Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
African Journal of Health Professions Education
versión On-line ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.14 no.4 Pretoria dic. 2022
http://dx.doi.org/10.7196/AJHPE.2022.v14i1639
RESEARCH
Promoting critical thinking through simulation-based healthcare training (SBHT): A scoping review
C HenricoI; N OostdamII
IPhD; Department of Emergency Medical Care, Faculty of Health Sciences, University of Johannesburg, South Africa
IIBHS; Department of Emergency Medical Care, Faculty of Health Sciences, University of Johannesburg, South Africa
ABSTRACT
BACKGROUND. Critical thinking (CT) is an essential graduate attribute for health professions (HP) students. Yet, achieving a higher level of CT in HP students through education is often difficult for educators. SBHT has proven to be an effective strategy to promote CT, but it is not clear how this educational pedagogy should be implemented to achieve higher levels of CT.
OBJECTIVE. To identify and describe the use of simulation-based healthcare training (SBHT) strategies to promote CT in HP students.
METHODS. Based on the revised methodology of Levac et al., a scoping review was conducted on studies reporting an improvement in CT through.
simulation-based healthcare education published between January 2010 and August 2021.
RESULTS. Twenty articles were included. Through thematic analysis, three main themes were identified: contact simulations, computer-based simulations, and debriefing. The focus was on how these approaches were used to promote CT. Various subthemes were also identified.
CONCLUSION. Correctly planning and implementing a simulation-based experience that relates to the relevant learning activities, combined with repeat practice and guided reflection during the debriefing stage, improves the CT skills of HP students.
Promoting critical thinking (CT) within a health professions (HP) curriculum is often a complex task for academic staff. However, despite the complexity and difficulty in achieving CT in students, CT is considered by the World Health Organization (WHO) to be a core competency or graduate attribute for professional proficiency in almost all HP qualifications.^ The South African Qualifications Authority (SAQA) states that various critical outcomes must be embedded in all qualifications, the first of which is that the graduate should be able to display critical and creative thinking as they identify and solve problems.[2] Hence, CT forms an integral part of all South African (SA) health professions (HP) curricula.
CT is a complex notion. It is a process of carefully analysing and applying knowledge and information gathered from various sources to make informed decisions.[3] It consists of three components: gathering of information; processing (or thinking) skills; and cognitive processes (reflection and contextual perspective).[4] The ability to think critically should be viewed from two perspectives when including it in a teaching strategy: (i) mental habits and (ii) cognitive skills.[5] The notion of CT has received scholarly attention over the years, with the importance of fostering CT during graduate training being well documented.[6,7] It is therefore surprising that a universally accepted teaching strategy suitable for the promotion of CT across HP curricula has not been agreed upon.[3,8,9-
Simulation-based healthcare training (SBHT) is a pedagogical method that is often professed to have the ability to enhance the CT skills of students in a safe and controlled environment.[10] SBHT could be used to bridge the gap between theoretical knowledge obtained in class and practical knowledge gained while interacting with patients during clinical placements.[8]
Although it seems evident that SBHT could facilitate the CT of HP students,[10-14] it is not clear which SBHT strategy would best suit the
promotion of CT for HP students. A similar review focusing on the promotion of CT through simulation-based healthcare training could not be traced. The aim of this scoping review is therefore to identify and describe the use of SBHT strategies to promote the CT of the HP students. These insights could provide guidance for health educators on suitable teaching strategies for facilitation of CT in HP curriculum.
Methods
This study used the methodological framework for scoping reviews as defined by Levac et al.[15,16] The first five steps of Levac's framework were followed.[16,17] The optional consultation step was excluded, as each author charted the data separately and had a consensus discussion before collating, summarising and reporting the data. The study protocol was registered on OSF (ref. no. wa48q-v1; reg. link: https://osf.io/wa48q).
It was agreed that the aim of the review was to consult existing literature to identify and describe the use of SBHT strategies to promote CT in HP students. Hence, the question identified was: 'What is known from the existing literature about promoting CT through SBHT?' (Step 1)
Identifying the relevant literature
The PRISMA-ScR (Supplementary File 1) was used to conduct a comprehensive literature review (Step 2).[18] All journal articles and grey literature, of any study design published in English between 1 January 2010 and 1 August 2021, were included in this scoping review. The following databases were consulted: Medline, CINAHL, EBSCOhost, Web of Science and Cochrane. Grey literature was searched through Google Scholar. Additionally, manual searching of the reference lists of included articles was conducted. A librarian was consulted to provide guidance on search strategies (Supplementary file 1: https://www.samedical.org/file/1940). Fig. 1 presents an overview of the selection process.
Study selection
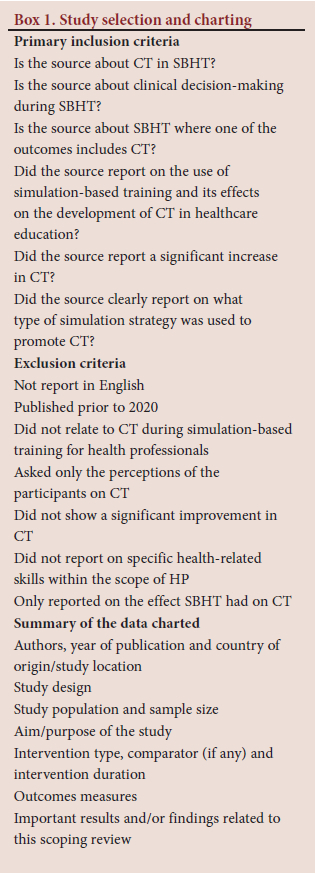
Two stages of screening were used during the review process. The titles and abstracts of the retrieved sources were read to identify relevancy of the sources. Thereafter full sources were read and assessed to determine if they met the inclusion and exclusion criteria. If there was uncertainty on a source's eligibility, consensus between the two researchers was reached. Sources were included (Step 3) if they focused on promoting CT during SBHT for HP students (Box 1).
Charting the data
An online reference management system was used to export all the search results, and to screen the remaining records and eliminate duplicates. The data were then charted in an Excel (MicroSoft Corp., USA) spreadsheet. The information that was collected and charted (Step 4) is summarised in Box 1 (detailed charted list - Supplementary File 2: https://www.samedical.org/file/1941).
Narrative thematic analysis was conducted on the charted data (Step 5). This analysis was guided by the main research question. Concepts were grouped and themes and subthemes emerged that allowed the research team to contextualise and map the outcomes.
Results
Twenty articles were included in the review: six studies were conducted in the USA, seven in Asia, and two in Australia. United Arab Emirates, Germany, Canada, Saudi Arabia and SA each produced one. A quantitative research approach was used in 15 of the included articles; only two studies used a qualitative and two a review design, while one adopted a mixed-methods design. Most of the included articles sampled students within the nursing profession (55%); 15% of the articles did not identify the HP discipline sampled; 10% of the articles sampled radiology and oral health students respectively, and a mere 5% sampled physical therapy students. The remaining 5% of articles did not specify the medical related students they sampled.
Three themes of contact simulations, computer-based simulations, and debriefing were identified in this scoping review which encapsulate the SBHT approaches used to promote CT (Table 1). Although the findings of the review are presented according to the identified themes, there are instances where these themes and subthemes were integrated to achieve the promotion of CT across sources.
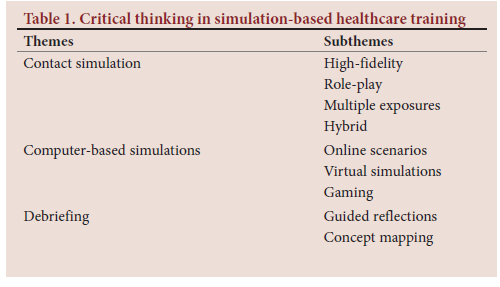
Contact simulations
Simulations conducted in a contact manner were the most dominant theme. Subthemes included high-fidelity simulations (HFS); simulations through role-play; simulations allowing multiple exposures to the clinical event; and hybrid simulations.
Most of the studies included in this review looked at promoting CT through HFS (40%). One study compared HFS with Low Fidelity Patient Manikins (LFPM) and concluded that using HFS is advantageous when looking at increasing CT skills.[19] Hagemann et al.[20] concluded that when improving the CT of students through HFS, it is crucial that the design of the simulated activity combines a practical simulation session with debriefing. Similarly, Munroe et al.[21] used a fully immersive HFS to evaluate the effect on CT in an emergency department. The fidelity of simulation-based experience must be appropriate for the knowledge or skill the simulation is designed to assess or teach. It is therefore essential that simulated scenarios go through validity and reliability testing before implementation, by means of review by experts or by peers with simulation-based experience.
Another study used HFS to foster CT in a mock critical-care setting. Study participants expressed that they preferred HFS to a learning activity that used a real person - often a student - playing the role of patient. The study recommended that all aspects of fidelity should be considered, including the appropriate clothing for the manikin, when aiming to promote CT.[22-
One study combined role-playing within HFS, paying attention to the environment of the simulation experience. Students each played three roles, including a non-medical role. Allowing students the opportunity to switch roles enables them to view the scenario from different perspectives. Ultimately HFS offer a potentially effective tool for engaging the CT skills of HP students, by giving them an opportunity to think like seasoned practitioners. Follow-up debriefings are very important. The authors also suggested that learning should be scaffolded in the lead-up to the HFS experience and students should be allowed to familiarise themselves with the simulation equipment prior to the event.[4]
Scaffolding various learning activities before the simulation-based healthcare experience was a major outcome of Louw.[23] This study used HFS and embedded various problems related to HP curriculum outcomes. These problems required CT as a problem-solving strategy. The study recommended that post-simulation reflection must be conducted.[23]
The last source included in this review combined HFS with the use of Standardised Patients (SP).[24] This study clearly indicated that SBHT provides both subjective and objective advantages over traditional teaching methods.
Role-play took on the form of virtual role-playing and realistic role-playing within a SBHT experience. Arunachalam et al.[25] evaluated virtual role-playing of a clinic setting as a model to promote CT.[25] The authors used metacognitive scaffolding to guide the students in the thinking process, to promote the CT of HP students.[25]
Another study used realistic role-play in a clinical simulation setting.[26 A role-play script based on the researcher's clinical experience as well as the content of the course, was used. The focus was to investigate the differences in students' CT skills when performing a simulation task after education was delivered by either (i) role-play or (ii) lecture. The author concluded that using simulation after role-play was a more effective teaching method.[26] Similar to Ertmer et al.,[4] Kim also stressed that students need to be exposed to various roles in realistic role-play situations, that will lead to an improvement in their CT skills.
Many of the included sources reported on the benefit of exposing students to the simulation-based healthcare (SBH) experience more than once.[4,26-29] In one source the evidence showed that simulation-based experiences that use different case scenarios each time over a period of time were best suited to enhanced CT.[29] The authors recommend that low-fidelity simulations, medium-fidelity simulations and HFS need to be integrated with repeated simulation experiences.[29] Another study demonstrated that more repetitions of a SBH scenario produced greater changes in the CT of HP students.[28] This is in line with a study that aimed to identify the effects of differing numbers of simulation exposures (one, two or three) on the CT skills of students.[27] CT scores varied according to the number of exposures students had in the course. With a single exposure, there were no statistically significant gains in CT, whereas three exposures produced significant gains in CT.[27] Further studies that focused on HFS also noted the importance of multiple exposures, stating that multiple simulation-based exposures will offer greater value to the students.[4,19,26] Literature suggests that there might be a decrease in CT over time if the simulation-based experience is not repeated.[19]
The final subtheme was hybrid simulations that use a variety of simulation strategies and modalities. One source reported that a hybrid simulation improved the CT of HP students.[30]
Computer-based simulations
Virtual or online simulations were used in 35% of the included sources. The subthemes included online scenarios, virtual scenarios and gaming.
Online scenarios are simulation-based experiences that are conducted through an online medium. One study used online role-playing SBH experience by collecting patient scenarios and converting them to digital teaching files.[31] The findings support the integration of scenario-based simulations within the curriculum to promote CT.[31] The authors concluded that the interactive scenarios should be complemented by text-based knowledge[31] through scaffolding.[23] Improved CT for HP students was also reported in a study aimed at examining effectiveness of branching path simulation in promoting the CT skills of undergraduate students, via an online medium.[32]
During virtual simulations, a patient is presented in an interactive, virtual manner. One study used virtually simulated patients to investigate the development of CT.[33] The study concluded that engaging in virtual simulations may support the increase of CT of the participants through role-playing and learning through trial and error.
A third subtheme that emerged was healthcare simulation-based gaming. In an explorative study, CT was measured using a contextual game. The study reported that the experimental group outperformed the control group with regard to CT.[34] Another source allowed participants to complete five virtual simulation experiences within a fixed time period.[35] The study showed that as experience levels increased, CT of students also increased.
Debriefing
Only 30% of sources included in this review focused on the debriefing phase of the simulation experiences. Debriefing can be done through various methods, mainly through guided reflection and concept mapping.
Guided reflection
A study determined the relationship between CT and the level of reflection and found a statistically significant positive relationship when students were asked to debrief through reflective journaling, supporting the relationship between CT and reflection.[36] One study reported on the use of a reflective debriefing immediately after a simulation. The author suggests that debriefing is the most important component of a simulation, as it consolidates learning that (often subconsciously) took place during the simulation. It is an essential cognitive step in the CT process.[23] The importance of reflection in action is alluded to by Mai et al.[22]Simulation experiences should be supported by a reflection process that allows the students to think critically about their actions. Follow-up debriefing sessions allow deeper insights to emerge and appreciation for clinical decision-making to develop.[22] A role-play study stated that through reflection students can gain insight into their own thinking that allows deeper understanding and fosters CT. The authors used reflection with a silent individual debriefing, followed by a collaborative debriefing (as a group) and an individual interview to promote CT.[41]
Concept mapping
The second subtheme for debriefing is the use of concept mapping. A concept map includes the learning outcomes associated with the simulation-based experience. In a pilot study, concept mapping during debriefing improved the CT of participants.[37] The concept map took the form of an active learning activity and assisted in guiding the debriefing discussions. Concept mapping helped the students engage in more CT than a group discussion on its own.[37]
Discussion
This scoping review confirms that CT can be promoted through SBHT. More importantly, it identified the simulation-based strategies that will yield a definite improvement in CT for HP students as they engage with simulation-based experiences.
Higher levels of fidelity (realism) during the simulation-based experience translates into the promotion of CT for HP students.'201 This finding might be attributed to HFS allowing a realistic learning experience where students are required to make decisions in a similar way to how they would in real clinical settings.[22] There are many simulation modalities that can be included in HP teaching activities. These modalities can be used as standalone strategies or combined in a hybrid simulation-based experience.[30] However, it can be deduced that the type of simulation modality is not the most important consideration. Each simulation-based activity should be planned and align with the expected learning outcomes, it needs to go through validity and reliability testing, and all types of fidelity should be addressed to ensure a true HFS experience - not only physical fidelity, but also conceptual and psychological fidelity.[38] It is important to remember a comprehensive active learning approach, involving all of the student's senses, is needed to foster CT.[41] The importance of including all the student's senses could explain why role-playing in simulation-based experiences was effective in promoting CT. All sources on role-playing reported the importance of allowing the student to play multiple roles in the scenario, not only the role of their chosen profession.
It is clear from this scoping review that no matter what approach is taken with the simulation-based experience (contact or computer based), scaffolding the learning activities to align them with the desired learning outcomes is ideal.[23] In addition, multiple exposures are preferable to a single exposure.[19]
Debriefing is an often-overlooked part of the SBH experience, most likely due to the time it takes to conduct.[39] Debriefing allows the students to develop new insights as they learn through experience. Learning through experience is the highest level of learning on the Miller's Framework,[40] and has been linked to the promotion of CT in current literature. It is therefore no surprise that studies that focused on debriefing during simulation-based experiences showed an improvement in the CT of students. Even though some studies did not initially focus on debriefing, they still concluded on the value of a debriefing in the promotion of CT. Debriefing can take many forms. This scoping review supports the notion that simulation-based activities that are combined with debriefing, through a reflection process, foster CT.[36] Debriefings should be conducted directly after the simulation-based experience[24] and be structured around the learning outcomes identified when planning the simulated experience.[37] This could be done by means of a concept map.
With the use of concept maps, educators can infuse theoretical concepts and discipline-specific implications.[37] This integrated approach seems to influence the students' ability to think critically. Once again, scaffolding of learning is important, even if it is through concept mapping that provides theoretical and instructional support during the debriefing experience.[37] In summary, correctly implemented simulation-based experiences with repeat practice and guided reflection will improve the CT of HP students.[7]
Conclusion
Although some articles do not show a distinct improvement in the CT of HP students when they engage with SBHT,[6] many authors have illustrated that SBHT has the potential to promote the CT of students within an HP domain. The aim of this scoping review was to identify how SBH education can be used to foster CT for HP students. To improve the CT of HP students through simulation-based training, this review identified that educators must appropriately plan the simulation-based experience, choose the correct simulation modality that aligns with the intended learning outcomes, and subject the activity to validity and reliability testing before implementation. Educators need to scaffold the learning and allow the student multiple exposures when teaching a skill. Lastly, a structured debriefing conducted directly after the simulation-based experience to allow for reflection is vital for the promotion of CT.
Declaration. None.
Acknowledgements. None.
Author contributions. Both authors conceptualised and designed the study, found sources and subjected sources to inclusion and exclusion criteria. KH was responsible for data analysis and both authors interpreted the results. KH drafted the article and both authors approved the final version.
Funding. None
Conflicts of interest. None
References
1. Levac D, Colquhoun H, O'Brien KK. Scoping studies: Advancing the methodology. Implement Sci 2010;5(1). https://doi.org/10.1186/1748-5908-5-69 [ Links ]
2. World Health Organization. Global standards for the initial education of professional nurses and midwives. Switzerland: WHO; 2009. https://www.who.int/hrh/nursing_midwifery/hrh_global_standards_education.pdf (accessed 9 February 2022). [ Links ]
3. South Africa. South African Qualifications Authority Act of 1995. NSB Regulations No. 452 of 1998. Government Gazette No. 18787, 1998. (Published under Government Notice R452) https://saqa.org.za/sites/default/files/2019-11/NSB%20Regulation%20No.%20R.%20482%2C%201998%20-%20English%20Version.pdf (accessed 9 February 2022). [ Links ]
4. Von Colln-Appling C, Giuliano D. A concept analysis of critical thinking: A guide for nurse educators. Nurse Educ Today 2017;1(49):106-109. https://doi.org/10.1016/j.nedt.2016.11.007 [ Links ]
5. Ertmer PA, Strobel J, Cheng X, et al. Expressions of critical thinking in role-playing simulations: Comparisons across roles. J Comput High Educ 2010;22(2):73-94. https://doi.org/10.1007/s12528-010-9030-7 [ Links ]
6. Scheffer C, Valk-Draad MP, Tauschel D, et al. Students with an autonomous role in hospital care - patients' perceptions. Med Teach 2018;40(9):944-952. https://doi.org/10.1080/0142159X.2017.1418504 [ Links ]
7. Blakeslee JR. Effects of high-fidelity simulation on the critical thinking skills of baccalaureate nursing students: A causal-comparative research study. Nurse Educ Today 2020;92:104494. https://doi.org/10.1016/j.nedt.2020.104494 [ Links ]
8. Svellingen AH, S0vik MB, R0ykenes K, Bratteb0 G. The effect of multiple exposures in scenario-based simulation - A mixed study systematic review. Nurs Open 2021;8(1):380-394. https://doi.org/10.1002/nop2.639 [ Links ]
9. Persico L. A Review: Using Simulation-based Education to Substitute Traditional Clinical Rotations. JOJ Nurse Health Care 2018; 9(3):555-762 https://doi.org/10.19080/JOJNHC.2018.09.555762 [ Links ]
10. Turrise SL, Thompson CE, Hepler M. Virtual simulation: Comparing critical thinking and satisfaction in RN-BSN students. Clin Simul Nurs 2020;46:57-61. https://doi.org/10.1016/j.ecns.2020.03.004 [ Links ]
11. Deitz GD, Fox AK, Fox JD. The effect of individual and team characteristics on simulation-enhanced critical thinking: A multilevel analysis. Market Educ Rev 2021;1-14. https://doi.org/10.1080/10528008.2021.1957689 [ Links ]
12. Louw A. Cognitive load theory in simulations to facilitate critical thinking in radiography students. Afr J Health Prof Educ 2021;13(1):41. https://doi.org/10.7196/AJHPE.2021.v13i1.1313 [ Links ]
13. Salleh SM, Tasir Z, Shukor NA. Web-based simulation learning framework to enhance students' critical thinking skills. Procedia - Social Behav Sci. 2012;64:372-381. https://doi.org/10.1016/j.sbspro.2012.11.044 [ Links ]
14. Albert S. Applied critical thinking in strategy: Tools and a simulation using a live case. J Educ Business 2021;96(4):252-259. https://doi.org/10.1080/08832323.2020.1792395 [ Links ]
15. Bunt B, Gouws G. Using an artificial life simulation to enhance reflective critical thinking among student teachers. Smart Learning Environments 2020;7:12 https://doi.org/10.1186/s40561-020-00119-6 [ Links ]
16. Arksey H, O'Malley L. Scoping studies: Towards a methodological framework. Int J Soc Res Method 2005;8:19-32. https://doi.org/10.1080/1364557032000119616 [ Links ]
17. Sucharew H, Macaluso M. Methods for research evidence synthesis: The scoping review approach. J Hosp Med 2019;14(7):416-418. https://doi.org/10.12788/jhm.3248 [ Links ]
18. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med 2018(169):467-473. https://doi.org/10.7326/M18-0850 [ Links ]
19. Ka Ling F, Lim Binti Abdullah K, Seng Chiew G, Danaee M, Chan CMH. The impact of high fidelity patient simulation on the level of knowledge and critical thinking skills in code blue management among undergraduate nursing students in Malaysia. SAGE Open Nurs. 2021;11(2). https://doi.org/10.1177%2F21582440211007123 [ Links ]
20. Hagemann V, Herbstreit F, Kehren C, et al. Does teaching non-technical skills to medical students improve those skills and simulated patient outcome? Int J Med Educ 2017(8):101-113. https://doi.org/10.5116/ijme.58c1.9f0d [ Links ]
21. Munroe B, Buckley T, Curtis K, Morris R. Designing and implementing full immersion simulation as a research tool. Australas Emerg Nurs J 2016;19:90-105. https://doi.org/10.1016/j.aenj.2016.01.001 [ Links ]
22. Mai JA, Pilcher RL, Frommelt-Kuhle M. Fostering interprofessional collaboration and critical thinking between nursing and physical therapy students using high-fidelity simulation. J Interprof Educ Pract 2018;10:37-40. https://doi.org/10.1016/j.xjep.2017.11.002 [ Links ]
23. Louw A. Cognitive load theory in simulations to facilitate critical thinking in radiography students. Afr J Health Prof Educ 2021;13(1):41. https://doi.org/10.7196/AJHPE.2021.v13i1.1313 [ Links ]
24. Bartlett RS, Bruecker S, Eccleston B. High-fidelity simulation improves long-term knowledge of clinical swallow evaluation. Am J Speech Lang Pathol 2021;30(2):673-686. https://doi.org/10.1044/2020_AJSLP-20-00240 [ Links ]
25. Arunachalam S, Priya E, Saxena K, Andiesta NS. Virtual role-playing simulation as clinic: A model for experiential learning of critical thinking skills. J Dent Educ 2021;85(S1):1055-1058. https://doi.org/10.1002/jdd.12472 [ Links ]
26. Kim E. Effect of simulation-based emergency cardiac arrest education on nursing students' self-efficacy and critical thinking skills: Roleplay versus lecture. Nurse Educ Today 2018;61:258-263. https://doi.org/10.1016/j.nedt.2017.12.003 [ Links ]
27. Shin H, Ma H, Park J, Ji ES, Kim DH. The effect of simulation courseware on critical thinking in undergraduate nursing students: Multi-site pre-post study. Nurse Educ Today 2015;35(4):537-542. https://doi.org/10.1016/j.nedt.2014.12.004 [ Links ]
28. Macauley K, Brudvig TJ, Kadakia M, Bonneville M. Systematic review of assessments that evaluate clinical decision making, clinical reasoning, and critical thinking changes after simulation participation. J Phys Ther Educ 2017;31(4):64-75. https://doi.org/10.1097/JTE.0000000000000011 [ Links ]
29. Al Gharibi K, Arulappan J. Repeated simulation experience on self-confidence, critical thinking, and competence of nurses and nursing students - An integrative review. SAGE Open Nurs 2020;6 https://doi.org/10.1177/2377960820927377 [ Links ]
30. Unver V, Basak T, Ayhan H, et al. Integrating simulation based learning into nursing education programs: Hybrid simulation. Technol Health Care 2018;26(2):263-270. https://doi.org/10.3233/THC-170853 [ Links ]
31. Abuzaid MM, Elshami W Integrating of scenario-based simulation into radiology education to improve critical thinking skills. Rep Med Imaging 2016;9:17-22. https://doi.org/10.2147/RMI.S110343 [ Links ]
32. Rababa M, Masha'al D. Using branching path simulations in critical thinking of pain management among nursing students: Experimental study. Nurse Educ Today 2020;86:104323. https://doi.org/10.1016/j.nedt.2019.104323 [ Links ]
33. Peddle M. Participant perceptions of virtual simulation to develop non-technical skills in health professionals. J Res Nurs 2019;24(3-4):167-180. https://doi.org/10.1177/1744987119835873 [ Links ]
34. Chang CY, Kao CH, Hwang GJ, Lin FH. From experiencing to critical thinking: A contextual game-based learning approach to improving nursing students' performance in electrocardiogram training. Educ Technol Res Dev 2020;68(3):1225-1245. https://doi.org/10.1007/s11423-019-09723-x [ Links ]
35. Luu C, Talbot TB, Fung CC, et al Development and performance assessment of a digital serious game to assess multi-patient care skills in a simulated pediatric emergency department. Simul Gaming 2020;51(4):550-570. https://doi.org/10.1177/1046878120904984 [ Links ]
36. Padden-Denmead ML, Scaffidi RM, Kerley RM, Farside AL. Simulation with debriefing and guided reflective journaling to stimulate critical thinking in prelicensure baccalaureate degree nursing students. J Nurs Educ 2016;55(11):645-650. https://doi.org/10.3928/01484834-20161011-07 [ Links ]
37. Odreman HA, Clyens D. Concept mapping during simulation debriefing to encourage active learning, critical thinking, and connections to clinical concepts. Nurs Educ Perspect 2020;41(1):37-38. https://doi.org/10.1097/01.NEP.0000000000000445 [ Links ]
38. Wolters Kluwer. Increasing fidelity and realism in simulation for nursing students. https://www.wolterskluwer.com/en/expert-insights/increasing-fidelity-and-realism-in-simulation (accessed 16 February 2022). [ Links ]
39. Ostovar S, Allahbakhshian A, Gholizadeh L, Dizaji S, Sarbakhsh P, Ghahramanian A. Comparison of the effects of debriefing methods on psychomotor skills, self-confidence, and satisfaction in novice nursing students: A quasi-experimental study. J Adv Pharm Technol Res 2018;9(3):107-112. https://doi.org/10.4103/japtr.JAPTR_291_18 [ Links ]
40. Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65(9):S63-67. https://doi.org/10.1097/00001888-199009000-00045 [ Links ]
 Correspondence:
Correspondence:
K Henrico
karienr@uj.ac.za
Accepted 13 July 2022














