Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Health SA Gesondheid (Online)
versão On-line ISSN 2071-9736
versão impressa ISSN 1025-9848
Health SA Gesondheid (Online) vol.25 Cape Town 2020
http://dx.doi.org/10.4102/hsag.v25i0.1421
ORIGINAL RESEARCH
Anaemia prevalence and dietary diversity among women in the rural Free State, South Africa
Elizabeth M. JordaanI; Violet L. van den BergI; Francois C. van RooyenII; Corinna M. WalshI
IDepartment of Nutrition and Dietetics, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIDepartment of Biostatistics, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Anaemia, a global public health problem that particularly affects women, holds major consequences for human health.
AIM: Determining dietary diversity, prevalence of anaemia and contraception use.
SETTING: Rural women, 25-49 years, in the Free State Province, South Africa.
METHODS: In a cross-sectional descriptive quantitative study, dietary diversity was determined with a 24-h recall; biochemical markers of anaemia, iron deficiency and inflammation were measured; and contraceptive use was recorded
RESULTS: Of 134 women (median age 41 years), 51.5% had medium, and 44.8% had low dietary diversity. Overall, 76.9% consumed flesh meats and fish, but only 25.4% ate dark green leafy vegetables. Anaemia was present in 4.6%; 1.5% presented with iron deficiency; and 0.7% presented with iron deficiency anaemia, evidenced by low ferritin levels. However, 45.0% had elevated C-reactive protein (CRP). Overall, 7.5% presented with elevated homocysteine levels, but only 3.8% had low red cell folate levels. More than half (54.1%) reported menstruating regularly and 71.6% used injectable contraceptives. Significant associations were found between median mean corpuscular volume (MCV) and mean corpuscular haemoglobin (MCH) and dietary diversity score.
CONCLUSIONS: Although the prevalence of anaemia is low in this population, elevated CRP in almost half indicates that inflammation may mask iron deficiency. The older median age of the sample and approximately half of the women not menstruating regularly may also contribute to the low anaemia prevalence. Attention should be given to the women's diets as almost half consume diets of low diversity, and not all consume foods rich in haemopoietic nutrients.
Keywords: anaemia; dietary diversity; folate; iron; iron deficiency.
Introduction
The global public health problem of anaemia affects women living in both developed and developing countries and holds major consequences for human health as well as economic development (Kassebaum & the Global Burden of Anemia Collaborators [GBD] 2016; World Health Organization [WHO] 2008). Although anaemia can occur in all stages of the lifecycle, it is more prevalent among women and young children (WHO 2014). Women of childbearing age lose iron through their menstrual blood loss, while pregnant women have an increased need for iron and therefore have a greater risk for developing anaemia (Milman 2011). According to findings of the South African National Health and Nutrition Examination Survey (SANHANES-1) published in 2013, the prevalence of anaemia among women of child-bearing age (15-54 years) ranged from 23.1% to 24.7% (Shisana et al. 2013). Research directed at nutritional anaemias largely focuses on iron-deficiency anaemia which remains the most dominant form of anaemia in the world (Kassebaum & GBD 2016). In 2011, 29% of non-pregnant women suffered from anaemia, while globally half a billion women of reproductive age are affected by it (Stevens et al. 2013). In contrast, however, little global data exist on the contribution of folate deficiency towards the development of anaemia (Balarajan et al. 2011).
Anaemia is defined as a significant reduction in the mass of circulating red blood cells, resulting in a diminished oxygen binding capacity of blood (Bunn 2011). Nutritional anaemias result from the insufficient bioavailability of haemopoietic nutrients (iron, vitamin B12 and folic acid) which could lead to symptoms including extreme fatigue and lethargy, amongst others (Biesalski & Erhardt 2007). A study conducted by Abrahams, Mchiza and Steyn (2011) concluded that a large proportion of the South African population is in a stage of nutrition transition where changes in dietary patterns are affecting health outcomes. This transition could also impact on anaemia.
The World Health Assembly aims to achieve a 50% reduction in the prevalence of anaemia amongst reproductive women by 2025 (WHO 2014). In order to improve maternal health and thus ensure a woman's safe passage into motherhood, quality reproductive health services, accompanied by a series of well-timed interventions, should be implemented (UN 2010). A diet sufficient in all the required nutrients before and during pregnancy in order to enhance fertility, to support the pregnancy and the growing foetus, and to promote long-term health is of utmost importance (Derbyshire 2011), as the effect of poor nutritional status may follow both the mother and child for decades (Gallagher 2012).
Contraception could possibly play a role in lowering the risk for iron deficiency anaemia as it aids in reducing the number of pregnancies and the time interval between consecutive pregnancies (thus reducing the amount of iron needed for more pregnancies in a shorter time interval) (UNDP/UNFPA/WHO/WB 1998). The continuous use of contraceptives has been found to decrease the risk for anaemia significantly (Bellizzi & Ali 2018; Haile et al. 2017) possibly by reducing the amount of blood (menstrual) lost during this time (Yeasmin et al. 2010).
According to the WHO (2008), estimates of the prevalence of anaemia are only useful when associated with the prevailing causal factors (e.g. poor dietary intake) in specified settings. It is essential to collect accurate information concerning these factors, as they are multiple and complex and can serve as the basis for the development of appropriate interventions (WHO 2008).
Although various studies related to anaemia have been conducted in South Africa, limited data are available regarding the prevalence of anaemia among Southern African women in general and in the Free State province in particular. This study aimed to determine the prevalence of anaemia, dietary diversity, as well as contraceptive use in women aged 25-49 years in three rural towns in the Free State and to determine associations between biochemical indices and dietary diversity.
Research methods and design
Background
This study reports on findings from the 'Assuring Health for All in the Free State' (AHA-FS) research programme, which was an epidemiological study that aimed to determine how living in rural and urban areas affected lifestyle and indicators of health. The Free State Rural Development Partnership Programme (FSRDPP) includes the Trompsburg, Philippolis and Springfontein municipalities, where students from the Department of Nutrition and Dietetics at the University of the Free State do their rural internship. These three towns formed part of the rural phase of the AHA-FS study. A multidisciplinary research team investigated the socio-demographic status, household food security, dietary intake, levels of physical activity, as well as the knowledge, attitudes and practices related to nutrition, and reported health status of the study population by using standardised questionnaires. In addition to a medical examination, anthropometric measurements and blood specimens were also obtained for various investigations.
Research design and aim
For the purpose of this study, data from the rural phase of the original study were used and applied in a cross-sectional investigation.
Haematological abnormalities of both HIV-infected and HIV-uninfected persons in the AHA study population have been published by Groenewald et al. (2011), but data on the risk factors associated with the development of anaemia within these communities have not been investigated.
Population and sampling
All households in the township areas (excluding farms) in the rural towns of Trompsburg, Philippolis and Springfontein could participate in the original study. For this study, the total population of 134 women aged 25-49 years who were HIV-uninfected, gave informed consent and were not pregnant at the time of data collection were selected from the AHA-FS database.
Measuring instruments and procedures
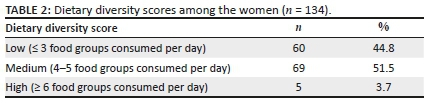
Information was obtained via structured interviews. A 24-h recall was used to determine individual dietary diversity. The dietary diversity score was determined by using the tool developed by the Food and Agriculture Organization (FAO). This tool summarises the number of food groups obtained from the 24-h recall into nine standardised food groups, namely starchy staples, dark green leafy vegetables, other vitamin A-rich fruit and vegetables, other fruits and vegetables, organ meat, flesh meat and fish, eggs, legumes, nuts and seeds and milk and milk products (FAO 2011). According to this tool, a low dietary diversity score was allocated if three food groups or less were consumed, a medium score where four to five food groups were consumed and a high score where six or more food groups were consumed. Questions relating to contraceptive use were included in the health questionnaire.
After an overnight fast, staff and registrars from the Department of Chemical Pathology, University of the Free State, collected respondents' blood the next morning. The samples were stored immediately in ice-filled containers and transported to the laboratory. The blood samples were analysed according to standard techniques at the National Health Laboratory Service Laboratory at the University of the Free State. Full blood counts were determined using a Roche Sysmex XT 2000i® analyser, serum ferritin using a Beckman Coulter Synchron LX20, and transferrin and homocysteine levels using BN Prospec System nephelometric technology. Serum folate levels were recorded using a Bayer Advia Centaur System. C-reactive protein (CRP) was determined by means of the immunoturbidimetric method.
Anaemia was diagnosed when haemoglobin levels were below 12.0 g/dL (WHO 2008). According to the WHO (2008), iron deficiency is diagnosed when ferritin levels are below 15.0 ng/mL and haemoglobin levels are still greater than 12.0 g/dL. Iron deficiency anaemia is diagnosed when both ferritin and haemoglobin levels are below 15.0 ng/mL and 12.0 g/dL, respectively. These cut-off values were also used in this study to define iron deficiency and iron deficiency anaemia. CRP was considered elevated if greater or equal to 5 mg/L (NHLS reference values).
Statistical analysis
Statistical analysis was performed using the Predictive Analytics SoftWare (PASW) Statistics Student version 22.0 by Statistical Package for the Social Sciences (SPSS) (IBM 2013). Frequencies and percentages were recorded for categorical data and medians and percentiles for continuous data. Only six out of the 134 women in the sample suffered from anaemia (haemoglobin < 12.0 g/dL), which made determining associations, especially between women suffering from anaemia and those who did not, difficult. The Kruskal-Wallis test and post-hoc Dunn's test were used to compare iron and anaemia status markers among dietary diversity scores. Type I error rate was set at 5% (p < 0.05).
Ethical considerations
Ethical approval was obtained from the Health Sciences Research Ethics Committee of the University of the Free State (ETOVS number 21/07), the Department of Health and local municipalities, 2007/01/25. Each respondent was assigned a particular number to ensure confidentiality. Ethical approval was obtained from the Health Sciences Research Ethics Committee of the University of the Free State the Department of Health and local municipalities. Participation was voluntary and respondents could withdraw from the study at any time.
Results
Of the complete data set available as part of the "AHA-FS" study, 38.5% related to women between 25 and 49 years of age. After applying the exclusion criteria, 23.3% of the original data set could be included in the current study, resulting in a sample size of 134 women, with a median age of 41 years.
The women's diet was predominantly based on starchy staples (Table 1). Flesh meat and fish, which are rich sources of iron, were consumed by more than three-quarters of the women, whereas sources of folate (dark green leafy vegetables and organ meats) were consumed by only approximately a quarter of the sample.

Overall, almost half (44.8%) of the women had a low dietary diversity score, while 51.5% had a medium dietary diversity score. Only a relatively small percentage (3.7%, 5/134) of the women had a high dietary diversity score (Table 2).
The percentage of women in this study presenting with low dietary diversity scores (≤ 3 food groups consumed per day) differs from various other studies related to dietary diversity undertaken in South Africa (Table 3).

The medians for all the blood values (haemoglobin, haematocrit, MCV, MCH, transferrin saturation, ferritin, homocysteine, red cell folate levels and CRP) were within normal limits (Table 4).
Low haemoglobin levels were observed in 4.6% (6/134) of the women with only a small percentage presenting with low haematocrit (3.1%, 4/134), mean corpuscular volume (MCV) (3.1%, 4/134) and mean corpuscular haemoglobin (MCH) (7.6%, 10/134). Elevated MCH was present in a quarter (25.2%, 33/134) of the women.
Below normal transferrin saturation was found in 12.2% (9/134) of the women, with 1.4% (1/134) displaying low ferritin levels. The prevalence of anaemia, iron deficiency and iron deficiency anaemia in the current study was much lower than the findings of the SANHANES-1 published in 2013 (Table 5). Even though only 4.6% of the sample suffered from anaemia, seven out of the 134 women (5.2%) who presented with a low MCH, but normal haemoglobin levels were at risk for developing anaemia.
Both the medians for homocysteine and red cell folate were also within normal limits. Elevated homocysteine levels occurred in 7.5% (10/134) of the women and 3.8% (5/134) had low red cell folate levels.
The median for CRP was normal (4.6 mg/L); however, 45.0% of the women presented with elevated CRP.
When assessing the prevalence of iron deficiency, it is important to consider menstruation patterns and contraceptive use (Table 6). Just over half (54.1%) of the women regularly menstruated and almost three quarters (71.6%) of them currently or previously made use of injectable contraceptives.

As expected, a significant association was found between median haemoglobin and whether the women still menstruated or not (p = 0.008) (Table 7). These median haemoglobin levels were within the normal range for both women who menstruated (13.7 g/dL) and women who did not (14.2 g/dL). No significant association was found between haemoglobin levels and women who currently or previously used injectable contraceptives and those that did not (p = 0.847). A significant association was found between ferritin levels and whether women had elevated CRP (p = 0.044).
CRP, C-reactive protein; MCV, mean corpuscular volume; MCH, mean corpuscular haemoglobin.
No significant associations were found between dietary diversity scores and any of the blood parameters (p > 0.05), except for median MCV (p = 0.029) and median MCH (p = 0.019). Median MCV were within the normal range for both the group with low dietary diversity scores (94.9 fl) and those with medium to high dietary diversity scores (92.9 fl). Similarly, median MCH were also within the normal range for those who had a low dietary diversity score (31.0 pg/cell), as well as those who had a medium to a high score (30.0 pg/cell). No significant associations were found between haemoglobin and the intake of flesh meats and fish food group (p = 0.511) and the organ meats group (p = 0.281).
Discussion
With this study, we aimed to assess the dietary diversity, presence of anaemia and related factors (menstruation and contraceptive use) in a group of women aged 25-49 years living in low socio-economic townships in the rural Free State towns of Trompsburg, Philippolis and Springfontein. As a result of the significant effects of anaemia on human health (e.g. reduced resistance to blood loss during delivery leading to increased maternal morbidity and mortality) (Kassebaum & GBD 2016), it was considered desirable to determine the need for intervention studies within this population.
Almost half of the women in this study had a low dietary diversity score, indicating that their diet needed attention in terms of the nutrient adequacy. The prevalence of low dietary diversity in this study was similar to that of the SANHANES-1 study (Table 3) (Shisana et al. 2013).
Almost a quarter of the women did not consume flesh meat and fish, which are excellent sources of the more bioavailable haem iron. The diets of the women seemed to be mostly starch-based, with low intakes of other iron-rich foods including organ meats, eggs and dark green leafy vegetables. Only a quarter of the women consumed dark green leafy vegetables, and an even smaller proportion ate legumes, which are also a rich source of folate. Dark green leafy vegetables are excellent sources of folate and the less bioavailable form of non-haem iron (Milman 2011), the absorption of which can be impaired by phytates present in some grains. The low intake of iron and folate-rich sources was similar to findings in a study conducted on non-pregnant women older than 19 years living in rural areas in KwaZulu-Natal (Kolahdooz, Spearing & Sharma 2013).
In this study, only a small proportion of the women had low haemoglobin levels indicative of anaemia. This is much lower than that reported in the SANHANES-1 study, where almost a quarter of the women between 16-35 years and 35-44 years in South Africa and 17.6% of women between 16 and 35 years in the Free State suffered from anaemia (Shisana et al. 2013). The prevalence of anaemia in this study was also much lower than the results from a systematic review by Stevens et al. (2013). Their review included population representative data where, in 2011, 29% of non-pregnant South African women aged 15-49 years suffered from anaemia. According to the National Food Consumption Survey - Fortification Baseline (NFCS-FB) survey, conducted in 2005 among women of reproductive age (15-35 years), 23.2% of women in the Free State Province suffered from anaemia (Labadarios et al. 2007). These studies, however, did not report on menstruation and contraceptive use, which may account for some of the differences.
In our study population, almost half of the women were not menstruating, and a large proportion of the sample made use of injectable contraceptives. Both of these factors may have decreased their risk of developing iron deficiency and thus possibly contributed to the low prevalence of iron deficiency in the current sample. Indeed, women in the sample who were still regularly menstruating had significantly lower median haemoglobin levels than those who were not. Results from the current study showed that a large number of women were currently or had previously made use of injectable contraceptives. Studies by Bellizzi and Ali (2018) and Haile et al. (2017) support the fact that the risk for anaemia is decreased with the use of contraceptives. The SANHANES-1 study did not report on contraceptive use and the effects thereof on anaemia.
Iron deficiency anaemia develops in three stages. The first stage is characterised by the depletion of iron stores, which is confirmed by low serum ferritin levels. During the second stage, serum ferritin decreases further with transferrin saturation decreasing as well. In the third stage, haemoglobin levels decrease, microcytosis and hypochromia of the erythrocytes develop, and signs and symptoms of anaemia appear (Gaw et al. 2008).
Low MCV levels, indicating microcytic anaemia, and low MCH levels, indicating hypochromic anaemia, in combination with decreased haemoglobin levels indicate iron deficiency anaemia. A quarter (25.2%) of the women in our study had increased levels of MCH, which is seen in macrocytic anaemia. Considering these factors, in combination with ferritin levels, it is evident that a very small percentage (1.4%, 1/134) had low iron stores. Serum ferritin levels in this study were much higher than reported in SANHANES-1, where 13.5% of women aged 16-35 years had low serum ferritin levels (Shisana et al. 2013). The higher serum ferritin levels in this study may have been linked to contraception, as a study on non-pregnant women, aged 18-40 years, in Bangladesh, Chile, China, the Dominican Republic, Pakistan, Thailand and Tunisia, in the period 1988-1992, concluded that contraceptive use has a beneficial effect on ferritin levels (UNDP/UNFPA/WHO/WB 1998).
It is important to consider that serum ferritin levels may be elevated because of inflammation and infection (Gaw et al. 2008). As ferritin is an acute phase protein that is sensitive to inflammation, some authors suggest that ferritin may rather be a marker of inflammation than iron status in individuals who are suffering from chronic inflammation, commonly seen in overweight and obese individuals (Dignass, Farrag & Stein 2018; Khan et al. 2016). In order to correct ferritin for inflammation, Thurnham, Northrop-Clewes and Knowles (2015) proposed a method using CRP and α1-acid glycoprotein (AGP). AGP was unfortunately not measured as part of the main study and adjusted ferritin could therefore not be determined. It is, however, important to note that almost a third of the women in this study presented with elevated ferritin levels. Considering that CRP was elevated in almost half (45.0%) of the women, and a significant association was found between elevated CRP and ferritin levels, prevalence of iron deficiency could thus be underestimated. Cappellini et al. (2017), proposed that iron deficiency be diagnosed in the presence of inflammatory conditions when serum ferritin levels fall below 100 mcg/L. When applying this cut-off value to the women in this study who presented with inflammation (elevated CRP), 74.1% (20/27) suffered from iron deficiency. Although this method has only recently been proposed, it is worth noting that the prevalence of iron deficiency can be greatly affected by the presence of inflammation.
When taking into account the WHO (2007) haemoglobin and serum ferritin cut-off values for diagnosing iron status, one woman (0.7%) suffered from iron deficiency anaemia (low ferritin and haemoglobin) and two women (1.5%) had an iron deficiency (low ferritin only). Iron deficiency anaemia was present in 9.7% of women of reproductive age in the SANHANES-1 study. Differences in the prevalence of anaemia and iron deficiency anaemia could also be attributed to the older median age of the women in this study compared to the SANHANES-1 study (Shisana et al. 2013). Women of younger fertile age have a greater risk for developing anaemia, particularly because of iron deficiency, because of blood loss during menstruation (Yeasmin et al. 2010).
Homocysteine levels rise and spill into the circulation when either folate or vitamin B12 is lacking, thus possibly indicating folate or vitamin B12 deficiency (Litchford 2012). Overall, 3.8% of the women had red cell folate levels below the reference value, indicating low folate status, which was much lower than the estimated prevalence of folate deficiency in 25% - 72% of women of reproductive age (Milman 2011). This difference could be because of the small sample size in this study, but also because of the intake of starchy staples, fortified with folic acid, by all of the women. Optimal folate status in women of childbearing age is of utmost importance as neural tube closure occurs at 28 weeks of pregnancy, a time when most pregnant women do not yet know that they are pregnant (Derbyshire 2011).
Median MCV and MCH decreased significantly as dietary diversity scores increased; however, all of these medians were still within the normal range. The unexpected direction of these associations may reflect on the effects of the mandatory fortification of food in South Africa. Studies conducted by Keats et al. (2019) and Garcia-Casal et al. (2018) found that food fortification had a small, but significant effect on the lowering of the prevalence of anaemia.
Although no significant association could be found between any of the blood parameters, except for MVC and MCH, and dietary diversity score, as well as any of the blood parameters and the flesh meats and fish food group and the organ meats group, there is literature suggestive of the fundamental importance of iron and folate in maternal health (WHO 2006). When considering what is known now regarding the low prevalence of anaemia and the adequacy of the women's diets in this study, it may possibly be an indication of the effect of the mandatory food fortification of maize meal and wheat flour with folic acid and iron, amongst others, that came into effect in South Africa in October 2003 (DoHSA 2007). Food fortification may be a solution to address micronutrient malnutrition, particularly in terms of iron and folate; however, implementing other solutions as well as further studies may add value.
Limitations of the study
The small sample size proved to be the greatest limitation of this study, which may question whether it is representative. The older median age may also have impacted on the representativity as the majority of the women may have presented with menopause. This could have impacted on the low prevalence of anaemia. The prevalence of iron deficiency and iron deficiency anaemia may also have been underestimated as it was not possible to adjust for inflammation in this study. However, we believe that this study is still of value as it provides an indication of the dietary adequacy and the prevalence of anaemia in these women.
The dietary assessment reflects only one day of the diet of the women, which is not necessarily an accurate representation of the overall dietary adequacy. When interpreting dietary diversity scores, it is important to keep in mind that the quantity of food consumed is not measured; the diet can vary across seasons where some foods are only available in large quantities and at low affordable prices for short periods of time; and that the variety available in rural areas may differ from that of urban areas (FAO 2011).
Conclusion and recommendations
The women in this study consumed a diet with moderate variety which was based on starchy staple foods. Even though these women consumed little foods from the iron and folate containing food groups, the prevalence of iron deficiency, iron deficiency anaemia and folate deficiency was low. The low prevalence could be attributed to the large percentage with elevated CRP levels, almost half of the women not menstruating and the older median age.
The results of this study will be used to plan sustainable community-based intervention strategies to improve the dietary adequacy of the women living in the Free State, where the dietetics students from the Department of Nutrition and Dietetics of the University of the Free State provide key nutrition services. These strategies should be appropriate and culturally acceptable and should involve the diversification of the diets of women living in the Free State, specifically focusing on improving the intake of iron and folate-rich food sources, as well as reducing those factors that may inhibit the absorption. We believe that projects encouraging the growing of vegetable gardens that are currently being implemented in the low socio-economic communities in Trompsburg, Philippolis and Springfontein should receive more attention, along with the promotion of raising chickens.
These interventions are important, even though the prevalence of anaemia in our study population is low, as the consequences of the nutrition transition may still impact on the health of these women and their offspring. We believe that the effectiveness of already established nutrition intervention strategies, as well as the strategies mentioned earlier, would benefit from further research on this population. Also, a follow-up study to identify the reasons for high levels of serum ferritin is recommended.
Reducing the burden of disease in developing communities in South Africa can be expected to contribute to sustainable livelihoods and improved health outcomes.
Acknowledgements
The National Research Foundation (NRF) is gratefully acknowledged for its financial assistance in the original study. We also acknowledge all the volunteers from the Springfontein, Trompsburg and Philippolis who participated in the study.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
This article is based on research conducted by E.M.J. under the supervision of C.M.W. and co-supervision of L.v.d.B and F.C.v.R.
Funding information
The National Research Foundation (NRF) is gratefully acknowledged for its financial assistance in the original study. No additional funding was sought for this study.
Data availability statement
Data sharing is not applicable to this article as no new data were created or analysed in this study.
Disclaimer
The views expressed in this article are the authors' own and not an official position of the institution or funder.
References
Abrahams, Z., Mchiza, Z. & Steyn, N.P., 2011, 'Diet and mortality rates in Sub-Saharan Africa: Stages in the nutrition transition', BioMed Central Public Health 11(1), 801-812, viewed 15 January 2015, from https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-11-801. [ Links ]
Ampath, 2010, Ampath desk reference: Guide to laboratory tests, Ampath, Centurion. [ Links ]
Balarajan, Y., Ramakrishnan, U., Ozaltin, E., Shankar, A.H. & Subramanian, S.V., 2011, 'Anaemia in low-income and middle-income countries', The Lancet 378(1), 2123-2125, viewed 15 January 2015, from https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)62304-5/fulltext. [ Links ]
Bellizzi, S. & Ali, M.M., 2018, 'Effect of oral contraception on anemia in 12 low- and middle-income countries', Contraception 2018(1), 236-242, viewed 28 June 2018, from https://pubmed.ncbi.nlm.nih.gov/29133111/. [ Links ]
Biesalski, H.K. & Erhardt, J.G., 2007, 'Diagnosis of nutritional anemia - Laboratory assessment of iron status', in K. Kraemer & M.B. Zimmerman (eds.), Nutritional anemia, pp. 37-44, Sight and Life. [ Links ]
Bunn, H.F., 2011, 'Approach to the anaemias', in L. Goldman & A.I. Schafer (eds.), Goldman's Cecil medicine, pp. 1031-1039, W.B. Saunders, St. Louis, MO. [ Links ]
Cappellini, M.D., Comin-Colet, J., De Francisco, A., Dignassm, A., Doehnerm W., Lam, C.S.P. et al., 2017, 'Iron deficiency across chronic inflammatory conditions: International expert opinion on definition, diagnosis, and management', American Journal of Hematology 2017(92), 1068-1078, viewed 28 June 2018, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5599965/. [ Links ]
Chakona, G. & Shackleton, G., 2017, 'Minimum dietary diversity scores for women indicate micronutrient adequacy and food insecurity status in South African towns', Nutrients 9(812), viewed 28 June 2020, from https://www.mdpi.com/2072-6643/9/8/812. [ Links ]
Department of Health South Africa (DoHSA), 2007, A reflection of the South African maize meal and wheat flour fortification programme (2004 to 2007), DoHSA, Pretoria. [ Links ]
Derbyshire, E., 2011, Nutrition in the childbearing years, Wiley-Blackwell, West Sussex. [ Links ]
Dignass, A., Farrag, K. & Stein, J., 2018, 'Limitations of serum ferritin in diagnosing iron deficiency in inflammatory conditions', International Journal of Chronic Diseases 2018(1), viewed 26 June 2019, from https://www.hindawi.com/journals/ijcd/2018/9394060/. [ Links ]
Food and Agriculture Organisation (FAO), 2011, Guidelines for measuring household and individual dietary diversity, FAO, Rome. [ Links ]
Gallagher, M.L., 2012, 'Intake: The nutrients and their metabolism', in L.K. Mahan, S. Escott-Stump & J.L. Raymond (eds.), Krause's food and the nutrition care process, pp. 32-142, Saunders, St. Louis, MO. [ Links ]
Garcia-Casal, M.N., Peña-Rosas, J.P., De-Regil, L.M., Gwirtz, J.A. & Pasricha, S.R., 2018, 'Fortification of maize flour with iron for controlling anaemia and iron deficiency in populations', Cochrane Database of Systematic Reviews 2018(1), viewed 26 June 2019, from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010187.pub2/epdf/full. [ Links ]
Gaw, A., Murphy, M.J., Cowan, R.A., O'Reilly, D.J., Stewart, M.J. & Shepherd, J., 2008, Clinical biochemistry: An illustrated colour text, 4th edn., Churchill Livingstone Elsevier, Edinburgh. [ Links ]
Groenewald, A.J., Van Wyk, H.J., Walsh, C.M., Van der Merwe, L.J. & Van Zyl, S., 2011, 'Staging and haematological abnormalities of HIV-infected persons in the rural Free State Province of South Africa', African Journal of Primary Health Care Family Medicine 3(1), 222, viewed 15 January 2015, from https://doi.org/10.4102/phcfm.v3i1.222 [ Links ]
Haile, Z.T., Kingori, C., Teweldeberhan, A.K. & Chavan, B., 2017, 'The relationship between history of hormonal contraceptive use and iron status among women in Tanzania: A population-based study', Sexual & Reproductive Healthcare 13, 97-102, viewed 28 June 2018, from https://pubmed.ncbi.nlm.nih.gov/28844365/. [ Links ]
International Business Machines (IBM) Corporation, Released 2013, IBM SPSS Statistics for Windows, Version 22.0, Armonk, IBM Corporation, NY. [ Links ]
Kassebaum, N.J. & the Global Burden of Anemia Collaborators (GBD), 2016, 'The global burden of anemia', Hematology/Oncology Clinics of North America 30(2), 247-308, viewed 18 February 2018, from https://pubmed.ncbi.nlm.nih.gov/27040955/. [ Links ]
Keats, E.C., Neufeld, L.M., Garrett, G.S., Mbuya, M.N.N. & Bhutta, Z.A., 2019, 'Improved micronutrient status and health outcomes in low- and middle-income countries following large-scale fortification: Evidence from a systematic review and meta-analysis', American Journal of Clinical Nutrition 109(1), 1696-1708, viewed from 26 June 2019, https://academic.oup.com/ajcn/article/109/6/1696/5475063 [ Links ]
Khan, A., Khan, W.M., Ayub, M., Humayun, M. & Haroon, M., 2016, 'Ferritin is a marker of inflammation rather than iron deficiency in overweight and obese people', Journal of Obesity 2016(1), viewed 28 June 2018, from https://www.hindawi.com/journals/jobe/2016/1937320/. [ Links ]
Kolahdooz, F., Spearing, K. & Sharma, S., 2013, 'Dietary adequacies among South African adults in rural KwaZulu-Natal', PLoS One 8(6), 1-6, viewed 15 January 2015, from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0067184. [ Links ]
Labadarios, D., Steyn, N.P. & Nel, J., 2011, 'How diverse is the diet of adult South Africans?', Nutrition Journal 10(1), 33-43, viewed 15 January 2015, from https://nutritionj.biomedcentral.com/articles/10.1186/1475-2891-10-33#:~:text=Conclusion,vegetables%2C%20were%20the%20least%20consumed. [ Links ]
Labadarios, D., Swart, R., Maunder, E.M.W., Kruger, H.S., Gericke, G.J., Kuzwayo, P.M.B. et al., 2007, National Food Consumption Survey - Fortification Baseline (NFCS-FB), SADoH, Pretoria. [ Links ]
Litchford, M.D., 2012, 'Clinical: Biochemical assessment', in L.K. Mahan, S. Escott-Stump & J.L. Raymond (eds.), Krause's food and the nutrition care process, pp. 191-208, Saunders, St. Louis, MO. [ Links ]
Milman, N., 2011, 'Anemia-still a major health problem in many parts of the world', Annals of Hematology 90(1), 369-377, viewed 15 January 2015, from https://link.springer.com/article/10.1007%2Fs00277-010-1144-5. [ Links ]
National Health Laboratory Services (NHLS), 2014, NHLS Handbook, NHLS Publication, viewed 15 January 2015, from https://www.nhls.ac.za/diagnostic-services/type-of-tests/ [ Links ]
Oldewage-Theron, W. & Kruger, R., 2011, 'Dietary diversity and adequacy of women caregivers in a peri-urban informal settlement in South Africa', Nutrition 27(1), 420-427, viewed 15 January 2015, from https://pubmed.ncbi.nlm.nih.gov/20688475/. [ Links ]
Shisana, O., Labadarios, D., Rehle, T., Simbayi, L., Zuma, K., Dhansay, A. et al., 2013, South African National Health and Nutrition Examination Survey (SANHANES-1), HSRC Press, Cape Town. [ Links ]
Stevens, G.A., Finucane, M.M., De-Regil, L.M., Paciorek, C.J., Flaxman, S.R., Branca, F. et al., 2013, 'Global, regional, and national trends in haemoglobin concentration and prevalence of total and severe anaemia in children and pregnant and non-pregnant women for 1995-2011: A systematic analysis of population-representative data', The Lancet 1(1), e16-e25, viewed 15 January 2015, from https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(13)70001-9/fulltext. [ Links ]
Thurnham, D.I., Northrop-Clewes, A. & Knowles, J., 2015, 'The use of adjustment factors to address the impact of inflammation on vitamin A and iron status in humans', The Journal of Nutrition 145(1), 1137S-1143S, viewed 28 June 2018, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4410494/. [ Links ]
United Nations (UN), 2010, The Millennium development goals report 2010, UN, New York, NY. [ Links ]
United Nations Development Programme/United Nations Population Fund/World Health Organization/World Bank (UNDP/UNFPA/WHO/WB), 1998, 'Effects of contraceptives on hemoglobin and Ferritin', Contraception 58(1), 261-273, viewed 15 January 2015, from https://pubmed.ncbi.nlm.nih.gov/9883381/. [ Links ]
World Health Organization (WHO), 2006, Iron and folate supplementation, WHO, Geneva. [ Links ]
World Health Organization (WHO), 2007, Assessing the iron status of populations, WHO, Geneva. [ Links ]
World Health Organization (WHO), 2008, Worldwide prevalence of anaemia 1993-2005: WHO global database on anaemias, WHO, Geneva. [ Links ]
World Health Organization (WHO), 2014, Comprehensive implementation plan on maternal, infant and young child nutrition, WHO, Geneva. [ Links ]
Yeasmin, T., Haque, S., Yeasmin, S. & Amin, R., 2010, 'Iron status in women using oral contraceptives', Bangladesh Journal of Physiology and Pharmacology 26(1&2), 25-29, viewed 15 January 2015, from https://www.banglajol.info/index.php/BJPP/article/view/19963. [ Links ]
 Correspondence:
Correspondence:
Elizabeth Jordaan
cronjeem@ufs.ac.za
Received: 13 Feb. 2020
Accepted: 05 Aug. 2020
Published: 06 Oct. 2020














