Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.12 n.2 Pretoria Jun. 2020
http://dx.doi.org/10.7196/AJHPE.2020.v12i2.1182
RESEARCH
Enhancement of plastic surgery training by including simulation in education and training programmes
C P G NelI; G J van ZylII; M J LabuschagneIII
IMB ChB, MHPE, FC Plast Surg (SA), MMed (Plastic Surgery), PhD; Department of Plastic and Reconstructive Surgery, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIMB ChB, MFamMed, PhD; Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIMB ChB, MMed (Ophthalmology), PhD; School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: This research investigated the possibility of integrating simulation in plastic surgery residency training. The problem addressed was the lack of knowledge about using simulation as a teaching method to enhance the training of plastic surgeons. There was a lack of empirical evidence regarding learning outcomes that could be mastered by simulation-based education and training and their specific cognitive levels
OBJECTIVES: To identify and describe: (i) learning outcomes for plastic surgery education and training for which simulation might be an important (essential and useful) training method; and (ii) simulation modalities, linked to specific cognitive levels, to establish the influence of simulation on plastic surgery education and training. The objectives entail determining the importance of simulation in plastic surgery training and identifying simulation modalities most suited to attain specific outcomes
METHODS: Data were collected by means of a Delphi survey to obtain consensus from an expert panel comprising 9 plastic surgeons, supplemented by semi-structured interviews conducted with 8 national and international role players in simulation and postgraduate education
RESULTS: Learning outcomes, levels of training, possible simulation modalities, cognitive levels and descriptive verbs and phrases were described, as these pertain to learning. Participants agreed that simulation in medical education can be used to enhance postgraduate plastic surgery training, with special reference to specific outcomes and cognitive levels. Participants made recommendations for the planning and support of the implementation, aimed at ensuring the quality of training
CONCLUSION: The objectives set were achieved and the results of the study serve as encouragement and guidance in the striving for the enhancement of postgraduate plastic surgery education and training, and in other medical disciplines
Simulation is in widespread use for professional health education; however, by itself, it is not a guarantee that adequate learning will occur. Simulation has to be integrated with the outcomes of the curriculum, applicable simulation modalities have to be used, the learning environment must be conducive to education and training, and the features and uses of simulation have to be optimally and correctly incorporated into the training programme.[1] To revolutionise medical education, an increased efficiency of education by standardising the curriculum, an individualisation of education and a shift from time-based training to competency-based training are essential.[2] Residents (registrars/specialists in training) may receive little guidance in terms of the knowledge, competencies, skills and attitudes that they are expected to acquire during residency. Surgical training in the 21st century is characterised by an increasingly objective, standardised approach using equipment such as simulators to optimise patient safety, surgical care and hospital resources, and to minimise errors.[3] The driving forces behind this are developments in medical error statistics, evidence-based medicine and fewer attending hours. Through increased accuracy, simulation can improve results and lower risk and procedure cost because of fewer procedures and less operating room time.[3]
The Accreditation Council for Graduate Medical Education (ACGME) and the American Board of Medical Specialties (ABMS) identify six core competencies for residents: patient care, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism and systems-based practice.[4] A joint initiative of the ACGME and ABMS, the Plastic Surgery Milestone Project, compiled descriptors and targets for residents' performance, based on the abovementioned core competencies. These descriptors and targets (outcomes) are categorised at five training levels, starting at level 1, where the resident demonstrates the mastering of milestones expected of an incoming resident, moving up to level 5, where the resident has advanced beyond performance targets set for residency and can graduate.[5]
Simulation represents a safe and standardised postgraduate training method, and provides a yardstick for gauging residents' ability to perform certain procedures, surgery and teamwork in a clinical setting.[4] The American College of Surgeons (ACS) introduces simulation in training and education for general surgery in three phases, i.e. skills training, procedure training and team training. Plastic surgery should follow this simulation initiative with modifications appropriate to the specialty.[4] Phase 1, skills, is included in the residents' general surgery training, but phase 2, procedures, focuses on the development of procedures specific to plastic surgery. For phase 3, competencies in teamwork, the competencies for plastic surgery resemble those for general surgery and include team-training simulators to improve communication in emergency departments, clinics, operating rooms and hospital wards.[4]
In many plastic surgery programmes it is problematic to balance clinical, hands-on education and training with the didactic programme.[6] Work and duty-hour restrictions add another layer of complexity to surgical education. The rate-limiting step in learning is not the transmission of information from the teacher to the learner, but the processing of the information by the learner.[6] Educational technology offers unique tools to help learners acquire and process the information needed to become masters in their surgical specialty.[6]
To understand the concepts of learning effectiveness and learning at different cognitive levels or domains of competence, necessitates examining learning theories and making these applicable to plastic surgery. According to Kolb's learning cycle,[7] learners must have a concrete experience on which to reflect. Through their reflection, students are able to formulate abstract concepts and make appropriate generalisations, after which they solidify their understanding by testing the implications of their knowledge in new situations. This provides them with an objective experience, and the cycle continues. Learners with different learning preferences will have strengths in different quadrants of Kolb's cycle.[7]
To build knowledge and understanding, learners need to understand the 'context of an unknown learning situation'.[7] This can be achieved through a process called instructional scaffolding,[8] during which sufficient support is provided to promote learning when concepts and skills are introduced to students. This support may include resources such as a list of intended learning outcomes when they enter the programme or a new clinical environment.[7] Learning outcomes should be formulated using Bloom's taxonomy, designating the levels of cognition, i.e. knowledge, understanding, application, analysis, synthesis and evaluation.[8,9] Anderson's adapted version of this taxonomy uses verbs to describe the six levels of cognition (levels 1 - 6), i.e. remember, understand, apply, analyse, evaluate and create.[8] Subsequently, in medical education, scales were developed to indicate competence, the most frequently encountered being Miller's pyramid,[9,10] which builds up from knowledge of (knows how), to competence in performance and independent action (shows how). This pyramid can be used as a guide for planning and assessing student learning, especially the mastery of skills.[10] A relationship is recognised between Miller's pyramid for developing skills and competence and the type of simulator most appropriate for each level, as well as the degree of simulator fidelity and the nature of skills that can be developed with each type of simulator.[11] A comparison between Bloom's taxonomy and Miller's pyramid can also be drawn.[12] Bloom's levels of remembering and understanding equal Miller's knowledge, while application boils down to know how and show how (competence), and analysing, evaluating and creating can be equalised with Miller's doing and integrating into practice (independent action).[13] Simulation can be applied to developing and demonstrating higher-order levels of thinking, which approximate the levels of thinking required in clinical practice.[12] With the development of simulator technology providing greater degrees of fidelity, simulators can be employed as precision instruments in the measurement of performance in the clinical setting. Simulation makes it possible to assess the development from the 'knows how' to the 'shows how' category in Miller's framework.[14] Simulators are valid instruments for use in assessment, on condition that the simulator type has sufficient fidelity to elicit the expected competencies and performance level, and students have had previous exposure to the simulators during training.[11,12]
Aims and objectives
The aim of the larger study was to identify and describe: (i) learning outcomes for plastic surgery education and training for which simulation might offer an important (essential and useful) training method; and (ii) simulation modalities, linked to specific cognitive levels, to establish the influence of simulation on plastic surgery education and training as far as knowledge, skills, clinical competence and professional conduct are concerned. The objectives discussed in this article are those set to:
(i) determine the importance of simulation in plastic surgery training;
(ii) identify simulation modalities most suited to attain specific outcomes; and (iii) determine whether simulation can enhance student learning at different cognitive levels.
Methods
A descriptive research design was followed, and a qualitative and quantitative approach was regarded best suited to attain the objectives.[13] The methods used to attain the objectives mentioned above, were: (i) a Delphi survey; and (ii) semi-structured interviews. These two data collection methods are discussed separately.
Delphi survey
Data collection
Data were collected using a survey questionnaire, which consisted of three parts: part 1 (questions regarding the importance of simulation as a method) comprised items in two main categories, i.e. medical knowledge and patient care, with 18 sections in total, divided into five education and training levels totalling 453 learning outcomes. These learning outcomes for the Delphi survey were developed (adapted) from the literature[6] and categorised in training levels used as point of departure in compiling the Delphi questionnaire.[6]
The participants (panel members) had to indicate the importance of simulation as an education and training method for each of the outcomes by indicating whether simulation was an essential method, a useful method or not applicable/important in training a plastic surgeon as far as a specific outcome was concerned. In part 2 of the questionnaire (simulation modalities), the participants had to give their opinions on each learning outcome and indicate which type of simulation modality (low-tech simulation or high-tech simulation) would be best suited for achieving a learning outcome. In part 3 of the questionnaire (cognitive levels), the participants had to indicate which level of learning should be addressed by simulation to achieve the specific outcome.
Sample
Nine experts in plastic surgery and clinical simulation were selected purposively according to a set of criteria (approved by the Evaluation and Ethics Committee, Faculty of Health Sciences, University of the Free State (UFS), Bloemfontein, South Africa (SA)). The main criteria were expertise and experience in the field of the study.[14] The selected experts who agreed to participate in the Delphi process were qualified plastic surgeons -knowledgeable about medical education, serve as policymakers, leaders and managers in postgraduate education and are of high national and international academic and scientific standing.
The aim of the Delphi process was to reach a level of consensus among participants on the statements in the questionnaire. For this study 66.7% (n=6/9) of participants was regarded as consensus.[13,15]
Data analysis
The researcher analysed the data. Responses were entered into a computer spreadsheet for the calculation of consensus or stability. The results were reported separately, listing the experts' comments on simulation as a method to train plastic surgeons, the uses and applicability of simulation modalities, as well as the levels of cognition that might be addressed by simulation.
Reliability and trustworthiness
Reliability was ensured by making use of a pilot study, determining strict criteria in sample selection, and by using a carefully constructed Delphi questionnaire based on a detailed literature study. The pilot study entailed pretesting of the Delphi questionnaire by a plastic surgeon, a medical education specialist and a clinician; no changes were recommended. Reliability was ensured by carefully constructed and tested Delphi questionnaires and interview guides. Trustworthiness of the qualitative study was ensured by subjecting the research protocol to the Evaluation and Ethics Committee, Faculty of Health Sciences, UFS, by conducting an in-depth literature study and by providing a thorough description of the research project, as well as written feedback to the participants.
Semi-structured interviews Data collection
Interviews were conducted to obtain an in-depth, comprehensive overview of the contribution of simulation to postgraduate plastic surgery education and training. An interview guide, developed by the first author (CPGN) on the basis of a literature review, was used.
The questions used in the interview guide were as follows (with the objectives to which they are linked in brackets):
• Can simulation be used to enhance student learning at different cognitive levels? (Objective (i): to determine whether simulation can enhance student learning at different cognitive levels.)
• Which types of simulation or simulation modalities might lead to effective learning? (Objective (ii): to identify simulation modalities most suited to attain specific outcomes.)
• Any recommendation(s) you would like to make when considering including simulation in specialist training? (Both the aim and the objectives.)
Questions 1 - 4, 7 - 11 and 13 are not included here, because the data are not directly applicable to the objectives of this article. The findings reported regarding questions 3, 4 and 7 were dealt with in an article, 'Simulation in plastic surgery: Features and uses that lead to effective learning'.[14]
Sample
Professionals with experience in simulation and postgraduate education were requested to participate in the semi-structured interviews. Participants, selected according to a set of criteria, were directors of simulation units, heads of clinical medical departments, programme directors of medical and nursing programmes, education management specialists, researchers and representatives from the simulation industry. The sample size was determined by the point of data saturation, i.e. when no new information was offered. Written consent was obtained from the participants.
Data collection
The first author (CPGN) conducted individual interviews based on a single interview guide with 8 participants. All interviews were audio-recorded, transcribed by the interviewer and checked by an individual who was not part of the study. Field notes taken during the interviews contributed to the data.
Data analysis
Data were analysed using the grounded theory approach that requires continued comparison of data, following the data analysis steps of coding, categorisation and theory generation.[16] Theory building occurred by finding patterns in the data, which continued until saturation of data was reached. [17]
Reliability and trustworthiness
Reliability was ensured by making use of explorative studies, determining strict criteria for sampling, using the carefully constructed interview guide, as well as an interview process that was audio-taped, transcribed and carefully described. Trustworthiness of the interviewing process was ensured by involving voluntary interviewees with a clear understanding of what the interviewer expected from them, and using open-ended questions, as well as transcribing of and verifying the accuracy of data. Scientific record-keeping ensured dependability.
Ethical approval
Ethical approval to conduct the research was obtained from Health Sciences Research Ethics Committee, UFS (ref. no. ECUFS 122/2015).
Results
Data collected by means of parts 1 - 3 of the Delphi questionnaire survey and questions 5, 6 and 12 of the semi-structured interviews are reported. Data on simulation modalities and cognitive levels are summarised and qualitative perspectives are shared on how simulation can be used to enhance student learning at different cognitive levels, as well as on the types of simulation modalities that may lead to effective learning. Recommendations made by the interviewees are discussed with a view to possibly including simulation in specialist training.
Delphi survey (parts 1 - 3)
After completing round 2 of the Delphi process, sufficient consensus (92.05%) was achieved and the process came to an end. Participants indicated that they would not be changing their answers in a third round. The results are summarised in Table 1.
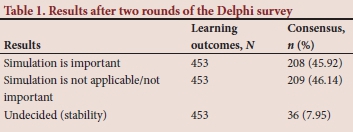
Consensus was reached on 45.92%, i.e. 208 of the 453 learning outcomes (descriptors in the form of statements), indicating that simulation as a method of training for plastic surgeons was important. Consensus was reached on 209 (46.14%) statements, indicating that simulation was not applicable/not important as a method of training. Consensus could not be reached on 36 (7.95%) statements, but stability was reached.
The results of the 18 sections of the Delphi questionnaire were summarised. Each section dealt with the learning outcomes categorised on five education and training levels indicated as L1 - 5. The first statements related to medical knowledge, while the statements in the second part (in italics) related to patient care.
The participants in the Delphi survey indicated where simulation might play a role of importance and be of value as one of the training methods in the specialist training of plastic surgeons. The Delphi participants indicated which type of simulation modality, i.e. low-tech and/or hightech, could be applied, and the cognitive level that would be addressed by the simulation. The different descriptive phrases/verbs that were used to formulate these specific learning outcomes at the five education and training levels, and the proposed simulation modality and cognitive levels at which learning will take place, are described. This was done to serve as an example and to provide an overview of the data that had been gathered during the Delphi process.
The section on surgical care (section 1), which consisted of the main categories, i.e. medical knowledge and patient care, resulted in 14 learning outcomes (covering five training levels) indicated by the Delphi panel as outcomes for which simulation can be used as a training method. The schematic overview includes descriptive verbs (underlined in the Delphi questionnaire), simulation modalities and cognitive levels (Fig. 1).
Statements on medical knowledge are in ordinary print and statements on patient care are in italics.
It is important to understand that by changing the action verb in an outcome or by formulating a simulation scenario at a higher cognitive level, learning that may occur will be at a higher cognitive level and will influence the effectiveness of learning.
The discussion on section 1, i.e. surgical care, serves as an example (Fig. 1). Simulation was indicated as a possible method for training plastic surgeons at different cognitive levels related to the training level, using low- and/or high-tech simulation modalities and simulated patients. The underlined verbs/action words (Fig. 1) give an indication of the cognitive level at which learning most probably will take place.
The other sections that were addressed (in the sequence in which they appeared in the Delphi questionnaire) are wound care, tissue transfer, congenital anomalies, head and neck, maxillofacial trauma, facial aesthetics, non-cancer breast surgery, breast reconstruction, reconstruction of trunk and perineum, upper-extremity trauma, non-trauma hand, cosmetic trunk and lower extremity, lower extremity, system-based practice, practice-based learning and improvement, professionalism and interpersonal and communication skills.
Twenty learning outcomes indicated by the participants to be attained through simulation were in the sections on system-based practice (including patient safety, resource allocation and practice); six of the 20 were in the domain of patient safety. The section on practice-based learning and improvement, including investigate, evaluate and assimilate, entailed five learning outcomes, while research and training had four learning outcomes.
In the section on professionalism (ethics and values, and personal accountability), the participants in the Delphi survey indicated three learning outcomes that may be attained by simulation; these were in the domain of personal accountability.
In the interpersonal and communication skills section, participants indicated two learning outcomes that may be attained through simulation. Although the participants indicated fewer outcomes to be attained by means of simulation in the domain of the softer skills, it must be emphasised that they were of the opinion that simulation was applicable at the higher cognitive levels, mostly cognitive level 6, i.e. evaluate and create.
Semi-structured interviews
The enhancement of student learning through simulation at different cognitive levels, and the types of simulation modalities that may lead to effective learning, were addressed by the first two questions to the interviewees. Simulation provides the opportunity to learn at different cognitive levels, e.g. remembering information (during preparation, understanding and applying, using low-fidelity simulators); analysing and evaluation (using high-fidelity simulators); and developing and formulating new concepts and ideas. Using interprofessional teams in multipurpose, complex scenarios, with real-world experiences, can ensure learning at different cognitive levels. Simulated patients play an important role in the training of registrars in a safe environment. The curriculum outcomes must be aligned with the objectives of simulation; however, using both low- and high-tech modalities while training and experiencing the holistic scenario will emphasise integration, group work and the multidisciplinary approach.
Recommendations (made by the interviewees when considering including simulation in specialist training - the third question) were focused on curriculum and training initiatives, aspects that should be in place, and suggestions on planning and support aimed at ensuring the quality of training. The emphasis should be on employing persons knowledgeable in curriculum and simulation development.
Data gathered by means of the semi-structured interviews were triangulated with data gathered through parts 1 - 3 of the questionnaire survey, and by means of the literature review, to identify aspects for compiling a framework to serve as a directive when considering the inclusion of simulation as one of the methods to train plastic surgeons.
Discussion
This discussion of learning outcomes, levels of training, possible simulation modalities, cognitive levels and descriptive verbs and phrases pertaining to learning, paved the way for investigating the role of simulation in medical education. Recommendations for considering the inclusion of simulation in specialist training were offered.
Of the proposed learning outcomes for plastic surgery training, the participants in the Delphi survey reached consensus that 45.92% of the proposed learning outcomes for such training could be supported by including simulation as an instructional method in the postgraduate education and training programme. The participants thought that simulation should be implemented progressively at all five training levels during the training years. In the earlier years of training, students should concentrate more on remembering and understanding concepts, followed by the mastering and application of skills, demanding analysis, evaluation and creating (synthesis) in the later years of training as proposed in the literature.[10]
The Delphi participants expressed the opinion that simulation is an important method for training students in medical knowledge, skills, competencies and patient care; however, they did not favour simulation as a teaching method for the 'softer skills', e.g. team training, patient safety, interpersonal and communication skills, professionalism, ethics, values and personal accountability, although the literature suggests that soft skills also be trained through simulation.[18,19] Delphi participants emphasised the importance of these skills being trained at higher cognitive levels to reach maximum competency and proficiency in professional conduct.
With regard to the type of simulators used, the participants agreed that the simulation type should be in line with the objectives/stated outcomes of the scenarios: scenarios involving higher cognitive levels would demand learning with the use of high-tech simulators and simulated patients. Simulation provides opportunities for learning that involve different cognitive levels. It is important to identify the competence/expertise/ proficiency that is required at each training level and for the qualified professional, as also pointed out in the literature.[11,12]
When introducing simulation in specialist training, the following is recommended:
• Develop an integrated, structured education and training system, including theoretical lectures, simulation sessions and clinical work on real patients - striving to find a balance between the different components.
• Align the simulation plan with the curriculum according to a scientific and co-ordinated process and guidelines.
• Develop a training course for trainers before implementing simulation in the plastic surgery programme.
• Research the role of simulation in assessment carefully before implementation.
• Evaluate the workplace environment on a continuous basis and carefully consider feedback received from role players.
From the results of this study, and supported by the literature,[2-5,11-14,20,21] a clear reasoning process built the argument favouring the implementation of simulation in postgraduate plastic surgery education and training programmes. The study results clearly indicate that certain processes must be in place and steps should be taken to ensure that adequate learning will occur, and that simulation outcomes are integrated with the objectives and outcomes of the curriculum in an environment that is conducive to learning. It is evident from the research that simulation in plastic surgery education and training programmes will enhance effective learning, but further research is needed for ultimate success.[13,22]
Conclusion
Aspects worthy of further investigation with a view to integrating simulation successfully in postgraduate plastic surgery education and training programmes include considerations and challenges for effective and efficient implementation of appropriate simulation modes. Another aspect that needs to be investigated more profoundly is the use of simulation for assessment in medical education and training. Recommendations for compiling guidelines for the implementation of simulation as part of postgraduate plastic surgery education and training programmes must be compiled to serve as a directive.
Therefore, having determined that simulation does make a contribution to plastic surgery education and training, and having identified outcomes that can be attained best by using specific (identified) simulation modes, we trust that the objectives achieved through this study will serve as encouragement and guidance in the striving for the enhancement of postgraduate plastic surgery education and training, and in other medical disciplines.
Declaration. None.
Acknowledgements. The authors gratefully acknowledge the assistance received from: (i) the participants in the study, who were willing to take part in the pilot testing and quality control of the Delphi questionnaires, and the role players in the explorative study conducting the exploratory interviews; (ii) the Delphi panel and interviewees involved in the research for their valuable contributions and their time in completing the questionnaires and participating in individual semi-structured interviews; (iii) Prof. G Joubert, head, Department of Biostatistics, Faculty of Health Sciences, UFS, for her advice during the early stages of the research, protocol development and quality assurance of the study; and (iv) Dr H Bezuidenhout, UFS, for support regarding the scientific formulation and language editing of the manuscript, as well as editing of the references.
Author contributions. CPGN designed the study, compiled the protocol, collected data and performed the analysis, interpreted data and wrote the manuscript; GJvZ and MJL were promotors of the study, reviewed the protocol and manuscript and contributed substantially to the conceptualisation, design, analysis and interpretation of data and scientific content. All authors approved the final version of the manuscript.
Funding. This research was partially funded by a grant from the Health and Welfare Sector Education Training Authority (HWSETA).
Conflicts of interest. None.
References
1. Issenberg SB, McGaghie WC, Petrusa ER, et al. Features and uses of high-fidelity medical simulations that lead to effective learning. Med Teach 2005;27(1):10-28. https://doi.org/10.1080/01421590500046924 [ Links ]
2. Satava R. Emerging trends that herald the future of surgical simulation. Surg Clin North Am 2010;90(3):623-633, https://doi.org/10.1016/j.suc.2010.02.002 [ Links ]
3. Rosen JM, Long SA, McGrath DM, Greer SE. Simulation in plastic surgery training and education: The path forward. Plast Reconstr Surg 2009;123(2):729-738. https://doi.org/10.1097/PRS.0b013e3181958ec4 [ Links ]
4. Mittal MK, Duman KR, Edelson PK, et al. Successful implementation of the American College of Surgeons/ Association of Program Directors in Surgery, Surgical Skills Curriculum via a 4-week consecutive simulation rotation. Soc Simul Health 2012;7(3):147-154. https://doi.org/10.1097/SIH.0b013e31824120c6 [ Links ]
5. American Board of Medical Specialists and Accreditation Council for Graduate Medical Education. The Plastic Surgery Milestone Project. A joint initiative. 2013. J Grad Med Educ 2014;6(1s1):225-242. https://doi.org/10.4300/JGME-06-01s1-24 [ Links ]
6. Neumeister MW. Technology and education: The future of plastic surgery training. Plast Reconstr Surg Glob Open 2016;4(6):e777. https://doi.org/10.1097/GOX.0000000000000780 [ Links ]
7. Bloom BS, Engelhart MD, Furst EJ, Hill WH, Kratwohl DR. Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook I, Cognitive Domain. New York: Longmans Green, 1956. [ Links ]
8. Taylor DCM, Hamdy H. Adult learning theories: Implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach 2013;35:e1571-e1576. https://doi.org/10.3109/0142159X.2013.828153 [ Links ]
9. Atherthon JS. Learning and teaching Bloom's taxonomy. 2011. https://www.economicsnetwork.ac.uk/archive/atherton_learning/bloomta (accessed 15 May 2020). [ Links ]
10. Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65(9):S63-S67. [ Links ]
11. Alinier GP. A typology of educationally focused medical simulation tools. Med Teach 2007;29(8):e243-e250. https://doi.org/10.1080/01421590701551185 [ Links ]
12. Labuschagne MJ. Clinical simulation to enhance undergraduate medical education and training at the University of the Free State. PhD thesis. Bloemfontein: University of the Free State, 2012:1-282. [ Links ]
13. Nel CPG. Simulation in postgraduate plastic surgery education and training. PhD thesis. Bloemfontein: University of the Free State, 2019:11-13. [ Links ]
14. Nel CPG, van Zyl GJ, Labuschagne MJ. Simulation in plastic surgery: Features and uses that lead to effective learning. Afr J Health Professions Educ 2020 (accepted). [ Links ]
15. Dajani JS, Sincoff MZ, Talley WK. Stability and agreement criteria for the termination of Delphi studies. Technol Forecast Social Change 1979;13(1):83-90. 'https://doi.org/10.1016/0040-1625(79)90007-6 [ Links ]
16. Byrne M. Grounded theory as a qualitative research methodology - brief article. AORN J 2001;73(6):1155-1156. https://doi.org/10.1016/S0001-2092(06)61841-3 [ Links ]
17. Labuschagne MJ, Nel MM, Nel PPC, van Zyl GJ. Recommendations for the establishment of a clinical simulation unit to train South African medical students. Afr J Health Professions Educ 201446(2):2-6. https://doi.org/10.7196/AJHPE.534 [ Links ]
18. Arbogast P, Rosen J. Simulation in plastic surgery training: Past, present and future. IntechOpen 2012:235-256. https://doi.org/10.5772/28550 [ Links ]
19. Scalese RJ. Energising medical education through simulation: Powering minds, not just machines. Proceedings of the 6th Asia Pacific Medical Education Conference (APMEC), 19 - 22 February 2009, Singapore. Singapore: APMEC, 2009. [ Links ]
20. Cregan P, Watterson L. High stakes assessment using simulation: An Australian experience. Stud Health Technol Inform 2005;111:99-104. [ Links ]
21. Nel CPG, Labuschagne MJ, van Zyl GJ. Why is research needed on simulation to enhance plastic surgery education and training? Int J Cross-Disciplinary Subjects Educ 2018;9(1):3301-3308. [ Links ]
22. Nel CPG, Labuschagne MJ, van Zyl GJ. Simulation in plastic surgery: A research agenda to improve teaching, learning and clinical expertise/professional competence. Proceedings of the Ireland International Conference of Education (IICE), 25 - 28 April 2016. Dublin: IICE, 2016:56-62. [ Links ]
 Correspondence:
Correspondence:
C P G Nel
nelcpg@ufs.ac.za
Accepted 14 November 2019














