Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
African Journal of Health Professions Education
versión On-line ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.13 no.4 Pretoria dic. 2021
http://dx.doi.org/10.7196/ajhpe.2021.v13i4.1293
RESEARCH
Understanding of clinical reasoning by undergraduate students and clinical educators in health and rehabilitation sciences at a South African University: The implications for teaching practice
H TalbergI; F Camroodien-SurveII; S L AmosunIII
IMPhil (HES); Department of Health and Rehabilitation Sciences, Faculty of Health Sciences, University of Cape Town, South Africa
IIM ECI; Department of Health and Rehabilitation Sciences, Faculty of Health Sciences, University of Cape Town, South Africa
IIIPhD; Department of Health and Rehabilitation Sciences, Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: Clinical reasoning (CR) is a skill acquired by students under supervision of clinical educators (CEs) when transitioning from classroom to clinical practice to optimise patient care. However, intra- and inter-professional differences in the definition and facilitation of CR have been reported. At the University of Cape Town, a teaching development grant was obtained and used for a staff development initiative aimed at improving the CR skills of undergraduate health and rehabilitation students
OBJECTIVES: To gain insight into the understanding of CR among CEs and a cohort of third-year students across 4 professional programmes, using an interpretive approach
METHODS: The CEs responsible for third-year supervision (n=45) were invited to take part in a self-developed electronic survey and an initial workshop that explored their understanding of CR. The qualitative survey data, as well as workshop feedback and discussion, were analysed. Students' understanding was explored during focus group discussions
RESULTS: There were areas of commonality and differences among CEs. They agreed on a cyclical step-like process to CR and the need to cue students to develop this expertise in clinical settings. The approach of CEs in occupational therapy was client focused; physiotherapy CEs described a higherorder thinking; and audiology and speech and language pathology CEs described a structured procedure informed by evidence. Students were unable to conceptualise a complete picture to reasoning and decision-making
CONCLUSION: The difference between students' understanding of CR and their poor awareness of strategies employed by CEs to facilitate reasoning could account for difficulties in transitioning from classroom to practice. This scenario suggests that divisions need to look at creating more purposeful strategies to teach students about the CR process and how the facilitation may occur within the clinical setting
Transitioning from classroom to clinical setting presents multiple challenges for health science students. These challenges range from a lack of generic skills and professional behaviours to difficulties translating the taught skills and theory into patient management, raising further concerns about the existence of a 'theory-practice gap'.[1] Even under the supervision of clinical educators (CEs), students struggle with the complexity of the clinical situations they encounter. CEs are also challenged when facilitating students' learning in these complex clinical contexts, while providing effective service to patients.[2]
Skill in clinical reasoning (CR) is necessary to guide students and educators in assessing, assimilating, retrieving and/or discarding components of information that affect patient care.[3,4] Failure to develop CR is considered one of the key reasons for students' lack of confidence and effectiveness in the clinical area, ultimately influencing their academic success.[5] While the explicit development of CR is a foundation requirement of entry-level practice education,[6] it cannot be assumed to develop in the absence of specific educational strategies.[4] Therefore, CEs need to create learning opportunities that explain the multidimensional nature of CR to students to support them in developing these capabilities and scaffold the development as they progress through their clinical years.
'Until well into the 17th century, academic medicine was almost exclusively a theoretical affair. Reasoning played an important role, but it was exclusively employed to defend theses or to construct logical arguments, rather than to arrive at diagnoses or to select therapies.'[7] Over the years, there were many attempts to integrate theoretical knowledge with clinical experience, and thus the value of teaching CR to students became more evident. However, CR is not taught explicitly in all health profession educational programmes. Another challenge is the existence of different interchangeable terminologies, definitions and concepts for CR.[3,8-10] Differences among healthcare professionals regarding the CR processes were also noted. While medical professionals focus on a cognitive psychology perspective, nursing or physiotherapy professionals adopt an interpretive and sociocultural lens that goes beyond the cognition.[6] These discrepancies possibly contributed to a potential mismatch between CEs' and students' understanding of CR, and how learning and teaching may be facilitated.[10] It could also account for the lack of student awareness of the cues being provided by the CEs, which ultimately results in a lack of development in the area. Therefore, it seems that educators and students would benefit from attempts to develop a common understanding of the concept of CR and its terms.
Understanding the CR process is challenging.[11] In the broadest and most general sense, it 'can be summarised as the thinking and decision making of a health care provider in clinical practice,'[11] leading to clinical decision-making. CR was also defined as 'an inferential process used by practitioners to collect and evaluate data and to make judgments about the diagnosis and management' of patients' concerns.[12] It includes the application of cognitive and psychomotor skills based on theory and evidence, as well as the reflective thought process to direct individual changes and modifications in specific patient situations. Current research in CR suggests that the process of applying knowledge and skill, integrated with the intuitive ability to vary an examination or treatment based on reflection and interaction to achieve a successful outcome for an individual patient, separates expert clinicians from novices.
Teaching CR needs to be made tangible so that students can merge it into their own developmental processes in clinical practice,[13] utilising a range of capabilities - cognitive, metacognitive, social and emotional skills - during clinical decision-making.[6] Acknowledging that CR is a core competence of healthcare professional education in linking theory to practice, it is important to know if CEs create the necessary active learning environments for students to enhance CR.
At the University of Cape Town (UCT), the Department of Health and Rehabilitation Sciences (DHRS) offers 4-year undergraduate programmes in audiology, occupational therapy (OT), physiotherapy (PT) and speech and language pathology (SLP). The programmes are structured with the basic sciences and introductory profession-specific courses taught in the first 2 years. Limited clinical exposure is introduced in the second year, focusing on communication skills, clinical interviewing and basic examination skills. Students move to more independent practice in their third year and are exposed to a range of diverse clinical settings: hospitals, clinics, schools, non-governmental organisation (NGO)-run sites and old-age care facilities. During their fourth year, clinical hours are increased, with students working in tertiary care and complex environments. On-site clinical training is provided largely through CEs employed by the university.
Although there are some differences in the organisation of clinical education across the 4 undergraduate programmes, the students spend 4 - 6 weeks on each block placement. The CEs generally give 1 - 4 hours per week of individual facilitation to their respective students across their allocated sites. Working with clinicians or site personnel, CEs are required to optimise learning opportunities and ensure that student learning outcomes are met. Learning is enhanced through group teaching and peer-led sessions. Formative assessments are offered midway in a placement, and students' written portfolios create additional learning opportunities to facilitate growth and improvement before summative end-of-block assessments.
Although not always stated explicitly, developing CR is one of the key goals of clinical teaching.[13] Yet, CR as a concept is not formally taught in undergraduate programmes in the DHRS, except in OT. The two main steps in the CR process involve gathering and analysing information (diagnostic reasoning) and deciding on therapeutic actions specific to a patient's circumstances and wishes (therapeutic reasoning).'131 Differences have been reported in the thinking processes between 'expert' and 'novice' healthcare practitioners. In the context of student training in the DHRS, CEs are the expert healthcare professionals, while the students attempting to merge classroom theory with clinical reality are the novices. Two questions emerged from this scenario: (i) How is CR being taught in the DHRS at UCT?; and (ii) Are the differences in teaching of CR part of the barrier in students' inability to integrate their theoretical knowledge into clinical practice?
To respond to these questions, the DHRS applied for and obtained a teaching and development grant (TDG) from the Department of Higher Education and Training in 2014 to address the difficulties that students experience in transitioning from their second year to their third and fourth clinical years - moving from a theoretical to a more clinical paradigm. The broad purpose of the grant was to observe teaching practices in clinical courses, develop improved teaching strategies among CEs across the 4 different programmes and work at improving student performance in profession-specific clinical courses. A staff development initiative was conceptualised, which was aimed at developing an educational approach to teaching CR to students across the 4 professional programmes in the DHRS. It was hypothesised that the developed framework will improve the experiences of students in their integration of theoretical knowledge into clinical practice.
To achieve this outcome, the TDG-funded programme undertook the following 5 key activities over a 3-year period:
• The collection of baseline data on: (i) the understanding of students and CEs regarding CR; (ii) teaching strategies used by CEs to facilitate students' CR; and (iii) challenges faced by CEs in developing CR.
• The training of CEs through workshops on CR, identifying the challenges students encountered and to target strategies to facilitate reasoning.
• Informing students of the teaching strategies, followed by evaluating the awareness of the use of these strategies in the clinical setting.
• Monitoring and evaluating the impact of the developed framework.
• Development of a training tool for CEs regarding CR.
This article draws on some of the survey information obtained in the collection of baseline data, the initial facilitated workshop with third-year CEs and the focus group discussions with third-year students. It aims to:
• Provide insight into the initial understanding of CR among CEs across divisions.
• Provide insight into the initial understanding of CR among third-year students across the 4 undergraduate professional programmes in the DHRS.
• Discuss differences and similarities in the understanding of the CR process between CEs and students and the implications thereof.
It is assumed that if CEs and students share similar views or have an awareness of each other's perceptions of CR, the education process is likely to be more effective.
Methods
At the start of the project, a decision was made to investigate third- and fourth-year students and CEs separately. It was presumed that there would be different issues raised in the different years, possibly requiring different facilitation. Hence, only third-year students and CEs were included in this phase, with the hope of repeating the process for fourth-year students at a later stage. All the CEs involved in teaching of third-year students in the 4 professional programmes (n=45) were invited to take part in a self-developed electronic survey that was conducted via Survey Monkey. The researchers, some of whom had CE roles, were excluded from the data collection process. The questionnaire was developed with the assistance of the Education Development Unit (EDU), taking into account the overall outcomes of the project. This review provided some validation of the questionnaire, and all stakeholders reached agreement regarding the relevant questions. There was no piloting process, and all information obtained was used. Informed consent was obtained from the CEs before the administration of the survey questionnaire, which was completed anonymously. The first part of the questionnaire sought information regarding the CEs' clinical teaching experience and expertise, formal teaching education and years of professional experience. Three open-ended questions were then posed:
• What is your description of CR?
• How would you facilitate CR with a student who struggles with the integration of theoretical knowledge in clinical practice?
• What are the main problems associated with enhancing CR in third-year students entering clinical practice?
A response rate of 35.5% (n=16) was achieved, comprising 7 PTs, 4 OTs,
3 audiologists, and 2 SLPs. The qualitative data were extracted by an independent assistant and core phrases highlighted for analysis by the researchers.
This baseline survey information was explored further in a facilitated workshop for third-year CEs. Of the CEs invited, 24 attended. CEs were provided with literature on various forms of CR and small-group interdisciplinary discussions on types of CR introduced. CEs were then encouraged to reach consensus on their own understanding of the process of CR and what steps students ultimately would need to go through and understand when working with clients for successful outcomes. These conclusions are presented in the results section. Discussions on strategies and problems encountered in the CR facilitation process were tabled and formed the basis for subsequent workshops. These discussions are not within the scope of this article.
Purposeful sampling was used to recruit third-year students in audiology, OT, PT and SLP for focus group discussions around the topic of CR. The recruitment invitation was sent through the university's electronic communication site (VULA) on the individual clinical pages of each of the 4 academic programmes. Separate focus groups were also planned for each discipline, as it was important to appreciate each discipline's understanding of CR, as well as how each discipline experienced the teaching of CR. All 175 registered third-year students were eligible to participate. Of these, 9 PT, 5 OT and 4 SLP students and 1 audiology student participated. The response rate was very low, probably because the timing was close to the end of academic year examinations. Consequently, a single focus group discussion was held for each of the 3 professional programmes, i.e. OT, PT and SLP. The audiology student was interviewed separately.
Students were informed of the purpose of the study and signed informed consent forms, as well as a confidentiality agreement before participation. The groups were audio-taped and facilitated by a CE from a professional discipline different to that of the students in their group. This was to avoid any preconceived bias with regard to how teaching happened in that specific discipline, and to ensure that students would feel more open to discussion by not 'knowing' the facilitator. Each group was asked the same 3 core questions:
• What is your understanding of CR?
• What are the difficulties you experience with CR in practice?
• How do you pick up CR cues given by the CE?
However, the depth of discussion could develop at the discretion of the facilitator. These questions aligned to the questions asked in the initial survey of CEs. The findings of the first question are reported in this article.
The audio-recording of each focus group discussion and interview was transcribed and analysed as a single case.[10] An inductive approach was used to analyse the transcription. The principal investigator did an initial analysis, highlighting the core findings. The researchers then worked in pairs to further discuss, analyse and define key areas in line with the research focus. For the purpose of this article, 2 authors again reviewed the core data. Where there were differences in opinion or interpretation, the third author was approached to assist in reaching a consensus.
Ethical approval
Ethical approval (ref. no. HREC/REF 693/2014) to use the information in the first phase of the project for research purposes, was obtained from the Human Research Ethics Committee, UCT.
Results
Survey of clinical educators
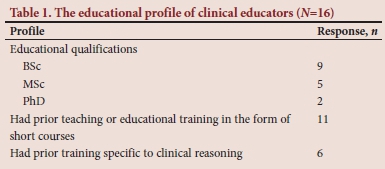
The educational profiles of the CEs are presented in Table 1. The average years of experience as a CE at UCT was 6.9 (2 - 30) years. CEs spent an average of 6 hours per week in direct supervision of the students. The sites where CEs were mostly deployed for clinical supervision are presented in Table 2.

Clinical educators' description and understanding of clinical reasoning
The PTs described CR as a 'higher order thinking process in the clinical setting', highlighting the concepts of 'gathering information, interpreting and creating hypothesis, utilizing information as part of an intervention, and then reflection on outcomes'. One of the CEs described CR as the process used to make sense of all the information gathered on a patient and then how to use the information to identify and analyse (by linking theory to observations) the patient's problems, plan and implement an appropriate intervention and re-evaluate the outcome, using reflection'.
The OTs had a clear theoretical construct of CR, framing it in terms of whether it was 'procedural, narrative, conditional etc.', talking about 'conscious cognitive application and procedural categories of thinking about thinking'. None of the other disciplines framed the process using theoretical terminology. The other noticeable feature regarding OT decision-making was that it was very client focused, using information on the clients' circumstances and values to support their reasoning.
The audiologists' CEs seemed to have the most procedural approach to decision-making, speaking about collecting information in a 'structured way' and being guided by clinical protocols and diagnosis in management.
The SLP CEs described CR as 'the process that a person uses to formulate an opinion on management of a case'. SLPs also referred to using the theoretical knowledge to assist clinical decision-making.
Workshop 1 for clinical educators
Twenty-four CEs completed the first workshop and agreed to have their comments and opinions recorded for study purposes. They all indicated an improvement in their own understanding of CR after the workshop (Table 3).
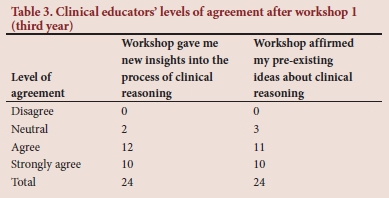
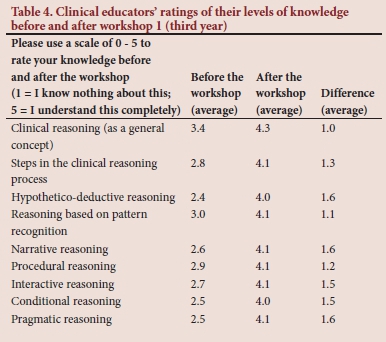
Most participants agreed that workshop 1 gave them new insights into the process of CR and that it confirmed their pre-existing ideas about CR (Table 4).
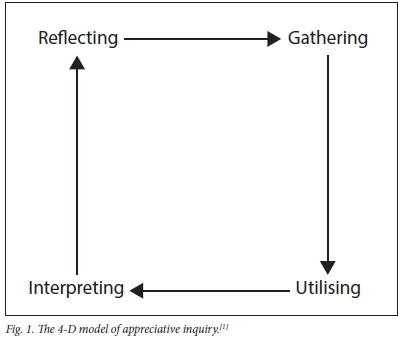
Through discussion, there was disciplinary agreement that CR is a comprehensive, cyclical process. This was elaborated on by all participating CEs to create a 4-step concept of the CR process (Fig. 1). The first step involved gathering of information, which occurred in multiple ways. It drew on reading, listening and visual cues relating to a specific client and context. Many CEs perceived this as the integration and/or application of their theoretical knowledge into clinical practice. Step 1 led to step 2, where, after appropriate clinical assessment, interpretation of the gathered information allowed them to generate a working hypothesis or diagnosis. The interpretation was used in step 3, which involved the management of the client. These first 3 steps happened logically, as treatment decisions linked to theory and knowledge that were gained through experience. Decisions were then prioritised for maximum effect. In step 4, overall effectiveness was constantly monitored through reflection and outcome measures.
Students' focus groups
Data from students revealed that there were differences in their understanding of CR. The PT students (n=7) struggled to voice a clear definition or understanding of CR. They focused mostly on their relationships with the CEs, and how this either facilitated or hindered their learning on clinical block placements:
'Strategies that do work, having a good relationship, supervisors who are really patient, who are willing to help, knowledgeable, available and just approachable to be honest.'
The students' responses showed their lack of awareness of strategies employed by their CEs to guide them, as they considered the questions posed by their CEs as a hindrance rather than a facilitator of the CR process: 'You need to be able to go to your supervisor and say "I've clinically reasoned to come to this conclusion of what I'm doing" and then to be able to say that that's right and that's wrong or just guide you on the right path, um, instead of asking further questions and being like why did you think, you've got the answer there, you know what I mean. Be more straightforward.'
The SLP students (n=4) described CR as transference of knowledge obtained in the classroom, accessing evidence, considering contextual relevance and being able to formulate an intervention plan. There was a strong emphasis on the importance of supporting their practice with the literature/ evidence. They seemed to understand that in addition to the evidence that was required, you had to think and reason about whether it was relevant to context and that this process defined reasoning:
'You still have to take whatever information you have and make it patient specific.'
'Um and what I've seen as well is that clinical reasoning can be something that can actually come out of the clinical setting and that particular type because for instance if today I plan that I'm going to do aim A because Joseph Duffy [name of author in the literature] did it and he found that it works for patients with aphasia and I find that with my patient it doesn't work well because of the context that I'm in. If I restructure whatever he said and do it in a way that is context specific and tailored for my patient, I can write it down with the rationale that is backed by Duffy's evidence.'
One of the audiology students saw CR as a more procedural process.
Situations that differed from the regular caseload could not be easily reasoned through, leaving students unable to make decisions about assessment and treatment:
'They are going to feel uncomfortable when you test the ear, so I wasn't prepared for that. I think it was only mentioned once or twice in my course so when I actually assessed this patient, I was quite flustered because I didn't really know what to do.'
The OT students (n=5) saw CR as the ability to problem solve, reflect in action and evaluate in hindsight. One student commented:
'It kinda got, like why did you do that, and I had to think about why they did that, ... and just be forced to go, this is why I did this, this is why
I did that.'
Another OT student stated:
'Reflection is a big part of it, um, which we obviously did throughout our blocks and also like you, clinical reasoning happens while you [are] doing a session so, in action or out of action.'
The OT students displayed a theoretical knowledge of reasoning strategies and approaches, which was different to that of the other students. However, although they grasped the idea, they did not draw out the process as comprehensively as the CEs, and did not describe all the steps they would go through in the decision-making process.
Discussion
Over a 3-year period, several TDG-funded key activities were carried out to address the difficulties that undergraduate students in the DHRS at UCT experience in transitioning into the clinical years of their education programmes. This article reports on the initial stages of the activities, which aimed to gain insight into the understanding of CR among CEs and students.
According to the literature, there were discrepancies among CEs regarding basic CR terms,[8,9] and there seemed to be initial differences in the focus of the description of CR among the CEs of the different disciplines that took part in the baseline survey. The PTs focused on the process that required a higher-order thinking in the clinical setting. The OTs framed their description as client focused. The CEs for audiology and SLP focused on structured procedure that was informed by evidence from the literature. However, through a workshop process, it became clear that, although the naming of the CR type or core descriptors may have differed, there was an underlying agreement that CR is a cyclic step-like process, whereby information is obtained, processed, used and reflected on to provide the best care for clients.
In contrast, students did not portray the same understanding of the CR process. Unlike some students who perceived CR as an instrumental, clinician-centred process that is dependent on knowledge and context,[10] PT students linked CR to relationships with CEs and how they could facilitate or hinder learning. For OT students, their understanding was related to the process of identifying the problems that were most important to the patient.[12] Students in audiology and SLP would require clinical decision-making skills when appraising the available evidence in an effort to select the most appropriate treatment.[12]
The data showed that there is a gap between CEs and students' perceptions of the process of CR and the components that need to be in place for reasoning to develop.[11] Educators seem to share a common understanding of the components of the reasoning process and can define the steps involved. However, it is apparent that they see this as a cyclical process, where one step leads to another, drawing on multiple cues and information.[4] Students, however, do not seem to grasp the entirety of the process or note when CEs are trying to develop their CR. They recognise parts of what is required, but do not seem to easily put it all together. This process may be developmental in nature, changing as they progress through the clinical years, moving from novice to more independent practice.
Even the OT students, who had the strongest sense of what reasoning relied on and could label the types of reasoning strategies they needed to use, did not break the process down as succinctly as the CEs or note the cues used by CEs to facilitate CR. They are formally taught reasoning strategies as part of a preclinical course, which clearly puts them ahead of the other disciplines in recognising aspects needed for CR.
Perhaps the best alignment between CEs and students was in the audiology discipline, where procedure seemed to be key. This alignment could speak to the nature of the work that audiologists are involved in, especially at a third-year level. However, this observation cannot be generalised.
Study limitations
The sample size, particularly of students, provides a limited view of the topic. Unfortunately, the long-term intention to complete focus group discussions with fourth-year students, which may have added deeper insight into the understanding of CR development across clinical years, was not feasible within the period of funding. This remains an area for investigation.
Conclusion
CR is a complex, learnt process that needs to be explicitly taught and guided in the clinical setting. There are inter-disciplinary differences among CEs in defining CR across the health and rehabilitation sciences. This speaks to the different scopes of the professions within clinical contexts. However, when probed, all the disciplines recognised the complex cyclic nature of the process, which relies on multiple cues and inputs for success. Of concern are the differences between CEs and their students. This leads to students potentially missing key cues from CEs guiding them through the CR process and a lack of awareness that the CE is stimulating the process. This mismatch may be consistent with the literature, alluding to the gap between theoretical knowledge and its clinical implementation. Divisions need to consider how to minimise the disconnect between CEs and students to reduce the gap. Explicit teaching around the nature of CR and the strategies of facilitation by CEs could aid in this process.
Future research
Although not discussed within the scope of this article, there are some common strategies that can be drawn on to guide students entering clinical practice. These include formal training with students around types of reasoning and strategies used by CEs to facilitate CR, as well as a conscious effort by educators to make their own thinking practices of CR visible to students during sessions. The facilitation of the students' CR process through shared awareness is the key to closing the gap and aligning the mismatch between the perceptions of CEs and students as to what CR entails.
Declaration. None.
Acknowledgements. The author acknowledges the assistance of clinical educators Ms Naila Edries Khan (physiotherapy) and Ms Tasneem Mohomed (occupational therapy), and Prof. Francois Cilliers (Education Development Unit (EDU)) in co-ordinating the project.
Author contributions. HT and FC-S: main body of the article, discussion and conclusions; SLA: literature review and introduction, content oversight and flow.
Funding. The project was funded by a Department of Higher Education and Training development grant aimed at faculty development.
Conflicts of interest. None.
References
1. Newton JM, Billett S, Jolly B, Ockerby CM. Lost in translation: Barriers to learning in health professional clinical education. Learn Health Soc Care 2009;8(4):315-327. https://doi.org/10.1111/j.1473-6861.2009.00229.x [ Links ]
2. Dhaliwal G. Developing teachers of clinical reasoning. Clin Teach 2013;10(5):313-317. https://doi.org/10.1111/tct.12082 [ Links ]
3. Simmons B. Clinical reasoning: Concept analysis. J Adv Nurs 2010;66(5):1151-1158. https://doi.org/10.1111/j.1365-2648.2010.05262.x [ Links ]
4. Wu B, Wang M, Grotzer TA, Liu J, Johnson JM. Visualizing complex process using a cognitive-mapping tool to support the learning of clinical reasoning. BMC Med Educ 2016;16(216). https://doi.org/10.1186/s12909-016-0734-x [ Links ]
5. Wrenn J, Wrenn B. Enhancing learning by integrating theory and practice. Int J Teach Learn High Educ 2009;21(2):258-265. [ Links ]
6. Ajjawi R, Smith M. Clinical reasoning capability: Current understanding and implications for physiotherapy educators. Focus Health Professional Educ 2010;12(1):60-73. [ Links ]
7. Custers EJFM. Training clinical reasoning: Historical and theoretical background. In: Ten Cate O, Custers E, Durning S, eds. Principles and Practice of Case-based Clinical Reasoning Education, Innovation and Change in Professional Education. Heidelberg: Springer, 2018. https://doi.org/10.1007/978-3-319-64828-6_2 [ Links ]
8. Musgrove JL, Morris J, Estrada CA, Kraemer RR. Clinical reasoning terms included in problem solving exercises: J Grad Med Educ 2016;8(2):180-184. https://doi.org/10.4300/jgme-d-15-0041L1 [ Links ]
9. Dhaliwal G, Ilgen J. Clinical reasoning: Talk the talk or just walk the walk? J Grad Med Educ 2016;8(2):274-276. https://doi.org/10.4300%2FJGME-D-16-00073.1 [ Links ]
10. Cruz EB, Moore AP, Cross V. A qualitative study of physiotherapy final year undergraduate students' perceptions of clinical reasoning. Musculo Sci Pract 2012;17(6):549-553. https://doi.org/10.1016/j.math.2012.05.013 [ Links ]
11. Furze J, Black L, Hoffman J, Barr JB, Cochran TM, Jensen GM. Exploration of students' clinical reasoning development in professional physical therapy education. J Phys Ther Educ 2015;29(3):22-33. https://doi.org/10.1097/00001416-201529030-00005 [ Links ]
12. Atkinson HL, Nixon-Cave K. A tool for clinical reasoning and reflection using the International Classification of Functioning, Disability and Health (ICF) framework and patient management model. Phys Ther 2011;91(3):416-430. https://doi.org/10.2522/ptj.20090226 [ Links ]
13. Delany C, Golding C. Teaching clinical reasoning by making thinking visible: An action research project with allied health clinical educators. BMC Med Educ 2014;14:20. https://doi.org/10.1186/1472-6920-14-20 [ Links ]
 Correspondence:
Correspondence:
H Talberg
heather.talberg@uct.ac.za
Accepted 19 November 2020














