Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.13 n.4 Pretoria Dec. 2021
http://dx.doi.org/10.7196/ajhpe.2021.v13i4.1338
RESEARCH
Medical students' perceptions of global health at the University of Cape Town, South Africa: The gap between interest and education
M PotterI; P NaiduII; L PohlIII; K ChuIV
IMB ChB; Livingstone Hospital, Gqeberha, South Africa
IIMB ChB; Centre for Global Surgery, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town, South Africa
IIIMB ChB; Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
IVMPH; Centre for Global Surgery, Department of Global Health, Faculty of Medicine and Health Sciences, Stellenbosch University, Cape Town; and Department of Surgery, Faculty of Health Sciences, University of Cape Town, South Africa
ABSTRACT
BACKGROUND: Global health competencies are an increasingly important part of medical training; however, there is currently no integrated formal global health curriculum at South African (SA) medical schools, and perceptions of medical students towards global health have not been reported
OBJECTIVES: To describe SA medical students': (i) perceptions of global health; (ii) access to global health education (GHE); (iii) awareness of global surgery as a global health priority; and (iv) perceived relevance of select medical specialties to global health
METHODS: Medical students at the University of Cape Town (UCT), SA, were invited to complete a 35-item survey over 2 months in 2018. The survey was designed on REDCap (Research Electronic Data Capture) and distributed by email. All responses were anonymised and self-reported
RESULTS: Of 1 640 medical students, 245 (18%) completed the survey. Only 66 (27%) reported GHE in medical school, whereas 213 (87%) reported a career interest in global health. Childhood in a rural setting was a positive predictor of a career interest in global health, while lack of medical resources and infrastructure in resource-limited communities was the most commonly cited barrier to a career in global health. Most students identified family medicine and infectious diseases as the two most important specialties in global health delivery. The majority of students had limited insight into global surgery, which ranked low as a past and future global health priority
CONCLUSION: UCT medical students are interested in global health careers, but lack formalised GHE or global surgery education during their medical studies to support and encourage integrating global health into their future careers
Global health is the study and practice of improving health equity worldwide.[1] The academic field of global health is developing rapidly, leading to the establishment of global health departments and dedicated centres at universities worldwide. This situation is mirrored with global surgery, or the equitable access to timely and quality surgical care, which was identified as a key global health priority in 2015.[2] There is increasing recognition that global health competencies should be formally incorporated into medical school curricula, especially in low- to middle-income countries (LMICs), where many global health conditions, such as HIV/AIDS and tuberculosis, as well as maternal mortality and equitable surgical access, have a disproportionate footprint.[3]
Since its inaugural meeting in 2008, the Consortium of Universities for Global Health (CUGH) set out to identify and describe 11 core domains of competency in global health to address the rapid expansion of global health programmes without a standardised curriculum to guide them. The domains described by CUGH focus on interprofessional knowledge and skills for working within the field and are intended to be applicable across disciplines at four levels of competency.[4] These competencies serve as important tools for setting assessable standards for knowledge and performance in medical school training, and are critical to curriculum development and evaluation.[4] With ongoing research to identify perspectives of global health competencies needed in undergraduate training in settings outside of North America, many of the core competency domains remain relevant while other discipline-specific competencies have emerged.[4]
Addressing healthcare disparities through the lens of global health requires local perspective and ownership to bring about sustainable change.[1] SA, an upper middle-income country, has one of the most inequitable healthcare systems in the world, with a fractured health system and resource distribution between the public and private health sectors.[5] The incoming National Health Insurance (NHI) proposes a substantial reorganisation of the current healthcare system to achieve health equity and, as such, adopts many of the same core principles espoused by CUGH[4] and the Sustainable Development Goals (SDGs) 1, 2, 3, 5 and10.[6] SA medical schools provide formal education in public health, a discipline from which 7 of the CUGH principles were adapted.[4] Students may gain indirect exposure to global health concepts and competencies through public health curricular activities, or directly through self-directed extracurricular involvement (such as student societies and research). Nevertheless, global health education (GHE) is yet to be widely implemented in SA medical schools and, to date, the University of Cape Town (UCT) does not include CUGH domains in its curriculum. While student perceptions of global health have been well described in several high-income country (HIC) settings,[3,7,8] CUGH competencies were developed with a focus on students in North America; hence, there is a paucity of literature describing perceptions held by medical students from LMICs and SA, in particular.
Surgical care is a key component of universal health coverage and is recognised as a core specialty in the global health agenda.[2] However, a previous study conducted in the USA demonstrated little knowledge of global surgery concepts.[9]
Determining SA medical students' perceptions of global health may assist in identifying gaps in knowledge related to CUGH domains of global health competency, and may inform the development of context-relevant GHE. The objectives of this study were to describe SA medical students': (i) perceptions of global health; (ii) access to GHE; (iii) awareness of global surgery as a global health priority; and (iv) perceived relevance and contribution of select medical specialties to global health.
Methods
Setting
This study was conducted at the Faculty of Health Sciences, UCT.
Study design
A 35-item survey was adapted from a survey administered to US medical students,[9] eliciting an interest in global health, as well as knowledge of global health definitions and competencies under CUGH domain 1 (global burden of disease) and domain 2 (globalisation of health and healthcare).[4] Additional questions added in our adapted survey included further demographic and global surgery-specific questions. Our survey was designed on REDCap (Research Electronic Data Capture) version 8.4.3 (Vanderbilt University, USA) and distributed by email to all 1 640 medical students (first - sixth year) at UCT. The survey was voluntary, and all responses were self-reported and anonymised. The survey included basic demographic information, including place of birth, rurality of childhood setting and previous residence in another LMIC. Participants were asked if they had received any form of GHE, which was defined as any formal (curriculum based) or informal class/workshop/course (online or offline) that provided teaching of global health concepts and/or competencies.
Global health knowledge and career interest were ascertained. Interest in a career was reported as a percentage of a participant's career dedicated to global health work; a threshold of 50% was used to model predictors of interest in a career in global health. Self-reported perceptions of disciplines within global health were included. Respondents were allowed to select up to five statements that they perceived as being appropriate definitions of global health. Knowledge of global surgery as a global health priority was assessed, with specific questions on key global surgery publications. The perceived relevance and contribution of medical specialties to global health were also ascertained: participants selected 2 medical specialties that they perceived to have had the greatest impact on global health in the past 25 years; the 2 medical specialties that they perceived as potentially having the greatest impact on global health in the next 25 years; the 2 medical specialties that should be global health priorities, but are not currently prioritised by national or international agendas; and the single medical specialty that serves as the best indicator of a robust health system in terms of its contribution towards achieving universal health coverage, which is embodied by the World Health Organization (WHO)-defined objectives of equity in access, quality and cost-effectiveness of the specific medical specialty.[10]
The options for these questions were limited and included emergency medicine (EM), family medicine (FM), infectious diseases (ID), obstetrics and gynaecology (OBGYN), paediatrics, psychiatry, surgery and 'other' (for which respondents provided a specific medical specialty not listed above). Participants were also asked to compare 5 medical specialties - FM, OBGYN, ID, EM and surgery - regarding several characteristics, using a 5-point Likert scale.
Study population
Preclinical students were defined as those in the first, second or third year and clinical students as those in the fourth, fifth or sixth year of the Bachelor of Medicine and Surgery (MB ChB) degree programme.
Data analysis
Data were exported from REDCap and all analyses were performed on RStudio version 1.1.442 for Apple (RStudio Inc., USA). Descriptive statistics were used to characterise Likert-type questions. Continuous variables were expressed as means (with standard deviation (SD)) or medians (with interquartile range (IQR)). Categorical data were presented as frequencies and percentages. Continuous variables were compared using either Student's f-test (for normally distributed data) or Wilcoxon's rank-sum test (for skewed data). Depending on the distribution of data, either x2or Fisher's exact test was applied to compare categorical data. Logistic regression was used to identify associations with interest in a global health career. Several factors were evaluated through univariate regression and those with p<1.0 were included in the multivariate analysis. A p-value of <0.05 was considered statistically significant.
Ethical approval
Ethical approval was given by the UCT Human Research Ethics Committee (ref. no. HREC 2018/111). Participant consent was obtained electronically; there was no benefit or risk to participants.
Results
Demographics
The survey was emailed to 1 640 UCT medical students and completed by 245 (18% response rate). Of these, 150 (61%) were preclinical and 95 (39%) were clinical students. One hundred and sixty-four (67%) identified as female and 81 (33%) as male. The majority of respondents (n=228; 93%) were born in SA, and 34 (14%) had lived in another LMIC for at least 1 year. Two hundred and nine (85%) reported childhood in an urban setting and 36 (15%) in a rural setting (Table 1).

Global health education
The majority of respondents (n=170; 73%) reported no previous formal or informal GHE. There was no significant difference between preclinical and clinical students (p=0.1).
Perception of global health concepts
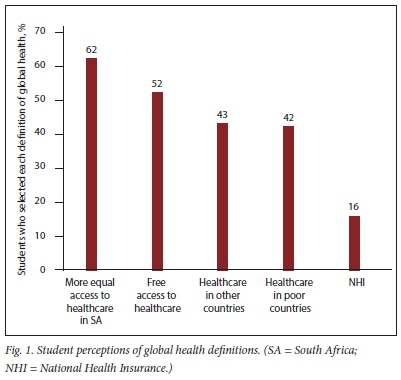
Respondents perceived the following to be in line with the concept of global health (Fig. 1): equitable access to healthcare (n=151; 62%); free healthcare (n=126; 52%); healthcare in other countries (n=106; 43%); healthcare in poor countries (n=104; 42%); and the proposed NHI in SA (n=38; 16%).
Knowledge of global surgery as a global health priority
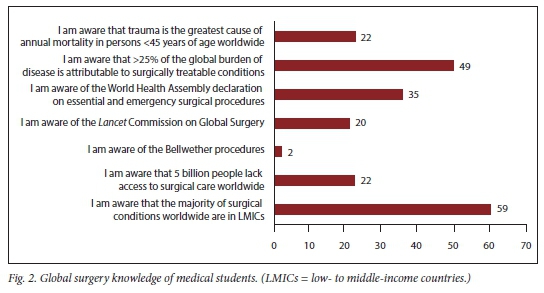
One hundred and twenty (49%) respondents accurately identified that more than a quarter of the global burden of disease are from surgical conditions. One hundred and forty-five (59%) respondents were aware that the majority of surgical conditions worldwide occur in LMICs. Twenty-two percent (n=54) accurately identified trauma as the greatest cause of annual mortality in persons <45 years of age worldwide.[1] Fifty (20%) respondents were aware of the Lancet Commission on Global Surgery, while 86 (35%) had knowledge of the World Health Assembly (WHA) declaration on essential and emergency surgical procedures - two landmark publications in the field of global surgery (Fig. 2).
Global health career interest
A total of 213 (87%) participants expressed interest in incorporating global health into their career. The mean (SD) of desired career time and effort for global health endeavours was 41 (27)%. There was no significant difference between preclinical and clinical students (p=0.67). The most commonly perceived barrier to a career in global health (Table 2) was available medical resources and infrastructure in resource-limited communities (n=156; 72.6%), followed by lack of exposure to global health training in early career (n=145; 67.4%). Sixty-seven (25%) participants perceived a lack of role models as a barrier to incorporating global health into their careers.

Predictors of global health career interest
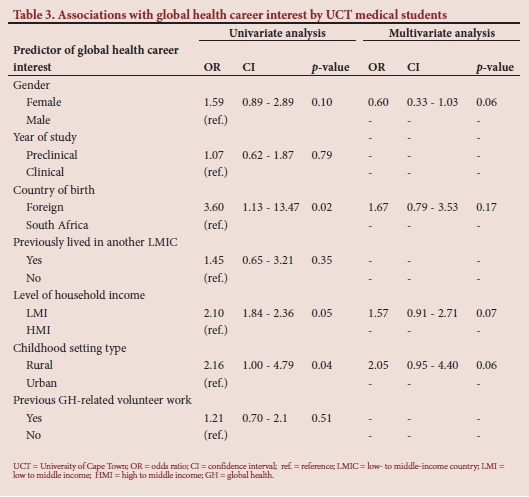
Logistic regression was used to model factors associated with global health career interest (Table 3). On univariate analysis, the following factors were associated with an increased likelihood of global health career interest: being born in a foreign country (odds ratio (OR) 3.6; p=0.02); being raised in a low- to middle-income household (OR 2.1; p=0.05); and a childhood in a rural setting (OR 2.16; p=0.04). On multivariate analysis, there were no significant associations with an interest in a global health career. Previous GHE (n=66; 27%) was not associated with a career interest in global health (OR 1.21; p=0.51), nor was there a significant association with having a specific career choice and wanting to work in global health practice. Other predictors assessed included gender, year of study and student society involvement, but these were not found to be significantly associated (Table 3).
Perceptions of contributions by specific medical specialties to global health
Perceptions of the contribution of various medical specialties to global health are shown in Fig. 3. ID was the most common response (n=171; 70%), followed by OBGYN (n=107; 44%) and FM (n=98; 40%). ID (n=111; 45%), FM (n=99; 40%) and OBGYN (n=68; 28%) were also perceived as the medical specialties that would have the highest global health impact during the next 25 years. Surgery ranked low for both its perceived impact on global health delivery in the past 25 years and in the next 25 years (n=28; 11% and n=41; 17%, respectively). Psychiatry (n=125; 62%) and surgery (n=51; 21%) were considered the top two specialties that respondents believed should be global health priorities, but that are not currently prioritised by national or international agendas. FM (n=172; 70%) was the most commonly selected medical specialty as the best indicator for a robust health system in terms of universal health coverage, while surgery was the least common (n=1; <1%).
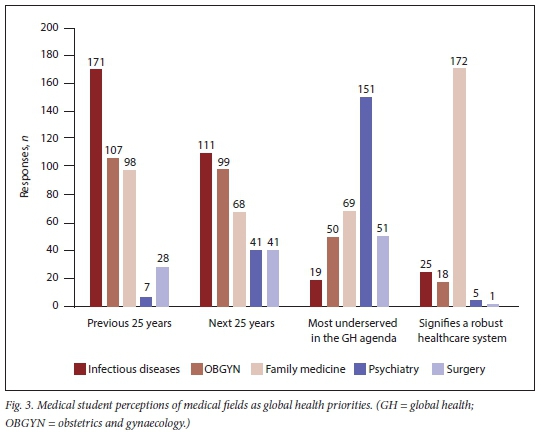
ID was regarded as having the largest focus on preventive care and being the most likely medical specialty in which to integrate a career in global health. FM was regarded as the most cost-effective specialty to address global health in resource-limited settings. Surgery ranked lowest in all fields.
Discussion
The current study found that the majority of UCT medical students reported no formal or informal GHE. Nonetheless, most students were interested in incorporating global health in their future careers; this interest should be leveraged. The knowledge and perceptions of students towards global health help to inform the contextual discourse around the field; however, with such limited exposure to GHE, factors contributing to these perceptions should be explored and approaches for addressing misperceptions through focused GHE prioritised.
The HIV/AIDS epidemic, which has affected southern Africa disproportionately compared with other regions, defined the field of global health as uniting international funders, scientists and civil society to work together to reduce new infections and decrease mortality.[11] Due to its infectious disease origins, general perceptions of global health are often narrow and not inclusive of other essential fields. In addition, because global health is historically derived from public health,[11] as well having a strong focus on health access and equity, it is often limited to more traditionally 'primary healthcare' specialties such as FM and OBGYN.[12] This limitation may account for the perceptions held by UCT students and their prioritisation of medical fields within global health.
Today, global health examines health priorities transnationally and espouses a multifaceted, interdisciplinary approach to addressing health challenges that are no longer restricted to disease-based and clinical interventions.[12] Global health leaders and advocates have imperatively called for the inclusion of medical school curricula to improve the preparation of medical students to engage with and understand the tenets of global health.[4,12]
Students' knowledge of global surgery was very limited. Surgery was consistently ranked low in terms of its contribution across various perceived aspects of global health. Furthermore, it was considered as the medical field that was least amenable to a career in global health. Recently, however, surgery has been shown to be an indispensable field within the scope of global health.[13] Surgery requires strong infrastructure with regard to training, interdisciplinary co-operation and cost-effectiveness, and has been proposed as the best indicator of a robust healthcare system.[2] However, <1% of medical students agreed with this statement. This undervaluing of global surgery was also found in a comparable US study,[3] recapitulating the existing global misperception that surgery is a costly and inefficacious component of healthcare and has historically been neglected on the global health agenda.[14]
Our study also provides invaluable insights into how students prioritise other fields within global health. Notably, unlike surgery, where participants demonstrated limited insight into its significant contribution towards global health, the majority of students held an astute perception of current underservice of mental health and its warranted inclusion in the global health agenda, exemplified by its inclusion in the SDGs.[6]
Much of global health should be prioritised in LMICs; therefore, formal GHE in Africa is imperative. However, global health centres and training programmes are unintuitively concentrated in HICs.[1] In 2017, UGHE was launched in Rwanda, marking the first African dedicated global health centre that incorporated global health concepts throughout the medical school curriculum. It defined a new type of educational system in healthcare with an African identity - restructuring curricula to equip medical students to deliver equitable health services.[15] As far as we are aware, this is the only African medical school that has incorporated specific global health competencies into their formal curriculum, and not formally using CUGH domains. SA medical schools should consider restructuring their medical school currciula to incorporate formal global health competencies using the CUGH framework.[16]
With the increasing view that health between countries is inter-related, it has been argued that all medical students should be provided dynamic training in core global health competencies that can be applied across all medical fields, and to address perceived gaps in GHE.[17] To amend inaccurate perceptions of global health and to improve the preparation of medical students, specific global health learning outcomes, including global surgery, have been proposed.[18] Nevertheless, there is no consensus on standardisation in GHE.[1,9] Moreover, redefining the global health agenda in SA also provides an opportunity to address key misperceptions highlighted by this study and to integrate previously neglected fields, particularly global surgery. The perceptions highlighted in this study may help to inform key gaps in knowledge and areas of focus for a context-specific global health curriculum. We suggest that formal global health competencies be incorporated into SA medical school curricula, guided by the CUGH framework.
In the past, GHE ofHIC students has largely hinged on the provision of a clinical or research rotation in LMICs.[9] These elective experiences not only have a significant impact on student development in clinical skills and cultural competencies,[19,20] but are also an independent predictor of interest in a global health career and future practice in underserved communities.[21-23] As is the case at many other universities, students spend the major part of their training in the resource-limited public sector health system, often working in health facilities in extremely poor neighbourhoods and witnessing health inequities. Notably, students from a perceived rural childhood setting were more interested in pursuing a career in global health. Mirroring global trends, SA rural communities are typically poorer and experience greater barriers in accessing quality healthcare.[24] This exposure to learning in resource-poor settings is uniquely positioned to engage SA students in a global health curriculum. SA has the capacity to harness the benefits of training in resource-poor settings and integrate this training into a global health curriculum to foster future global health leaders.
Developing a comprehensive global health medical school curriculum for the SA context requires interdisciplinary input and collaboration. Furthermore, a wider variety of skills and knowledge training is required to analyse the impact of major social, economic, political, cultural and environmental factors that influence healthcare.[12]
Study limitations
We acknowledge that this study has several limitations. This was a single-institution study and may not be representative of the perceptions of students of other SA institutions; there was a relatively low response rate; and the responses were self-reported (as opposed to validated or standardised questions), which are subject to bias owing to varying interpretation of the questions by different participants. While the survey highlighted some key perceptions, the response options limited the depth of response interpretation, potentially warranting future qualitative interview- and focus group-based research. Further research should be undertaken to evaluate students' perceptions of what should be included in a future global health curriculum.
Conclusion
GHE is gaining traction as a potentially influential tool for achieving health equity and for broadening the scope of future health professionals, particularly in LMICs.[25] This study suggests that while the majority of UCT medical students are interested in a career involving global health, they need a more formalised education curriculum. Interpreting students' attitudes towards and perceptions of global health may help to inform an appropriate curriculum in SA. Incorporating specific GHE into medical curricula may serve to amend the misperceptions and encourage future leaders in global health. CUGH's 11 global health competency domains could be a useful framework.
Declaration. None.
Acknowledgements. I wish to thank Prof. Kathryn Chu, Dr Priyanka Naidu and Ms Megan Naidoo for their guidance and support.
Author contributions. Conception of the study: MP, LP, KC; literature review: MP; data cleaning: MP; statistical analysis: MP, PN; data interpretation: MP, PN LP, KC; writing of the article: MP, PN; review/editing of article: MP, PN, LP, KC.
Funding. None.
Conflicts of interest. None.
References
1. Gukas ID. Global paradigm shift in medical education: Issues of concern for Africa. Med Teach 2007;29(9-10):887-892. https://doi.org/10.1080/01421590701814286 [ Links ]
2. Meara JG, Leather AJ, Hagander L, et al. Global surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Int J Obstet Anesth 2016;25:75-78. https://doi.org/10.1016/j.surg.2015.02.009 [ Links ]
3. Cox JT, Kironji AG, Edwardson J, et al. Global health career interest among medical and nursing students: Survey and analysis. Ann Glob Health 2017;83(3-4):588-595. https://doi.org/10.1016/j.aogh.2017.07.002 [ Links ]
4. Jogerst K, Callender B, Adams V, et al. Identifying interprofessional global health competencies for 21st-century health professionals. Ann Glob Health 2015;81(2):239. [ Links ]
5. Ataguba JE, Akazili J, McIntyre D. Socioeconomic-related health inequality in South Africa: Evidence from general household surveys. Int J Equity Health 2011;10:48. https://doi.org/10.1186/1475-9276-10-48 [ Links ]
6. Griggs D, Stafford-Smith M, Gaffney O, et al. Sustainable development goals for people and planet. Nature 2013;495(7441):305. [ Links ]
7. Drain PK, Holmes KK, Skeff KM, Hall TL, Gardner P. Global health training and international clinical rotations during residency: Current status, needs, and opportunities. Acad Med 2009;84(3):320-325. https://doi.org/10.1097/acm.0b013e3181970a37 [ Links ]
8. Jeffrey J, Dumont RA, Kim GY, Kuo T. Effects of international health electives on medical student learning and career choice: Results of a systematic literature review. Fam Med 2011;43(1):21-28. [ Links ]
9. Mehta AXT, Murray M, Casey KM. Medical student perceptions of global surgery at an academic institution: Identifying gaps in global health education. Acad Med 2017;92:1749-1756. [ Links ]
10. Gwatkin DR, Ergo A. Universal health coverage: Friend or foe of health equity. Lancet 2011;377(9784):2160-2161. https://doi.org/10.1016/s0140-6736(10)62058-2 [ Links ]
11. Brandt A. How AIDS invented global health. N Engl J Med 2013;368(23):2149-2152. https://doi.org/10.1056/nejmp1305297 [ Links ]
12. Yudkin JS, Bayley O, Elnour S, Willott C, Miranda JJ. Introducing medical students to global health issues: A Bachelor of Science degree in international health. Lancet 2003;362(9386):822-824. https://doi.org/10.1016/s0140-6736(03)14276-6 [ Links ]
13. Göpfert A, Mohamedbhai H, Mise J, et al. Do medical students want to learn about global health? Glob Health Action 2014;7:23943. https://doi.org/10.3402/gha.v7.23943 [ Links ]
14. Koplan JP, Bond TC, Merson MH, et al. Towards a common definition of global health. Lancet 2009;373(9679):1993-1995. https://doi.org/10.1016/s0140-6736(09)60332-9 [ Links ]
15. Binagwaho A. University of Global Health equity's contribution to the reduction of education and health services rationing. Int J Health Policy Manag 2017;6(8):427-429. https://doi.org/10.15171/ijhpm.2017.56 [ Links ]
16. Mullan F, Frehywot S, Omaswa F, et al. Medical schools in sub-Saharan Africa. Lancet 2011;377(9771):1113-1121. https://doi.org/10.1051/pmed/2011026 [ Links ]
17. Saba N, Brewer TF. Beyond borders: Building global health programs at McGill University Faculty of Medicine. Acad Med 2008;83(2):185-191. https://doi.org/10.1097/acm.0b013e31816094fc [ Links ]
18. Johnson O, Bailey SL, Willott C, et al. Global health learning outcomes for medical students in the UK. Lancet 2012;379(9831):2033-2035. https://doi.org/10.1016/s0140-6736(11)61582-1 [ Links ]
19. Cherniak WA, Drain PK, Brewer TF. Educational objectives for international medical electives: A literature review. J Assoc Am Med Coll 2013;88(11):1778-1781. https://doi.org/10.1097/acm.0b013e3182a6a7ce [ Links ]
20. Kumwenda B, Royan D, Ringsell P, Dowell J. Western medical students' experiences on clinical electives in sub-Saharan Africa. Med Educ 2014;48(6):593-603. https://doi.org/10.1111/medu.12477 [ Links ]
21. Adams LV, Wagner CM, Nutt CT, Binagwaho A. The future of global health education: Training for equity in global health. BMC Med Educ 2016;16(1):296. https://doi.org/10.1186/s12909-016-0820-0 [ Links ]
22. Haq C, Rothenberg D, Gjerde C, et al. New world views: Preparing physicians in training for global health work. Fam Med 2000;32(8):566-572. [ Links ]
23. Gjerde CL, Rothenberg D. Career influence of an international health experience during medical school. Fam Med 2004;36(6):412-416. https://doi.org/10.1186/s12909-015-0483-2 [ Links ]
24. Harris B, Goudge J, Ataguba JE, et al. Inequities in access to health care in South Africa. J Public Health Policy 2011;32(Suppl 1):S102-S123. https://doi.org/10.1057/jphp.2011.35 [ Links ]
25. Liu Y, Zhang Y, Liu Z, Wang J. Gaps in studies of global health education: An empirical literature review. Glob Health Action 2015;8:25709. https://doi.org/10.3402/gha.v8.25709 [ Links ]
 Correspondence:
Correspondence:
M Potter
matthew.potter@alumni.uct.ac.za
Accepted 5 November 2020














