Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.14 n.1 Pretoria Mar. 2022
http://dx.doi.org/10.7196/AJHPE.2021.v14i2.1341
RESEARCH
The lived experience of health sciences students' participation in an interprofessional community-based stroke class
M KloppersI; F BardienII; A TitusIII; J BesterIV; G Inglis-JassiemV
IM OT; Division of Occupational Therapy, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIBSc Logopaedics, M Audiology; Division of Speech, Language and Hearing Therapy, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIIM Physio; Division of Physiotherapy, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IVB OT, MPhil HE; Division of Occupational Therapy, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
VM Physio; Division of Physiotherapy, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
ABSTRACT
BACKGROUND: Collaborative approaches in healthcare contexts may provide better care for patients. Interprofessional circuit-based group therapy could counter profession-specific tribalism. There is no evidence on interprofessional education (IPE) community-based interventions on student learning in the health professions
OBJECTIVE: To explore undergraduate health sciences students' experience of being involved in community-based interprofessional circuit-based group therapy
METHODS: Semi-structured interviews were inductively analysed exploring undergraduate health sciences students' experience of involvement in an IPE community-based stroke intervention
RESULTS: A total of 12 final-year students participated, with representation from physiotherapy, occupational therapy and speech therapy. This IPE opportunity beneficially impacted students' collaborative competencies in knowledge, attitudes, skills and behaviours. This community-based rotation immersed students in a service-delivery environment where patient management was co-ordinated by a multiprofessional rehabilitation team. The integrated stroke circuit group activity aimed to enhance further interconnectedness between student participants. Students who were exposed to this clinical activity reported an understanding of (i) patients' unique contexts; (ii) role development and complementary overlap between health professions; and (iii) the value of joint interventions to both patients and rehabilitation teams in resource-constrained settings
CONCLUSION: These students have been primed in their practice-readiness as healthcare professionals for the 21st century who will promote quality care, and embrace collaborative professional practice and person-centredness
The current healthcare context requires professionals to work collaboratively to provide the best possible care.[1] Interprofessional education (IPE) is an approach that facilitates learning from, with and about one another to allow for more effective collaboration in the delivery of safe and high-quality person-centred care.[2-5] The World Health Organization framework on IPE and collaborative practice[2] suggests that exposure to IPE creates the opportunity to develop skills to join the workforce as collaborative practice-ready practitioners. Although educators may prepare health professions students to understand the roles of team members to develop their capacity to communicate outside the boundaries of their own profession,[6] offering shared learning opportunities is still a challenge in health education.[7]
People with stroke require management by an interprofessional team, owing to the related functional implications and long-term morbidity of this condition.[8,9] Mortality due to stroke has decreased, leading to more survivors with disabilities,[10] increasing the burden of care, particularly for poor people in urban and rural settings.[10] This results in a greater demand for community-based stroke rehabilitation,[11] often provided as group-based interventions.[12] These group-based interventions, often called group therapy, may involve a few patients (with similar impairment or levels of disability) who receive an exercise or education class, facilitated by a single therapist.[13] It is therefore plausible that a single therapist may be inclined to provide a more profession-specific intervention, such as a physiotherapist focusing mainly on lower-limb strengthening or balance
re-education.[12] These traditional group-based interventions provide peer support and create the opportunity for patients to interact socially. According to English et al.,[12] circuit-based interventions involve a more 'tailored intervention program, focusing on the practice of functional tasks received within a group setting [...] and could involve participants physically moving between workstations. Circuit-based interventions allow for targeting of multiple impairments and functional limitations by fewer healthcare professionals, which is ideally suited to resource-constrained environments where one is able to simultaneously address the needs of more patients. Circuit-based interventions therefore allow for intensive practice of specific exercises or functional tasks with more than two participants per therapist.[13]
The repetitive practice of functional tasks engages patients in tasks graded to suit individual needs, and encompasses group dynamics, including peer support and psychosocial benefits.[13] This approach provides a cost- and time-efficient alternative for community-based stroke rehabilitation.[14]
Interprofessional circuit-based therapy, in which different stroke rehabilitation therapists contribute to the structure and facilitation of workstations on the circuit, could be a clinical activity to counter so-called tribalism, in which professions tend to act in isolation.[15] It could also provide opportunities for mutual learning, which is a recognised need to remodel health professions education.[15] However, there is no evidence on the potential value of an interprofessional approach to community-based stroke intervention on student learning in the clinical training of healthcare professionals. This necessitated exploring the lived experiences of undergraduate health sciences students while planning and executing a community-based interprofessional functional circuit-group activity (IFCGA) during a clinical rotation.
Methods
The research was conducted at a community-based rehabilitation centre that offered individual and group rehabilitation services provided by health sciences students, including medical and dietetics students, facilitated by qualified therapists. To facilitate holistic care at this resource-constrained clinical site, an interprofessional approach for clients with stroke was sought by the managing healthcare professional team, which entailed collaborative planning and execution of stroke group classes (e.g. using single stations in a circuit class to address multiple therapeutic goals). This integrated circuit group activity was similar to the circuit class therapy proposed by English et al.[13] to save time, space and manpower. One of the adaptations included that all group members at a station (6 - 10 stroke group members) had to engage in activities that contributed toward the collaborative goals as planned by the healthcare professionals. In addition, multiple 'circuit stations' were uniquely integrated into a storyline that more closely simulated real-life situations, feeding into an overarching theme for each group class. Themes were purposely chosen based on challenges identified by members of the stroke group (e.g. grocery shopping after receiving a social grant). Storylines were developed by the healthcare professionals to target multiple impairments and functional disabilities of stroke group members (which were assessed prior to inclusion in the group class). These storylines therefore targeted multiple domain-related goals of the International Classification of Functioning[16] (body functions and structures, activity and participation) such as independence in physical shopping tasks, plus treating memory deficits by, for example, drafting a shopping list. Group members with stroke were encouraged to help each other if or when needed to closely simulate real-life scenarios (e.g. asking fellow shoppers for assistance in a busy store).
Final-year undergraduate students (speech-language and hearing, and occupational and physiotherapy) who received clinical training at this site were included in the planning and execution of the stroke group classes. The managing healthcare professionals provided an orientation session to all students where the aims and processes of the functional circuit-group class were explained. The students were allowed to self-select peers from the three different professions to form smaller groups, who were then responsible for the planning and execution of a specific station. Due to the disproportionate number of students placed at the clinical site, some of these peer groups had more physiotherapy and/or occupational therapy students. The clinical site's managing healthcare professionals and academic staff from the three divisions provided support and mentoring to the smaller peer groups during their initial planning session, as well as the final planning session before the stroke group class. During these two sessions, staff facilitated peer groups on aspects such as: (i) alignment between their therapeutic goals and selected activities; (ii) the feasibility, resource requirements and time allocation of each station; and (iii) the flow and cohesion between different stations to contribute to the holistic storyline of the stroke group class. Students were encouraged to meet separately as many times as they deemed necessary, whether face-to-face or via email and messages. Staff were also available to the smaller peer groups during the interim period for troubleshooting via email and/or cellular phone messages. A final walk-through presentation of the circuit stations was done a few days before the stroke group class, with peer groups describing their activities to each other and the managing staff. Although all staff were available for potential contingency management on the day of the stroke group class, the whole activity was independently managed and executed by the students.
A descriptive phenomenological design was followed in this study, which allowed for a description of the 'lived experiences of individuals'.[17] Final-year undergraduate students from three health sciences divisions (speech-language and hearing, and occupational and physiotherapy) were purposively sampled. Potential participants were approached if they were first-time final-year students and involved in the joint planning and execution of the IFCGA (with no prior experience of IFCGA). All students who fulfilled the criteria participated in the study.
Semistructured individual interviews were conducted with the students by an independent experienced interviewer within 3 working days following the IFCGA. An interview guide with predetermined open-ended questions was used to question participants regarding their roles and experiences during the planning and execution phases of the IFCGA.
The audiorecorded interviews were transcribed verbatim by non-affiliated individuals. Thematic analysis was conducted by the research team to delineate emerging themes. The framework of Burnard[18] was used to analyse the transcriptions inductively. Ethical and institutional approval was obtained before commencement of the study (ref. no. HREC N18/02/2019). Participant information was de-identified during the interview process by not referring to their names on the recording to ensure anonymity.
Trustworthiness and credibility were addressed by using an independent interviewer and peer examination of the themes by various members of the interprofessional research team. Providing relevant information about the research process and context, procedures, research participants and interviewers addressed transferability. Clear and comprehensive documentation of the research procedure enables replication of the study, which addressed dependability. Research team members familiar with qualitative research addressed confirmability.
Results
Twelve students participated (i.e. two physiotherapy, four occupational therapy and six speech, language and hearing therapy students) in the study. All participants were involved in the joint planning and execution of the IFCGA during their clinical rotation at the community-based rehabilitation centre.
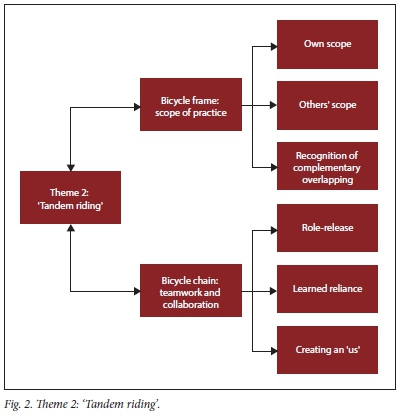
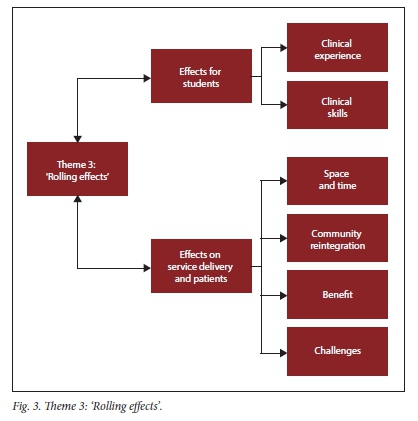
Three themes emerged from the data analysis, namely: (i) IPE wheel; (ii) tandem riding; and (iii) rolling effects. Each theme and its categories are depicted in Figs 1 - 3. The analogy of a bicycle has been used to illustrate the interconnectedness of themes.
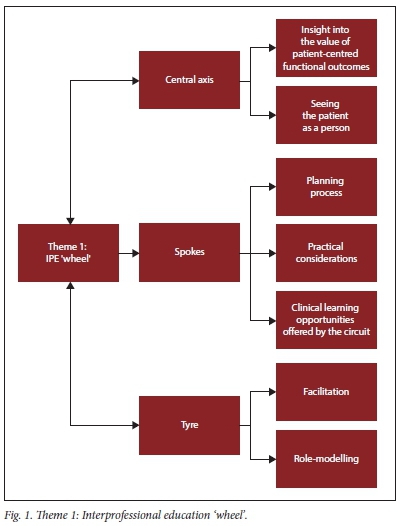
Theme 1: IPE 'wheel'
Theme 1, outlined in Fig. 1, highlights the IPE experiences of students participating in IFCGA, and reflects an iterative learning cycle of planning, execution and reflection. This learning cycle pivots around patients, their context and preferences, with momentum provided through facilitation and role-modelling by the IPE rehabilitation team. The three categories of this theme represent the bicycle wheel and its component parts (central 'axis', 'spokes' and 'tyre').
The 'central axis' category represents person-centredness, where students recognised the patient as a person and developed insight into the value of person-centred outcomes. The 'spokes' represent the experiential learning cycle provided by interactive learning opportunities from planning to execution of the IFCGA, where repetition allowed students to make clinical adjustments. The 'tyre' category emphasises the teaching approach, role-modelling and facilitation by the rehabilitation team providing impetus for the students' learning. Table 1 contains verbatim quotations in support of the categories and subcategories of this theme.
Theme 2: 'Tandem riding'
Collaborative teamwork, such as two cyclists working together in tandem to achieve an easier and efficient riding experience, was required (Fig. 2). Students affirmed their own and others' professional scope and the value of complementary overlap between professions. Integrated planning and execution led to group cohesion, which fostered learned reliance and appreciation for working together. The second theme consists of two categories: (i) scope of practice; and (if) teamwork and collaboration. The first category encompasses the scope progression experienced during collaborative participation in the IFCGA. Principles of teamwork such as communication, shared responsibility and collaborative goal-setting in category 2 led to a positive experience of interdependence among students. Table 2 contains verbatim quotations in support of the categories and subcategories of theme two.
Theme 3: 'Rolling effects'
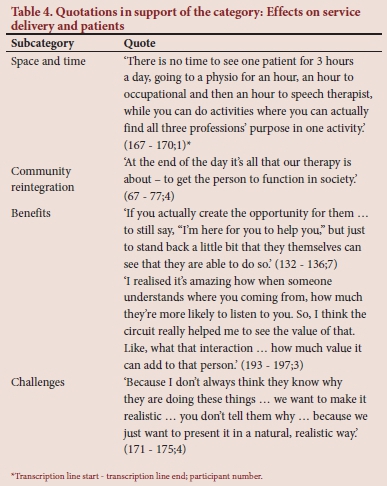
If the IPE wheel (theme 1) and collaborative tandem riding (theme 2) had occurred, the resultant 'tyre tracks' allowed for successful IPE interventions for all involved. Theme 3 (Fig. 3) describes the students' perception of these effects on various role-players. Students valued the positive learning environment created by this IPE activity, which triggered their curiosity to learn and resulted in perceived improvement of their clinical skills. Table 3 provides verbatim quotations in support of the category relating to the effects for students. The 'service delivery' category highlighted how students valued the realistic simulation, patient challenges and logistical implications. Students acknowledged the improved motivation and patient participation in this real-life simulated group activity. Table 4 highlights verbatim quotations in support of the category 'effects on service delivery and patients'.
Discussion
The findings of this study highlighted the experiences of undergraduate physiotherapy, occupational, and speech and language therapy students exposed to an interprofessional clinical learning activity in a community setting. Responses reflected a positive impact on self-development and a realised codependency on other team members, including patients, in achieving health outcomes. Students recognised patients by no longer viewing them as passive recipients of therapeutic input, but rather autonomous beings who could direct and contribute to their own healthcare management.
Students' understanding of their own role expanded when they identified the unique and valuable contribution that their profession could make. The collaborative planning and execution of the stroke group class allowed them to incorporate team goals and to role-release in the absence of another profession. This encouraged thinking beyond their specific professional role.[6] Planning and working collaboratively also fostered a deeper understanding of others' roles, which is a core competency for person-centred collaborative practice.[19] These final-year students also approached patient management holistically to reach overarching functional goals, which highlighted how shared learning opportunities led students to not only appreciate their distinctive roles, but also what they could offer to patients.[6] Providing interprofessional clinical practice training enhances respect for other professionals, including opportunities to value interprofessional care in delivering effective healthcare.[20] Similar positive outcomes to learners' experience of IPE were reflected in a recent review, which reported enhanced understanding of the roles and responsibilities of other professionals, beneficial changes in perceptions of other professionals and the overall value of working collaboratively.[21]
The nature of this clinical activity (IFCGA) lends itself to creating a cohesive 'us'. This cohesiveness stemmed from joint communication, clear expectations of an integrated end-goal, a shared passion for helping others and the requirement of close co-operation with different professions. Working together with peers from other professions became a less threatening learning opportunity, and peer-to-peer teaching allowed freedom to approach each other. The students were also able to observe collaboration between clinicians from different professions. Students reported feeling more confident in seeking collaboration after this exposure, including when starting their professional careers. The IFCGA provided a platform for collaborative learning in an interprofessional environment that fostered the development of effective working relationships with fellow healthcare professionals, as described by Guraya and Barr.[7]
Through the collaborative IFCGA activity, students identified benefits for service delivery, the patients and themselves. They noted that it reduced the service delivery load while providing care to more people, in less time and with fewer resources. A core assumption of IPE is thus highlighted by the better use of scarce resources through enhanced collaboration between professionals.[3,21] Students felt that they were providing more contextually appropriate treatment to achieve residential and community reintegration, thus realising that patients bring a wealth of knowledge and experience to the clinical encounter. This form of role-release to the patient highlighted patient-centredness and how patients became partners in their recovery trajectory. Conducting the activity in a group context was also thought to contribute to the socioemotional peer-to-peer support patients needed to foster hope for their recovery.[13,22] Realistic simulation of everyday activities allowed students to see how patients engaged with enjoyment, which carried over to the students' experience.
These students recognised the role that facilitators fulfilled in supporting the formulation of goals and ensuring equal participation by interprofessional team members, including students, thus highlighting the value of facilitators in creating a learning environment conducive to collaborative learning experiences.[3]
Future research
It is recognised that the staff who facilitated this IPE activity may have influenced the students' experience, owing to their commitment and belief in this teaching and learning strategy. The experiences and characteristics of the IPE facilitators could be explored in future studies.
Conclusion
The IFCGA clinical opportunity beneficially impacted final-year health professions students' collaborative competencies in their knowledge, attitudes, skills and behaviours. Health sciences students at Stellenbosch University are exposed to IPE theory and philosophy in preclinical years that are accompanied by regular contact with various professions during clinical training. Students who participated in this study were immersed in a service-delivery environment where patient interventions are co-ordinated by a multiprofessional rehabilitation team that conducts weekly planning discussions (based on the International Classification of Functioning[16] framework) and joint home-based therapy visits. Within this already rich IPE clinical context, the IFCGA was nested to enhance further interconnectedness between students. Scaffolding these students' collaborative competencies has brought them closer to future professional practice. These students have been primed in their practice readiness as healthcare professionals for the 21st century who will embrace teamwork, which promotes quality person-centred care.
Declaration. None.
Acknowledgements. The research team wish to thank Mrs L Kleineibst, physiotherapist at the Bishop Lavis Rehabilitation Centre, for her invaluable input in the conceptualisation of the integrated circuit group activity and her dedication to student training on the clinical platform.
Author contributions. All authors contributed to the conceptualisation of the project and manuscript, data analysis and content development. They all participated in the critical review of the intellectual content, and approved the final version of the manuscript.
Funding. Fund for Innovation and Research into Learning and Teaching at Stellenbosch University.
Conflicts of interest. None.
References
1. Takahashi S, Brissette S, Thorstad K. Different roles, same goal: Students learn about interprofessional practice in a clinical setting. Nurs Leadersh 2010;23(1):32-39. https://doi.org/10.12927/cjnl.2010.21727 [ Links ]
2. Gilbert JHV, Yan J, Hoffman SJ. A WHO report: Framework for action on interprofessional education and collaborative practice. J Allied Health 2010;39(2):196-197. http://www.who.int/hrh/resources/framework_action/en/ (accessed 11 February 2019). [ Links ]
3. Reeves S, Fletcher S, Barr H, et al. A BEME systematic review of the effects of interprofessional education: BEME Guide No. 39. Med Teach 2016;38(7):656-68. https://doi.org/10.3109/0142159x.2016.1173663 [ Links ]
4. Thistlethwaite J. Interprofessional education: A review of context, learning and the research agenda. Med Educ 2012;58-70. https://doi.org/10.1111/j.1365-2923.2011.04143.x [ Links ]
5. Ateah CA, Snow W, Wener P, et al. Stereotyping as a barrier to collaboration: Does interprofessional education make a difference ? Nurse Educ Today 2011;31(2):208-213. https://doi.org/10.1016/j.nedt.2010.06.004 [ Links ]
6. Konrad SC, Browning DM. Relational learning and interprofessional practice: Transforming health education for the 21st century. Work 2012;41:247-251. https://doi.org/10.3233/wor-2012-1295 [ Links ]
7. Guraya SY, Barr H. The effectiveness of interprofessional education in healthcare: A systematic review and metaanalysis. Kaohsiung J Med Sci 2018;34(3):160-165. https://doi.org/10.1016/j.kjms.2017.12.009 [ Links ]
8. Hilari K. The impact of stroke: Are people with aphasia different to those without? Disabil Rehabil 2011;33(3):211- 218. https://doi.org/10.3109/09638288.2010.508829 [ Links ]
9. Kirkevold M. The unfolding illness trajectory of stroke. Disabil Rehabil 2002;24(17):887-898. https://doi.org/10.1080/09638280210142239 [ Links ]
10. Mayosi BM, Flisher AJ, Lalloo UG, Sitas F, Tollman SM, Bradshaw D. The burden of non-communicable diseases in South Africa. Lancet 2009;374:934-947. https://doi.org/10.1016/s0140-6736(09)61087-4 [ Links ]
11. Wasserman S, de Villiers L, Bryer A. Community-based care of stroke patients in a rural African setting. S Afr Med J 2009;99(8):579-583. https://doi.org/10.1111/j.1747-4949.2009.00275.x [ Links ]
12. English C, Hillier S, Stiller K, Warden-Flood A. Circuit class therapy versus individual physiotherapy sessions during inpatient stroke rehabilitation: A controlled trial. Arch Physical Med Rehab 2007;88(8):955-963. [ Links ]
13. English C, Hillier S, Lynch E. Circuit class therapy for improving mobility after stroke. Cochrane Database Syst Rev 2017;6:CD007513. https://doi.org/10.1002/14651858.cd007513.pub3 [ Links ]
14. Wevers L, van der Port I, Vermue M, Mead G, Kwakkel G. Effects of task-oriented circuit class training on walking competency after stroke. Stroke 2009;40:2450-2459. https://doi.org/10.1161/strokeaha.108.541946 [ Links ]
15. Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: Ttransforming education to strengthen health systems in an interdependent world. Lancet 2010;376(9756):1923-1958. https://doi.org/10.1016/s0140-6736(10)61854-5 [ Links ]
16. World Health Organization. Towards a common language for functioning, disability and health ICF. Geneva: WHO, 2002. http://www.who.int/classiftcations/icf/training/icfbeginnersguide.pdf (accessed 27 September 2017) [ Links ]
17. Creswell J, Miller D. Determining validity in qualitative inquiry. Theory Pract 2000;39(3):124-130. https://doi.org/10.1207/s15430421tip3903_2 [ Links ]
18. Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Educ Today 1991;11(6):461-466. https://doi.org/10.1016/0260-6917(91)90009-y [ Links ]
19. Lait J, Suter E, Arthur N, Deutschlander S. Interprofessional mentoring: Enhancing students' clinical learning Nurse Educ Pract 2011;11(3):211-215. https://doi.org/10.1016/j.nepr.2010.10.005 [ Links ]
20. Pinto A, Lee S, Lombardo S, et al. The impact of structured inter-professional education on health care professional students' perceptions of collaboration in a clinical setting. Physiother Can 2012;64(2):145-156. https://doi.org/10.3138/ptc.2010-52 [ Links ]
21. Reeves S, Perrier L, Goldman J, Freeth D, Zwarenstein M. Interprofessional education: Effects on professional practice and healthcare outcomes (update). Cochrane Database Syst Rev 2013;2013(3):CD002213. https://doi.org/10.1002/14651858.cd002213.pub3 [ Links ]
22. Kloppers M. Die uitkomste wat fisies-gestremde kliënte bereik deur hul deelname aan rehabilitasie by 'n gemeenskapsrehabilitasiesentrum in die Wes-Kaap. MOccTher thesis, Stellenbosch University. Stellenbosch, 2012. http://hdl.handle.net/10019.1/71707 [ Links ]
 Correspondence:
Correspondence:
M Kloppers
maatje@sun.ac.za
Accepted 10 February 2021














