies for Theory Construction in Nursing. 5th ed. Essex: Pearson, 2011. [ Links ]
15. Dickoff J, James P, Wiedenbach E. Theory in a practice discipline. Part 1: Practice oriented theory. Nurs Res 1968;17(5):415-435. [ Links ]
16. Hsieh H, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15(9):1277-1288. https://doi.org/10.1177/1049732305276687 [ Links ]
 Correspondence:
Correspondence:
B Scrooby
belinda.scrooby@nwu.ac.za
Accepted 16 May 2022.














