Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Health SA Gesondheid (Online)
versión On-line ISSN 2071-9736
versión impresa ISSN 1025-9848
Health SA Gesondheid (Online) vol.27 Cape Town 2022
http://dx.doi.org/10.4102/hsag.v27i0.1694
REVIEW ARTICLE
In-hospital interventions to promote relational practice with families in acute care settings: A scoping review
Waheedha EmmamallyI; Christen ErlingssonII; Petra BrysiewiczII
IDiscipline of Nursing, School of Nursing and Public Health, University of KwaZulu-Natal, Durban, South Africa
IIDepartment of Health and Caring Sciences, Faculty of Health and Life Sciences, Linnaeus University, Kalmar, Sweden
ABSTRACT
Relational practice is characterised by genuine interaction between families and healthcare professionals that promotes trust and empowerment. Positive clinical outcomes have been associated with relational practice. To assess and examine in-hospital interventions designed to promote relational practice with families in acute care settings of emergency departments, intensive care units and high care units. The preferred reporting Items for Systematic Reviews and Meta-Analyses guidelines informed the design of this scoping review. To identify relevant studies, databases (Academic Search Complete; CINAHL; PubMed; PsyInfo) and the search engine Google Scholar were searched using terms for core elements of relational practice and family engagement. Of the 117 articles retrieved, eight interventional studies met the search criteria. The interventions focused on relational practice elements of collaborating with and creating safe environments for families, whilst only one addressed healthcare professionals being respectful of families' needs and differences. In relation to the nature of engagement of families in interventions, the focus was mainly on improving family functioning. Family engagement in the interventions was focused on involving families in decision-making. The scoping review revealed a limited number of in-hospital interventions designed to promote relational practice with families in acute care settings. Further research is encouraged to develop such interventions.
CONTRIBUTION: The scoping review has highlighted specific elements of relational practice that have been overlooked in the mapped interventions. This provides guidance on where future interventional research may be focused
Keywords: acute care setting; collaborations; family engagement; family-healthcare professional interactions; relational practice.
Introduction
Families play an important role in caring for their loved ones in acute healthcare settings, whilst simultaneously assisting healthcare professionals (HCPs) with vital information for the treatment of the patient (Bhalla et al. 2014). Moreover, research has demonstrated that HCP and family collaboration in acute care settings leads to positive patient outcomes of recovery and satisfaction with care (Indovina et al. 2016; Williams, Nolan & Keady 2009). Inclusive of positive relationships between HCPs and families is the relational practice approach, which is defined as an approach that invests in creating meaningful relationships between individuals (Zou 2016). Relational practice with families in healthcare settings centres on HCPs and family members who enter into a relationship, fully prepared to share their true personalities and grow together (Jordan 2010). An important aspect of collaborating with families is to know how families define themselves, as this definition directs the role and expectations of families during the illness experience of their loved ones. For this reason, the current study adopted Doane and Varcoe's (2007) definition of a family, as a relational process where family members are interlinked with their experiences, emotions and social circumstances.
Core elements of relational practice include individuals consciously connecting and growing towards each other, authenticity in caring, whereby individuals are transparent and genuine in their emotions, being attuned to each other's needs whilst honouring differences, mutual trust and respect between individuals leading to self-empowerment (Fletcher 1998; Jordan 2010). Self-reflection in relational practice encourages HCPs to confront prejudices that may be present in family encounters (Duffey & Somody 2011; Hartrick 2008). Relational practice is about HCPs creating safe environments for families through therapeutic communication (Doane & Varcoe 2007). The authors elaborate that in creating safe environments, HCPs promote feelings of security that facilitates families to share their emotions. Healthcare professionals are encouraged to acknowledge the contextual factors that may shape a patient's and family's responses to experiences and interactions with people (Zou 2016). These include personal characteristics, and socio-political, cultural and geological factors that affect how patients and families manage their illness. Jordan (2010) speaks about the element of HCPs being fully involved in relationships with families thus supporting families to grow.
Equally important to a relational practice approach is the active engagement of families in their care (Shields 2015). Family engagement requires that HCPs actively partner with families, acknowledging that families hold the expertise to improve their healthcare experiences (Burns et al. 2018). Family engagement speaks to HCPs working with families at every level of the healthcare system to transform care whilst preserving their dignity (Shield 2015). Three dimensions are proposed when reviewing family engagement in an intervention, namely, the focus of the intervention, the structure of the family engagement and the level of family engagement (Knafl et al. 2017). Knafl et al. (2017) explains that when a family is actively engaged in an intervention, the intervention becomes relevant and acceptable to them. Workload pressures, a rapid-paced environment and high patient acuities in the acute care settings often challenge relational interactions and active engagement with families (Hetland et al. 2018). Amidst these challenges, HCPs working in acute care settings need guidance to meaningfully connect with families (Östlund & Persson 2014). It is therefore important to identify whether existing interventions which are designed to promote family and HCP collaboration address the core elements of relational practice and the nature of family engagement. To this end, the review aims to assess and examine in-hospital interventions designed to promote relational practice with families in acute care settings of emergency departments (EDs), intensive care units (ICUs) and high care units (HCUs).
Methods
Research design
A scoping review following the preferred reporting items for Systematic Reviews and Meta-Analyses (Page et al. 2021) and the five-stage framework proposed by Arksey and O'Malley (2005) was conducted. A scoping review methodology was chosen over other reviews as it allowed for a broad overview of key concepts on the relatively understudied area of relational practice (Colquhoun et al. 2014).
Stage 1: Identifying the research questions
The authors formulated the research questions guided by the population, concept and context (PCC) and closely aligned to the aim of the review. The research questions were as follows: 1) What in-hospital interventions are available to promote relational practice with families in acute care settings of EDs, ICUs and HCUs? 2) What elements of relational practice did the interventions address? 3) What was the nature of family engagement in the interventions?
Stage 2: Identifying relevant studies
A search strategy detailing search terms (see Table 1) and identified databases were developed in consultation with a specialist librarian. Search terms related to relational practice and family engagement were applied to the following databases: Academic Search Complete, CINAHL, MEDLINE and PubMed, PsyINFO and the search engine Google Scholar. After selecting relevant titles from the initial results, the authors identified additional keywords to refine the search. The inclusion criteria of the review included: A population of HCPs working in acute care settings and family members visiting acute care settings; the concept was in-hospital interventions occurring in the acute care settings (namely EDs, ICUs and HCUs) and the context of the studies were the nature of family engagement and elements of relational practice. Studies had to include outcome measures related to a specific core element of relational practice with family members. The core elements are included in Table 3.
Stage 3: Study selection
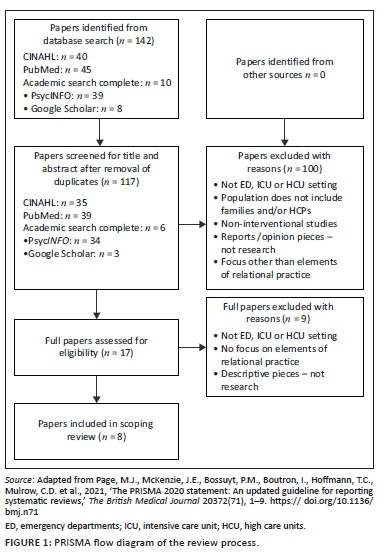
Three authors were involved in the review process. Articles in English which were published between January 2005 and December 2018 were included in the review and this was informed by the interest in relational practice and quality outcomes of complex healthcare contexts in the literature (Williams et al. 2009). The database search yielded 142 papers with 25 duplicate papers being removed by the first author (WE). The remaining 117 papers underwent a two-phase review process involving two authors (WE and PB) working independently. Two authors screened the titles and abstracts against the inclusion criteria and a further 100 papers were excluded. The remaining 17 papers underwent a full-text assessment by the same independent authors. This resulted in eight papers for the final review. After each stage, the two authors met to discuss the results of their independent review and resolve any emerging issues, with discrepancies being resolved by the third author (CE). Figure 1 shows the review process.
Stage 4: Charting the data
A data extraction table was developed by the reviewers for relevant data extraction and management of the eight papers included in the final review.
Stage 5: Collating, summarising and reporting the results
The three research questions of the scoping review guided this stage of collating, summarising and synthesising the studies. The details of the included studies are shown in Table 2.
Review findings
Overview of interventions in included studies
All eight studies originated in developed countries. Three studies originated in the United States and the remaining five originated in the United Kingdom, Iceland, the Netherlands, Hong Kong and Australia (Table 2). Most of the studies were conducted in an ICU setting (Chien et al. 2006; Eggenberger & Sanders 2016; Jacobowski et al. 2010; Mitchell et al. 2009; Van Mol et al. 2016; White et al. 2018), one in the ED (Blackwell et al. 2017), and one study was conducted across hospital departments, including the ICU setting (Svavarsdottir et al. 2015). The studies were primarily quantitative in approach.
With regard to the participants who were targeted by the intervention, five studies focused on nurses and family members (Chien et al. 2006; Eggenberger & Sanders 2016; Mitchell et al. 2009; Svavarsdottir et al. 2015; White et al. 2018). The interventions of the remaining three studies targeted multidisciplinary team participation, namely those of Jacobowski et al. (2010) (medical doctors, families, nurses); Van Mol et al. (2016) (families, nurses, spiritual care workers, a social worker, a psychologist, medical doctors - intensivists) and Blackwell et al. (2017) (patients, family members, a medical doctor-palliative care, nurses and ED management staff).
Seven studies used multicomponent family interventions. These were educational and/or psychological support programmes for families (Blackwell et al. 2017; Chien et al. 2006; Jacobowski et al. 2010; Van Mol et al. 2016), educational and training programmes for nurses (Eggenberger & Sanders 2016; Svavarsdottir et al. 2015), and a support programme for families with an educational component for nurses (White et al. 2018). The study by Mitchell et al. (2009) described a single component intervention of involving family members in the basic care of their loved one admitted in ICU. All studies described the component/components of the interventions in detail.
Seven studies conducted pre- and post-test measurements using validated quantitative tools (Chien et al. 2006; Eggenberger & Sanders 2016; Jacobowski et al. 2010; Mitchell et al. 2009; Svavarsdottir et al. 2015; Van Mol et al. 2016; White et al. 2018). Majority (n = 5) of the studies reported that the interventions had positive outcomes of improved family support and improved family decision-making (Chien et al. 2006; Jacobowski et al. 2010; Mitchell et al. 2009; Van Mol et al. 2016; White et al. 2018). Outcomes of increased clinician skills and confidence were noted in the interventions of Svavarsdottir et al. (2015); Eggenberger and Sanders (2016); Blackwell et al. (2017) and White et al. (2018). Regarding reports of sustainability of the interventions, three studies discussed plans to ensure sustainability of the interventions (Blackwell et al. 2017; Svavarsdottir et al. 2015; Van Mol et al. 2016). The contents of the interventions are detailed in Table 2.
Elements of relational practice addressed by the interventions
The authors utilised the core elements of relational practice described by Duffey and Somody (2011); Fletcher (1998); Hartrick (2008), Jordan (2010); Doane and Varcoe (2007) and Zou (2016) to answer the question of 'What elements of relational practice did the interventions address?' (Refer to Table 3). All eight studies focused on relational elements of, consciously preparing to collaborate and involve families through authentic connection and creating safe environments through actions of therapeutic communication & providing information. Comparatively, only two studies (Eggenberger & Sanders 2016; Svavarsdottir et al. 2015) addressed relational elements of empathetic understanding of families through self-reflection by the HCPs. The relational element of appreciating the factors that influenced experiences and relationships was evidenced in the intervention by Blackwell et al. (2017) and Chien et al. (2006). Finally, Chien et al. (2006) looked at the relational practice element of HCPs being attuned to families' needs whilst honouring their cultural and social differences.
Nature of family engagement in the interventions
The nature of family engagement in the interventions of the reviewed studies was analysed using the three dimensions of family engagement in an intervention, namely, the focus of the intervention, the structure of the family engagement and the level of family engagement (Knafl et al. 2017). Regarding the focus of the intervention, four of the studies focused on improving family relationships to optimise family functioning (Eggenberger & Sanders 2016; Jacobowski et al. 2010; Svavarsdottir et al. 2015; Van Mol et al. 2016). The structure of family engagement involved key family figures in the intervention (Blackwell et al. 2017; Chien et al. 2006; Jacobowski et al. 2010; Mitchell et al. 2009; Van Mol et al. 2016; White et al. 2018). Family engagement in the interventions of the studies was the active involvement of families in decision-making (Eggenberger & Sanders 2016; Jacobowski et al. 2010; Mitchell et al. 2009; Svavarsdottir et al. 2015; Van Mol et al. 2016; White et al. 2018).
Discussion
A limited number of studies (n = 8) were retrieved that included interventions for promoting relational practice with families in acute care settings. All the studies in the review were conducted in developed countries, where health resources, cultural and social perspectives of a family's role during illness and hospitalisation and the family's experience of illness may be different from that of developing countries (Shields 2015). According to the author, these differences play a crucial role in determining whether interventions maybe effectively translated to socially and culturally diverse populations. It is accordingly suggested that future studies be carried out in developing countries to provide valuable information on the socio-cultural and economic factors that may affect the development of family focused interventions.
The reviewed studies used different study designs with two studies being randomised controlled trials. Vincent (2010) stated that conducting randomised controlled trials in complex healthcare settings may be limited because of problems with timing and working with culturally diverse populations, adding that it may also be unrealistic to conduct studies on relationships in controlled environments. All the studies in the review used validated quantitative measures to assess the impact of the intervention on the participants. However, a limitation in using primarily quantitative measures to collect data is that quantitative measures do not capture the unique emotions and experiences of participants (Edelstein et al. 2017). It is recommended that future studies include qualitative approaches that are advantageous in collecting rich data on participant experiences, as well as mixed methods approaches, where quantitative and qualitative study approaches complement each other.
Similar to other interventional studies by Torke et al. (2016) and Heyland et al. (2018), the majority of the reviewed studies described multiple-component interventions. However, there is no compelling evidence that indicates whether multicomponent interventions are more effectively translated to practice than single-component interventions (Eldh & Wallin 2015; Squires et al. 2014). The majority of the reviewed studies focused on nurses as participants in their interventions. This may be attributed to the idea that collaboration and support of families are viewed as a nursing responsibility (Malliarou et al. 2014), or that nurses have a unique and constant relationship with families and patients and are thus best suited for interventions with families (Adams et al. 2014). However, collaborating with families must be a shared goal of all HCPs (Casimiro et al. 2015) and to this end, future interventions should strive to include all HCPs in family focused interventions.
When considering the outcomes of the interventions reported in the included studies, the family members indicated that their perceived expectations and needs were met by the interventions. Torke et al. (2016) recounted similar results in their studies, concluding that family and HCP collaboration may be improved with family members being involved in intervention development. Only a few reviewed studies included plans to sustain the interventions that had been developed. The importance of reporting on plans for sustainability is that it allows for maximisation of resources, realisation of health outcomes and on-going support and engagement by participants (Walugembe et al. 2019).
It was notable, that the interventions in the review, developed for acute care settings did address some elements of relational practice. Previous research has called for strategies to support family collaboration in acute care setting (Mackie, Marshall & Mitchell 2017).The element of HCPs respecting families' needs and honouring family differences in terms of their values systems and practices (Fletcher 1998; Jordan 2010) were addressed in only one of the reviewed studies. This finding maybe attributed to the fact that the studies were conducted in acute care settings, which are known to as task-oriented healthcare settings (Lloyd, Elkins & Innes 2018). The workload and time pressures often restrict HCP's interactions with families.
The nature of family engagement in the interventions varied, according to the dimensions proposed by Knafl et al. (2017). Although most studies focused on optimising family functioning through the interventions, the interventions concentrated only on key family members. This may reflect limited attention to considering the family as a unit of care, that is, where each family member contributes to the well-being of the other and the family context impacts on the success of family-focused interventions (Knafl et al. 2017). The interventions of the current review involved family members as active participants. This can be contrasted to the results of a scoping review by Goodridge et al. (2018), which revealed that the family engagement in interventions was confined to family members receiving information. Engaging actively with family members indicates a possible movement of HCPs towards acknowledgement that families possess the expertise to contribute their own healthcare by virtue of their unique life experiences (Hartrick-Doane 2014).
Review limitations
Although the authors were rigorous in the review process, by using a recognised methodology it is possible that some studies could have been missed. Publication in English as an inclusion criterion may have led to the omission of important interventional studies published in other languages. Most of the studies identified in this scoping review were conducted in the ICU, thus limiting translation to other acute care settings especially the ED, which is characterised by transient care and focuses on rapid throughput of patients.
Conclusion
The findings of this review reiterate the fact that there is a scarcity of interventional studies focusing on genuine connection between families and HCPs in acute care settings. The interventions of the reviewed studies indicated variability regarding inclusion of the elements of relational practice and the nature of family engagement in the interventions. Taking into account the positive outcomes of family and HCP collaboration in the reviewed studies, it is recommended that ongoing training and education to capacitate HCPs relationally should be a major component in future interventions seeking to promote relational practice with families.
Acknowledgements
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
All authors have contributed to the conceptualisation, acquisition and analysis of data, as well as drafting and refining the manuscript.
Ethical considerations
This article followed all ethical standards for research without direct contact with human or animal subjects.
Funding information
The study was supported by a grant from the National Research Foundation (Research and Innovation Support and Advancement), reference: KFNU2016/02/A13.
Data availability
Data are available on special request from the corresponding author, W.E.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
Adams, J.A., Anderson, R.A., Docherty, S.L., Tulsky, J.A., Steinhauser, K.E., Bailey, D.E. Jr., 2014, 'Nursing strategies to support family members of ICU patients at high risk of dying', Heart Lung 43(5), 406-415. https://doi.org/10.1016/j.hrtlng.2014.02.001 [ Links ]
Arksey, H. & O'Malley, L., 2005, 'Scoping studies: Towards a methodological framework', International Journal of Social Research Methodology 8(1), 19-32. https://doi.org/10.1080/1364557032000119616 [ Links ]
Bhalla, A., Suri, V., Kaur, P. & Kaur, S., 2014, 'Involvement of the family members in caring of patients an acute care setting', Journal of Postgraduate Medicine 60(4), 382-385. https://doi.org/10.4103/0022-3859.143962 [ Links ]
Blackwell, R.W., Lowton, K., Robert, G., Grudzen, C. & Grocott, P., 2017, 'Using experience-based co-design with older patients, their families and staff to improve palliative care experiences in the emergency department: A reflective critique on the process and outcomes', International Journal of Nursing Studies 68, 83-94. https://doi.org/10.1016/j.ijnurstu.2017.01.002 [ Links ]
Brown, B.J., 2016, 'Mutuality in health care: review, concept analysis and ways forward', Journal of Clinical Nursing 25, 1464-1475. https://doi.org/10.1111/jocn.13180 [ Links ]
Burns, K.E.A., Misak, C., Herridge, M., Mead, M.O. & Oczkowski, S., 2018, 'Patient and family engagement in the ICU. Untapped opportunities and under-recognized challenges', American Journal of Respiratory and Critical Care Medicine 98(3), 310-319. https://doi.org/10.1164/rccm.201710-2032CI [ Links ]
Casimiro, L.M., Hall, P., Kuziemsky, C., O'Connor, M. & Varpio, L., 2015, 'Enhancing patient-engaged teamwork in healthcare: An observational case study', Journal of Interprofessional Care 29(1), 55-61. https://doi.org/10.3109/13561820.2014.940038 [ Links ]
Chien, W.T., Chiu, Y.L., Lam, L.W. & Ip, W.Y., 2006, 'Effects of a needs-based education programme for family carers with a relative in an intensive care unit: A quasi-experimental study', International Journal of Nursing Studies 43(1), 39-50. https://doi.org/10.1016/j.ijnurstu.2005.01.006 [ Links ]
Colquhoun, H., Levac, D., O'Brien, K.K., Straus, S., Tricco, A.C., Perrier, L. et al., 2014, 'Scoping reviews: Time for clarity in definition, methods, and reporting', Journal of Clinical Epidemiology 67(12), 1291-1294. https://doi.org/10.1016/j.jclinepi.2014.03.013 [ Links ]
Doane, G.H. & Varcoe, C., 2007, 'Relational practice and nursing obligations', Journal of Advanced Nursing Science 30(3), 192-205. https://doi.org/10.1097/01.ANS.0000286619.31398.fc [ Links ]
Duffey, T. & Somody, C., 2011, 'The role of Relational-Cultural Theory in mental health counseling', Journal of Mental Health Counseling 33(3), 223-242. https://doi.org/10.17744/mehc.33.3.c10410226u275647 [ Links ]
Edelstein, H., Schippke, J., Sheffe, S. & Kingsnorth, S., 2017, 'Children with medical complexity: A scoping review of interventions to support caregiver stress', Child Care Health Development 43(3), 323-333. https://doi.org/10.1111/cch.12430 [ Links ]
Eggenberger, S.K. & Sanders, M., 2016, 'A family nursing educational intervention supports nurses and families in an adult intensive care unit', Australian Critical Care 29(4), 217-223. https://doi.org/10.1016/j.aucc.2016.09.002 [ Links ]
Eldh, A.C. & Wallin, L., 2015, 'How single is "single" - Some pragmatic reflections on single versus multifaceted interventions to facilitate implementation: Comment on "translating evidence into healthcare policy and practice: Single versus multifaceted implementation strategies - Is there a simple answer to a complex question?"', International Journal on Health Policy Management 4(10), 699-701. https://doi.org/10.15171/ijhpm.2015.133 [ Links ]
Fletcher, J.K., 1998, 'Relational practice: A feminist reconstruction of work', Journal of Management Inquiry 7(2), 163-186. https://doi.org/10.1177/105649269872012 [ Links ]
Goodridge, D., Henry, C., Watson, E., McDonald, M., New, L., Harrison, H.L. et al., 2018, 'Structured approaches to promote patient and family engagement in treatment in acute care hospital settings: Protocol for a systematic scoping review', Systematic Reviews 7(35), 1-7. https://doi.org/10.1186/s13643-018-0694-9 [ Links ]
Hartrick, G., 2008, 'Relational capacity: The foundation for interpersonal nursing practice', Journal of Advanced Nursing 1997(26), 523-528. https://doi.org/10.1046/j.1365-2648.1997.t01-12-00999.x [ Links ]
Hartrick-Doane, G., 2014, 'Beyond relational oblivion', Advances in Nursing Science 37(2), 84-86. https://doi.org/10.1097/ANS.0000000000000021 [ Links ]
Hetland, B., McAndrew, N., Perazzo, J. & Hickman, R., 2018, 'A qualitative study of factors that influence active family involvement with patient care in the ICU: Survey of critical care nurses', Intensive & Critical Care Nursing 44, 67-75. https://doi.org/10.1016/j.iccn.2017.08.008 [ Links ]
Heyland, D.K., Davidson, J., Skrobik, Y., des Ordons, A.R., Van Scoy, L. J., Day, A.G. et al., 2018, 'Improving partnerships with family members of ICU patients: Study protocol for a randomized controlled trial', Trials 19(1), 1-11. https://doi.org/10.1186/s13063-017-2379-4 [ Links ]
Indovina, K., Keniston, A., Reid, M., Sachs, K., Zheng, C., Tong, A. et al., 2016, 'Real-time patient experience surveys of hospitalized medical patients', Journal of Hospital Medicine 11(4), 251-256. https://doi.org/10.1002/jhm.2533 [ Links ]
Jacobowski, N.L., Girard, T.D., Mulder, J.A. & Ely, E.W., 2010, 'Communication in critical care: Family rounds in the intensive care unit', American Journal of Critical Care 19(5), 421-430. https://doi.org/10.4037/ajcc2010656 [ Links ]
Jordan, J.V., 2010, Theories of psychotherapy. Relational-cultural therapy, American Psychological Association, Washington, DC. [ Links ]
Knafl, K.A., Havill, N.L., Leeman, J., Fleming, L., Crandell, J.L. & Sandelowski, M., 2017, 'The nature of family engagement in interventions for children with chronic conditions', Western Journal of Nursing Research 39(5), 690-723. https://doi.org/10.1177/0193945916664700 [ Links ]
Mackie, B.R., Marshall, A. & Mitchell, M., 2017, 'Acute care nurses' views on family participation and collaboration in fundamental care', Journal of Clinical Nursing 27(11-12), 2346-2359. https://doi.org/10.1111/jocn.14185 [ Links ]
Malliarou, M., Gerogianni, G., Babatsikou, F., Kotrotsiou, E. & Zyga, S., 2014, 'Family perceptions of intensive care unit nurses' roles: A Greek perspective', Health Psychology Research 2(1), 1-4. https://doi.org/10.4081/hpr.2014.994 [ Links ]
Mitchell, M., Chaboyer, W., Burmeister, E. & Foster, M., 2009, 'Positive effects of a nursing intervention on family-centered care in adult critical care', American Journal of Critical Care 18(6), 543-552. https://doi.org/10.4037/ajcc2009226 [ Links ]
Östlund, U. & Persson, C., 2014, 'Examining family responses to family systems nursing interventions: An integrative review', Journal of Family Nursing 20(3), 259-286. https://doi.org/10.1177/1074840714542962 [ Links ]
Page, M.J., McKenzie, J.E., Bossuyt, P.M., Boutron, I., Hoffmann, T.C., Mulrow, C.D. et al., 2021, 'The PRISMA 2020 statement: An updated guideline for reporting systematic reviews,' The British Medical Journal 20372(71), 1-9. https://doi.org/10.1136/bmj.n71 [ Links ]
Shields, L., 2015, 'What is "family centred care"?', European Journal of Person Centred Healthcare 3(2), 139-144. https://doi.org/10.5750/ejpch.v3i2.993 [ Links ]
Squires, J.E., Sullivan, K., Eccles, M.P, Warwick, J. & Grimshaw, J.M., 2014, 'Are multifaceted interventions more effective than single-component interventions in changing health-care professionals' behaviours? An overview of systematic reviews', Implementation Science 9(152), 1-22. https://doi.org/10.1186/s13012-014-0152-6 [ Links ]
Svavarsdottir, E.K., Sigurdardottir, A.O., Konradsdottir, E., Stefansdottir, A., Sveinbjarnardottir, E.K., Ketilsdottir A. et al., 2015, 'The process of translating family nursing knowledge into clinical practice', Journal of Nursing Scholarship 47(1), 5-15. https://doi.org/10.1111/jnu.12108 [ Links ]
Torke, A.M., Wocial, L.D., Johns, S.A., Sachs, G.A., Callahan, C.M., Bosslet, G.T. et al., 2016, 'The family navigator: A pilot intervention to support intensive care unit family surrogates', American Journal of Critical Care 25(6), 498-507. https://doi.org/10.4037/ajcc2016730 [ Links ]
Van Mol, M.M., Boeter, T.G., Verharen, L., Kompanje, E.J., Bakker, J. & Nijkamp, MD., 2016, 'Patient- and family-centred care in the intensive care unit: A challenge in the daily practice of healthcare professionals', Journal of Clinical Nursing 26(19-20), 3212-3223. https://doi.org/10.1111/jocn.13669 [ Links ]
Vincent, J.L., 2010, 'We should abandon randomized controlled trials in the intensive care unit', Critical Care Medicine 38(10 Suppl), S534-S538. https://doi.org/10.1097/CCM.0b013e3181f208ac [ Links ]
Walugembe, D.R., Sibbald, S., Janzen Le Ber, M.J. & Kothari, A., 2019, 'Sustainability of public health interventions: Where are the gaps?', Health Research Policy and Systems 17(8), 1-7. https://doi.org/10.1186/s12961-018-0405-y [ Links ]
White, D.B., Angus, D.C., Shields, A.M., Buddadhumaruk, P., Pidro, C., Paner, C. et al., 2018, 'A randomized trial of a family-support intervention in intensive care units', The New England Journal of Medicine 378(25), 2365-2375. https://doi.org/10.1056/NEJMoa1802637 [ Links ]
Williams, S., Nolan, M. & Keady, J., 2009, 'Relational practice as the key to ensuring quality care for frail older people: Discharge planning as a case example', Quality in Aging 10(3), 44-55. https://doi.org/10.1108/14717794200900024 [ Links ]
Zou, P., 2016, 'Relational practice in nursing: A case analysis', Nursing and Health Care 1(1), 1-5, viewed 12 November 2017, from http://edelweisspublications.com/edelweiss/article/Relational-Practice-Nursing-Case-Analysis-NHC-16-102.pdf. [ Links ]
 Correspondence:
Correspondence:
Waheedha Emmamally
emmamally@ukzn.ac.za
Received: 10 May 2021
Accepted: 29 Oct. 2021
Published: 14 Feb. 2022














