Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
African Journal of Health Professions Education
versión On-line ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.14 no.3 Pretoria sep. 2022
http://dx.doi.org/10.7196/AJHPE.2022.v14i3.1570
RESEARCH
Student review of doctor-patient communication skills training in a South African undergraduate medical programme
D SwinfenI; M LabuschagneII; G JoubertIII
IMB ChB, MHPE; Clinical Simulation and Skills Unit, School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIMB ChB, MMed (Ophthalmol), PhD; Clinical Simulation and Skills Unit, School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIMSc; Department of Biostatistics, School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND. Barriers to the training of doctor-patient communication in the South African (SA) context have been well explored through qualitative research at several SA medical schools. However, this aspect of training has not been reviewed in a systematic way by a large number of students. A student review of doctor-patient communication skills training in the undergraduate medical programme of a medical school in SA was obtained to improve training and identify further research needs.
OBJECTIVE. To investigate doctor-patient communication skills training in the undergraduate programme of a medical school in SA to identify shortcomings and further research needs.
METHODS. A descriptive, cross-sectional design was used. Data were collected through an anonymous questionnaire based on Hardens extended vision of the curriculum. Printed anonymous questionnaires, distributed to all the fourth- and fifth-year undergraduate medical students, were analysed quantitatively. Open-ended questions were analysed qualitatively using grounded theory.
RESULTS. The sample comprised 106/132 fifth-year students (response rate 80.3%) and 65/120 fourth-year students (response rate 54.2%). Frequent training in history-taking was reported by >75% of students, while >60% reported infrequent training in breaking bad news. More than 50% of participants indicated that senior doctors seldom or never modelled patient-centred communication in the clinical teaching milieu. Students preferred experiential learning to didactic methods.
CONCLUSION. Medical students want to see patient-centred communication unequivocally modelled in the clinical setting. A greater emphasis on practical training in context-specific communication skills is required. Positive role-modelling is needed in the clinical environment.
According to Silverman, accomplished doctors should be 'humane and compassionate, empathetic and supportive'.[1] Conversely, consultations devoid of empathy and compassion can leave patients feeling confused and humiliated.[2] Effective doctor-patient communication improves patient care[3,4] and job satisfaction of doctors,[5] while it reduces healthcare costs[4 and the risk of litigation.[6] The myths that communication skills and empathy cannot be taught have been debunked.[7,8] It is therefore clear why professional regulators require medical trainees to become skilled communicators. [9,10]
Guidelines for best practice based on international medical education evidence emphasise a focus on patient-centredness and experiential learning to nurture effective doctor-patient communication.[8,11,12] Many challenges exist in terms of the adaptation and application of these guidelines to the South African (SA) context. Doctors working in the public health sector struggle to provide adequate healthcare due to staff shortages and a high burden of disease, leaving them with limited time for clinical teaching. Additionally, they often lack grounding in medical education.[13] Secondly, the cultural diversity in the SA context necessitates a particular emphasis on intercultural communication and learning of local languages to improve healthcare and ensure social accountability.[14] Thirdly, the effects of the hidden curriculum are evident in SA when doctor-patient communication modelled in the clinical setting reportedly contradicts the principles taught.[7,15]
At the University of the Free State (UFS) in Bloemfontein, limited information was available on how useful students find different facets of communication skills training and of the context-specific challenges encountered. Undergraduate medical students in the clinical phase of their training were therefore asked to review the doctor-patient communication skills training received during all phases of the programme. The study aimed to add to the knowledge of the doctor-patient communication skills training in the undergraduate medical programme at the UFS, enabling the development of the training programme and the identification of further research needs.
Methods
Study setting
At the UFS, the minimum duration of the undergraduate medical programme is 5 years. The programme is divided into three phases. Phase I is the introductory phase with a duration of 6 months. Phase II is the pre-clinical phase, lasting 2 years. Phase III is the clinical phase lasting 2.5 years. Communication skills training takes place throughout all three phases. In the introductory phase (phase I), communication skills training is included in three modules and the mode of delivery is lectures. In the pre-clinical phase (phase II), communication skills are taught through role-play with peers and simulated patients during the clinical skills module. During the clinical phase of the training (phase III), communication skills are taught formally through lectures, small-group discussions and interprofessional simulation. Training based on role-modelling occurs implicitly during the clinical rotations and community-based education.
Study design, measurement and participants
A descriptive cross-sectional quantitative design was used. Following a literature study, a questionnaire was designed to enable a student review of doctor-patient communication skills training in all three phases. Hardens extended vision of the curriculum formed the backbone of the questionnaire (appendix: https://www.samedical.org/file/1881). Themes in the questionnaire were the outcomes, content, educational methods, assessment methods, learning opportunities and educational environment pertaining to training of doctor-patient communication.[16] Questions were predominantly quantitative and focused on the frequency of training, and training opportunities. Statements rather than questions were used, allowing respondents to agree or disagree by choosing an option on a modified Likert scale. The categories 'not at all' and 'seldom' were grouped as infrequent when referring to the results in the text, and 'often' and 'almost always' as frequent. Open questions gave participants the opportunity to motivate their answers and add additional comments.
The study sample consisted of all medical students in their final and penultimate years of undergraduate studies. Printed anonymous questionnaires were distributed to all the fourth- and fifth-year undergraduate medical students at the UFS. More junior students were not included in the sample as they could not review the training through all three phases. The possibility of perceived threat to the respondents was reduced because the researcher is not involved in the tuition of students in the clinical phase of training. For the sake of convenience, students were asked to consider immediate completion. Students who completed their forms later inserted their questionnaires within a week into a sealed box held by their student group leader. The student group leaders returned these boxes to the researcher's office.
Statistical analysis
Data from the questionnaires were entered into an Excel (Microsoft, USA) spreadsheet, and quantitative data analysis was done by the UFS Department of Biostatistics. Categorical variables were summarised by frequencies and percentages, and numerical variables by medians and ranges. For the qualitative analysis, answers to open-ended questions were reviewed by the first author. Emerging subthemes, categories and subcategories were identified making use of grounded theory, by using open coding, axial coding and selective coding of the text. Verification of categories was done through consensus meetings with one of the co-authors.
Ethical considerations
The UFS Health Sciences Research Ethics Committee (HSREC) granted ethical approval (ref. no. UFS-HSD2019/0327/2506). Permission was obtained from the relevant authorities at the UFS. Voluntary completion of the questionnaire implied consent to participate in the study. Participation was anonymous, with a number allocated to each questionnaire to prevent disclosure of any personal information.
Results
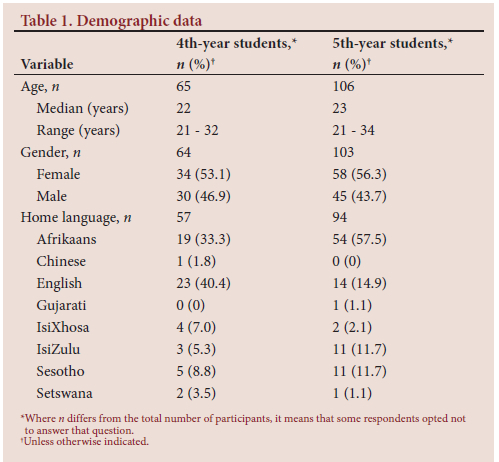
The study sample consisted of 106/132 fifth-year students (response rate 80.3%) and 65/120 fourth-year students (response rate 54.2%). Due to the difference in response rate, the year group results are presented separately. The demographic data of participants appear in Table 1, which shows that students represented diverse language groups. The remaining results are reported according to the themes in the questionnaire, based on Harden's extended view of the curriculum.[16]
Outcomes
According to >80% of participants, educators informed them frequently of the expected outcomes during the clinical training phase.
Content
More than 75% of participants in both year groups reported frequent training in history-taking during the pre-clinical and clinical part of the programme (Table 2). Most final-year students rated their history-taking ability as excellent. However, >60% of respondents in both groups reported infrequent practical training in breaking bad news. More than 85% of respondents rated themselves as novices or average in this particular skill. In terms of managing language and cultural differences during the consultation, more than half of the respondents (mean 62.6% of fourth-year students over phase I - III; mean 65.7% of fifth-year students over phase I -III) reported infrequent training throughout the programme (Table 2).
Students were asked to rank communication skills training methods that they had experienced during all phases of training, from 1 (most preferred method) to 6 (least preferred). Both groups ranked small-group practice with simulated patients the highest (Table 3). The fifth-year students equally favoured receiving feedback after an observed consultation. The least preferred methods in both year groups were lectures and video recording of student consultations. Table 3 also indicates whether these methods were used during the various phases of training.
Assessment
More than 60% of respondents in both groups concluded that the assessment content in the clinical phase frequently demonstrated the importance of doctor-patient communication skills (Table 2). According to the fourth-year students, the optimal method for assessing doctor-patient communication skills was the objective structured clinical examination (OSCE), while fifth-year students most frequently mentioned assessment in the clinical setting.
Learning opportunities
According to 90% of students, opportunities to develop doctor-patient communication skills in the introductory phase were infrequent (Table 2). More than 50% of students indicated frequent opportunities in the pre-clinical phase, while 80% of students stated that frequent learning opportunities were available in the clinical phase. More than 70% of participants reported infrequent opportunities for reflection on their communication with patients during the clinical training phase (Table 2).
Learning environment
More than 70% of students indicated that the learning environment in the clinical phase promoted the development of communication skills, owing to increased contact with patients. The question regarding the role-modelling of patient-centred communication elicited conflicting opinions. Over 40% of respondents in both groups reported that senior doctors were often or almost always good role models. However, >50% of students in both groups indicated that senior doctors seldom or never modelled patient-centred communication (Table 2).
Student suggestions for improvement to the training of doctor-patient communication skills
Subsequent to analysis of open questions, the following framework of suggestions emerged: educator factors; healthcare factors; student factors; and training factors. In terms of educator factors, students recommended that senior doctors should receive training on the importance of communication skills, and made a plea for greater humility of doctors when communicating with patients. Regarding the healthcare environment, participants in the study remarked that the workload adversely influenced the possibility of acquisition of communication skills. Student factors that were highlighted were the importance of choosing whether to emulate positive or negative role models. The importance of individual student commitment to the acquisition of skills was emphasised. Recommendations based on training factors were:
• devote more time to the training of communication skills
• facilitate an earlier and gradually phased entry into the clinical phase
• include more bedside teaching of communication skills and feedback from experienced doctors who observe clinical consultations
• consider continuous assessment of students' communication skills with patients
• increase the frequency of interactive practice sessions with simulated or real patients, emphasising students' preference for active learning methods
• orientate students to the clinical phase by placement in family medicine as early as possible, owing to the holistic approach and patient-centred care witnessed
• include clinical communication competency as part of the prerequisite skills recorded in the clinical rotation logbooks.
Discussion
A likely explanation for the discrepancy in response rates between the year groups is the fact that more fifth-year students opted for immediate completion of questionnaires. The results are discussed according to the themes in the questionnaire, namely outcomes, the content of training, educational methods, assessment, learning opportunities and educational environment.[16] Subsequently, suggestions for improvement of training based on analysis of open questions will be discussed. Direct quotes from students' comments are indicated by their study year and questionnaire number in brackets after the quote; for example, 4.18 represents questionnaire number 18 completed by a fourth-year student.
Outcomes
The fact that students were informed of expected outcomes conforms to scholarly recommendations that educators should elucidate the purpose of training regularly to optimise student engagement.[17] More discussions regarding the aims of doctor-patient communication skills training in the introductory and pre-clinical phases might be useful, as students reported not being made aware frequently of the expected outcomes during these phases.
Content
Students reported frequent training in history-taking, but asked for more frequent practical training sessions in breaking bad news. Students cited the following examples:
'Doctors avoid talking about breaking bad news.' (4.14)
'Doctors are usually blunt and unsympathetic.' (4.63)
'We always need to make the picture clear and explain to the patient after the registrar broke the news in an unprofessional and cold manner.' (5.100)
These descriptions align with a literature review showing that many qualified doctors have not received formal tuition in this task, find it stressful and might avoid the task altogether for fear of how the patient might react.[18] SA scholars recommended that communication and the handling of loss and grief should be an integral part of the medical curriculum.[19] Training interventions have been shown to increase student confidence and lead to a noticeable improvement in students' ability to convey bad news sensitively.[20]
Students indicated the need for more frequent training in managing language and cultural differences, and reported communication difficulties due to a lack of fluency in Sesotho and Afrikaans. Sesotho is the home language of 71.9% of residents in the Free State Province of SA, while Afrikaans is the home language of 10.9% of Free State residents.[21] Lack of fluency in Sesotho was not only mentioned by students speaking Afrikaans or English as their home language, but also several students who spoke isiZulu at home and English as an additional language. Students expressed frustration at the lack of professional interpreters. Some students deliberately avoided seeing patients whose language they could not speak by asking other students to attend to them. These findings are supported by research recommendations for a greater focus on the acquisition of local languages and the availability of interpreters in the SA medical education context.[8,16]
Educational methods
Students valued feedback, direct observation and practical interactive methods in terms of communication skills training. Students from both year groups ranked small-group training with simulated patients as the most effective educational method. Final-year students ranked observation of their consultants with real patients as equally effective. Research evidence confirmed that these experiential methods are most effective.[8] An unexpected finding was that many students disliked peer practice, e.g.: 'With peers, students tend to make a joke of everything.' (5.56) 'Small group [sic] practice often resulted in chaos.' (5.51)
These remarks are contrary to research that indicated peer practice of communication skills training as a low-cost, effective teaching method.[22] Facilitators should make provision for students who find small-group sessions particularly stressful by creating a safer environment for peer practice. One way to achieve this is by establishing clear ground rules regarding peer feedback.[23]
Assessment
Assessment significantly influences learning.[16] Students reported that assessments in the clinical phase showed that communications skills were deemed important. Fourth-year students considered the OSCE as the best method to assess doctor-patient communication, while fifth-year students most frequently indicated assessment in the clinical setting, as reflected by the following comment:
'Real contact with real patients because then you are expected to behave professionally in real-life situations.' (5.48)
Medical education scholars have confirmed the need for authentic assessment, and emphasise the importance of using workplace-based assessment tools such as the mini-clinical evaluation exercise (mini-CEX) and constructive feedback by trained assessors to provide ongoing formative assessment.[24]
Learning opportunities
In this review, students reported infrequent opportunities to develop communication skills in the initial phase of training. Earlier clinical exposure was one of the student recommendations to improve communication skills training, which was in accordance with research findings that early clinical exposure promotes the development of a mature and empathic approach towards patients.[25] Students reported infrequent opportunities to reflect on their communication with patients. This finding agreed with conclusions reported in the literature that there is a greater focus on medical management of patients during the clinical phase. Formal communication tuition usually takes place in the pre-clinical phase when there is infrequent or no patient contact.[26] Archer and Meyer[7] recommend greater support for medical students to deal with challenges in their clinical years through discussions, constructive feedback and reflection.
Educational environment
Most students reported that the learning environment frequently enhanced communication skills training. However, students who reported that the learning environment was not conducive to developing communication skills gave the following examples:
'You feel pressured and overloaded with the amount of patients.' (5.3)
'Everything is rushed.' (4.46)
'The learning environment is very goal-orientated and not focused on patients' well-being.' (4.4).
Students who indicated that senior doctors were good role models described them as professional, experienced and good mentors. Students pointed out inconsistencies, such as:
'Some doctors really talk and listen to their patients, but others are [expletive language] inhumane with how little regard they have for them.' (5.30)
'Some doctors exhibit good communication skills, while others are demeaning and unprofessional.' (4.11)
Similar experiences that left students conflicted and uncomfortable have been described in other SA medical education studies.[7,15-Student suggestions that doctors should be held accountable for poor communication with patients corresponded with research recommendations. Matthews and van Wyk[15] propose that performance indicators of clinical educators should include an appraisal of their professionalism and communication with patients. Students' descriptions of the pressure on clinical teachers resonate with findings in the medical education literature regarding the detrimental impact of workload and staff shortages on the training of students in the SA public healthcare sector.[13]
A student who observed that they witness good and bad examples, and ultimately have to choose their own behaviour, commented:
'Some doctors just don't care about how they speak to patients and some do. We see both daily and then decide how we want to be.' (4.12)
This opinion is in keeping with Benbassat's[27] perspective that medical students should be encouraged to reflect on the behaviour of clinical teachers and develop discernment in terms of which behaviour to emulate.
In their suggestions to improve training, students highlighted the importance of each student's responsibility to engage. This aligns with the educational principle of active learning and taking ownership of learning.[28] From their comments, it was clear that students found the approach to communication skills training in the clinical phase fragmented and lacking coherence. Other researchers in the broader SA medical education context have pointed out similar inconsistencies in communication skills training, and a more standardised, integrated and interdisciplinary approach was recommended.[15]
Strengths and limitations of the study
The high response rate and the data collection tool that enabled the probing of a vast area of medical education in a short time were strengths of the study. Open-ended questions encouraged student reflection, and participants engaged well with the questionnaire. Their answers showed compassion and indignation, which was encouraging. The anonymity of the questionnaire gave students the courage to voice their concerns regarding the behaviour of doctors towards patients.
Limitations of the study included the cross-sectional design, which provided sparse information compared with longitudinal designs. Potential recall bias could have limited the conclusions that can be drawn from the results. The generalisability of the data is limited, as the research was conducted at a single SA medical school. However, the challenges identified resemble those reported by other SA medical educators. The fact that only students participated gives an incomplete picture, as the perspectives of patients, caregivers and educators are not represented.
Recommendations
The findings of the student review confirm the need for a greater emphasis on the learning of local languages and managing cultural differences. Additionally, the need for more frequent practical training sessions in breaking bad news is clear. Peer practice needs to be facilitated by skilled facilitators, with an adequate facilitator-to-student ratio. Educators across different phases of the training programme should meet to discuss how the training and assessment of communication skills can be co-ordinated, and whether earlier clinical exposure could be trialled. Communication skills lectures should be augmented with interactive small-group teaching sessions.
Teaching and assessment need to be undertaken by clinical teachers who have had training in doctor-patient communication. A reflective portfolio to log challenging communication scenarios and subsequent insights could be considered. Medical educators should deliberate on strategies to address doctors' unprofessional behaviour towards patients to reduce the negative impact on both patients and trainees. Possible strategies include additional staff training in professionalism for all clinical teachers. Anonymous multi-source feedback on professionalism and teaching skills could form part of the key performance indicators of clinical teachers.
Conclusion
This student review provides medical educators in SA with food for thought. Familiar themes emerge in SA studies focusing on communication skills training in medicine: students are ill-equipped to deal with language and cultural aspects of consultations in the diverse healthcare setting. Poor role-modelling of communication skills remains prevalent, yet no clear framework is available to improve the working conditions for clinician-educators or to assess their professionalism. These issues need to be reviewed and addressed at the level of public health managers and professional regulators. Further research is required to assess the communication needs of patients and the views of educators.
Medical educators should place a greater emphasis on experiential learning of doctor-patient communication, including complex skills such as breaking bad news and managing language and cultural differences. Clinical teachers should be empowered by guidance, training and practical support to model patient-centred communication.
Declaration. This article is based on research conducted by DS in partial fulfilment of the requirements for the structured Master's degree in Health Professions Education (MHPE) in the Division of Health Sciences Education, Faculty of Health Sciences, UFS.
Acknowledgements. The authors wish to thank the study participants for their enthusiastic contributions, and Dr Daleen Struwig, medical writer/editor, for technical and editorial preparation of the manuscript.
Author contributions. DS and ML conceptualised and planned the execution of the study. DS wrote the research protocol, collected the data and wrote the first draft of the article. ML was the study supervisor and contributed to editing of the article. GJ performed the statistical analysis, assisted with the interpretation of data and contributed to editing of the article. All the authors approved the final version of the article.
Funding. The study was funded by a Health and Welfare Sector Education and Training Authority bursary.
Conflicts of interest. None.
References
1. Silverman BD. Physician behavior and bedside manners: The influence ofWilliam Osler and the Johns Hopkins School of Medicine. Baylor Univ Med Cent Proc 2012;25(1):58-61. https://doi.org/10.1080/08998280.2012.11928784 [ Links ]
2. Dolezal L. The phenomenology of shame in the clinical encounter. Med Health Care Philos 2015;18(4):567-576. https://doi.org/10.1007/s11019-015-9654-5 [ Links ]
3. Riedl D, Schüssler G. The influence of doctor-patient communication on health outcomes: A systematic review. Psychosom Med Psychother 2017;63(2):131-150. https://doi.org/10.13109/zptm.2017.63.2.131 [ Links ]
4. Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: A systematic review. Br J Gen Pract 2013;63(606):e76-e84. https://doi.org/10.3399/bjgp13X660814 [ Links ]
5. Deng S, Yang N, Li S, Wang W, Yan H, Li H. Doctors' job satisfaction and its relationships with doctor-patient relationship and work-family conflict in China: A structural equation modelling. Inquiry 2018;55:004695801879083. https://doi.org/10.1177/0046958018790831 [ Links ]
6. Huntington B, Kuhn N. Communication gaffes: A root cause of malpractice claims. Baylor Univ Med Cent Proc 2003;16(2):157-161. https://doi.org/10.1080/08998280.2003.11927898 [ Links ]
7. Archer E, Meyer IS. Applying empathic communication skills in clinical practice: Medical students' experiences. S Afr Fam Pract 2021;63(1):a5244. https://doi.org/10.4102/safp.v63i1.5244 [ Links ]
8. Berkhof M, van Rijssen HJ, Schellart AJM, Anema JR, van der Beek AJ. Effective training strategies for teaching communication skills to physicians: An overview of systematic reviews. Patient Educ Couns 2011;84(2):152-162. https://doi.org/10.1016/j.pec.2010.06.010 [ Links ]
9. Frank JR, Snell LS, Sherbino J. CanMEDS 2015 Physician Competency Framework. http://canmeds.royalcollege.ca/en/framework (accessed 3 May 2021). [ Links ]
10. Health Professions Council of South Africa. Core competencies for undergraduate students in clinical associate, dentistry and medical teaching and learning programmes in South Africa. Pretoria: HPCSA, 2014. http://www.hpcsa-blogs.co.za/wp-content/uploads/2017/04/MDB-Core-Competencies-ENGLISH-FINAL-2014.pdf (accessed 3 May 2021). [ Links ]
11. Bachmann C, Abramovitch H, Barbu CG, et al. A European consensus on learning objectives for a core communication curriculum in health care professions. Patient Educ Couns 2013;93(1):18-26. https://doi.org/10.1016/j.pec.2012.10.016 [ Links ]
12. Von Fragstein M, Silverman J, Cushing A, Quilligan S, Salisbury H, Wiskin C. UK consensus statement on the content of communication curricula in undergraduate medical education. Med Educ 2008;42(11):1100-1107. https://doi.org/10.1111/j.1365-2923.2008.03137.x [ Links ]
13. Burch V. Medical education in South Africa: Assessment practices in a developing country. PhD thesis. Rotterdam: Erasmus University, 2007. https://core.ac.uk/download/18508920.pdf (accessed 3 May 2021). [ Links ]
14. Matthews MG, van Wyk JM. Exploring a communication curriculum through a focus on social accountability: A case study at a South African medical school. Afr J Prim Health Care Fam Med 2018;10(1):a1634. https://doi.org/10.4102/phcfm.v10i1.1634 [ Links ]
15. Matthews MG, van Wyk JM. Improving communication in the South African healthcare context. Afr J Health Professions Educ 2018;10(4):194-198. https://doi.org/10.7196/AJHPE.2018.v10i4.1000 [ Links ]
16. Quirk ME, Harden RM. Curriculum planning and development. In: Dent JA, Harden RM, Hunt D (editors). A Practical Guide for Medical Teachers. 5th ed. London: Elsevier, 2017:4-11. [ Links ]
17. Ley T, Kisielewska J, Collett T, Burr S. Improving communication for learning with students: Expectations, feedback and feedforward. https://doi.org/10.15694/mep.2019.0000141 [ Links ]
18. Alelwani SM, Ahmed YA. Medical training for communication of bad news: A literature review. J Educ Health Promot 2014;3(1):51. https://doi.org/10.4103/2277-9531.134737 [ Links ]
19. Ganca LL, Gwyther L, Harding R, Meiring M. What are the communication skills and needs of doctors when communicating a poor prognosis to patients and their families? A qualitative study from South Africa. S Afr Med J 2016;106(9):940-944. https://doi.org/10.7196/SAMJ.2016.v106i9.10568 [ Links ]
20. Johnson J, Pangioti M. Interventions to improve the breaking of bad or difficult news by physicians, medical students, and interns/residents: A systematic review and meta-analysis. Acad Med 2018;93(9):1400-1412. https://doi.org/10.1097/ACM.0000000000002308 [ Links ]
21. Statistics South Africa. Provincial Profile Free State Report 03-01-12. Community Survey 2016. StatsSA, 2016. http://cs2016.statssa.gov.za/?portfolio_page=community-survey-2016-provincial-profile-free-state-2016 (accessed 3 May 2021). [ Links ]
22. Bosse HM, Schultz J, Nickel M, et al. The effect of using standardised patients or peer role play on ratings of undergraduate communication training: A randomised controlled trial. Patient Educ Couns 2012;87(3):300-306. https://doi.org/10.1016/j.pec.2011.10.007 [ Links ]
23. Kurtz S, Silverman J, Draper J. Teaching and Learning Communication Skills in Medicine. 2nd ed. Oxford: Radcliffe Publishing Ltd, 2005. [ Links ]
24. Norcini J, Burch V Workplace-based assessment as an educational tool: AMEE Guide No. 31. Med Teach 2007;29(9):855-871. https://doi.org/10.1080/01421590701775453 [ Links ]
25. Yardley S, Littlewood S, Margolis SA, et al. What has changed in the evidence for early experience? Update of a BEME systematic review. Med Teach 2010;32(9):740-746. https://doi.org/10.3109/0142159X.2010.496007 [ Links ]
26. Levinson W, Roter D. The effects of two continuing medical education programs on communication skills of practicing primary care physicians. J Gen Intern Med 1993;8(6):318-324. https://doi.org/10.1007/BF02600146 [ Links ]
27. Benbassat J. Role modeling in medical education: The importance of a reflective imitation. Acad Med 2014;89(4):550-554. https://doi.org/10.1097/ACM.0000000000000189 [ Links ]
28. Harden RM, Laidlaw J. Essential Skills for a Medical Teacher: An Introduction to Teaching and Learning in Medicine. 2nd ed. London: Elsevier, 2016. [ Links ]
 Correspondence:
Correspondence:
D Swinfen
swinfend@ufs.ac.za
Accepted 26 October 2021














