Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Health Professions Education
On-line version ISSN 2078-5127
Afr. J. Health Prof. Educ. (Online) vol.12 n.2 Pretoria Jun. 2020
http://dx.doi.org/10.7196/AJHPE.2020.v12i2.1172
RESEARCH
Burnout and associated factors in undergraduate medical students at a South African university
L J van der MerweI; A BothaII; G JoubertIII
IMB ChB, MMedSc, DA (SA), PhD (HPE); Undergraduate Medical Programme Management, School of Clinical Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIPhD (Counselling Psychology); Department of Psychology, Faculty of Humanities, University of the Free State, Bloemfontein, South Africa
IIIBA, MSc; Department of Biostatistics, School of Biomedical Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Medical students are at risk of burnout owing to various challenges
OBJECTIVES: To investigate burnout and associated factors among undergraduate students at a South African medical school
METHODS: In this cross-sectional study, findings of the Copenhagen Burnout Inventory (CBI), demographic data and information related to resilience were collected by means of an anonymous self-administered questionnaire. Associations between burnout subscales and various factors were determined
RESULTS: Five-hundred students (preclinical, n=270; clinical, n=230) completed the questionnaire. CBI mean scores for preclinical and clinical students were 17.9 and 17.4 (personal), 22.3 and 21.9 (work related) and 24.8 (patient related; clinical students only), respectively. High scores on the subscale reflect low levels of burnout in related areas. Male students and students with high self-reported resilience and low stress had significantly lower burnout levels. White preclinical students had lower levels of personal and work-related burnout, and black clinical students had less patient-related burnout
CONCLUSIONS: High mean scores in all three burnout subscales indicated low burnout levels among students. Academic and personal stress, as well as perceived poor support from institutional structures, were associated with significantly higher personal and work-related burnout, but not patient-related burnout in clinical students
Burnout is common among healthcare practitioners and medical students. Between 15% and 20% of physicians experience mental health problems in their working lifetime.[1,2] Approximately 63.4% of medical students were vulnerable to burnout, with half of these having chronic burnout.[3]
Medical students are at risk of burnout owing to various demands placed on them, including academic workload, emotional and physical challenges, and meeting the standards required of healthcare professionals from public and governance structures.[4-6] Burnout, defined as emotional exhaustion, depersonalisation and a sense of low personal accomplishment[7] may predict dropout and suicide ideation among medical students. Depression and suicidal ideation have been reported as 27.2% and 11.1%, respectively.[8] The prevalence of burnout ranges between 18% and 82%.[9,10] Understanding burnout and its related factors is essential to protect students during training,[3] and should be addressed timeously to prevent depression and dropout.[11]
Academic performance may be impeded by increasing levels of distress,[12] and students' ability to function effectively as future healthcare workers must be ensured.[13] Personal characteristics, the learning environment and perceptions regarding support play a role in protecting against or facilitating recovery from burnout.[3] As future healthcare professionals entering the workforce, medical students should be monitored for threats to their wellbeing, including burnout, and institutions should focus on strategies to relieve burnout and its effects to ensure effective performance.[14]
The aim of this study was to investigate burnout among undergraduate students at a South African (SA) medical school, and the influence of factors such as demographic profile, perceived stressors and support on their levels of burnout.
Methods
This study formed part of a larger research project on resilience in undergraduate medical students. For the purpose of this article, quantitative data regarding burnout and associated factors were collected by means of a standardised, validated questionnaire that also obtained demographic data and information related to resilience.
The target population included all students in the undergraduate medical programme at an SA university, who were invited to participate in a questionnaire survey. All undergraduate students who were registered in the 5-year MB ChB programme, from first to final year, were eligible to participate.
A pilot study on 5 students in the undergraduate nutrition and dietetics programme determined whether the time taken to complete the questionnaire was sufficient, and it identified any logistical issues related to completion of the questionnaire. The data from the pilot study were not included for analysis.
The questionnaires were distributed to all undergraduate medical students during classroom contact sessions. Students were informed that their participation was voluntary and anonymous.
The questionnaire included variables such as demographic data (age, gender, race, year of study), information regarding recent major stressful life events, levels of support, perceptions of the learning environment, perceptions regarding resilience and academic performance, and the Copenhagen Burnout Inventory (CBI).[15] The CBI measures three areas of burnout: personal, work related and patient related. It consists of 19 items rated on a 5-point Likert scale. In the CBI, 'Personal burnout is "the degree of physical and psychological fatigue and exhaustion experienced by the person", work-related burnout refers to "the degree of physical and psychological fatigue and exhaustion that is perceived by the person as related to his/her work", and patient- (client-) related burnout refers to "the degree of physical and psychological fatigue and exhaustion that is perceived by the person as related to his/her work with clients'.[15]
The possible range for the score on the 6 items on personal burnout is 6 - 30, with 6 indicating high and 30 low burnout. The 7 items on the work-related burnout subscale can yield scores between 7 and 35, with 7 indicating high and 35 low burnout. On the patient-related subscale, a range of 6 - 30 can be scored on the 6 items, with 6 indicating high and 30 low burnout.[15] Therefore, the higher the score obtained on a subscale, the less likely the student is to experience burnout in that particular area.
A total score of 95 indicates low burnout, while a score of 19 indicates high burnout. In this study, preclinical students did not complete the patient-related burnout subscale. Therefore, the scores in each of the three subscales were described separately, and a total score was not determined. The alpha coefficients for the various subscales were between 0.85 and 0.87 for a US adult sample.[15]
In addition to anonymous completion of the questionnaire, data were managed with strict confidentiality. Statistical analysis of quantitative data was performed using SAS software (SAS Institute, USA). Descriptive statistics and reliability coefficients were calculated, and the associations between burnout, demographic and other factors affecting resilience were determined.
Ethical approval
Approval to conduct the study was obtained from the Health Sciences Research Ethics Committee of the Faculty of Health Sciences, University of the Free State, Bloemfontein, SA (ref. no. HSREC 63/2017). Permission to include the students in the research was granted by the relevant university authorities.
Results
The sample population comprised 696 students. A total of 500 students completed the questionnaires and were divided into preclinical (n=270; response rate 79.2%; year 1 and 2; mean age 20 years) and clinical (n=230; response rate 62.0%; year 3, 4 and 5; mean age 22.6 years) groups. Preclinical students had not yet been exposed to patients in the clinical training environment, and could therefore not comment on patient-related burnout. The participants included 61.9% female students in the preclinical and 56.5% in the clinical groups. Only 20.5% of preclinical and 17.3% of clinical students reported that they were first-generation students (defined in this study as students whose parents had never been enrolled in post-school higher education).
Table 1 shows the CBI scores measured in personal and work-related burnout areas for both the preclinical and clinical groups, and patient-related burnout for the clinical group.
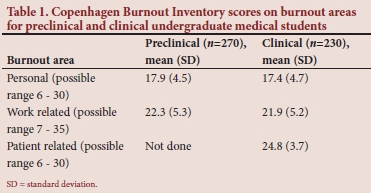
The mean scores for preclinical and clinical students were similar in both personal and work-related burnout areas. Both groups had high scores in the personal and work-related subscales, indicating low burnout. Clinical students demonstrated high scores in the patient-related subscale, with a mean score of 24.8. The reliability coefficients were calculated for preclinical students in the personal (0.84) and work-related (0.81) subscales, and for clinical students in the personal (0.88), work-related (0.85) and patient-related (0.82) subscales.
In Table 2, self-reported resilience and factors related to burnout are shown, and Table 3 (http://www.ajhpe.org.za/public/files/1172.doc) summarises the associations between burnout subscales and related factors.
In both the preclinical and clinical groups, first-generation students did not show significantly higher levels of burnout than those who were not first generation. The term 'first-generation student' originated in the USA. In SA, Heymann and Carolissen[16] indicated that first-generation status is one of many factors that may influence students' experiences in higher education. In both groups, significantly higher scores were obtained by male students on the subscales for personal burnout. In the clinical group, male students also had significantly higher scores on the work-related subscale. Female students in the clinical group had a slightly higher score on the patient-related subscale, but this was not statistically significant.
Students (N=500) self-reported ethnicity as black (n=151), coloured (n=41), white (n=262), Indian (n=36), Asian (n=5) and other (n=4). One student did not indicate ethnicity. For the purpose of this article, black and white students were included in the analysis to determine the possible associations with burnout, as meaningful conclusions could not be drawn with small numbers of students from other ethnic groups. Black students in the preclinical group had significantly lower scores (indicating higher burnout) on both personal and work-related subscales. In the clinical group, black students had significantly higher scores than white students on the patient-related subscale. The slightly lower subscale scores among black students, which related to personal and work-related burnout, did not differ significantly from the white students' scores.
In both groups, self-reported high resilience and no/minor levels of stress were associated with significantly less personal and work-related burnout, as well as lower patient-related burnout in clinical students.
The majority of students experienced academic stress, which was associated with significantly more burnout in personal and work-related subscales, but not among clinical students in the patient-related subscale. Students reported their academic performance to be above or the same as the class average, and low percentages of students had previously or were currently repeating an academic year.
Personal stress was also associated with significantly more burnout on the personal and work-related subscales for both student groups. In contrast, clinical students who reported personal stress had less patient-related burnout, although this was not statistically significant.
Financial stress was not associated with significantly higher burnout, and there were too few other stressors reported to allow for the assessment of an association between other stressors and burnout. The majority of students (preclinical, 97.7%; clinical, 93.8%) did report some stressors, but only clinical students had significantly more personal and work-related burnout than students who reported no stressors.
Relationship break-up in the preceding 12 months was reported by more preclinical than clinical students and was associated with slightly lower scores on burnout subscales. No clear association between parents' divorce or major illness/health events and burnout could be made owing to the low number of students who reported these stressors.
Major illness in a family member in the preceding 12 months was not associated with significantly more burnout, although clinical students did score slightly lower on the personal burnout subscale when reporting this stressor. Preclinical students who reported death of a close friend or family member scored significantly lower on the work-related but not on the personal burnout subscale. Preclinical students who reported no major life events in the preceding 12 months also had significantly higher work-related burnout subscale scores.
Most of the preclinical (66.5%) and clinical (76.1%) students indicated satisfaction with support received from family. The level of satisfaction was not associated with burnout subscale scores. Most students reported satisfaction with support received from friends and peers. Those who were either neutral or somewhat to very dissatisfied with such support, did have slightly lower burnout scores, although these were not statistically significant.
Although preclinical students were mostly neutral or satisfied with support received from School of Medicine academic staff, those who reported dissatisfaction scored significantly lower on personal and work-related subscales. Clinical students were more dissatisfied with support from the School of Medicine; this was associated with significantly lower scores on personal burnout subscales, and a tendency to lower work-related, but not patient-related subscale scores.
Preclinical students who were somewhat to very dissatisfied with support received from the Faculty of Health Sciences (administrative) staff scored significantly lower on personal and work-related subscales. Although similar patterns were seen among clinical students, these were not statistically significant, and there were no clear associations with patient-related burnout.
Although most students were neutral or dissatisfied with support from institutional student affairs staff, there were no significant associations with personal and work-related subscale scores. Overall, preclinical students were more satisfied than clinical students with the support they received from the university environment, while clinical students were more satisfied than preclinical students with the support they received from family and friends.
Associations between students' perceptions of the learning environment at the School of Medicine and the three burnout subscales were also determined. Many (40.9%) preclinical students agreed that the learning environment in the School of Medicine was collaborative rather than competitive, while 32.6% of clinical students agreed with this perception. A clear pattern was noted, i.e. that students who disagreed with the statement that the learning environment was collaborative rather than competitive, also scored lower on all the relevant subscales. In both groups, students' perceptions of a competitive rather than collaborative learning environment were therefore associated with higher burnout.
The majority of preclinical (82.6%) and clinical (67.0%) students agreed that student education was a high priority for the staff in the School of Medicine. In both groups, scores on the burnout subscales indicated low levels of burnout. Students who perceived that holistic support was available to them in the School of Medicine (preclinical, 57.3%; clinical, 42.3%) also scored significantly higher on the relevant subscales.
Of the preclinical and clinical students, 64.4% and 56.1%, respectively, were satisfied with the learning environment. There were significant differences in burnout subscales (personal and work-related) of preclinical and clinical students, with higher scores obtained by students who were satisfied with the learning environment. A similar pattern was observed for patient-related burnout scores among clinical students. Overall, clinical students were less satisfied with the learning environment in the School of Medicine compared with preclinical students.
Discussion
Eckleberry-Hunt et al.[17] cautioned against a pathology-based approach to burnout research, opposed to an approach that emphasises resilience within a positive psychological context. Therefore, a cut-off score has not been used in this study to determine whether students had burnout, but their scores on the three subscales (personal, work related and patient related) have been reported throughout.
Demographic factors, including gender and ethnicity, may place students at greater risk of burnout and affect their resilience.[3,18-20] However, cultural and contextual factors related to resilience in SA youth have not yet been researched extensively.[21] Davenport[11] cited the findings of a meta-analysis, which reported a higher prevalence of burnout in Middle Eastern countries, possibly related to the impact of ongoing conflict, and in North America, where more studies are done in this field than in Europe. This meta-analysis did not report on studies conducted specifically in Africa.[11]
In the current study, male students had significantly lower burnout in both personal and work-related subscales, similar to studies in other populations.[19,20] Female students in the clinical group had slightly higher scores in patient-related subscales, indicating lower burnout in this area. Gender as a protective factor preventing burnout should be taken into consideration when planning interventions.
Black students in the preclinical group scored significantly lower on personal and work-related burnout subscales. This was not the case for clinical students, where black students scored significantly higher on patient-related subscales. It could be argued that black students in the early years of study are more susceptible to burnout, but that the clinical environment may protect them against it. Although very few participants in this study were first-generation students, this was not associated with higher burnout, indicating that students without relatives who had previous experience of tertiary education, are not more vulnerable to burnout. However, black students from historically disadvantaged backgrounds may be predisposed to burnout in the early years of study, which may impact on their risk of depression or dropout.
Overall, >80% of preclinical and clinical students perceived themselves as having high resilience. This was associated with significantly higher scores on all the burnout subscales, demonstrating self-awareness in both student groups. This finding was contrary to that in a study in Pakistani medical students who demonstrated a lack of awareness, which predisposed them to higher burnout, leading to the promotion of self-awareness strategies when attempting to prevent burnout.[20]
The perceived high resilience and low burnout seen in this group of undergraduate medical students are worth noting in the context of the 5-year curriculum offered by the institution, which may be alleged to place greater time pressure on students. As individual and environmental factors influence resilience and burnout, this study provides valuable insight into the learning environment in medical school, which may contribute to protecting students from burnout and foster positive care.[17]
Medical studies are associated with various stressors.[22] In this study, most students reported some stressors that were associated with generally lower scores on the burnout subscales, indicating more burnout. Approximately one-third of both preclinical and clinical students who reported no or minor levels of stress, had higher subscale scores in all three burnout areas.
Academic stress is inextricably linked to medical training[3,20] and >80% of students in this study reported such stress. It was also associated with significantly lower scores on the personal and work-related burnout subscales in preclinical and clinical students. However, the majority of students reported that their academic performance was above or the same as the class average, revealing that academic stress and related burnout did not impact on academic performance of students in this programme, as has been described previously.[22] More than 90% of all students in this study perceived their academic performance to be the same as or above the class average. A small percentage of students had previously failed (preclinical, 19.6%; clinical, 17.8%) or were currently repeating (preclinical, 15.2%; clinical, 1.74%) the academic year. These findings warrant further research to accurately explore the association between perceived academic stress and recorded academic performance. More preclinical than clinical students reported that they were currently repeating the academic year, indicating that students' academic progress may improve with increasing seniority.
Approximately half of the students reported personal stress, which was associated with significantly lower scores on personal and work-related burnout subscales. In contrast, despite 56.3% of clinical students reporting personal stress, their burnout scores were higher on the patient-related subscale. This finding may indicate that students increasingly develop resilience and effective coping strategies as they mature into their professional identity - a positive prospect for the future physician workforce. Further investigation into the factors that promote resilience in spite of personal stress is warranted, as resilience is regarded as a predictor of wellbeing that may buffer against stress.[23]
Financial stress was reported by approximately one-third of students, although it was not associated with significantly lower burnout subscale scores. This finding was unexpected in light of the current discourse related to government funding of higher education in SA[24] and the literature pointing to debt as a significant stressor in higher education.[3] Further research in this regard is recommended.
Major life events may contribute to stress in student populations.[3] Therefore, this study determined the prevalence of relationship break-up, parents' divorce, major illness or health events, major illness in a family member and death of a close family member or friend as major life events in the preceding 12 months. While slightly lower scores on the burnout subscales were observed, students reporting any of these major life events did not have significantly more burnout. The exception was the death of a close family member or friend, which was associated with significantly lower scores in work-related burnout among the preclinical students. In this study, major life events probably did not predispose students towards burnout, as reported by Dyrbye et al.,[3] further emphasising the reported high resilience in this study population.
Social support and autonomy are associated with wellbeing and resilience.[25-27] In this study, the majority of preclinical and clinical students were satisfied with the support received from family, friends and peers, and no significant differences were observed in burnout subscales among students who were not satisfied with the support received from these sources. Preclinical students reported more satisfaction with School of Medicine academic staff and Faculty of Health Sciences support staff than clinical students, and increased levels of satisfaction were associated with significantly lower burnout. However, patient-related burnout among clinical students was not significantly higher in those who reported dissatisfaction with support received from Faculty of Health Sciences support staff. These findings suggest the need for increased emphasis on medical school support strategies that are visible and accessible to students across the preclinical and clinical years of study.
Most students reported that they were not satisfied with the support received from institutional student affairs staff, which was also associated with slightly higher burnout in both student groups. The fact that medical students in this programme are somewhat isolated from the general campus environment in terms of academic calendar and geographical training areas, may contribute to their less favourable perception of institutional support. It did not significantly contribute to burnout and was therefore negligible.
The competitive nature of medical school is a known cause of stress among students.[28] Generally, 30 - 40% of students in this study perceived the learning environment in the School of Medicine to be collaborative rather than competitive. Students who perceived the environment as competitive had significantly higher burnout. The majority of participants in this study agreed that students' education was a high priority for academic staff, and >40% of students felt that holistic support was available. These factors were associated with lower burnout in all three subscales.
More than half of all students indicated satisfaction with the learning environment, which was also associated with lower burnout in all the subscales. Preclinical students were generally more satisfied with the learning environment than clinical students. This finding could be attributed to preclinical training being mainly limited to the university environment, where lecture facilities, practical training spaces and resources such as staff and equipment are maintained by the institution. However, clinical training takes place in hospitals and clinics outside institutional authority where under-staffing, lack of resources and increased service delivery and patient loads may place greater demands on students rotating in these areas, as well as on academic staff responsible for student training and patient care. The effect of adverse working environments on staff wellbeing has been highlighted in the UK.[29] The findings from this study underline the need to promote wellbeing and resilience among medical students who are trained in a challenging environment, as resulting mental health problems may be associated with poor patient care.[13]
Study limitations
The study was conducted during the second semester (July - November) of an academic year over a period of 2 months. Differences in burnout scores could be seen during periods of increased academic pressure, e.g. assessment. It would therefore be valuable to repeat the burnout inventory at a different time of the year.
The results reported in this paper should not be viewed in isolation, because a single, once-off measure of burnout may not accurately reflect all the nuances impacting on student wellbeing. The additional information obtained regarding coping styles and resilience from the larger study, which falls beyond the scope of this paper, will contribute to a more balanced and comprehensive view of this student population.
Conclusions
In this cross-sectional study on preclinical and clinical undergraduate medical students in a 5-year MB ChB programme, high scores on personal and work-related subscales and patient-related subscales for clinical students, using the CBI, revealed a low level of burnout.
Male students and students who self-reported high levels of resilience and low levels of stress had significantly lower burnout, as indicated by higher scores on the personal and work-related subscales of the burnout inventory, while white preclinical students had lower personal and work-related burnout and black clinical students had lower patient-related burnout.
Preclinical students who perceived a high level of holistic institutional staff support, and who reported a collaborative rather than competitive learning environment that prioritises student education and academic development, had significantly lower personal and work-related burnout. Both preclinical and clinical students who were satisfied with the learning environment had significantly lower burnout in both personal and work-related subscales.
Major life events, perceived support from family, friends and peers, as well as being a first-generation student, did not significantly impact on burnout scores. Few students reported financial stressors and other major life events such as relationship break-up, parents' divorce or major illness (self/family). These events were not associated with higher burnout, with the only exception being the death of a close family member or friend in the preceding 12 months reported by preclinical students, which led to lower scores on the personal and work-related subscales, indicating higher burnout.
This study confirms that medical students are at risk of burnout owing to academic and other stressors, and that the learning environment in medical school should focus on promoting resilience and wellbeing.
Recommendations
The authors recommend that academic stressors should be addressed and support provided to cope with these and other stressors, including personal losses, and stressors such as the death of or disease in close family members and friends. Efforts should be increased to ensure student satisfaction with the learning environment, especially among clinical students who are exposed to the public healthcare training environment external to the tertiary institution. The impact of adverse training or working conditions should be investigated further, as the wellbeing of current and future healthcare professionals may be at risk. Appropriate support for vulnerable students, such as preclinical female and black students, should be investigated and implemented, and current strategies in the existing teaching and learning environment should be enhanced to optimise student wellbeing.
Declaration. None.
Acknowledgements. Dr Daleen Struwig, medical writer/editor, Faculty of Health Sciences, University of the Free State, for technical and editorial preparation of the manuscript.
Author contributions. All authors contributed equally to the manuscript.
Funding. Partial funding was obtained from the Research Directorate, University of the Free State.
Conflicts of interest. None.
References
1. Boisaubin EV, Levine RE. Identifying and assisting the impaired physician. Am J Med Sci 2001;322(1):31-36. https://doi.org/10.1097/00000441-200107000-00006 [ Links ]
2. Zwack J, Schweitzer J. If every fifth physician is affected by burnout, what about the other four? Resilience strategies of experienced physicians. Acad Med 2013;88(3):382-389. https://doi.org/10.1097/ACM.0b013e318281696b [ Links ]
3. Dyrbye LN, Power DV, Massie FS, et al. Factors associated with resilience to and recovery from burnout: A prospective, multi-institutional study of US medical students. Med Educ 2010;44(10):1016-1026. https://doi.org/10.1111/j.1365-2923.2010.03754.x [ Links ]
4. Dyrbye LN, Thomas MR, Shanefelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among US and Canadian students. Acad Med 2006;81(4):354-373. https://doi.org/10.1097/00001888-200604000-00009 [ Links ]
5. Howe A, Smajdor A, Stockl A. Towards an understanding of resilience and its relevance to medical training. Med Educ 2012;46(4):349-356. https://doi.org/10.1111/j.1365-2923.2011.04188.x [ Links ]
6. McCann CM, Beddoe E, McCormick K, et al. Resilience in the health professions: A review of recent literature. Int J Wellbeing 2013;3(1):60-81. https://doi.org/10.5502/ijw.v3i1.4 [ Links ]
7. Prayson RA, Bierer SB, Dannefer EF. Medical student resilience strategies: A content analysis of medical students' portfolios. Perspect Med Educ 2017;6(1):29-35. https://doi.org/10.1007/s40037-016-0313-1 [ Links ]
8. Rotenstein LS, Ramos MA, Torre M, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students. A systematic review and meta-analysis. JAMA 2016;316(21):2214-2236. https://doi.org/10.1001/jama.2016.17324 [ Links ]
9. Fares J, Al Tabosh H, Saadeddin Z, El Mouhayyar C, Aridi H. Stress, burnout and coping strategies in preclinical medical students. N Am J Med Sci 2016;8(2):75-81. https://doi.org/10.4103/1947-2714.177299 [ Links ]
10. Ishak W, Nikravesh R, Lederer S, Perry R, Ogunyemi D, Bernstein C. Burnout in medical students: A systematic review. Clin Teach 2013;10(4):242-245. https://doi.org/10.1111/tct.12014 [ Links ]
11. Davenport L. 'Alarming' rate of burnout in med students. Medscape. 2018. https://www.medscape.com/viewarticle/893466_print (accessed 23 August 2018). [ Links ]
12. Wilkinson TJ, McKenzie JM, Ali AN, Rudland J, Carter FA, Bell CJ. Identifying medical students at risk of underperformance from significant stressors. BMC Med Educ 2016;16:43. https://doi.org/10.1186/s12909-016-0565-9 [ Links ]
13. Wood DF. Mens sana in corpore sano: Student well-being and the development of resilience. Med Educ 2015;50(1):20-23. https://doi.org/10.1111/medu.12934 [ Links ]
14. Olsen KD. Physician burnout - a leading indicator of health system performance? Mayo Clin Proc 2017;92(11):1608-1611. https://doi.org/10.1016/j.mayocp.2017.09.008 [ Links ]
15. Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen burnout inventory: A new tool for the assessment of burnout. Work Stress 2005;19(3):192-207. https://doi.org/10.1080/02678370500297720 [ Links ]
16. Heymann L, Carolissen R. The concept of 'first-generation student' in the literature: Implications for South African higher education. S Afr J High Educ 2011;25(7):1378-1386. [ Links ]
17. Eckleberry-Hunt J, Kirkpatrick H, Barbera T. The problems with burnout research. Acad Med 2018;93(3):367-370. https://doi.org/10.1097/ACM.0000000000001890 [ Links ]
18. Dyrbye LN, Thomas MR, Eacker A, et al. Race, ethnicity, and medical student well-being in the United States. Arch Intern Med 2007;167(19):2103-2109. https://doi.org/10.1001/archinte.167.19.2103 [ Links ]
19. Backovic DV, Zivojinovic JI, Maksimovic J, MaksimoviC M. Gender differences in academic stress and burnout among medical students in final years of education. Psychiatr Danub 2012;24(2):175-181. [ Links ]
20. Muzafar Y, Khan HH, Ashraf H, et al Burnout and its associated factors in medical students of Lahore, Pakistan. Cureus 2015;7(11):e390. https://doi.org/10.7759/cureus.390 [ Links ]
21. Theron LC, Theron AMC. A critical review of studies of South African youth resilience, 1990 - 2008. S Afr J Sci 2010;106(7/8). https://doi.org/10.4102/sajs.v106i7/8.252 [ Links ]
22. Kötter T, Wagner J, Brüheim L, Voltmer E. Perceived medical school stress of undergraduate medical students predicts academic performance: An observational study. BMC Med Educ 2017;17(1):256. https://doi.org/10.1186/s12909-017-1091-0 [ Links ]
23. Shi M, Wang X, Bian Y, Wang L. The mediating role of resilience in the relationship between stress and life satisfaction among Chinese medical students: A cross-sectional study. BMC Med Educ 2015;15:16. https://doi.org/10.1186/s12909-015-0297-2 [ Links ]
24. Van Rensburg D, Fengu M. Zuma's fee-free higher education chaos. City Press, 27 January 2018. https://www.news24.com/SouthAfrica/News/zumas-fee-free-chaos-20180107-2 (accessed 23 August 2018). [ Links ]
25. Botha A, van den Berg H. Trauma exposure and life satisfaction among at-risk black South African adolescents. J Psychol Afr 2016;26(6):500-507. https://doi.org/10.1080/14330237.2016.1250422 [ Links ]
26. Prince-Embury S. Resiliency Scales for Children and Adolescents. A Profile of Personal Strengths. San Antonio: Harcourt Assessment Inc., 2006. [ Links ]
27. Rutter M. Resilience, competence and coping. Child Abuse Negl 2007;31(3):205-209. https://doi.org/10.1016/j.chiabu.2007.02.001 [ Links ]
28. Dyrbye LN, Thomas MR, Shanafelt TD. Medical student distress: Causes, consequences, and proposed solutions. Mayo Clin Proc 2005;80(12):1613-1622. https://doi.org/10.4065/80.12.1613 [ Links ]
29. Sull A, Harland N, Moore A. Resilience of health-care workers in the UK; a cross-sectional survey. J Occup Med Toxicol 2015;10(1):20. https://doi.org/10.1186/s12995-015-0061-x [ Links ]
 Correspondence:
Correspondence:
L J van der Merwe
merwelj@ufs.ac.za
Accepted 9 December 2019














