Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Health SA Gesondheid (Online)
versión On-line ISSN 2071-9736
versión impresa ISSN 1025-9848
Health SA Gesondheid (Online) vol.28 Cape Town 2023
http://dx.doi.org/10.4102/hsag.v28i0.2234
ORIGINAL RESEARCH
Job satisfaction among health professionals in a District of North West province, South Africa
Reabetswe A. MereI; Thembi V. SimbeniI; Mmampedi MathibeI; Mabina N. MogaleI; Sam T. NtuliII
IDepartment of Public Health, School of Healthcare Sciences, Sefako Makgatho Health Sciences University, Pretoria, South Africa
IIDepartment of Statistical Sciences, Faculty of Science and Technology, Sefako Makgatho Health Sciences University, Pretoria, South Africa
ABSTRACT
BACKGROUND: Job satisfaction has become an area of relevance and debate in public health as it is directly linked to staff absenteeism, retention and turnover of the workforce and as such, influences the organisational commitment of the workers and the quality of health services provided. It is therefore essential to discern what drives healthcare professionals to remain working in the public health sector.
AIM: This study aimed to determine job satisfaction and its associated factors among healthcare professionals.
SETTING: North-West province South Africa.
METHODS: A cross-sectional study was conducted among 244 healthcare professionals of different categories in three district hospitals. A self-administered structured questionnaire with 38 questions to measure job satisfaction was used to collect data. The chi-square test was used to compare groups, and a p-value < 0.05 was considered statistically significant.
RESULTS: Overall, 62% of the participants were not satisfied with their job. The most common factors that participants were not satisfied with include job security (52%), standard of care (57%), opportunity to develop (59%), payment or wages (76%), workload (78%) and working environment (89%). Job satisfaction was significantly influenced by age, job category and years of service
CONCLUSIONS: The predictors of job satisfaction include age, category of employees and years of service. Interventions are required to improve the degree of job satisfaction among health care professionals.
CONTRIBUTION: Findings of this study will assist informing plans that are geared towards enhancing healthcare worker job satisfaction, retention and consequent health systems strengthening.
Keywords: job satisfaction; healthcare professionals; cross-sectional studies; North West Province; working conditions; clinical staff; workforce; motivation.
Introduction
Healthcare professionals (HPs) have a significant influence on the provision of quality healthcare as well as healthcare access and are thus an important component of the healthcare system. For a health system to function effectively there must be health professionals who are sufficiently skilled, motivated and supported. HPs are the primary drivers of an efficient, effective and sustainable healthcare system (Khunou & Davhana-Maselesele 2016). It is thus vital to comprehend what motivates them to remain working in the public health sector. According to Blaauw et al. (2013), job satisfaction significantly plays a critical role in determining the motivation of the workforce and affects the organisational commitment of healthcare professionals and, as such, the quality of health services provided.
Job satisfaction of healthcare professionals has increasingly become an essential aspect of measure within the South African health system. A comparative study on job satisfaction and intention to leave of different categories of health workers in three Southern African countries indicated that job dissatisfaction was substantially higher in 47.9% of South Africa (SA) than in 29.0% of Malawi and 17.4% of Tanzania (Blaauw et al. 2013). The authors in this study also found that health professionals in SA were more than twice inclined to report an intention to resign as compared to those from the other two countries. In other studies conducted in sub-Saharan Africa, the proportion of healthcare professionals not satisfied with their job ranged from 25.7% to 68.3% (Akuffo et al. 2021; Geta et al. 2021; Merga & Fufa 2019; Mulugeta & Ayele 2015; Temesgen, Aycheh & Leshargie 2018). A similar study conducted among Australian healthcare professionals found that 17.0% of them where not satisfied with their jobs (Scanlan, Devine & Watkins 2021). In India, however, 2.8% of healthcare professionals were not satisfied with their job (Singh et al. 2019).
The World Health Organization's (WHO) Global strategy on human resources in the health workforce outlined a policy agenda to reach the sustainable development goals (SDGs) targets by 2030 and recommended the optimisation of performance, quality and impact of the health workforce (WHO 2016). Several studies indicated that job satisfaction benefits the health system as it is associated with building up employee motivation, performance, efficiency and retention (Blaauw et al. 2013; Merga & Fufa 2019). Furthermore, it assists organisations in achieving their objectives and goals. According to Mbindyo et al. (2009), the motivation of healthcare workers could lay the foundation for pushing and maintaining efforts towards reaching SDGs. Evaluation of job satisfaction in the healthcare sector is not a new phenomenon worldwide. In SA, studies have been conducted to evaluate job satisfaction and its associated factors among healthcare professionals; however, most of these studies concentrated mainly on professional nurses (Khamisa et al. 2015; Khunou & Davhana-Maselesele 2016; Morton et al. 2020; Payne et al. 2020). There is a paucity of information on the level of job satisfaction in all categories of healthcare professionals. Thus, this study's objectives were to determine job satisfaction and to determine factors associated with job satisfaction among all categories of healthcare professionals in Ngaka Modiri District in North-West province.
Research methods and design
Study design and setting
This cross-sectional study was conducted between December and January 2021 at Ngaka Modiri Molema District of the North West province SA. The study was conducted in three randomly selected public hospitals from four hospitals in the region. The total number of healthcare professionals from the three institutions was 393, with 196 at Zeerust/Lehurutshe Complex Hospital, 126 at Thusong/General De La Rey Complex Hospital and 71 at Gelukspan District Hospital.
Study population
The study population comprised all categories of healthcare professionals (i.e. medical practitioners, professional nurses, dieticians, physiotherapists, pharmacists, occupational therapists, radiographers and clinical associates) who were on duty during the data-collection period.
Inclusion and exclusion criteria
Healthcare professionals who served for less than 12 months in the hospital at the time of data collection, work part-time and were unwilling to give informed consent were excluded from the study. All the above-mentioned categories of health professionals, who have been on full-time employment for 12 months and more and willing to participate were included in the study.
Sampling and sample size
The required sample size for this study was determined using Yamane's (1967) formula:

Where:
n is the sample size
N is the population size of the three hospitals (393)
e is the sampling error (5%).
A non-response rate of 10% was expected, and the sample size was increased to 218. The facilities have different numbers of healthcare professionals. Thus, the sample was allocated proportionally to the hospitals. To distribute the tools to all categories of healthcare professionals, participants were grouped according to their professional category, and then from each group, a consecutive sampling technique was used to administer the questionnaire.
Recruitment
The researchers were responsible for recruiting study participants and coordinating the consenting process. The researchers recruited healthcare professionals during their tea times at their respective working stations by giving verbal information about the study and its purpose. Recruitment was done during the day and at night, in order to include all healthcare professionals who meet the criteria and are willing to participate in the study.
Data collection
A structured self-administered questionnaire was used for data collection, which is developed using relevant literature (Khamisa et al. 2015; Khunou & Davhana-Maselesele 2016; Morton et al. 2020; Payne et al. 2020). The tool includes demographic profiles such as gender, age, marital status, professional category, level of education and years of experience as a healthcare professional.
The second part of the questionnaire had 38 questions used to measure job satisfaction and answered as either dissatisfied 0, unsure 0 or satisfied 1 (dissatisfied was merged with unsure). The section that measures job satisfaction has nine dimensions: personal satisfaction (six items), workload (four items), staff relations (four items), opportunity to develop (five items), payment or wages (three items), job security (three items), standards of care (four items), leadership and supervision (five items) and working environment (four items). Data collection occurred for a period of four weeks from the first week of December to 29 December in year 2020.
Data analysis
Data were entered and analysed using the Microsoft Excel© Spreadsheet and statistical package STATA version 16, respectively. The total score for each item in the dimension of satisfaction was dichotomised into satisfied and dissatisfied using the mean score as a cut-off point, so a score equal to or above the mean value was considered satisfied otherwise dissatisfied. Comparison between the two groups was performed using the chi-square test. A p-value of less than 0.05 was considered statistically significant.
Reliability and validity
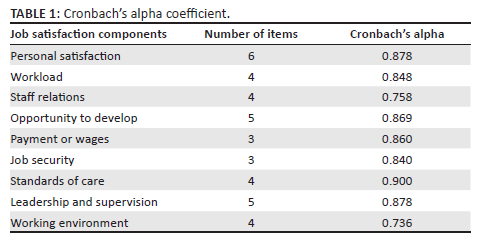
The reliability coefficient values ranged from 0.736 - 0.964, which are considered to range from acceptable to excellent (Table 1).
Ethical considerations
The Research Ethics Committee of Sefako Makgatho Health Sciences University gave ethical approval (SMUREC/H/172/2020) as this study was part of a Master of Public Health (MPH) research project. Permission to carry out this study was sought from the North West Department of Health and the managers of the three district hospitals where the study was being conducted. All the participants completed the informed consent and were assured that the data collected would be kept confidential and used only for this study. Participants were also informed that participation was voluntary and they were free to withdraw from the study at any time. Consent to publish study findings was also obtained from the participants.
Results
Demographic characteristics
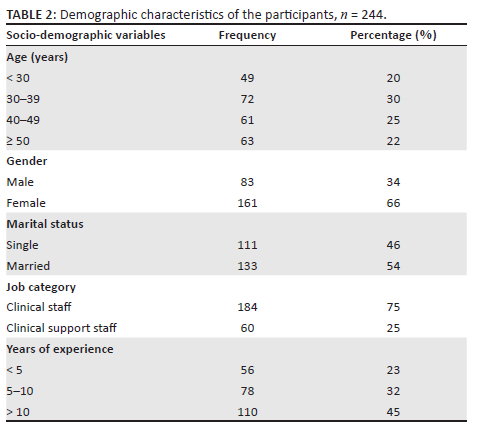
A total of 244 healthcare professionals participated in this study. Their mean age was 40.3 ± 11.1 years ranging from 23 - 64 years. More than two-thirds (75%) of the participants were aged less than 50 years and 66% were females. Slightly more than half (54%) were married and 75% were clinical staff (Table 2). The mean number of years working as a health care professional was 11.6 ± 8.4 years ranging from 1 - 36 years. Nearly half (45%) of the participants had more than 10 years of working experience as healthcare professionals.
Level of job satisfaction among health professionals
Overall, 62% of the participants were found to be dissatisfied with their job. The most common aspects that the participants were not satisfied with include: 52% job security, 57% standard of care, 59% opportunity to develop, 76% payment or wages, 78% workload and 89% working environment (Figure 1).
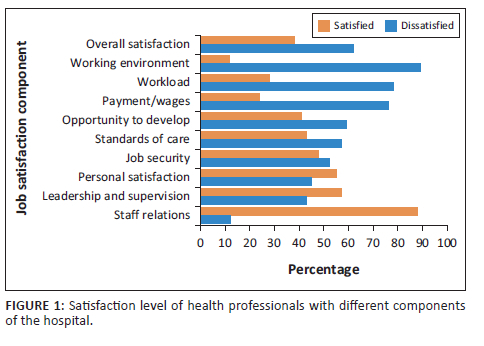
To determine items affecting job satisfaction under each dimension, the results showed that for the work environment dimension with four items, 91% availability of equipment, 87% state of hospital infrastructure and 84% maintenance of the hospital were the main contributors to job dissatisfaction. Meanwhile, for the workload dimension, all four items were identified to contribute to job dissatisfaction, 79% overall staffing levels, 76% my workload, 64% time available to get through my work and 62% of the hours I work.
In terms of payments or wages dimension with three items, 77% degree to which I am fairly paid and 75% of my salary or pay scale were found to be the main causes of job dissatisfaction. Five items for the opportunity to develop dimension are ordered from the highest to the lowest causes of job dissatisfaction: being funded for courses, opportunities I've to advance my career or prospects for promotion, opportunity to attend courses, time off for in-service training and extent to which I've adequate training for what I do.
Factors associated with overall job satisfaction among healthcare professionals
As shown in Table 3, there is no statistically significant association between gender (p > 0.05) and marital status (p > 0.05) with the overall level of satisfaction. A significantly greater proportion of healthcare professionals under 30 years were likely to be dissatisfied with their job as compared to the other age groups (p < 0.05). The result also showed that clinical staff and those with less than 5 years of working experience as healthcare professionals were significantly likely to be dissatisfied with their job (p < 0.05).
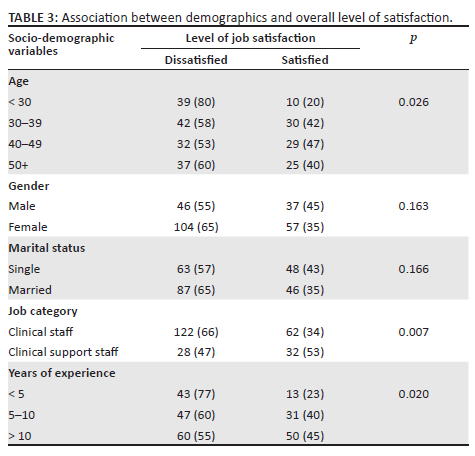
Table 4 shows the association between demographics and job satisfaction dimensions. The result revealed that the personal satisfaction dimension is statistically associated with age (p = 0.04) and years of working experience as a healthcare professional (p = 0.029). Participants aged less than 30 years and those with less than 5 years of working experience as healthcare professionals were more likely to be dissatisfied than the other groups.
The clinical staff (p < 0.001) and those aged 40 years and older (p = 0.015) were significantly dissatisfied with the dimension of the workload. The results also showed that participants aged < 30 years (p = 0.032) and those with less than 5 years of working experience as healthcare professionals (p = 0.004) were more likely to be dissatisfied with the staff relation dimension. The dimension of opportunity to develop was found to be statistically related to age (p = 0.001), job category (p = 0.007) and years of experience (p < 0.001). The younger age group, clinical support staff and those with less working experience were dissatisfied with the dimension of opportunity to develop.
Concerning the payments or wages dimension, female gender (p = 0.047), married (p = 0.009) and clinical staff (p < 0.001) were significantly dissatisfied with the dimension of payments or wages. The result revealed no statistically significant relationship between age (p = 0.08), gender (p = 0.458), marital status (0.646), job category (p = 0.251), years of experience (p = 0.128) and standard of care dimension. The leadership and supervision dimension were also found not significantly associated with age (p = 0.096), gender (p = 0.370), marital status (0.952), job category (p = 0.148) and years of experience (p = 0.098). Similarly, the finding also indicates no statistically significant association between age (p = 0.416), gender (p = 0.058), marital status (0.766), job category (p = 0.178), years of experience (p = 0.258) and the dimension of a working environment.
Discussion
The purpose of this study was to determine the level of job satisfaction and its associated factors among healthcare professionals in the Ngaka Modiri Molema District, North West province The finding revealed that nearly two-thirds (62%) of the participants were found not to be satisfied with their job. This finding is similar to studies conducted in Ethiopia that reported that 61.5% (Merga & Fufa 2019) and 65.1% (Mulugeta & Ayele 2015) of healthcare professionals were not satisfied with their job. The rate of job dissatisfaction observed in our study is higher than 44.8% (Geta et al. 2021), 25.7% (Akuffo et al. 2021), 17.0% (Scanlan et al. 2021), 14.8% (Qiu et al. 2021) and 2.8% (Singh et al. 2019) reported in previous similar studies. However, the finding of this study is slightly lower than the 68.3% found in a cross-sectional study conducted among healthcare professionals working in public hospitals in Ethiopia (Temesgen et al. 2018). The high job dissatisfaction rate observed in the present study is a cause for concern as dissatisfied healthcare professionals provide substandard and less effective healthcare.
In the present study, the main source of job dissatisfaction identified was the work environment, which accounted for more than two-thirds (89%) of the dissatisfied healthcare professionals. Our finding is similar to the findings of previous studies that reported that poor job satisfaction is because of the work environment (Akuffo et al. 2021; Bonenberger et al. 2014; Kumar et al. 2013; Mulugeta & Ayele 2015). Employees usually attain a feeling of satisfaction with their jobs when they are working in a clean environment with all adequate commodities and supplies as well as acceptable levels of environment and temperature (Munyewende, Rispel & Chirwa 2014).
Dissatisfaction with the workload is another important issue affecting 78% of healthcare professionals in our study. A similar finding was reported among nurses working in tertiary care hospitals in India (Gulavani & Shinde 2014) and medical practitioners and nurses in China (Jin et al. 2019). A high workload is associated with inappropriate treatment (Guan et al. 2021; Yang et al. 2019) and can be minimised by addressing the shortage of staff, proper planning of duty schedules and training staff to plan their priorities.
Consistent with a number of studies, most (76%) of the healthcare professionals were not satisfied with their wage studies (Akuffo et al. 2021; Anand et al. 2022; Asegid et al. 2014; Ayalew et al. 2019; Khunou & Davhana-Maselesele 2016; Kumar et al. 2013;). Khunou and Davhana-Maselesele (2016) stated that since the implementation of Occupational Specific Dispensation (OSD), no studies were conducted regarding the impact of this policy on the level of job satisfaction among healthcare professionals. Other essential factors that influence job satisfaction in the present study were job security, the standard of care and lack of opportunity to develop. Mengistu and Bali (2015) in their study found that lack of training opportunities, poor performance evaluation systems and poor working conditions were the main cause of job health professionals not being satisfied with their job.
Various socio-demographic characteristics such as age, sex, level of education and years of experience as healthcare professionals were found to be associated with job satisfaction (Asegid et al. 2014; Ayalew et al. 2019; Lu et al. 2016). However, other studies reported no association between socio-demographic factors and job satisfaction (Chaulagain & Khadkas 2012; Elsherbeny & El-Masry 2018). In this study, job satisfaction significantly increases with age and years of experience and is higher among clinical support staff. Concerning the relationship between demographics and job satisfaction dimensions, the study revealed that participants aged < 30 years were significantly not satisfied with personal satisfaction, workload, opportunity to develop and job security. In addition, female gender and married participants were significantly not satisfied with payment or wages, while the married respondents were also not happy with job security. Clinical staff were significantly unhappy with the workload, while clinical support staff were not satisfied with the opportunity to develop.
Study limitations
This study was conducted in three hospitals in the province which makes it difficult to generalise the findings of this study to the entire province. Another limitation is that the studies reviewed used different questionnaires to assess job satisfaction; moreover, the definitions of job satisfaction are different.
Conclusion
In conclusion, the findings of this study indicated that the healthcare professionals in these settings had a low level of job satisfaction. Working environment, workload, payment or wages, development opportunities, standards of care and job security were the most common dimensions that cause participants to remain not satisfied. In addition, demographic factors such as age, job category and years of service influence job satisfaction. The policymakers, healthcare managers and other stakeholders must establish and implement effective policies that will increase the job security of healthcare professionals and decrease their intention to leave their positions by enhancing their working conditions and job satisfaction, paying them fairly, fostering job prospects and stability and supporting competency-based career advancement. Additionally, the workload should be reduced by effective duty schedule planning, a decrease in healthcare professional turnover, greater recruitment of trained and experienced personnel and training of employees in the technique of prioritisation of activities.
Acknowledgements
The authors acknowledge the support of the Department of Health in North West, hospital managers and study participants in enabling the success of this study. The authors also acknowledge Dr Hendry van der Heever for his valuable contribution as a research supervisor in the research proposal development phase of this study.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
Conceptualisation, R.A.M.; investigation R.A.M.; methodology R.A.M.; data validation, R.A.M., T.V.S., M.M., N.M.M.; formal analysis R.A.M., T.V.S., M.M., N.M.M., T.S.N.; Writing original draft preparation, R.A.M.; writing review T.V.S., M.M., N.M.M., T.S.N.; supervision; T.V.S., M.M.; project administration, R.A.M.; funding acquisition R.A.M. All authors discussed the findings and contributed to the final manuscript.
Funding information
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
Akuffo, K.O., Agyei-Manu, E., Kumah, D.B., Danso-Appiah, A., Mohammed, A.S., Asare, A.K. et al., 2021, 'Job satisfaction and its associated factors among optometrists in Ghana: A cross-sectional study', Health and Quality Life Outcomes 19(1), 12. https://doi.org/10.1186/s12955-020-01650-3 [ Links ]
Anand, T., Kaur, G., Gupta, K., Thapliyal, S. & Lal, P., 2022, 'Job satisfaction among medical officers working in Delhi', Journal of Family Medicine and Primary Care 11(1), 155-161. https://doi.org/10.4103/jfmpc.jfmpc_268_21 [ Links ]
Asegid, A., Belachew, T. & Yimam, E., 2014, 'Factors influencing job satisfaction and anticipated turnover among nurses in Sidama Zone Public Health Facilities, South Ethiopia', Nursing Research and Practice 2014, 909768. https://doi.org/10.1155/2014/909768 [ Links ]
Ayalew, F., Kibwana, S., Shawula, S., Misganaw, E., Abosse, Z., Van Roosmalen, J. et al., 2019, 'Understanding job satisfaction and motivation among nurses in public health facilities of Ethiopia: A cross-sectional study', BMC Nursing 18, 46. https://doi.org/10.1186/s12912-019-0373-8 [ Links ]
Blaauw, D., Ditlopo, P., Maseko, F., Chirwa, M., Mwisongo, A., Bidwell, P. et al., 2013, 'Comparing the job satisfaction and intention to leave of different categories of health workers in Tanzania, Malawi, and South Africa', Global Health Action 6(1), 19287. https://doi.org/10.3402/gha.v6i0.19287 [ Links ]
Bonenberger, M., Aikins, M., Akweongo, P. & Wyss, K., 2014, 'The effects of health worker motivation and job satisfaction on turnover intention in Ghana: A cross-sectional study', Human Resources for Health 12(1), 43. https://doi.org/10.1186/1478-4491-12-43 [ Links ]
Chaulagain, N. & Khadka, D.K., 2012, 'Factors influencing job satisfaction among healthcare professionals at Tilganga eye centre, Kathmandu, Nepal', Age 35(56), 74-67. [ Links ]
Elsherbeny, E.E. & El-Masry, R., 2018, 'Job satisfaction among nurses working in Mansoura university hospital: Effect of socio-demographic and work characteristics', Egyptian Journal of Occupational Medicine 42(2), 227-240. https://doi.org/10.21608/ejom.2018.6807 [ Links ]
Geta, A., Biks, G.A., Dellie, E. & Yazachew, L., 2021, 'Job satisfaction and associated factors among health professionals working at public and private hospitals in Bahir Dar City, Northwest Ethiopia: A comparative cross-sectional study', BioMed Research International 2021, 6632585. https://doi.org/10.1155/2021/6632585 [ Links ]
Guan, X., Ni, B., Zhang, J., Zhu, D., Cai, Z., Meng, W. et al., 2021, 'Association between physicians' workload and prescribing quality in one tertiary hospital in China', Journal of Patient Safety 17(8), e1860-e1865. https://doi.org/10.1097/PTS.0000000000000753 [ Links ]
Gulavani, A. & Shinde, M., 2014, 'Occupational stress and job satisfaction among nurses', International Journal of Science and Research 3(4), 733-740. [ Links ]
Jin, Y., Wang, H., Wang, D. & Yuan, B., 2019, 'Job satisfaction of the primary healthcare providers with expanded roles in the context of health service integration in rural China: A cross-sectional mixed methods study', Human Resources for Health 17(1), 70. https://doi.org/10.1186/s12960-019-0403-3 [ Links ]
Khamisa, N., Oldenburg, B., Peltzer, K. & Ilic, D., 2015, 'Work related stress, burnout, job satisfaction and general health of nurses', International Journal of Environmental Research and Public Health 12(1), 652-666. https://doi.org/10.3390/ijerph120100652 [ Links ]
Khunou, S.H. & Davhana-Maselesele, M., 2016, 'Level of job satisfaction amongst nurses in the North-West Province, South Africa: Post occupational specific dispensation', Curationis 39(1), 1-10. https://doi.org/10.4102/curationis.v39i1.1438 [ Links ]
Kumar, R., Ahmed, J., Shaikh, B.T., Hafeez, R. & Hafeez, A., 2013, 'Job satisfaction among public health professionals working in public sector: A cross sectional study from Pakistan', Human Resources for Health 11(1), 2. https://doi.org/10.1186/1478-4491-11-2 [ Links ]
Lu, Y., Hu, X.M., Huang, X.L., Zhuang, X.D., Guo, P., Feng, L.F. et al., 2016, 'Job satisfaction and associated factors among healthcare staff: A cross-sectional study in Guangdong Province, China', BMJ Open 6(7), e011388. https://doi.org/10.1136/bmjopen-2016-011388 [ Links ]
Mbindyo, P., Gilson, L., Blaauw, D. & English, M., 2009, 'Contextual influences on health worker motivation in district hospitals in Kenya', Implementation Science 4(1), 43. https://doi.org/10.1186/1748-5908-4-43 [ Links ]
Mengistu, M.M. & Bali, A.G., 2015, 'Factors associated to job satisfaction among healthcare Workers at Public Hospitals of west Shoa zone, Oromia regional state, Ethiopia', Science Journal of Public Health 3(2), 161-167. https://doi.org/10.11648/j.sjph.20150302.12 [ Links ]
Merga, H. & Fufa, T., 2019, 'Impacts of working environment and benefits packages on the health professionals' job satisfaction in selected public health facilities in eastern Ethiopia: Using principal component analysis', BMC Health Services Research 19(1), 494. https://doi.org/10.1186/s12913-019-4317-5 [ Links ]
Morton, D., Topper, K., Bowers, C., Jardien-Baboo, S., Nyangeni, T. & Mabitja, M., 2020, 'Job satisfaction of nurses working in public hospitals: Perceptions of nurse unit managers in South Africa', British Journal of Nursing 29(17), 1024-1029. https://doi.org/10.12968/bjon.2020.29.17.1024 [ Links ]
Mulugeta, M.M. & Ayele, G.B., 2015, 'Factors associated to job satisfaction among healthcare workers at public hospitals of West Shoa Zone, Oromia Regional State, Ethiopia: A cross sectional study', Science Journal of Public Health 3(2), 161-167. https://doi.org/10.11648/j.sjph.20150302.12 [ Links ]
Munyewende, P.O., Rispel, L.C. & Chirwa, T., 2014, 'Positive practice environments influence job satisfaction of primary health care clinic nursing managers in two South African provinces', Human Resources for Health 12(1), 1-14. https://doi.org/10.1186/1478-4491-12-27 [ Links ]
Payne, A., Koen, L., Niehaus, D.J.H. & Smit, I.M., 2020, 'Burnout and job satisfaction of nursing staff in a South African acute mental health setting', South African Journal of Psychiatry 26, 1454. https://doi.org/10.4102/sajpsychiatry.v26i0.1454 [ Links ]
Qiu, D., Li, R., Li, Y., He, J., Ouyang, F., Luo, D. et al., 2021, 'Job dissatisfaction mediated the associations between work stress and mental health problems', Frontiers in Psychiatry 12, 711263. https://doi.org/10.3389/fpsyt.2021.711263 [ Links ]
Scanlan, L.M., Devine, S.G. & Watkins, D.L., 2021, 'Job satisfaction of mental healthcare workers in multidisciplinary teams', Journal of Mental Health 30(1), 80-87. https://doi.org/10.1080/09638237.2019.1644489 [ Links ]
Singh, T., Kaur, M., Verma, M. & Kumar, R., 2019, 'Job satisfaction among health care providers: A cross-sectional study in public health facilities of Punjab, India', Journal of Family Medicine and Primary Care 8(10), 3268-3275. https://doi.org/10.4103/jfmpc.jfmpc_600_19 [ Links ]
Temesgen, K., Aycheh, M.W. & Leshargie, C.T., 2018, 'Job satisfaction and associated factors among health professionals working at Western Amhara Region, Ethiopia', Health and Quality Life Outcomes 16(1), 65. https://doi.org/10.1186/s12955-018-0898-7 [ Links ]
World Health Organization, 2016, Global strategy on human resources for health: Workforce 2030, viewed 15 September 2022, from https://www.who.int/publications/i/item/9789241511131. [ Links ]
Yamane, T., 1967, Statistics an introductory analysis, 2nd edn., Harper and Row, New York, NY. [ Links ]
Yang, J.H., Liao, Y.F., Lin, W.B. & Wu, W., 2019, Prescribing errors in electronic prescriptions for outpatients intercepted by pharmacists and the impact of prescribing workload on error rate in a Chinese tertiary-care women and children's hospital', BMC Health Services Research 19(1), 1013. https://doi.org/10.1186/s12913-019-4843-1 [ Links ]
 Correspondence:
Correspondence:
Thembi Simbeni
thembi.khoza@smu.ac.za
Received: 02 Nov. 2022
Accepted: 13 Mar. 2023
Published: 22 May 2023














