Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Health SA Gesondheid (Online)
On-line version ISSN 2071-9736
Print version ISSN 1025-9848
Health SA Gesondheid (Online) vol.28 Cape Town 2023
http://dx.doi.org/10.4102/hsag.v28i0.2318
ORIGINAL RESEARCH
Impact of the COVID-19 pandemic on audiology services in South Africa: A preliminary study
Katerina Ehlert
Department of Speech-Language Pathology and Audiology, School of Healthcare Sciences, Sefako Makgatho Health Sciences University, Pretoria, South Africa
ABSTRACT
BACKGROUND: Hygiene-, work practices, travel, personal interactions and access to healthcare services changed for the majority of the world during the pandemic
AIM: This study aimed to discover the knowledge, impact and attitudes towards COVID-19 on the professional practices of public and private sector audiologists in South Africa
SETTING: The study included 76 audiologists registered with the Health Professions Council of South Africa (HPCSA) and employed in the public, educational, tertiary or private practice and private sector in South Africa
METHODS: A cross-sectional self-administered electronic survey study design was implemented
RESULTS: Audiologists had appropriate knowledge regarding COVID-19. During hard lockdown, 69% of respondents saw less than 40% of their usual patient load, only 31% saw 60% - 100% of their usual patient load. During lower lockdown levels, majority of respondents (73.7%) saw 60% - 100% of their patient load while 26.3% still saw less than 40% of their usual patient load. Only hearing aid reprogramming, hearing aid trouble shooting, cochlear implant pre-counselling and adult hearing screening could be offered via tele-audiology. The main challenges faced were fear of infection, infection control measures in the workplace, accessibility and limited services provided during the various lockdown levels
CONCLUSION: The pandemic and lockdown levels had a definite impact on audiological service provision and many adaptations regarding service delivery and infection control in the workplace were required
CONTRIBUTION: The relevance of this work for health services is the identification of the challenges experienced by audiologists during the pandemic and the opportunities to prepare for the future
Keywords: COVID-19; pandemic; audiological services; audiology; impact; knowledge; attitudes.
Introduction
The COVID-19 pandemic has had a profound impact on various aspects of life, affecting almost all people worldwide indiscriminately, albeit to varying degrees. It is evident that there will be lasting changes in behaviour and practices as a result of this global crisis (Blumenthal et al. 2020). Hygiene practices, travel, work practices, personal interactions and access to services have all been affected for the majority of the world's population (Eikelboom et al. 2021; Manchaiah et al. 2022).
The healthcare industry has needed to reconsider the traditional face-to-face delivery of clinical services because of the pandemic's person-to-person transmission of a respiratory illness that originated in December 2019 in China and quickly spread globally (Blumenthal et al. 2020). The pandemic surprised everyone with its sudden onset and rapid spread. Many people and industries, including healthcare, were unprepared for the consequences. In response, national lockdowns were introduced, instructing people to stay at home and follow social distancing guidelines to limit the spread of virus (Gunjawate et al. 2021; Parmar, Beukes & Rajasingam 2022). In March 2020, the South African government announced the first of a series of national lockdowns intended to slow the spread of the disease and ease the growing pressure on the already overburdened South African healthcare system (South African Government 2020).
Some of the effects of the pandemic and lockdown levels included:
-
reduced access to healthcare with hospitals and clinics being overwhelmed with COVID-19 patients, routine medical care and elective procedures were delayed or cancelled, leading to reduced access to healthcare for many people (American Medical Association 2021),
-
telehealth: telehealth, or remote healthcare services, became more prevalent during the pandemic as people sought to limit in-person contact. This had been particularly important for audiology services, which often involve close proximity between patients and healthcare providers (American Academy of Audiology [AAA] 2021),
-
changes in patient behaviour: patients had been more hesitant to seek healthcare services during the pandemic, particularly in the early stages when there was a lot of uncertainty about the virus. This had led to delayed diagnosis and treatment for many health conditions, including hearing loss (Centers for Disease Control and Prevention [CDC] 2021),
-
changes in audiology practices: audiologists had to adapt to new protocols to ensure the safety of their patients and staff. This included increased use of personal protective equipment (PPE), enhanced cleaning and disinfection procedures and changes in scheduling and patient flow to limit the number of people in the clinic at any given time (American Speech-Language-Hearing Association [ASHA] 2021),
-
increased awareness of hearing loss: the pandemic has highlighted the importance of communication and the challenges faced by people with hearing loss, particularly with the use of masks and social distancing.
This had led to increased awareness of hearing loss and the need for audiology services (The Hearing Review 2021).
Throughout the first, second, third and fourth waves of the COVID-19 pandemic, lockdown measures were implemented, resulting in significant disruptions to healthcare services, including nonessential services. Audiology departments had to cancel many existing clinical appointments, and only urgent cases were attended to, with audiologist-patient contact minimised. Moreover, many audiology professionals and practices lacked the necessary skills or equipment to provide audiology services remotely via telehealth, despite telehealth being approved as an acceptable service delivery method by the Health Professions Council of South Africa (HPCSA) (Ballachanda et al. 2020; Gunjawate et al. 2021; Parmar et al. 2022; HPCSA 2022).
The COVID-19 pandemic has significantly impacted healthcare and audiology services. However, providers have adapted to the new challenges and continued to provide crucial care to their patients. No studies have been conducted regarding the effects of the pandemic on audiologists in South Africa. This study aims to investigate the knowledge, impact and attitudes of public and private sector audiologists towards COVID-19 and its impact on their professional practices in South Africa. The findings of this study will inform professional bodies and employers about the impact of COVID-19 on audiology, enabling them to provide the necessary support and plan for the future of audiology services, including telehealth. Understanding how audiology services were affected during the pandemic and how audiologists responded to the changing needs of patients is essential in adapting and responding to these changes. Such perspectives can guide the necessary short- and medium-term changes for audiology in South Africa.
Methods
Study design
This study involved a cross-sectional self-administered electronic survey design to determine the impact of COVID-19 on professional practices of audiologists in South Africa. The main aim of the study was to determine the impact (including knowledge, practices and attitudes) of COVID-19 on professional practices of private and public audiologists in South Africa.
Data collection sites, population and sampling
The population for the study was all hearing care professionals (audiologists, acousticians and audiometrists) registered with the HPCSA and employed in the public, educational, tertiary or private sector in South Africa, as well as hearing care professionals who work in private practice. Simple random sampling was applied, with a target population size of 344 for this study. The total number of hearing care professionals registered with HPCSA was 3266. A 95% confidence interval with a 5% margin of error was used to calculate the target population size.
Data collection tool
The questionnaire used in the study was adapted from surveys performed in India and the United Kingdom (Gunjawate et al. 2021; Saunders & Roughly 2020) and validated for the South African context through a pilot study. Questions were removed, added and rephrased in order to improve the questionnaire. Google forms were used to develop and distribute the questionnaire electronically. The questionnaire included demographic information, practices during the pandemic, attitudes of audiologists and knowledge of COVID-19. Open and closed-ended questions were included, and the knowledge of COVID-19 was determined using multiple choice and true or false format questions.
Data collection procedure
Following ethical clearance, data collection was done through online distribution of the questionnaire link via social media, email lists and other online platforms including professional bodies such as HPCSA, South African Speech-Language and Hearing association (SASLHA) and South African Association of Audiologists (SAAA). Informed consent and clear instructions for completing the questionnaire were included in the electronic questionnaire links. As respondents completed the questionnaire, the data were automatically collected and stored in Google Forms. The researcher downloaded the data for analysis.
Data analysis
The first step involved data cleaning. This included removing any incomplete or irrelevant responses from the dataset. For example, if a respondent did not answer a particular question, or if they provided an answer that was clearly unrelated to the question, those responses were excluded from the analysis. Quantitative analysis of closed-ended questions was scrutinised using statistical methods such as descriptive statistics (e.g. mean, frequencies, percentages) and inferential statistics (Wilcoxon signed-rank test) was used to determine whether there was a statistical difference (p < 0.05) between services during hard- and lower lockdown levels and to identify patterns, trends and relationships among the variables. The variables considered in this study were knowledge on COVID-19 analysed using a memorandum, practices during the pandemic analysed using inferential statistics and attitudes of audiologists using descriptive statistics. Analysis of open-ended questions included thematic analysis, which involved coding and categorising the responses into themes or patterns to identify key issues, concerns or perspectives that emerge from the data.
Ethical considerations
Ethical clearance to conduct this study was obtained from the Sefako Makgatho Health Sciences University Research Ethics Committee (No. SMUREC/H/266/2021:UG), prior to the onset of data collection. Electronic informed consent was obtained from all respondents before completing the questionnaire.
Results
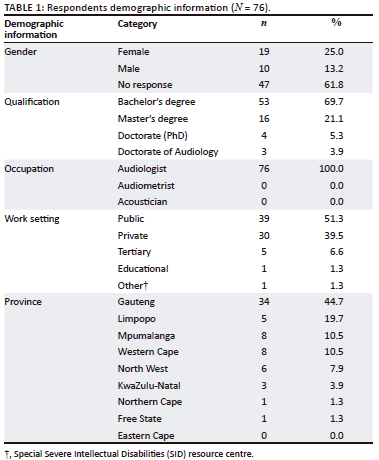
A total of 76 audiologists in South Africa participated in the study. A response rate of 23% was obtained, which is just below the recommended 25% or more for surveys (Genroe 2019). Table 1 describes the respondent demographics.
Knowledge of COVID-19
General questions about COVID-19 and management of COVID-19 patients were included. Respondents were required to respond with true or false. The majority of the respondents (93.7%, n = 71) were able to correctly identify the core symptoms of COVID-19, the way it can spread from person to person (97.4%, n = 74) and the social distancing that should be maintained from a person with COVID-19 (93.4%, n = 71).
Audiology practices implemented during the COVID-19 pandemic
During the COVID-19 pandemic, various levels of restrictions were employed. Hard lockdown included level 5 restrictions that indicated a high COVID-19 spread with a low health system readiness. Level 1, 2, 3 and adjusted level 4 restrictions indicated a low or moderate COVID-19 spread with a low-to-moderate health system readiness (COVID-19 regulations by South African Government 2020). Hard lockdown was when operations had to be ceased and every person was expected to be at home as movements were restricted, which only allowed essential services to be provided. Lower lockdown levels were when restrictions were eased which permitted more services to be provided. The various lockdown levels had fluctuating effects on the practices of audiologists. Majority of the respondents (77%, n = 58) reported that hard lockdown had a major impact on the practices of audiologists while 20% (n = 15) reported some impact, 1% (n = 1) reported minimal impact and 2% (n = 2) reported no impact. During lower lockdown levels, 17% (n = 13) reported major impact, 42% (n = 32) reported some impact, 3% (n = 2) reported minimal impact and 10% (n = 8) reported no impact on audiological practices.
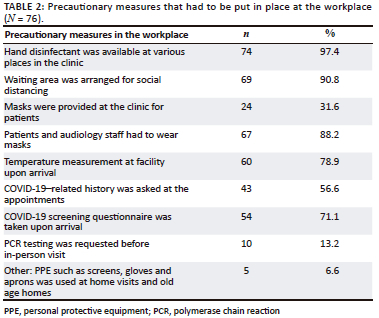
All respondents reported that their services had to adapt to the rules and regulations from the Department of Health during all lockdown levels. Patients had to be provided with prescreening case history forms (57%, n = 43), PPE had to be worn (88%, n = 67), social distancing was maintained in the workplace (91%, n = 69) as well as hands and surroundings had to be constantly sanitised or disinfected (97%, n = 74). Table 2 summarises the precautionary measures that had to be put in place at the workplace.
Appointments of patients were often postponed, and less patients were seen per day in order to accommodate these adaptations. During lower lockdown levels, the patient loads could increase, but still not to pre-pandemic levels. During hard lockdown, 69% (n = 52) of respondents saw less than 40% of their usual patient load; only 31% (n = 24) saw 60% - 100% of their usual patient load. During lower lockdown levels, majority of respondents (73.7%, n = 56) saw 60%-100% of their patient load while 26.3% (n = 20) still saw less than 40% of their usual patient load. Table 3 summarises the main aspects that were impacted by the pandemic and the way audiologists practiced audiology during the various lockdown levels.
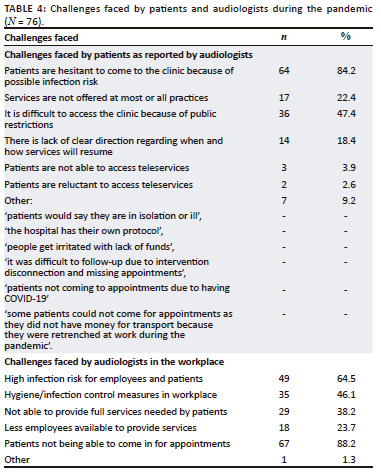
The main challenges faced by patients were hesitancy to come to the clinic because of infection risk (84%, n = 64) and difficulties accessing the clinic because of public restrictions (47%, n = 36). On the other hand, the main challenges faced by audiologists were patients unable to attend appointments (88%, n = 67), high infection risk for patients and employees (65%, n = 49) and infection control measures in the workplace (46%, n = 35). All the challenges faced by patients and audiologists during the pandemic are listed in Table 4.
The Wilcoxon signed-rank test was used to determine whether there is a statistical difference (p < 0.05) between services during hard- and lower lockdown levels and between adults and children. Results indicated that there was no statistical significance between audiological services offered during hard and lower lockdown levels. Urgent audiological cases were addressed during all lockdown levels, and in general most cases were not postponed for more than 4 weeks. Table 5 describes how audiological services were affected by hard and lower lockdown levels for adults and children.
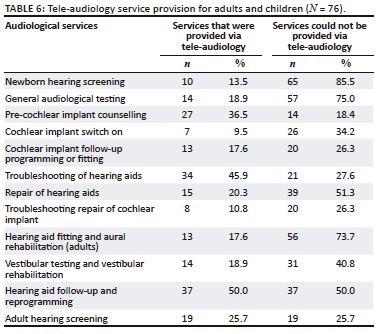
The main services that could not be provided via tele-audiology included newborn hearing screening (86%, n = 65), general audiological testing (75%, n = 57), hearing aid fitting and aural rehabilitation in adults (74%, n = 56), repair of hearing aids (51%, n = 39) and hearing aid follow-up and reprogramming (50%, n = 37). Table 6 describes the audiological services that could and could not be provided via tele-audiology for both adults and children.
Attitudes towards the COVID-19 pandemic
A Likert scale was used to measure the attitudes of audiologists towards the COVID-19 pandemic. Five statements were included, and respondents were asked to indicate whether they strongly agree, agree, neutral or disagree. The majority of respondents (> 50%) continued to provide services during the pandemic and did not cancel appointments because of COVID-19 symptoms in patients. The respondents' responses are described in Table 7.
Discussion
The study conducted sheds light on the impact of the COVID-19 pandemic on audiology services in South Africa. Of the total participants, 40% worked in private practice, and 50% worked in public health. The study included participants from all the provinces in South Africa except for the Eastern Cape. The findings of the study suggest that audiologists had sufficient knowledge about COVID-19, and appropriate infection control measures were implemented. This is in contrast to a study conducted in India, which reported that audiologists had poor practices towards infection control measures, especially hand washing, highlighting the need for better awareness among audiologists about appropriate and standard infection control measures (Gunjawate et al. 2021). It can be inferred that the consistent media attention, training provided at the workplace and COVID-19 regulations by the South African Government (2020), Department of Health websites (NDOH 2022) and the CDC (2022) ensured that healthcare workers had access to the required information regarding the virus's knowledge, transmission and precautionary measures.
The study also reported that the hard lockdown significantly impacted audiological services, as 77% of respondents experienced a decrease in their patient load. Even during lower lockdown levels, the majority of respondents (74%) saw 60% - 100% of their patient load, while 26% still saw less than 40% of their usual patient load. Consequently, many patients had to delay or cancel appointments, resulting in reduced access to services. Patients were hesitant to come to the clinic because of the risk of infection. Tele-audiology became mandatory, and audiologists had to adapt quickly to provide these services. A study conducted in South Africa by Swanepoel et al. (2020) supports the finding that lockdown levels significantly affected audiological services. The study found that during hard lockdown, 69% of respondents saw less than 40% of their usual patient load and only 31% saw 60% - 100% of their usual patient load. Moreover, appointments were often postponed, and fewer patients were seen per day (72%) to comply with the restrictions. Another study conducted in the United Kingdom by Atkinson, Shipway and Woodcock (2021) reported that audiology services were reduced by an average of 62% across the country during the first wave of the pandemic, with some services being closed completely. During the second wave of the pandemic, which occurred during lower lockdown levels, services were still reduced by an average of 38%.
The services that could not be provided via tele-audiology in the current study included newborn hearing screening, general audiological assessment, hearing aid fitting and aural rehabilitation for adults, repair of hearing aids, vestibular assessment and rehabilitation and cochlear implant switch on. The services that could be provided via tele-audiology included troubleshooting of hearing aid, hearing aid follow-up and reprogramming, pre-cochlear implant counselling and adult hearing screening. Similar studies conducted in the United Kingdom and internationally reported tele-audiology barriers for verification, paediatrics, earmould adjustments, diagnostics, complex patients and assessing mental health. The tele-audiology service delivery difficulties included suitable technology and technical support, data protection, competence and confidence of audiologists, rapport and patient interaction and change in working patterns. Accessibility challenges for patients were sight difficulties, severe hearing loss and no access to technology (Eikelboom et al. 2021; Manchaiah et al. 2022; Parmer et al. 2022). Similarly, the current study highlighted the challenges and limitations in tele-audiology service delivery, emphasising the need for audiologists to consider improvement and development in the capacity for telehealth service provision.
In the present study, urgent cases were treated similarly during hard and lower lockdowns for both adults and children. The most common services provided were audiological assessments, hearing aid fittings and troubleshooting, followed by electrophysiological measures and vestibular assessments and rehabilitation. These findings are supported by AAA (2020), which reported that emergency audiological services were still available during the pandemic. For example, if a patient experienced sudden hearing loss or had an issue with their hearing aid that required immediate attention, they could still seek emergency services from their audiologist. Furthermore, amplification in children is considered an emergency, as the impact of hearing loss can cause lifelong delays (Yoshinaga-Itano 2020).
The main challenges faced by audiologists in this study were patients not being able to attend appointments, a high infection risk for employees and patients, hygiene and infection control measures in the workplace, an inability to provide the full range of services required and fewer employees being available to provide services. Patients reported hesitance to come to the clinic because of the possible risk of infection, difficulty accessing the clinic and not all services being offered. These outcomes are supported by AAA (2020) and ASHA (2020), which identified limited availability of PPE, reduced access to audiology equipment, reduced patient volumes, limited tele-audiology services and compliance with infection control measures as challenges faced by audiologists.
Audiologists' attitudes towards the COVID-19 pandemic indicated that the majority (72%) would continue providing services even if there was a positive case in the workplace, and they would provide treatment to patients exhibiting symptoms of COVID-19. Several studies support the finding that audiologists are committed to providing services during the pandemic, despite the risks. A scoping review found that 71% of respondents reported that they continued to provide in-person services during the pandemic. The review also found that audiologists were implementing a range of measures to minimise the risk of COVID-19 transmission, including wearing PPE, conducting screenings of patients prior to appointments and increasing cleaning and disinfecting protocols in their clinics (Aggarwal et al. 2021). Another study surveyed audiologists in the United Kingdom and found that 75% of respondents continued to provide in-person services during the pandemic, with 64% of those reporting that they had modified their practices in response to the pandemic (Saunders & Roughley 2021). This highlights the commitment of audiologists to continuing service delivery during the pandemic, despite the risks.
The findings of this study should be interpreted with caution, as the sample size was relatively small. However, the study represents audiologists from eight of the nine provinces in South Africa. Despite these limitations, the study provides important insights into the impact of COVID-19 on audiology services in South Africa. The study highlights the importance of infection control measures, tele-audiology and adapting to new technologies to ensure that patients receive the care they need, even during a pandemic. Overall, the findings of this study are consistent with other studies that report the impact of COVID-19 on audiology services worldwide.
Conclusion
The pandemic and associated lockdowns had a significant impact on the delivery of audiological services, requiring adaptations in service provision and infection control measures in the workplace. Tele-audiology was implemented to a limited extent because of equipment, access and connectivity challenges. This work is relevant for health services as it identifies the challenges experienced by audiologists during the pandemic and opportunities to prepare for the future. The COVID-19 pandemic had a profound sociological, psychological and professional impact. Although the pandemic has passed with lifestyle changes and effective treatments and vaccines, this study highlights the need for the audiology profession to adopt new clinical technologies and business models for improved reimbursement, service delivery and patient-centred care. COVID-19 has accelerated the future of healthcare, and audiologists have a unique opportunity to prepare for tele-audiology and improved service delivery to make it accessible for all.
Acknowledgements
The author would like to thank Dr. R. Hornby for assistance with formulation of the questionnaire and the pilot study, as well as R.E. Mzunga, M.L. Maledimo, R.N. Mcetywa and N.S. Simelane (final year undergraduate students at Sefako Makgatho Health Sciences University in 2021) for the assistance with data collection.
Competing interests
The author declares that no financial or personal relationships inappropriately influenced the writing of this article.
Author's contributions
K.E. drafted the article and was responsible for conceptualisation, methodology and formal analysis.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The data that support the findings of this study are available from the corresponding author, K.E, upon reasonable request.
Disclaimer
The views expressed in the submitted article are his or her own and not an official position of the institution or funder.
References
AAA (American Academy of Audiology), 2020, Audiology in the era of COVID-19: Practice impact survey results, viewed 29 April 2023, from https://www.audiology.org/sites/default/files/publications/resources/Academy_COVID-19_Impact_Survey_Report.pdf. [ Links ]
AAA (American Academy of Audiology), 2021, Teleaudiology: Best practices for remote audiology services, viewed 28 April 2023, from https://www.audiology.org/sites/default/files/publications/resources/teleaudiology_best_practices.pdf. [ Links ]
Aggarwal, K., Gunjawate, D.R., Yerraguntla, K. & Ravi, R., 2022, 'Impact of COVID-19 pandemic on audiology practice: A scoping review', Clinical Epidemiology and Global Health 13, 100939. https://doi.org/10.1016/j.cegh.2021.100939 [ Links ]
American Medical Association, 2021, COVID-19's impact on patient access to care in 2020 and outlook for 2021, viewed 28 April 2023, from https://www.ama-assn.org/system/files/2021-03/covid-19-impact-access-care-report-2021.pdf. [ Links ]
ASHA (American Speech-Language-Hearing Association), 2021, Considerations for the reopening of audiology services during the COVID-19 pandemic, viewed 28 April 2023, from https://www.asha.org/Practice/reopening-audiology-services-during-the-covid-19-pandemic/. [ Links ]
Atkinson, J., Shipway, L. & Woodcock, K., 2021, 'The impact of the COVID-19 pandemic on audiology services in the United Kingdom', International Journal of Audiology 60(7), 485-491. [ Links ]
Ballachanda, B., Abrams, H., Hall III, J.W., Manchaiah, V., Minihane, D., Robler, S.K. & Swanepoel, D., 2020, 'Tele-audiology in a pandemic and beyond: Flexibility and suitability in audiology practice', Audiology Today 32(4), 12-21. [ Links ]
Blumenthal, D., Fowler, E.J., Abrams, M. & Collins, S.R., 2020, 'COVID-19 - Implications for the health care system', New England Journal of Medicine 383(15), 1483-1488. https://doi.org/10.1016/j.cegh.2021.100939 [ Links ]
CDC (Centers for Disease Control and Prevention), 2021, Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020, viewed 28 April 2023, from https://www.cdc.gov/mmwr/volumes/69/wr/mm6936a4.htm. [ Links ]
CDC (Centers for Disease Control and Prevention), 2022, Coronavirus disease (COVID-19) -transmission, viewed 30 June 2022, from https://www.cdc.gov/coronavirus/2019-ncov/easy-to-read/prevent-getting-sick/how-covid-spreads.html. [ Links ]
Eikelboom, R.H., Bennett, R.J., Manchaiah, V., Parmar, B., Beukes, E., Rajasingam, S.L. & Swanepoel, D.W., 2022, 'International survey of audiologists during the COVID-19 pandemic: Use of and attitudes to telehealth', International Journal of Audiology 61(4), 283-292. https://doi.org/10.1016/j.cegh.2021.100939 [ Links ]
Genroe, 2019, The Complete Guide to Acceptable Survey Response Rates, viewed 28 September 2022, from https://www.genroe.com/blog/acceptable-survey-response-rate-2/11504. [ Links ]
Gunjawate, D.R., Ravi, R., Yerraguntla, K., Rajashekhar, B. & Verma, A., 2021, 'Impact of coronavirus disease 2019 on professional practices of audiologists and speech-language pathologists in India: A knowledge, attitude and practices survey', Clinical Epidemiology and Global Health 9, 110-115. https://doi.org/10.1016/j.cegh.2020.07.009 [ Links ]
HPCSA (Health Professions Council of South Africa) corporate affairs, 2022, HPCSA Telehealth Guidelines, viewed 30 June 2022, from https://www.hpcsa-blogs.co.za/hpcsa-telehealth-guidelines/. [ Links ]
Manchaiah, V., Eikelboom, R.H., Bennett, R.J. & Swanepoel, D.W., 2022, 'International survey of audiologists during the COVID-19 pandemic: Effects on the workplace', International Journal of Audiology 61(4), 265-272. https://doi.org/10.1080/14992027.2021.1937348 [ Links ]
National Department of Health (NDOH), 2022, COVID-19 policies and guidelines, viewed 30 June 2022, from https://www.health.gov.za/covid19/downloads.html?type=policies. [ Links ]
Parmar, B., Beukes, E. & Rajasingam, S., 2022, 'The impact of COVID-19 on provision of UK audiology services & on attitudes towards delivery of telehealth services', International Journal of Audiology 61(3), 228-238. https://doi.org/10.1080/14992027.2021.1921292 [ Links ]
Saunders, G.H. & Roughley, A., 2021, 'Audiology in the time of COVID-19: Practices and opinions of audiologists in the UK', International Journal of Audiology 60(4), 255-262. https://doi.org/10.1080/14992027.2020.1814432 [ Links ]
South African Government, 2020, Regulations and guidelines - Coronavirus COVID-19, viewed 30 June 2022, from https://www.gov.za/covid-19/resources/regulations-and-guidelines-coronavirus-covid-19. [ Links ]
Swanepoel, D.W., Clark, J.L., Koekemoer, D. & Hall, J.W., 2020, 'Preliminary findings on the association between COVID-19 and self-reported hearing and tinnitus problems in South Africa', International Journal of Audiology 59(8), 487-489. [ Links ]
The Hearing Review, 2021, Study: COVID-19 pandemic heightens awareness of hearing loss, viewed 28 April 2022, from https://www.hearingreview.com/inside-hearing/research/study-covid-19-pandemic-heightens-awareness-of-hearing-loss. [ Links ]
Yoshinaga-Itano, C., 2020, 'Challenges to EHDI systems amid the COVID-19 crisis', The Hearing Journal 73(5), 43-45. https://doi.org/10.1097/01.HJ.0000666452.15264.95 [ Links ]
 Correspondence:
Correspondence:
Katerina Ehlert
katerina.ehlert@smu.ac.za
Received: 14 Jan. 2023
Accepted: 31 May 2023
Published: 29 Aug. 2023














