Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.14 n.2 Pretoria Jun. 2022
http://dx.doi.org/10.7196/ajhpe.2022.v14i1.1466
RESEARCH
The effect of the initial months of the COVID-19 national lockdown on MMed training activities at the University of the Free State, South Africa
C MeyerI; C BarrettII; G JoubertIII; N MofoloIV
IPhD; School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIMB ChB, MMed (Int Med); School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIMSc; Department of Biostatistics, School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IVMB ChB, MFamMed; School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Shortly after the first case of SARS-CoV-2 infection (COVID-19) had been reported in South Africa, a national lockdown was declared. Subsequently, the University of the Free State (UFS) changed from a contact delivery mode to remote multimodal teaching, learning and assessment
OBJECTIVES: To determine the effect of the initial months of the COVID-19 lockdown on MMed training activities at the UFS, specifically the demographic and health profile of students, research progress, academic activities and the clinical training environment
METHODS: A cross-sectional study using an anonymous self-administered questionnaire was used. All registered MMed students at the UFS were eligible to participate
RESULTS: A response was obtained from 134 (51.9%) of 258 registrars, most of whom were included in the analysis (n=118; 45.7%). Significant associations between the effect of the COVID-19 lockdown on day-to-day clinical work and the ability to work on MMed research (p<0.01) and self-directed learning time (p<0.01) were noted. Changes in domestic circumstances affecting MMed research were reported by 26.9% of respondents. Worsening or new symptoms of stress were reported by 40.0% of respondents
CONCLUSION: The initial months of the COVID-19 lockdown might have far-reaching implications for registrars' academic progress. Registrars experienced adverse psychosocial consequences that might impede their academic progress
The first SARS-CoV-2 (COVID-19) infection in South Africa (SA) was recorded on 5 March 2020.[1] In response to the pandemic and in order to 'flatten the curve' and delay the spread of COVID-19, the SA government announced a 21-day national lockdown effective 27 March 2020, which was extended for 2 more weeks. Five alert levels were announced, with alert level 5 measures and regulations being the most stringent and alert level 1 the most lenient. Alert level 4 lockdown was implemented on 1 May, level 3 on 1 June, level 2 on 18 August, and level 1 on 21 September 2020.[2] Consequently, as with all universities countrywide, the University of the Free State (UFS) had to change from a contact delivery mode to remote multimodal teaching, learning and assessment, with ensuing challenges. These measures also affected postgraduate training.
Registrars are medical doctors receiving 48 - 60 months of supervised postgraduate training in public health hospitals to gain specialist-level expertise. Registrars are both Master's (MMed) students and healthcare workers - essential staff who had to continue working in hospitals during the lockdown. Tension exists between these dual roles, especially when service delivery affects training. In teaching hospitals, registrars often perform the bulk of clinical service delivery. This situation continues during the COVID-19 pandemic and many of the registrars are working on the frontline of the pandemic, often being deployed to function in areas outside their scope of practice, the effect of which should not be overlooked.[3] The risk of contracting COVID-19 in the workplace remains concerning. By 13 August 2020, at least 240 healthcare workers had died due to COVID-19 in SA, with 1 644 reported infections among doctors in the country.[4]
The compulsory research component of the MMed curriculum at the UFS[5] entails two modules, namely research methodology and a mini-dissertation. According to the milestones stipulated by the UFS, the research methodology module (12 credits) must be completed within 24 months of registration, and the mini-dissertation (64 credits) should be completed prior to enrolling for the Colleges of Medicine of SA (CMSA) final assessment. In the past, some registrars struggled to complete their research projects within the minimum residency period. Although a reduced clinical workload due to COVID-19 might provide an opportunity to work on academic activities, including research,[6] it is not known what effect the initial months of the national lockdown had on registrars at our institution.
The aim of the study was to determine the effect of the initial months (26 March - 30 June 2020) of the COVID-19 lockdown on MMed training activities at the UFS. The objectives were: (i) to describe the registrars' demographic and health profile relevant to the pandemic; (ii) to determine the effect of the lockdown on MMed research progress; (iii) to describe the effect on postgraduate academic activities and the clinical training environment; and (iv) to determine how these factors were inter-related.
Methods
Study design
A cross-sectional study using an anonymous self-administered questionnaire was conducted at the Faculty of Health Sciences, UFS, in Bloemfontein, SA.
Setting
The UFS, with its main campus in Bloemfontein, is one of nine universities in SA that offer medical specialist training programmes (MMed). The Faculty of Health Sciences at the UFS comprises five schools, namely the School of Clinical Medicine, School of Pathology, School of Biomedical Sciences, School of Health and Rehabilitation Sciences and School of Nursing. The MMed is offered in the School of Pathology (six disciplines, one of which is currently in abeyance) and the School of Clinical Medicine (25 disciplines, three of which had no registrars enrolled at the time of the study).
The Health Professions Council of SA (HPCSA) accredited training platforms for specialist training in the Free State are Universitas Academic Hospital, Pelonomi Academic Hospital, National Hospital, the Free State Psychiatric Complex and 3 Military Hospital in Bloemfontein, as well as Robert Mangaliso Sobukwe Hospital in Kimberley in the neighbouring Northern Cape Province. All training is performed in public hospitals.
Participant selection
MMed students (registrars) from all disciplines and registered as postgraduate students in the Faculty of Health Sciences were eligible to participate in the survey.
Measurement
A questionnaire was designed by the researchers (Appendix: https://www.samedical.org/file/1809) considering the requirements set for MMed training by the different stakeholders in medical specialist training, namely the training institution (UFS), the registration body (HPCSA), the examining body (CMSA) and the employers of the registrars (e.g. the Free State Province Department of Health or the National Health Laboratory Service (NHLS)). The researchers represent various elements of MMed training in the institution, namely the head of the School of Clinical Medicine (NM), MMed research co-ordinator (CM), research methodology module leader (GJ) and clinical research director (CB). Based on their experience in MMed training, the questionnaire was face-validated by the researchers. A pilot study was not performed.
The Postgraduate Office of the Faculty of Health Sciences sent an email requesting participation to all registrars, with a link to the information document and questionnaire, on 14 June 2020, followed by two reminder emails before closing on 30 June 2020. The questionnaire could be completed within 10 minutes on various electronic devices. Participation was voluntary and anonymous.
All data from the questionnaire were automatically captured via the REDcap (Research Electronic Data Capture; Vanderbilt University, USA) survey software hosted at the UFS.
Statistical analysis
Statistical analysis was performed by the Department of Biostatistics, Faculty of Health Sciences, UFS, using the statistical analysis software package SAS/ STAT version 9.4 (SAS Institute Inc., USA). Results were summarised by frequencies and percentages (categorical variables) and means and standard deviations or percentiles (numerical variables). Associations between categorical variables were analysed using x2, or Fisher's exact test in the case of sparse cells. Qualitative data obtained from responses to the open-ended question were analysed by thematic analyses.
Ethical considerations
Approval to perform the study was obtained from the heads of the Schools of Pathology (SoP) and Clinical Medicine (SoCM), and the dean of the Faculty of Health Sciences. The study was approved by the Health Sciences Research Ethics Committee (ref. no. UFS-HSD2020/1029/30006) and the vice-rector: research, UFS.
Results
The questionnaire was distributed to all 258 registrars registered in the SoCM (n=238) and the SoP (n=20) at the time of the survey. In total, 134 responses were received (51.9% response rate), with 118 responses, representing 45.7% of the registrars at the UFS, included in the analysis. Sixteen incomplete questionnaires were excluded. Response rates of 43.3% (n=103/238) and 60.0% (n=12/20) were obtained from the SoCM and the SoP, respectively. Three respondents did not indicate their department of registration.
Demographic and health profile of registrars at the UFS
Table 1 summarises the demographic data of the participants compared with the total UFS registrar population. A similar number of male (49.6%) and female (50.4%) respondents participated in the survey. More than half of the respondents (51.7%) were 30 - 34 years of age, and 28.3% were in their second year of study. Extension of residency time was reported by 12.0% (n=9/75) of registrars in a 4-year programme, none (n=0/6) in a 4.5-year-programme and 6.3% (n=2/32) in a 5-year programme.
The majority of the respondents (74.1%) were married, living together or had a life partner. The median number of people living in the household was 3 (range 1 - 10). One-fifth (20.5%) of the respondents resided alone. At the time of the survey, the majority of the respondents (98.2%) were not living with a person who had been diagnosed with COVID-19, while 2 (1.8%) had family members awaiting results. Slightly more than a quarter (26.9%) of respondents reported changes in their domestic circumstances that had an effect on the progress of their MMed research, with 38.0% reporting that an adult in their household had been retrenched or suffered a salary reduction.
The health profile of respondents relative to COVID-19, their psychiatric history and psychological response to COVID-19 are summarised in Table 2. Approximately 60% (n=70; 59.3%) of respondents had no underlying comorbidities regarded as poor prognostic factors for COVID-19, 11 (9.3%) respondents did not select any of the options, leaving one-third (n=37; 31.3%) of respondents who reported comorbidities. A body mass index >30 kg/m2 and hypertension were reported by 14.8% and 13.0% of respondents, respectively, while two or more poor prognostic factors were reported by 12.2% (n=14/115) of respondents.
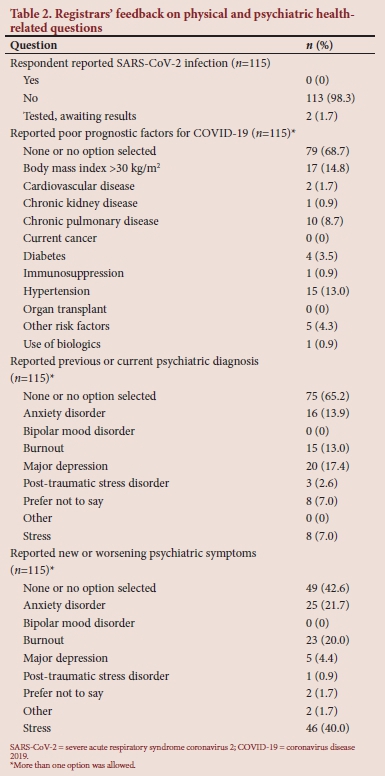
As shown in Table 2, 57.4% of respondents reported no previous or current psychiatric diagnosis, while some chose not to disclose a psychiatric diagnosis or did not select any option (7.0% and 7.8%, respectively). Major depression, anxiety disorder and burnout were reported by a number of respondents: 17.4%, 13.9% and 13.0%, respectively, while 19.6% (n=21/107) had two or more concomitant psychiatric diagnoses. No new psychiatric diagnosis or worsening of psychiatric symptoms was reported by 39.1% of respondents, while some respondents preferred not to indicate which psychiatric symptoms worsened, selected 'other', or did not answer the question (1.7%, 1.7% and 7.8%, respectively). Worsening or new symptoms of stress were reported most frequently (40.0%). More than one new psychiatric symptom or worsening of psychiatric symptoms was reported by 18.3% (n=21/115) of respondents, and 22.1% (n=25/113) experienced worsening of two or more psychiatric symptoms.
Effect of the lockdown on MMed research progress
The respondents' feedback related to the effect of the lockdown on their MMed research progress is summarised in Table 3.
The vast majority of respondents had completed the research methodology module (89.9%), but 46.2% had not yet obtained final institutional ethics committee approval for their research protocols. Nearly a quarter of the respondents who were >24 months into the programme (23.3%; n=14/60) had missed the milestone of obtaining institutional ethics approval by 24 months of residency time. Sixty-seven (57.3%) of 117 respondents reported doing retrospective data collection. A fifth (n=9/41; 22.0%) of respondents who conducted prospective studies were in the data collection phase at the time of the survey. With regard to the registrars on extension of residency time, 5 had not yet completed their research, 1 reported preparing a protocol, 1 reported being in the process of collecting data and 3 were writing the final research report.
In terms of the effect of the COVID-19 lockdown on time available to spend on MMed research, 46.5% of respondents reported no change. However, 27.1% of respondents reported that they had less time, and 9.7% reported that they had no time to work on MMed research. With reference to adhering to the UFS milestones for MMed research, 49.6% of the respondents reported that the lockdown had affected their ability to comply with the requirements, while 25.7% reported no effect on compliance.
Specific challenges related to their MMed research were reported by a notable number of respondents. Sixty-three (53.4%) respondents reported increased domestic duties due to lockdown, while psychological effects of working during the COVID-19 pandemic and the clinical workload related to COVID-19 were reported by 43.2% and 35.6%, respectively. Approximately one-third (31.4%) reported challenges with caring for and schooling children at home. Other challenges included restricted access to the library/librarian (27.1%), problems with access to patients or data (14.4%) and difficulties presenting the research proposal at a departmental research meeting (11.0%).
Forty-two participants responded to an open-ended question pertaining to challenges experienced during the lockdown. Themes that emerged were challenges regarding research and academic activities (35.7% of those responding to this question), challenges regarding the clinical working environment (7.1%), responsibilities towards children (47.6%), increased domestic responsibilities (42.9%) and emotional (14.3%) and financial challenges (9.5%).
Effect of the lockdown on postgraduate academic activities and the clinical training environment
The effects of the lockdown on postgraduate academic activities and the clinical training environment are summarised in Table 4. Only 8.6% reported that face-to-face academic meetings continued, while the use of electronic platforms only or a combination of electronic and face-to-face academic meetings was reported by 48.7% and 18.0%, respectively. Cancelling of all academic meetings was reported by 24.8% of respondents. In terms of the frequency of postgraduate academic meetings, 50.9% of respondents reported a decrease in the number of meetings, while 24.1% reported that no meetings took place.
Regarding the effect of lockdown on self-directed learning time, similar numbers of respondents reported that less time (37.1%) or more time (35.3%) was available. Two-thirds of respondents reported that the lockdown affected their ability to comply with the CMSA logbook, clinical rotations and clinical exposure.
Half of the respondents reported that they felt adequately prepared and trained to work in the frontline of the COVID-19 pandemic. It was noteworthy that 45.2% of respondents reported a decrease in their day-to-day clinical workload and activities, while 27.8% reported no change in workload. With regard to after-hours workload and activities, 38.3% of respondents reported unchanged conditions. A similar number (37.4%) reported an increase in their after-hours workload.
Slightly more than half of the respondents (51.3%) reported that they were part of a COVID-19 task team or involved in COVID-19 clinical work. The vast majority of respondents (74.6%) reported anxiety when nominated to a COVID-19 task team or when performing COVID-19 clinical work, although only 30.1% reported having direct contact with COVID-19 patients in the clinical environment. Most respondents (84.4%) expressed concern about infecting family members owing to the nature of the clinical training environment.
Most (n=80/116; 69.0%) respondents were satisfied with the communication received from the UFS Faculty of Health Sciences postgraduate administration office regarding studies and research, while 40.0% (n=46/115) were satisfied with the communication received from the Free State Province Department of Health and their respective departments about clinical workload and wellbeing.
Table 5 shows the association between the responses regarding the effects of COVID-19 lockdown on day-to-day clinical work, being seconded to a COVID-19 task team or requested to work with COVID-19 patients, and changed circumstances at home that affected MMed research progress on the one hand, and responses regarding the ability to perform certain MMed-related tasks on the other. A significant association was noted between the effect of the COVID-19 lockdown on day-to-day clinical work and how the ability to work on MMed research was affected (p<0.01), with those with an increased workload being more likely to report less time to work on MMed research and self-directed learning time (p<0.01). No association between changes in the day-to-day clinical workload and ability to adhere to MMed milestones (p=0.20) was found.
Increased day-to-day clinical workload and being seconded to a COVID-19 task team or requested to work with COVID-19-positive patients were both reported to affect registrars' ability to comply with the requirements of the CMSA logbook, clinical rotations and clinical exposure (p=0.04 and p=0.02, respectively). No association was noted between being seconded to a task team or requested to work with COVID-19 patients and the ability to work on MMed research (p=0.76), the ability to adhere to the milestones for MMed research (p=0.77) or self-directed learning time (p=0.26). Registrars who experienced lockdown-related changes in domestic circumstances that affected MMed research progress were more likely to report less or no time for research (p<0.01), and an inability to adhere to MMed research milestones (p<0.01).
The frequency of departmental meetings was not associated with day-to-day clinical workload, after-hours workload or being seconded to a task team or requested to work with COVID-19-positive patients.
Among the respondents who had been seconded to a COVID-19 task team or requested to work with COVID-19-positive patients, an association was noted between feeling inadequately prepared and trained to work on the frontline of the pandemic and experiencing anxiety when requested to work with COVID-19-positive patients. Of the respondents who reported that they were adequately prepared and trained to work on the frontline of the pandemic, approximately two-thirds (62.5%) nonetheless reported anxiety when requested to work with COVID-19 patients, compared with 88.9% of those who reported that they did not feel adequately prepared and trained (p=0.02).
Discussion
This study showed that the initial months of the COVID-19 lockdown affected registrars' MMed research progress, postgraduate academic activities and the clinical training environment. The most notable health concern was an increase in the incidence and worsening of self-reported stress.
The response rate for this questionnaire was similar to a previously published study sampling registrars in SA.[7] Departments with the highest percentage of responses in both the SoP and the SoCM were in line with the departmental size.
The self-reported prevalence of obesity and hypertension was lower than that of the general SA population[8] and healthcare workers in Limpopo Province.[9] The prevalence of burnout among respondents was markedly lower than previously reported.[10-14] Compared with medical students and medical doctors, fewer respondents reported depression[11,15] and anxiety disorder.[15] Under-recognition of burnout, depression and anxiety among registrars might have contributed to the low prevalence of burnout in our study.
Although it was alarming that 40% of respondents experienced worsening of stress so early in the pandemic, the reported stress was lower than COVID-19-related stress levels experienced by the general SA population, which increased by 56% between the start of the pandemic and mid-October 2020.[16] Healthcare workers, including registrars, working on the frontline of the COVID-19 pandemic experience symptoms of depression, anxiety, insomnia, distress, fear for family, friends and co-workers and fear of infecting people at home. Concerns about the discomfort of isolation, resource allocation and availability of personal protective equipment have been raised by healthcare workers both locally and abroad.[17-20] Many of these concerns were echoed in our findings.
Despite satisfactory interaction among registrars, the postgraduate office and clinical departments, psychological support was lacking. Screening for burnout and psychological symptoms is a necessary intervention that should be considered when facing global disease outbreaks. The present study was not designed to identify the causes and contributing factors for psychiatric conditions.
The tension between the dual role of healthcare worker and student in the COVID-19 era has recently highlighted the challenge of balancing priorities of patient care and training, including access to surgical cases and clinical exposure.[3,21] The reduced clinical caseload has caused some training programmes to change their didactic, surgical and clinical education to accommodate the consequences of the pandemic, while at the same time, institutions have been rethinking their assessment and graduation requirements.[6,22-26] In light of the COVID-19 pandemic, the senate of the CMSA, the examining body for specialist medical qualifications in SA, announced the postponement of oral/clinical/practical examinations of the first semester of 2020 to the second semester of 2020.[27] While the HPCSA has given guidance on how undergraduate medical training could continue during the COVID-19 pandemic, they failed to provide input on the management of postgraduate training, with the exception of a general announcement that practitioners were expected to continuously update their professional knowledge and skills to effectively manage patients in the context of the pandemic and other health conditions of public health importance.[28]
At a media briefing on 14 May 2020, Higher Education Minister Blade Nzimande announced that ''[f]rom 1 June 2020, all institutions would offer forms of remote multimodal flexible teaching and learning, supported by approved resourced plans.'[29] Remote multimodal teaching has certain shortcomings, and especially does not address all the needs of clinical training and the current requirements for logbooks, as stipulated by the CMSA. COVID-19 has prompted educational transformation and stimulated the debate on work-based assessment by the CMSA and identification of entrustable professional activities in SA, which could be regarded as positive outcomes of the pandemic.
COVID-19 and the lockdown may well affect timeous completion of residency for many registrars, given the large number who reported that lockdown affected CMSA logbook requirements, clinical rotations and experience, and the reduction or cancellation of academic meetings. These factors may have far-reaching implications. In the Free State Province, registrar employment contracts expire at the end of the allocated residency time. Consequently, registrars who do not complete their residency within the stipulated time may be left insufficiently prepared for examinations, as well as unemployed. Registrars likely to be most affected were those who were already behind their first milestone (obtaining final ethics committee approval for the research component of the MMed by 24 months) early in the pandemic, which represents 23.3% of the respondents in this cohort.
Various other factors should be considered when deciding on extension of residency time. It is important to identify registrars who experienced a higher day-to-day clinical workload due to the COVID-19 lockdown. Their increased workload affected both the ability to work on their MMed research and their self-directed learning time. Both increased day-to-day clinical work and being seconded to a task team or requested to work with COVID-19-positive patients affected registrars' ability to comply with CMSA logbook requirements, clinical exposure and rotations. Conversely, the lockdown resulted in cancellation of elective surgeries and significant reductions in both non-trauma- and trauma-related surgical admissions in the initial month of the lockdown (27 March - 30 April 2020), which might further affect registrars' ability to comply with logbook requirements.[3,30]
It is concerning that over a quarter of registrars experienced changes in domestic circumstances that affected their MMed research, significantly associated with no or decreased time to do research, resulting in non-adherence to the required milestones. Such challenges may have had far-reaching consequences on the demand for registrars' time, and may further affect their academic progress. Considering these factors, the UFS and the Free State Department of Health (FSDoH) made provision for the extension of residency time for several registrars. At this stage, the long-term impact of extending residency time on the institution and the country is unclear.
From what we have learnt from the effects of the initial months of the COVID-19 lockdown, we recommend that departments frequently monitor individual registrars' clinical exposure, logbook requirements, portfolio of learning, academic milestones and research progress. This will allow for informed decisions on timeous and appropriate interventions. In line with how adult postgraduate training should be structured, learning through feedback and reflection is especially relevant to mitigate delayed academic progress during the COVID-19 pandemic. 'Modernised' workplace-based assessment (WPBA) and feedback are strong tools in the MMed training armamentarium to evaluate individual registrar progress to inform appropriate remedial actions.[31,32] The importance of WPBA, as well as the supporting role of the clinical supervisor and mentor during this time, cannot be overemphasised.
In order to support registrar research during the lockdown, we recommend frequent departmental research meetings, scheduled supervisor-student consultations and targeted remedial interventions where necessary. All of these actions are easy to implement on a virtual platform. Structured mentoring programmes, which have been shown to be useful in improving research productivity and clinical skill advancement, may also benefit registrars.[33]
The COVID-19 lockdown has not only affected training and research, but also examinations. The CMSA postponed the 2020 first semester clinical examinations, as well as the second semester 2020 examinations. In light of this and the aforementioned factors, the training institution (UFS) and employers (FSDoH and NHLS) were required to make provision for extension of residency time. Long-term sequelae of the COVID-19 pandemic may make it necessary for universities, the CMSA and the HPCSA to review the minimum duration of MMed courses in order for registrars to fulfil the requirements for clinical experience and to complete their research.
Our study highlights the need to invest in registrar wellness. Registrars who suffer psychological consequences of the pandemic should be referred to the appropriate staff/registrar wellness programmes. A registrar wellness programme should be established in collaboration between the training institution, the employer and trainees, with interventions both at organisational and individual level. Establishment of a registrar wellness programme will require dedicated leadership, a wellness committee, regular needs assessments, assessment of trainee wellness, targeted interventions and regular reassessment.[34]
Although the present study did not investigate the role of peer support, it is acknowledged as an important aspect of resident support. Peer support groups are easy to implement and require minimal resources. 'Ice-cream rounds' (ICRs)[35] have been implemented in some Canadian institutions where trainees can discuss their work challenges and offer support with the aim of building resilience. ICRs have been shown to normalise challenges in medical training, decrease stress, reduce feelings of burnout and anxiety and improve collegiality between students, and can also be hosted virtually.[36-39] Departments should capitalise on the important role that peer support can play in specialist training and research. Further research to determine the causes and extent of the psychosocial stressors of registrars during the pandemic may identify other targeted interventions.
We acknowledge that registrars who were adversely affected by the lockdown might not have had or made time to complete the questionnaire.
Conversely, it could be argued that those who did complete the questionnaire might have used it as an opportunity to express their concerns. We further acknowledge that the respondent population was not entirely similar to the UFS registrar population, with a higher percentage of female respondents and a slight over-representation of respondents from younger age groups. Departments with the highest percentage of responses in both the SoP and the SoCM were in line with the departmental size. A limitation of the study was that it did not investigate the role of the clinical supervisor and mentor or peer-registrar support in the workplace during the initial months of the COVID-19 lockdown. This support/lack of support could thus not be reported on. Furthermore, we did not investigate the challenges that supervisors might have encountered during this time, which also warrants further investigation.
Conclusion
The impact of the initial months of the COVID-19 lockdown may have far-reaching implications on registrars' academic progress at the UFS. Registrars reported significant disruptions in clinical training, classroom teaching and MMed research progress that may impair their academic progress. The initial months of the COVID-19 lockdown also had an adverse psychosocial impact on registrars and their families, which may further impede their MMed research and academic progress.
Declaration. None.
Acknowledgements. The authors acknowledge the registrars who participated in this study despite the difficult time that they experienced due to the COVID-19 pandemic, and Dr Daleen Struwig, medical writer/editor, Faculty of Health Sciences, UFS, for technical and editorial preparation of the manuscript.
Author contributions. CM, CB, GJ and NM were jointly responsible for the development of the protocol, data collection and writing of the manuscript. GJ was responsible for the statistical analysis of data. All the authors approved the final version of the article.
Funding. None.
Conflicts of interest. None.
References
1. National Institute for Communicable Diseases. Coronavirus disease 2019 (COVID-19) caused by a novel coronavirus (SARS-CoV-2): Guidelines for case-finding, diagnosis, management and public health response in South Africa. https://www.nicd.ac.za/wp-content/uploads/2020/03/NICD_DoH_COVID-19_Guidelines_8_March_2020_finalpdf (accessed 26 October 2020). [ Links ]
2. South Africa. COVID-19/novel coronavirus. https://www.gov.za/Coronaviru (accessed 26 October 2020). [ Links ]
3. Al-Benna S. Impact of COVID-19 on surgical registrars' education and training. S Afr J Surg 2020;58(2):55-58. https://doi.org/10.17159/2078-5151/2020/v58n2a3323 [ Links ]
4. Staff Reporter. 240 healthcare workers have died from COVID-19 in SA, infection rate 5%. Independent Online, 13 August 2020. https://www.iol.co.za/news/south-africa/240-healthcare-workers-have-died-from-covid-19-in-sa-infection-rate-5-1954db22-d379-4aac-b1c6-01864a27848c (accessed 26 October 2020). [ Links ]
5. University of the Free State. Faculty of Health Sciences. Rule book: Postgraduate degrees and diplomas, 2020. https://apps.ufs.ac.za/dl/yearbooks/353_yearbook_eng.pdf (accessed 26 October 2020). [ Links ]
6. Schwartz AM, Wilson JM, Boden SD, Moore TJ Jr, Bradbury TL Jr, Fletcher ND. Managing resident workforce and education during the COVID-19 pandemic: Evolving strategies and lessons learned. J Bone Joint Surg 2020;5(2):e0045. https://doi.org/10.2106/JBJS.OA.20.00045 [ Links ]
7. Patel N, Naidoo P, Smith M, Loveland J, Govender T, Klopper J. South African surgical registrar perceptions of the research project component of training: Hope for the future? S Afr Med J 2016;106(2):169-171. https://doi.org/10.7196/SAMJ.2016.v106i2.10310 [ Links ]
8. Shisana O, Labadarios D, Rehle T, et al. The South African National Health and Nutrition Examination Survey, 2012: SANHANES-1: The Health and Nutritional Status of a Nation. Pretoria: HSRC Press, 2014. http://www.hsrc.ac.za/en/research-outputs/view/6493 (accessed 26 October 2020). [ Links ]
9. Skaal L, Pengpid S. Obesity and health problems among South African healthcare workers: Do healthcare workers take care of themselves? S Afr Fam Pract 2011;53(6):563-567. https://doi.org/10.1080/20786204.2011.10874153 [ Links ]
10. Zeijlemaker C, Moosa S. The prevalence of burnout among registrars in the School of Clinical Medicine at the University of the Witwatersrand, Johannesburg, South Africa. S Afr Med J 2019;109(9):668-672. https://doi.org/10.7196/SAMJ.2019.v109i9.13667 [ Links ]
11. Rossouw L, Seedat S, Emsley RA, Suliman S, Hagemeister D. The prevalence of burnout and depression in medical doctors working in the Cape Town Metropolitan Municipality community healthcare clinics and district hospitals of the Provincial Government of the Western Cape: A cross-sectional study. S Afr Fam Pract 2013;55(6):567-573. https://doi.org/10.1080/20786204.2013.10874418 [ Links ]
12. Sirsawy U, Steinberg WJ, Raubenheimer JE. Levels of burnout among registrars and medical officers working at Bloemfontein public healthcare facilities in 2013. S Afr Fam Pract 2016;58(6):213-218. https://doi.org/10.1080/20786190.2016.1198088 [ Links ]
13. Ishak WW, Lederer S, Mandili C, et al Burnout during residency training: A literature review. J Grad Med Educ 2009;1(2):236-242. https://doi.org/10.4300/JGME-D-09-00054. [ Links ]!
14. Liebenberg AR, Coetzee JF Jr, Conradie HH, Coetzee JF. Burnout among rural hospital doctors in the Western Cape: Comparison with previous South African studies. Afr J Prim Health Care Fam Med 2018;10(1):1568. https://doi.org/10.4102/phcfm.v10i1.1568 [ Links ]
15. Van der Walt S, Mabase W, Davids E, de Vries P. The burden of depression and anxiety among medical students in South Africa: A cross-sectional survey at the University of Cape Town. S Afr Med J 2019;110(1):69-76. https://doi.org/10.7196/SAMJ.2019.v110i1.14151 [ Links ]
16. Medical Brief. Survey: SA's stress levels up by 56% since start of pandemic. Medical Brief, 14 October 2020. https://www.medicalbrief.co.za/archives/survey-sas-stress-levels-up-by-56-since-start-of-pandem (accessed 26 October 2020). [ Links ]
17. Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3(3):e203976. https://doi.org/10.1001/jamanetworkopen.2020.3976 [ Links ]
18. Tan BYQ, Chew NWS, Lee GKH, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med 2020;173(4):317-320. https://doi.org/10.7326/M20-1083 [ Links ]
19. Gallagher TH, Schleyer AM. "We signed up for this!' - student and trainee responses to the COVID-19 pandemic. N Engl J Med 2020;382(25):e96. https://doi.org/10.1056/NEJMp2005234 [ Links ]
20. Pilane P. Health workers afraid of passing COVID to family. Mail & Guardian, 6 August 2020. https://mg.co.za/health/2020-08-06-health-workers-afraid-of-passing-covid-to-family/ (accessed 26 October 2020). [ Links ]
21. Bambakidis NC, Tomei KL. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg 2020;133(1):10. https://doi.org/10.3171/2020.3JNS20965 [ Links ]
22. Warhadpande S, Khaja MS, Sabri SS. The impact of COVID-19 on interventional radiology training programs: What you need to know. Acad Radiol 2020;27(6):868-871. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/en/covidwho-12556- (accessed 26 October 2020). [ Links ]
23. England E, Kanfi A, Flink C, et al. Radiology residency program management in the COVID era - strategy and reality. Acad Radiol 2020;27(8):1140-1146. https://search.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/en/covidwho-279400 (accessed 26 October 2020). [ Links ]
24. Rosen GH, Murray KS, Greene KL, Pruthi RS, Richstone L, Mirza M. Effect of COVID-19 on urology residency training: A nationwide survey of program directors by the Society of Academic Urologists. J Urol 2020;204(5):1039-1045. https://doi.org/10.1097/JU.0000000000001155 [ Links ]
25. Goldhamer MEJ, Pusic MV, Co JPT, Weinstein DF. Can COVID catalyze an educational transformation? Competency-based advancement in a crisis. N Engl J Med 2020;383(11):1003-1005. https://doi.org/10.1056/NEJMp2018570 [ Links ]
26. Kealey A, Alam F, McCreath G, Matava CT, Bahrey LA, Walsh CM. Real-world impact of COVID-19 pandemic on the assessment of anaesthesiology residents. Br J Anaesth 2020;125(5):e430-e432. https://doi.org/10.1016/j.bja.2020.08.016 [ Links ]
27. Colleges of Medicine of South Africa. Announcement to candidates (COVID-19). Announcement by the President of the CMSA: COVID-19 and the 2020 first semester clinical/oral/practical, fellowship, subspecialty and diploma examinations. https://cmsa.co.za/view_news_item.aspx?NewsID=1 (accessed 26 October 2020). [ Links ]
28. Health Professions Council of South Africa. COVID-19 outbreak in South Africa: guidance to health practitioners. Pretoria: HPCSA, 2020. https://www.hpcsa.co.za/Uploads/Events/Announcements/HPCSA_COVID-19_guidelines_FINAL.pdf (accessed 26 October 2020). [ Links ]
29. Parlimentary Monitoring Group. Minister on Plans to Save 2020 Academic Year; DHET 2020/21 Annual Performance Plan. Pretoria: PMG, 2020. https://pmg.org.za/committee-meeting/30224/ (accessed 26 October 2020). [ Links ]
30. Moustakis J, Piperidis AA, Ogunrombi AB. The effect of COVID-19 on essential surgical admissions in South Africa: A retrospective observational analysis of admissions before and during lockdown at a tertiary healthcare complex. S Afr Med J 2020;110(9):910-915. https://doi.org/10.7196/SAMJ.2020.v110i9.15025 [ Links ]
31. Sathekge MM. Work-based assessment: A critical element of specialist medical training. S Afr Med J 2017;107(9):728. https://doi.org/10.7196/SAMJ.2017.v107i9.12655 [ Links ]
32. Sathekge M. Time to review the contribution of work-based assessment in our high-stakes exams. Trans J Coll Med S Afr 2017;61(1):4-5 https://www.cmsa.co.za/view_document_list.aspx?Keyword=Transactions (accessed 11 March 2021). [ Links ]
33. Caruso TJ, Kung T, Piro N, Li J, Katznelson L, Dohn A. A sustainable and effective mentorship model for graduate medical education programs. J Grad Med Educ 2019;11(2):221-225. https://doi.org/10.4300/JGME-D-18-00650.2 [ Links ]
34. Sharp M, Burkart KM. Trainee wellness: Why it matters, and how to promote it. Ann Am Thorac Soc 2017;14(4):505-512. https://doi.org/10.1513/AnnalsATS.201612-1006PS [ Links ]
35. McGill University, Faculty of Medicine and Health Sciences. The WELL Office. Ice cream rounds. https://www.mcgill.ca/thewelloffice/our-services/pgme/wellness-support/wellness-curriculum/ice-cream-rounds (accessed 11 March 2021). [ Links ]
36. University of British Columbia, Faculty of Medicine. Postgraduate medical education. Ice cream rounds: What it is and how to bring it to your program. https://med-fom-pgme.sites.olt.ubc.ca/2017/01/17/ice-cream-rounds-what-it-is-and-how-to-bring-it-to-your-program/ (accessed 11 March 2021). [ Links ]
37. Calder-Sprackman S, Kumar T, Gerin-Lajoie C, Kilvert M, Sampsel K. Ice cream rounds: The adaptation, implementation, and evaluation of a peer-support wellness rounds in an emergency medicine resident training program. Can J Emerg Med 2018;20(5):777-780. https://doi.org/10.1017/cem.2018.381 [ Links ]
38. Hiranandani R, Calder-Sprackman S. Ice cream rounds: The implementation ofpeer support debriefing sessions at a Canadian medical school. Can Med Educ J 2020;11(4):e87-e89. https://doi.org/10.36834/cmej.69253 [ Links ]
39. Kearney H, Lukings J. Virtual ice cream rounds: Addressing medical clerk wellness during COVID-19. Can Med Educ J 2020;11(5):e84-e86. https://doi.org/10.36834/cmej.70251 [ Links ]
 Correspondence:
Correspondence:
C Meyer
meyerc@ufs.ac.za
Accepted 5 May 2021














