Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.14 n.2 Pretoria Jun. 2022
http://dx.doi.org/10.7196/ajhpe.2022.v14i1.1482
RESEARCH
Undergraduate dental students' perspectives on teaching and learning during the COVID-19 pandemic: Results from an online survey conducted at a South African university using a mixed-methods approach
R Moodley; S Singh; I Moodley
PhD; Discipline of Dentistry, School of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: Many institutions of higher education transitioned from classroom-based settings to remote settings as a response to the COVID-19 pandemic. However, it is unclear how undergraduate dental therapy and oral hygiene students responded to this transition in the learning environment
OBJECTIVES: To explore undergraduate dental students' knowledge, perceptions, attitudes and practices related to clinical and theory-based learning at a South African university
METHODS: A mixed-methods approach comprising a concurrent dominant status design (QUAN/qual) was used. Therefore, the study was a cross-sectional quantitative survey with descriptive qualitative data. An online, self-administered questionnaire with open- and closed-ended questions was developed to gain insights into students' knowledge, perceptions, attitudes and learning practices during the COVID-19 pandemic
RESULTS: Most respondents (n=86; 80.4%) agreed that they had the necessary skills to engage with online learning (p=0.04). Respondents in the first year (n=25; 76%), second year (n=24; 73%) and third year (n=32; 28%) were either unsure or did not agree that they understood online platform-based lectures better than classroom-based lectures. The major emergent themes included external (internet connectivity) and internal (students' coping skills) barriers to online learning
CONCLUSIONS: This study highlighted dental student challenges in embracing the blended approach of teaching and learning. While this may be a new norm for curriculum delivery, it is important to include student input in curriculum-related decision-making processes
As the COVID-19 pandemic ravaged through country-level health systems with crippling effects on world economies, new norms had to be set for social interaction and daily living. Institutions of higher education were not spared in this pandemic and centres for learning across the globe were forced to either close or opt for innovative teaching and learning platforms. Student teaching and learning were expected to continue, notwithstanding the restrictions of lockdown and social distancing measures.[1] Many higher education institutions strategised by transitioning from classroom settings to virtual platforms to facilitate learning, and thereby salvaged the 2020 academic year. However, training of health professionals, including dental professionals, is based on the union of three fundamental pillars: theory, laboratory practice and clinical practice.[1] While the theoretical aspects of a dental curriculum can be delivered through online teaching methods, clinical training is highly specialised. It is essential to acquire the basic clinical skills for competency, such as the administration of dental local anaesthesia and the restoration or extraction of a tooth, depending on the required scope of practice for the health professional.[2]
South African (SA) institutions of higher learning opted to transit to remote teaching and learning, using online platforms for most of the curriculum content, but this came with several challenges. Students' challenges included having access to electronic devices, internet access and a conducive learning environment within a family household. A further challenge with dental training was to find a balance between maintaining a safe environment for students and continuing with dental clinical practice, while reducing potential risk of infection to students and clinical staff.[3]
The move from classroom-based teaching to an online platform was made at the beginning of the pandemic. Chang et al.'s[4] study showed that all lectures, including problem-based lectures, were moved online. With SA into the second and the third wave in March/April 2021, online learning needed to continue. The researchers in the Chang et al.[4] study concluded that the COVID-19 virus had forced dental educators to revolutionise dentistry and that there was a need to develop new technology and a new model for dental education. Online and e-learning modules were popular and enhanced learning experiences.[5]
Blended learning is an approach where online learning is combined with face-to-face teaching. Given the positive feedback reported by Mehta et al.,[5] it would appear that students could be supportive of this approach to learning. While a blended learning approach was widely advocated for health sciences training in higher institutions in SA, it is unclear how undergraduate dental therapy and oral hygiene students responded to the transition in the learning environment owing to the COVID-19 pandemic. There is limited published evidence on the contextual influences on theory-based and clinical teaching in undergraduate dental training during COVID-19, as well as students' understanding and preparedness for learning during the pandemic. Such information could be critical in guiding and shaping undergraduate dental curriculum development, specifically when responding to sudden disruptions in the teaching and learning environment. It was therefore important to determine the undergraduate dental students' knowledge and attitudes towards learning during the COVID-19 pandemic. This study aimed to contribute to curriculum planning and review by determining undergraduate dental students' knowledge, attitudes and practices related to clinical and theory-based learning during COVID-19.
Methods
Research setting and context
The study was located in an institution offering undergraduate dental training in SA. There are currently two 3-year undergraduate degree programmes offered by the Discipline of Dentistry, i.e. Bachelor of Dental Therapy and Bachelor of Oral Hygiene - the latter commenced in 2020. This study was conducted at the end of the second semester in 2020. Students had therefore already been through 9 months of teaching and learning during the pandemic.
Research design
A mixed-methods approach comprising a concurrent dominant status design (QUAN/qual) was used. Therefore, the study was a cross-sectional quantitative survey with descriptive qualitative data. The online survey comprised both open- and closed-ended questions. The study examined knowledge, perceptions and practices of undergraduate dental students' learning during the COVID-19 pandemic and described their attitudes towards teaching and learning.
Participants
The study population included all full-time students registered at the Discipline of Dentistry, School of Health Sciences, University of KwaZulu-Natal, Durban, SA, for both programmes and across all 3 study levels. The total number of students registered for the 2020 academic year was 156, consisting of year 1 (n=55) (Bachelor of Dental Therapy, n=38; and Bachelor of Oral Hygiene, n=17); year 2 (n=54); and year 3 (n=47). The social media platform WhatsApp was used to recruit participants through a snowball sampling technique. An invitational message was sent to the first student to consider participation in the study. The message included a link to the informed consent documents and survey questionnaire. Once the student clicked on the link, he/she had to give consent by clicking on the relevant icon. The participant was then given a choice to complete the survey and to forward the survey link to the next student, with each participant remaining anonymous. The link remained open for ~6 weeks to allow students to participate.
Data collection and analysis
Data were collected using an online, self-administered questionnaire to gain insights into the students' knowledge, attitudes and practices towards learning during the COVID-19 pandemic. The researchers developed the data collection tool, which comprised 4 sections: section A covered student demographics; section B comprised knowledge; section C included attitudes; and section D covered practices. The questionnaire used mainly closed-ended questions, requiring Likert-scale format responses ranging from 1 (strongly agree), 2 (agree), 3 (not sure), 4 (disagree) to 5 (strongly disagree), and 2 open-ended questions to obtain qualitative data for more in-depth information. The open-ended questions included: What are the barriers that hinder online teaching? How can online teaching be improved? The questionnaire was administered in the English language, which is the medium of instruction in the undergraduate dental training programmes. All completed questionnaires were coded (e.g. P1) to maintain participant anonymity.
Data obtained from the questionnaires were captured onto an Excel spreadsheet (Microsoft Corp., USA) and analysed thereafter. The quantitative data were analysed using SPSS version 25.0 (IBM Corp., USA). Data analysis included univariate descriptive statistics such as frequency and mean distribution. An inferential statistical technique, the Pearson x2test, was used to determine a relationship between the independent variable (year of study) and the dependent variables (knowledge, attitudes and practices), with p<0.05 established as being statistically significant.
The qualitative data (obtained from the open-ended questions) were analysed using thematic analysis. The 6-step process as described by Braun and Clarke[6] was used for data analysis. The responses from each student were first transcribed verbatim. The data were coded and then organised into code groups. Each code group was further examined for patterns and emergent themes. Two members of the research team coded the data and explored the emergent themes independently. Thereafter, both members compared their findings and finalised the main themes and sub-themes together. Confirmability was established by quoting the actual responses of students.[6] Reliability/validity was achieved by conducting a pilot study among 5 first-year students. These data were not included in the final study. Confirmability was maintained by all 3 researchers, who ensured that the data received were from the participants. Dependability was achieved by all 3 researchers, who compared the data for accuracy. Credibility was maintained by the use of scientifically validated data collection methods, while transferability was established through the descriptions of the location of the study, sampling, time frame and data analysis. These descriptions could contribute to its application in other contexts.
Ethical approval
Ethical approval was received from the Humanities and Social Sciences Research Ethics Committee, University of KwaZulu-Natal (ref. no. HSSREC/00001601/2020) and gatekeeper permission was obtained prior to commencement of this study.
Results
There was a total of 111 participants in the study, with a response rate of 70.5%. More than half of the study population were female (n=72; 68%), while 1.9% (n=2) preferred not to disclose their identity. Ninety percent (n=97) of participants were registered for the dental therapy programme. There was almost an equal number of respondents over the 3 years of study: year 1 (n=33; 30.8%), year 2 (n=33; 30.8%) and year 3 (n=41; 38.3%).
Quantitative data analysis
Knowledge and perceptions towards learning
The majority of respondents (n=88; 82.2%) understood blended learning to be a combination of online lectures, face-to-face contact and self-study (Table 1). Only 11 first-year students (10.3%) and 6 second-year students (5.6%) did not agree or were unsure.
Most respondents (n=86; 80.4%) agreed that they had the necessary skills to engage with online learning and videos (p=0.04). Thirty first-year students (90%), 28 second-year students (85%) and 38 third-year students (93%) agreed that procedural videos and live demonstrations were better to understand than online learning.
The majority of respondents agreed that online learning had prepared them to take charge of their learning process (n=84; 78.5%). A significant statistical association was seen between participants' online learning preparedness to take charge of learning and having the necessary skills to engage with online learning (p=0.00).
In response to whether online learning helped them to engage better with other students in their class, only 7 third-year students (17%), 12 second-year students (36%) and 14 first-year students (42%) agreed.
Attitudes towards learning
There were varied responses to perceived support from peers during the lockdown. About 18 first-year students (55%), 15 second-year students (45%) and 25 third-year students (61%) indicated that peer support was available. The results suggested that more peer support occurred in the third year of study. The majority of respondents across all 3 years of study (first year (n=25; 76%), second year (n=24; 73%) and third year (n=32; 28%)) were either unsure or did not agree that they understood online platform-based lectures better than classroom-based lectures.
The results show that online learning was a significant stressor across all 3 years, with the majority of students agreeing (first year (n=22; 67%), second year (n=20; 61%) and third year (n=30; 73%)).
Most of the students (n=78; 73%) were concerned that they would transmit the virus to their family after patient contact. The majority of respondents (first year (n=27; 82%), second year (n=28; 85%) and third year (n=37; 90%)) agreed with the statement: 'I hope that COVID-19 would go away so that teaching and learning at university will return to the way it was.'
Learning practices
Participants agreed the student-teacher contact time was decreased during the pandemic (n=81; 76%). Respondents also agreed that they could not engage fully with online learning because of their home responsibilities (n=73; 68%). There was a significant association between gender and engagement with online learning due to home responsibilities (p=0.04).
Students agreed on the importance of maintaining social distancing in any student-related group activity (n=99; 93%). Maintaining social distancing in a group activity could be related to being worried about transmitting the virus to family from patients, staff and students (p=0.01). Almost half of the respondents were in their first year (n=18; 55%) and second year (n=19; 58%), while 41% of third-year students (n=17) agreed that they did not socialise with their friends owing to COVID-19.
Qualitative data analysis
What are the barriers that hinder online teaching?
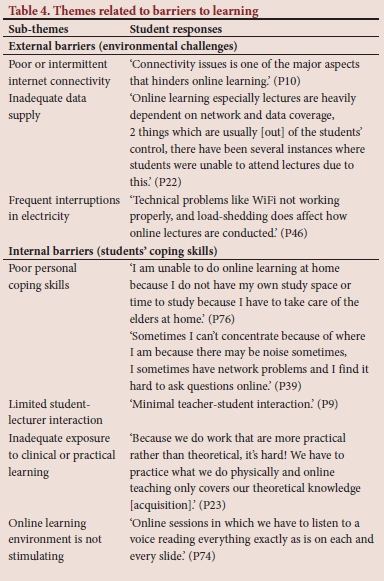
The major themes emerging from data analysis were related to external (environmental challenges) and internal barriers (students' coping skills) to online student learning. The external barriers highlighted the extent to which poor or intermittent internet connectivity, inadequate data supply and frequent interruptions in electricity supply (as a result of ongoing power cuts or load shedding) impacted on undergraduate learning in the identified study sample.
The change in the learning environment during the lockdown period, where students were sent back home, also seemed to have impacted on the learning environment. Respondents reported being distracted at home, but more importantly, they were required to contribute to household chores. This task-shifting compounded the distraction; the home environment was therefore not conducive to learning (Table 2).
Concurrently, respondents reported poor personal coping skills that could be construed as an internal barrier to online learning. These included poor concentration during online lectures, limited student-lecturer interaction and lack of peer-assisted support in learning.
From a clinical skills development perspective, respondents pointed out that online learning failed to address the acquisition of clinical or practical skills adequately. An exclusive focus on the online training platform without any exposure to the clinical or practical environment meant that respondents were not sufficiently trained for the translation of theory into clinical practice. This was seen as a significant limitation of focusing only on online teaching in the undergraduate programme (Table 3).
Another criticism of online learning was related to the delivery of lectures. Respondents suggested that the current delivery of some lectures was not conducive to a stimulating learning environment (Table 4).
How can online teaching be improved?
While respondents criticised the delivery mode of certain lecture sessions, they believed that opportunities did exist to improve and stimulate students' interest in online learning. Therefore, more effort was required from lecturers to increase and stimulate student engagement in the learning environment. Some suggestions included monitoring student attendance and finding innovative methods to create a more conducive online learning platform (Table 5). There was a reported need to reorganise the training programme so that shorter online contact sessions were held, with a more equitable distribution of learning tasks for self-directed learning, and clear instructions of the learning tasks to be conducted.
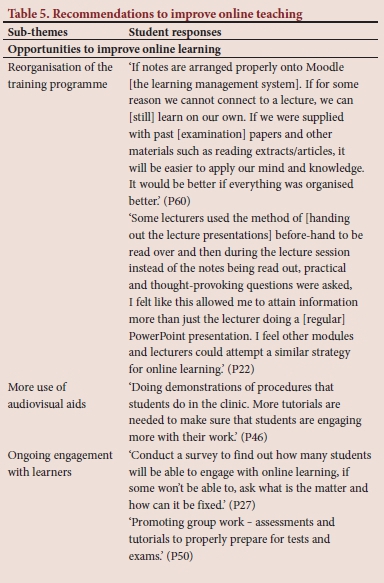
Other suggestions included the increased use of videos that could provide practical demonstration of the clinical concepts and procedures discussed. There was also a reported need for more student-lecturer interaction and the availability of recorded lectures. Respondents believed that it was necessary to consult with students to determine their readiness and coping abilities with online learning (Table 5).
As mentioned above, there was a need for more data availability and better internet connectivity, although respondents expressed awareness that challenges with internet connectivity were outside the scope of the university teaching programme.
Discussion
While respondents indicated preparedness for online learning, the majority of study participants across all 3 years of study were either unsure or did not agree that they understood the online platform-based lectures better than the classroom-based lectures. This finding is supported by other studies where students requested a repetition of the classes when the normal academic programme resumed.[7] Furthermore, only a few students in Rafi et al's[7] study supported the notion of continuing online classes once the regular classroom-based teaching was reinstated. Abbasi et al[8] reported that medical students perceived e-learning as not ideal and preferred face-to-face learning. These findings, however, are contrary to those of a study conducted in Shiraz, Iran, where a virtual learning package was found to be more effective than a lecture-based package.[9] These results suggest that the value placed on face-to-face classroom/clinical environment teaching should not be ignored, and indicate that clinical learning must consider the context-specific needs of the individual undergraduate training programme. Our study participants understood that blended learning is a combination of online lectures, face-to-face contact and self-study. As we navigate through this time, we hope that this method is carried into the future and is continued rather than reverting to traditional face-to-face methods only.
Additionally, students' learning experiences appear to be influenced by the year of study and whether the focus is on theory-based or clinical training. As part of the training programme, the final-year students are more involved in chairside learning and clinical training. Second-year students are engaged in preclinical training and clinical practice. In the final year, students are involved in restorative dentistry, minor oral surgery clinics and diagnostics clinics. The second-year students participate in restorative dentistry, minor oral surgery preclinical training and prevention dentistry clinics. There must therefore be an acute understanding of where the student is positioned in the undergraduate training programme and efforts should be put in place to support both traditionally based lectures and online learning, where applicable.[10] A hybrid approach to medical education is supported by other studies, but its effectiveness could be dependent on factors such as academic and institutional support.[11,12]
Respondents in this study emphasised the need for clinical exposure as part of the undergraduate training. This finding is supported by Hammond et al.,[1,14] who also reported that online teaching and learning cannot substitute real-world patient contact and time in the clinical environment. Additionally, YouTube links, virtual patient management and WhatsApp videos can be used to build student knowledge,[1,14] but even the most advanced technologies cannot replace chairside training.[2] Clinical teachers and students need to adapt to this changing environment and live in the 'new normal'.[2]
Students in the current study agreed that student-teacher interaction decreased with online teaching, which was consistent with the results of the Abbasi et al.[8] study, where 84% of students rated e-learning as having less student-teacher interaction. Engagement with the teacher is a dynamic process, where the students need the teacher's presence, and the teacher needs to know that the students are paying attention at the other end. In the Abbasi et al.[8] study, the students desired the interaction. Our study participants recommended that notes be uploaded on the learning channel before lectures, and a discussion and more lecturer-student interaction occur rather than a PowerPoint presentation by a lecturer. Similarly, Dumford and Miller[15] reported that participants in their study had less exposure to effective teaching methods and that lower-quality interactions were observed with online teaching. The findings therefore suggest that dental teaching staff require more support and training for improved online teaching.
This study also highlighted that, even though participants understood the importance of social distancing, they were concerned about infecting someone with the virus at home after treating patients in clinical dentistry.
These responses were further echoed in the qualitative data analysis. This analysis suggested that students struggled to cope with these changes in the physical learning environment, as indicated above. In a multi-country study, similar concerns were observed among 92% of dentists who were concerned regarding infection of their family at home.[16] COVID-19 stressors, such as difficulty to concentrate, fear, sadness, poor mental health and anxiety, could also be overwhelming for many individuals.[17]
The results of this study indicated that study participants could not engage fully in online learning because of responsibilities at home, and that the majority hoped that the 'virus would go away so that they can return to normal'. One of the themes arising from this study was that respondents indicated that lack of preparedness to deal with the changes in the learning environment could contribute to lack of confidence in self-directed learning. These study findings are consistent with those of Choi et al.,[18] who reported that 59.3% of students in their study felt less prepared and 22.7% felt less confident than before online learning. Moreover, the quality or lack of internet connectivity and frequent electricity outages threatened the connectivity viability of online learning. This finding is in contrast to that of Rafi et al.,[7] who indicated that 'network and power failure' was the main barrier facing participants in their study.
Respondents highlighted the need to be included in curriculum-related decision-making processes through the use of student surveys. This suggested a need for inclusive decision-making, where the student is also a stakeholder in undergraduate training. Therefore, inclusive planning and recognition of the duality in student roles and responsibilities are required in undergraduate training.
Interestingly, there was an inconsistency in the data. While students reported that they had adequate support during online learning, respondents further indicated that they could not engage fully with the online platform. This inconsistency may be due to under-reporting or over-reporting of data for social desirability.
Study strengths and limitations
This study provided valuable insights into online teaching and learning during the current pandemic; however, some limitations were noted. The study focused only on students' perspectives on learning during the pandemic. More research is required on dental academics' perspectives on teaching during this period. The generalisability of the findings is limited to the participating institution of higher education. The WhatsApp portal for conducting the research could have been a challenge for students who do not use this social media platform. The lack of respondent accountability in online surveys can affect the quality of the responses; therefore, questions needed to be short and unambiguous. Snowball sampling has its limitations, as the researchers have no control of the study population. Sampling bias and sample representation can be a problem with the snowballing technique. However, the researchers mitigated this challenge by sending several reminders using the invitational link for students to consider participating in the study. The response rate of 70% further suggested that adequate sample representation was obtained to answer the research question.
Conclusions
This study highlights dental student challenges when embracing the blended approach of teaching and learning. While this may be a new norm for delivery of the curriculum, the study suggests that it is important to include student input in curriculum-related decision-making processes.
Declaration. None.
Acknowledgements. The researchers would like to thank all the participants in this study.
Author contributions. RM: data collection, data analysis, interpretation of the quantitative results and manuscript preparation and writing. SS: data analysis, interpretation of the qualitative results, manuscript preparation, writing and final editing. IM: literature review, methodology, manuscript preparation and writing.
Funding. None.
Conflicts of interest. None.
References
1. Chavarria-Bolanos D, Gomez-Fernandez A, Dittel-Jimenez C, et al. E-learning in dental schools in the times of COVID-19: A review and analysis of an educational resource in times of the COVID-19 pandemic. Odovtos Int J Dental Sci 2020;22(3):69-86. https://doi.org/10.15517/ijds.2020.41813 [ Links ]
2. Sharka R, Abed H, Dziedzic A. Can undergraduate dental education be online and virtual during the COVID-19 era? Clinical training as a crucial element of practical competencies. MedEdPublish 2020;9. https://doi.org/10.15694/mep.2020.000215.1 [ Links ]
3. Iyer P, Aziz K, Ojcius DM. Impact of COVID-19 on dental education in the United States. J Dent Educ 2020;84(6):718-722. https://doi.org/10.1002/jdd.12163 [ Links ]
4. Chang T-Y, Hong G, Paganelli C, et al. Innovation of dental education during COVID-19 pandemic. J Dent Sci 2021;16(1):15-20. https://doi.org/10.1016/j.jds.2020.07.011 [ Links ]
5. Mehta S, Clarke F, Fleming P. An assessment of student experiences and learning based on a novel undergraduate e-learning resource. Br Dent J 2016;221(3):131-136. https://doi.org/10.1038/sj.bdj.2016.563 [ Links ]
6. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77-101. [ Links ]
7. Rail AM, Varghese PR, Kuttichira P. The pedagogical shift during COVID 19 pandemic: Online medical education, barriers and perceptions in central Kerala. J Med Educ Curric Dev 2020;7. https://doi.org/10.1177%2F2382120520951795 [ Links ]
8. Abbasi S, Ayoob T, Malik A, et al. Perceptions of students regarding e-learning during Covid-19 at a private medical college. Pak J Med Sci 2020;36(Suppl 4):S57-S61. https://doi.org/10.12669%2Fpjms.36.COVID19-S4.2766 [ Links ]
9. Moazami F, Bahrampour E, Azar MR, et al. Comparing two methods of education (virtual versus traditional) on learning of Iranian dental students: A post-test only design study. BMC Med Educ 2014;14(1):1-5. https://doi.org/10.1186/1472-6920-14-45 [ Links ]
10. Sheikhaboumasoudi R, Bagheri M, Hosseini SA, et al. Improving nursing students' learning outcomes in fundamentals of nursing course through combination of traditional and e-learning methods. Iran J Nurs Midwif Res 2018;23(3):217. https://doi.org/10.4103%2Fijnmr.IJNMR_79_17 [ Links ]
11. Rajab MH, Gazal AM, Alkattan K. Challenges to online medical education during the COVID-19 pandemic. Cureus 2020;12. https://doi.org/10.7759%2Fcureus.8966 [ Links ]
12. Comas-Quinn A. Learning to teach online or learning to become an online teacher: An exploration of teachers' experiences in a blended learning course. ReCALL 2011;23(3):218-232. https://doi.org/10.1017/S0958344011000152 [ Links ]
13. Hammond D, Louca C, Leeves L, et al. Undergraduate medical education and Covid-19: Engaged but abstract. Med Educ Online 2020;25:1781379. https://doi.org/10.1080/10872981.2020.1781379 [ Links ]
14. Kulkarni C, Wei KP, Le H, et al. Peer and self assessment in massive online classes. ACM Transact Comput Human Interact 2013;20(6):1-31. https://doi.org/10.1145/2505057 [ Links ]
15. Dumford AD, Miller AL. Online learning in higher education: Exploring advantages and disadvantages for engagement. J Comput High Educ 2018;30(3):452-465. https://doi.org/10.1007/s12528-018-9179-z [ Links ]
16. Ahmed MA, Jouhar R, Ahmed N, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health 2020;17(8):2821. https://doi.org/10.3390/ijerph17082821 [ Links ]
17. Centers for Disease Control and Prevention. Pandemics can be stressful. https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html (accessed 16 June 2020). [ Links ]
18. Choi B, Jegatheeswaran L, Minocha A, et al. The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: A national survey. BMC Med Educ 2020;20(1):1-11. https://doi.org/10.1186/s12909-020-02117-1 [ Links ]
 Correspondence:
Correspondence:
R Moodley
moodleyra@ukzn.ac.za
Accepted 2 August 2021














