Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Health SA Gesondheid (Online)
On-line version ISSN 2071-9736
Print version ISSN 1025-9848
Health SA Gesondheid (Online) vol.22 Cape Town 2017
http://dx.doi.org/10.1016/j.hsag.2016.12.002
FULL LENGTH ARTICLE
An elderly, urban population: Their experiences and expectations of pharmaceutical services in community pharmacies
Alta Janse van Rensburg; Irma Kotze*; Martie Susanna Lubbe; Marike Cockeran
Research Entity: Medicine Usage in South Africa (MUSA), Faculty of Health Sciences, North West University, Potchefstroom Campus, South Africa
ABSTRACT
OBJECTIVE: The aim of this study was to determine the pharmaceutical services experiences of an elderly, urban population in relation to their expectations in community pharmacy.
DESIGN: and setting: The study was a cross-sectional descriptive empirical study and was conducted by means of a structured questionnaire, designed and administered by the researcher, in face-to-face interviews at an old age residence in the participants' own dwellings (N = 242). The management of this specific village approached the researcher about healthcare concerns for their residents and granted permission for this study to be conducted. Main outcome and results: The sample population of elderly patients (n = 67) had a higher expectation of community pharmacists, in terms of pharmaceutical services, than what they had experienced. Significant differences were found in all aspects examined. Effect size, amongst others, revealed that expectations were not met in discussions about the effect of other medicines on their chronic medicine (d = 1.94); whether they had any medicines left from previous issues (d = 1.77) and questions regarding existing chronic conditions (d = 1.69). There was an association between questions, regarding the use of chronic medicines at pharmacies and at other healthcare professionals (d = 0.26), as well as the supply of written information at pharmacies and other healthcare professionals (d = 0.42). The study reveals that this population has expectations of their community pharmacists that are not met.
CONCLUSIONS: Pharmacists can be active members of the healthcare team and restore their professional image in the eyes of the community, if they renew their attitudes, have confidence in their abilities and understand their role in patient care. The community pharmacist should focus on the health-related quality of life of the individual patient and identify the immediate healthcare needs of their unique community, with specific reference to vulnerable populations like the elderly. Pharmacists should establish themselves as the go-to healthcare professional.
Keywords: Elderly, Pharmaceutical services, Experiences and expectations, Community pharmacy, Face-to face interview , Researcher-designed structured questionnaire
1. Introduction
Healthcare has evolved from bloodletting to a highly-sophisticated science. Constant improvements in healthcare, contributes to the increased life expectancy of humanity. In South Africa, life expectancy increased by 13 years since 1960 (Mayosi et al., 2012). Actuaries estimate that life expectancy will increase by 1.5 years every decade (Jacobzone, Cambois, & Robine, 2001). The resulting increased number of elderly would want to live healthier for longer (Vaupel, 2010). Pharmacists, with expert medicine knowledge, supplying supportive pharmaceutical services, have an important role to play in the health-related quality of life in the elderly population. The pharmacist is the most accessible healthcare professional (McGann, 2012): no appointments are needed and the public considers the pharmacist as the first port of call in healthcare (Oakley, 2015).
Elderly patients use more medicine than those under 60 years of age (Benjamin, 2010). They are more likely to experience medicine-related problems due to multi-morbidities and the associated polypharmacy. These problems are compounded by low levels of education and language, and cultural differences between healthcare professional and patients (Nobili, Garanttini, & Mannucci, 2011). In the light of the increased risk of medicine-related problems in elderly patients, the role of the community pharmacist should be examined.
Do community pharmacists contribute to an improved health-related quality of life in the elderly patient by supplying pharmaceutical services?
Do the elderly patients expect pharmaceutical services from their retail pharmacist?
2. Objective
The aim of this study was to determine the pharmaceutical services experiences of an elderly, urban population in relation to their expectations, in community pharmacy. The elderly are more likely to have multi-medicine and multi-disease conditions, and thus present a good population in which to examine the pharmaceutical services supplied by community pharmacy.
3. Ethical considerations
The study was approved by the Health Research Ethics Committee (HREC) of the Faculty of Health Sciences, North West University (NWU-00036-15-S1).
4. Research methods
A cross-sectional descriptive study was conducted. The researcher used a structured, researcher-designed questionnaire to conduct face-to-face interviews with the participants at their own dwellings.
The setting was an urban residence for the elderly with 242 residents. The management of this residence previously approached the researcher regarding healthcare concerns for their residents and granted permission for this study to be conducted. Participation was voluntary and written informed consent was obtained from all participants.
Participants had to comply with the following inclusion criteria:
• They had to be over 65 years of age. (In South Africa, the elderly are classified by the Older Person's Act (13 of 2006) as males of >65 years of age and females of >60 years of
age).
• They had to be ambulatory.
• They had to be able to administer own medicines. The resident nursing sister assisted in determining their ability to do so.
• They had to reside at specified residence for the duration of the study.
This specific population was questioned on their perception of pharmaceutical services as experienced in the past year. The questionnaire also determined their expectation of such services. One idea was addressed per question. The demographic data was obtained using closed-ended questions, with options of yes/no answers or stating a definite fact. The pharmaceutical services expectation and experience-questionnaire were structured using a four-point Likert scale. Pharmaceutical services, as indicated in the Pharmacy Act (53 of 1974 as amended in 1995), were used as guidelines in the development of the questionnaire. Participants were afforded an opportunity to raise questions regarding the study and/or regarding their health issues or medicines after the interview.
Validity and reliability in this study were ensured by using only one interviewer (Joubert & Ehrlich, 2012). The researcher was familiar with the language and culture of the participants, increasing the face validity of the study (Joubert & Ehrlich, 2012). The questionnaire was based on personal experiences of the study population over the past 12 months. Staff members of the Pharmacy Practice and Clinical Pharmacy departments of the School of Pharmacy at the North West University (NWU), Potchefstroom Campus, and the study leaders reviewed the questions and structure of the questionnaire to ensure it tested for required information (Maree, 2012). No pilot study was done, due to the sample size and time constraints of this study. The researcher also used questions adapted from those used in other studies in the field of pharmaceutical services and pharmaceutical care (Strand, Cipolle, Morley, & Frakes, 2004; Volume, Farris, Kassam, Cox, & Cave, 2001).
The data from the participants were collected during June 2015. Questions in the questionnaire focused on the following aspects: demographical profile of participants, chronic disease and medication profile of participants, preferences of participants relating to pharmacist and pharmacies, as well as participants' experiences and expectations of pharmaceutical services.
4.1. Statistical analysis
Data analysis was done with IBM SPSS Statistics for Windows, version 22.0 (IBM, 2013) in consultation with the Statistical Consultation Services of the NWU. Statistical significance was considered with a two-sided probability of p < 0.05. Practical significance of results was computed when the p-value was statistically significant (p < 0.05). Variables (age groups, gender, etc.) were expressed using descriptive statistics such as frequencies (n), percentage (%), means and standard deviations.
The two-sample t-test was used to compare the difference between the means of two groups. ANOVA was used for more than two groups. If a difference was indicated, a Tukey multiple comparison test was performed to determine which groups differed statistically significantly from one another. Cohen's d-value was used to determine the practical significance of the results (with d > 0.8 defined as a large effect with practical significance).
Chi-square tests were used to determine associations between proportions of two or more categorical variables. Cramer's V statistic was used to test the practical significance of this association (with Cramer's V > 0.5 defined as practically significant).
5. The evolution of pharmacy: medicine maker to medicine specialist?
Ancient writings make mention of dedicated healers who prepared remedies to cure ills. As civilisation developed, Greek, Roman, Chinese, Arab and Indian medicinal cultures merged, but they were always steeped in mysticism (Sonnedekker, 1976). It was only in the 19th century that the study of physiology, pharmacognosy, pharmacology and pharmaceutical chemistry brought scientific principles to the practice of pharmacy (Anderson, 2005). In the 1900s, industrialisation changed the face of pharmacy and the profession of pharmacy to that of medicine-trader as per physician prescription (Hepler & Strand, 1990). The role of pharmacists as healthcare professionals diminished, and they were viewed as shopkeepers that mainly compounded and distributed medicines.
In the 1980s, the abundance of prescribed medicines gave rise to an increased amount of adverse medicine reactions. The pharmacist was identified as the healthcare professional, competent to address the problem (Hepler & Strand, 1990). The pharmacist, with unique medicine therapyknowledge, should fulfil a clinical role: to provide individualised patient therapies and cooperate with other healthcare professionals and the patient to obtain positive healthcare outcomes (Al Shaqua & Zairi, 2001), as well as providing the traditional pharmaceutical support services. Pharmacists have the knowledge and skills to improve patients' health-related quality of life and they should take their place in the healthcare team (Wiedenmayer, Summers, Mackie, Gous, & Everard, 2006).
5.1. Pharmaceutical services in the community pharmacy setting in South Africa
The International Pharmaceutical Federation promotes pharmaceutical care, underpinned by the traditional support to the patient of dispensing, compounding, advice, counselling, supply of medical devices and supply of over-the-counter medications (FIP, 1998). In a message from the President of the Pharmaceutical Society of South Africa (Malan, 2015), pharmacists were encouraged to be the medicine experts and to use their unique skills to prevent, identify and resolve medicine-related problems, to recommend cost-effective therapy, and to counsel patients on medicine-therapy.
Most of the non-dispensing services offered in community pharmacy in South Africa are blood pressure monitoring, medicine monitoring, nutritional advice, blood glucose monitoring and infant care (Blignault, 2010). On average, 50% of a pharmacist's workday is devoted to dispensing, with 35% of the day spent on counselling patients regarding medicine and administration (Blignault, 2010).
Pharmacists are the primary gatekeepers to medicines in the community (Gous, 2011). The role of the pharmacist has further evolved from provider, dispenser, procurer and distributor of medicines to that of healthcare educator. Pharmacists now focus on the individual patient by providing the following: Counselling; medicine information; disease prevention; monitoring of medicine therapy; supply of pharmaceutical services; provision of pharmaceutical care and dispensing of medicine whether on prescription or over-the-counter (FIP, 1998; SAPC, 2010; Wiedenmayer et al., 2006).
The pharmacist should use the patient's need for medicine as a contact point to supply health education and pharmaceutical care (Wiedenmayer et al., 2006).
5.2. Pharmaceutical services in elderly populations
In 2009, the South African population included 7.8% of citizens over the age of 60 years, of whom 40% resided in Gauteng (Statistics South Africa, 2011). Of the persons aged 60-79 years, 51.8% suffered from at least one chronic condition (Phaswana-Mafuya et al., 2013; Statistics South Africa, 2011). The leading chronic diseases in South Africa are cardiovascular disease, chronic obstructive pulmonary disease, hypertension and diabetes mellitus (Steyn, Fourie, & Temple, 2006). Pharmaceutical care and the appropriate pharmaceutical services contribute to improved health literacy and the resultant effective use of medicines (Wooten, 2012). In 2010, South Africa had 24 registered pharmacists per 100 000 citizens. The public health sector services 85% of the population, where statistics show that there is one pharmacist per approximately 14 000 people (Smith, 2011). In private healthcare settings in South Africa, where the ratio is more realistic, pharmacist-patient and pharmacist-initiated patient interaction is still not common practice (Gray, Khan, & Sallet, 2002).
Thus the question of whether community pharmacists encourage patients, and particularly the more vulnerable elderly patients, to voice their questions and concerns over their medicine usage, can be asked.
6. Results and findings
The target population for this study was the ambulatory residents of a residence that housed 242 elderly pensioners, of which 67 (27.6%) participated in this study. Table 1 displays the demographics for the sample population.
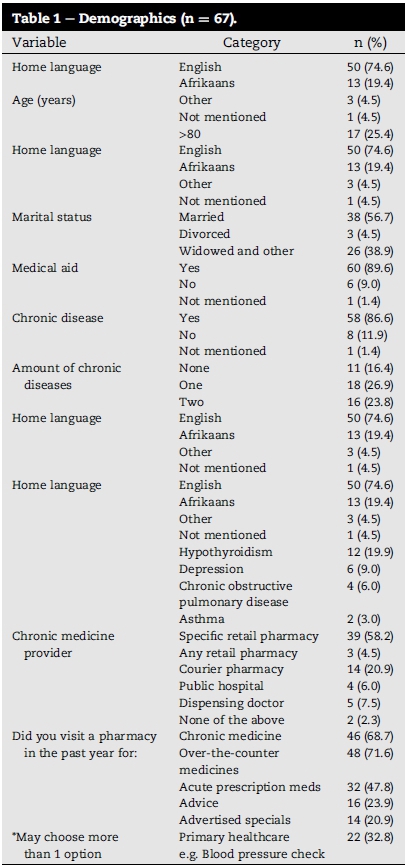
There were no chronic diseases reported by 11 (16.4%) of the participants. The other 56 (83.6%) participants reported five or less chronic diseases each. Only four (6.0%) participants reported five chronic diseases. Of the 56 participants that reported chronic conditions, 18 (26.9%) had a single chronic disease, 16 participants (23.8%) had two, while 15 (22.4%) had three chronic diseases (Table 1). The most prevalent chronic diseases were Hypertension 36 (53.7%), hypercholesteraemia 33 (49.35%), arthritis 20 (29.9%) and diabetes 14 (20.9%).
The participants were questioned about their demographic preferences for pharmacists/pharmacies (see Table 2).
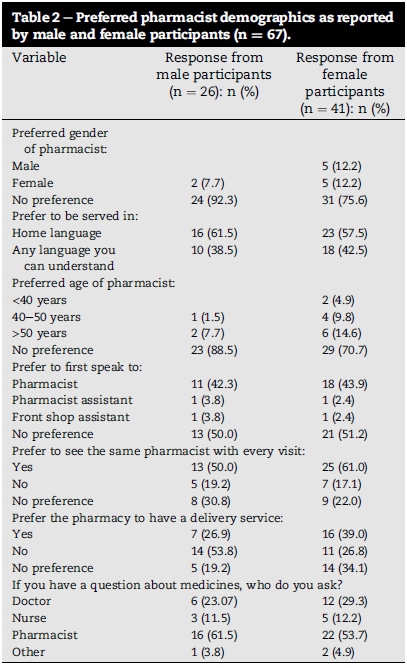
Participants had no specific preference in terms of pharmacy/ pharmacist demographics except that they would like to see the same pharmacist with every visit (male response 50.0% and female response 61.0%) and would prefer to be served in their home-language (male response 61.5% and female response 57.5%). The pharmacist was the first port-of-call for participants if they had a question regarding medicines (56.7%).
The participants were asked to report their experiences of health-related needs at community pharmacies and at other healthcare professionals (See Table 3). A comparison was made between the health-related services received at community pharmacies and those same services received at other healthcare professionals, be it clinic sisters, general practitioners, specialists or government hospitals.
Community pharmacists asked 10.4% of these patients if they were using any other medicines, and other healthcare professionals asked them 6.0% of the time. Questioning about existing chronic diseases revealed pharmacy with 6.0% and other healthcare professionals with 4.5%, while 6.0% of the participants reported that their pharmacists did discuss possible side effects of the medicines as opposed to 3.0% of their other healthcare professionals.
Community pharmacy met the expectations of this population, in terms of healthcare needs, far greater than what other healthcare professionals did. Statistically significant differences (p < 0.05) were found between the health-related services offered at community pharmacies and those offered at other healthcare professionals, in all aspects examined.
Table 4 shows the experience of pharmaceutical services in terms of pharmacist and pharmacy-related needs vs the expectation thereof, as reported by this specific population. There were practically (d > 0.08) significant differences between what the participants expected and what they experienced. There was an unmet expectation to speak to the pharmacist in a semi-private area (d = 0.76). The need to identify the pharmacist on duty (d = 0.55) and the need for seating space (d = 0.50) was not realised in community pharmacy. The participants expected the pharmacist to be able to answer their questions (d = 0.34) even when they did not need to purchase anything (d = 0.46). The expectation to reach the pharmacist telephonically was also not met (d = 0.18), albeit to a lesser extent.
Table 5 shows statistically and practically significant differences between the medicine-related experiences and expectations of the participants. They expected to receive information about the effect of other medicines on their chronic condition/medicines (d = 1.94). They expected questions regarding medicines left over from previous issues (d = 1.77) and whether they suffered from any other chronic conditions (d = 1.69). They were not always told how to take the medicine they received (d = 0.61), how to store the medicines (d = 1.45) and what the side effects could be (d = 1.51). They seldom received an explanation on what to do if they skipped a dose/taken an extra dose (d = 1.45). The participants were not questioned about possible allergies (d = 1.16). The purpose of the medicine, as issued at the time, was not explained to them (d = 1.07). They did not understand the terminology used (d = 0.34). The participants expected the community pharmacist to help them manage their medicines and conditions, but they did not experience this help (d = 1.13).
These participants had been, and would be willing to pay for healthcare services at the pharmacy. The difference between the current willingness to pay for services and the expectation to pay is statistically and practically significant (p = 0.784 and d = 0.03). The results are shown in Table 6.
The Pharmacy Act (SAPC, 2010a) makes provision for certain healthcare services for which pharmacists maycharge a fee (SAPC, 2010b). This was used as a guide to determine healthcare needs of the participants at a community pharmacy, and there were statistically (p < 0.001) and practically significant differences between the use of these services and their need thereof: Blood cholesterol monitoring (d = 0.91); blood glucose monitoring (d = 0.95); administration of prescribed injections (d = 0.84); peak flow measurement (d = 0.74) and blood pressure monitoring (d = 0.67). A lesser need for pharmacist-initiated therapy (d = 0.35) and urine analysis (d = 0.33) was indicated. Immunisation services (d = 0.37) and a call-out service (d = 0.58) are utilised, but no great need for these services was indicated. Liaison with healthcare professionals in chronic medicine authorisation (d = 0.64) and pharmacist assisted medicine management (d = 0.69) was not experienced by these participants. Most of the participants did regard the pharmacist as their partner in health (d = 0.13).
During the face-to-face interviews, participants had the opportunity to raise questions. There were 27 questions asked that were categorised as:
• Side effect related (29.6%)
• Medicine-use related (29.6%)
• Disease-related (25.9%)
• Pharmacy services-related (14.9%)
The demography of the population did not influence the type of question asked. Responses were compared for different age groups; being a medical aid member or not; the number of chronic conditions present at the time; preferred language and marital status. There were no statistically or practically significant differences or associations in these sub-groups.
7. Discussion
Health-related quality of life is defined by the World Health Organization as "a state of complete physical, mental and social well-being, not merely the absence of disease" and this includes the subjective measure of a "feeling of wellbeing" (WHO, 1997). Pharmacists have the responsibility not only to dispense medicines, but also to contribute to the improved health-related quality of life in the patient (Volume et al., 2001). The elderly have more chronic diseases than younger generations, and they therefore need pharmaceutical services to service their specific medicine-related needs (Mangoni & Jackson, 2004). In 2014, South Africa had 54 million citizens (Statistics South Africa, 2014), 3080 registered community pharmacists and 920 institutional pharmacists (SAPC, 2015). The public healthcare system is responsible for the health of 85% of the population (Mayosi et al., 2012), which means that private healthcare is only responsible for 15% of the population. The majority of the participants in this study (61.19%) procured chronic, acute and over-the-counter medicines from community pharmacies.
This study showed statistically significant differences (p < 0.05) between the participants' expectations and actual experiences in all the aspects of pharmaceutical services that were examined. Modig, Kristensson, Troein, Brorsson, and Midlöv (2012) found that a lack of information regarding medicines from their healthcare professional could cause anxiety in the elderly patient.
In Table 3, effect size shows statistically significant differences between healthcare needs at the pharmacy and other healthcare professionals (p < 0.05), which indicates that they more often understood the terminology that was used at the pharmacy, they were told what medicine they would receive and what the purpose of the medicine is. The pharmacist asked more often about existing chronic diseases or medicines they are currently taking, and they explained both the instructions and the storage conditions. This indicates that community pharmacists are playing a role in preventing medicine-medicine and disease-medicine interactions.
Table 4 shows the pharmacy and pharmacist-related experiences and expectations as reported by the study population. Pharmacy-related experiences include the layout of the pharmacy and the general appearance, identification and accessibility of pharmacy personnel. Statistically significant differences were found in all the aspects examined. There were no practically significant differences between their expectations and experiences. The participants indicated a need for a private/semi-private counselling area (d = 0.76), a desire to identify the pharmacist on duty with ease (d = 0.55) and expected sufficient seating while waiting to be served (d = 0.50). Effect size indicates that this corresponds with a study in Malaysia (Nagashekara, Sze-Nee, David, D'Souza, & Rathakrishnan, 2012), where 82% of the general population were adequately satisfied with pharmacy-related experiences.
In Table 5, the interaction between the patient and the pharmacist was examined and statistically significant differences between the medicine-related experiences and expectations of these participants were found in all the aspects examined. Effect size shows that they want to receive information about the effect of other medicines on their chronic condition/medicines (d = 1.94). They also expect to be asked about medicines left over from previous issues (d = 1.77), and whether they suffer from any other chronic conditions (d = 1.69). They expect to be asked about other medications they are taking (d = 1.57) and whether they had any allergies (d = 1.16). They are not told what medicine they receive (d = 0.83), or the purpose (d = 1.07) or storage conditions of the medicine (d = 1.45). The issue of possible side effects are not discussed (d = 1.51) and the participants receive no guidance on what to do if they take an accidental extra dose/skipped a dose (d = 1.51). There were, however, some practically significant associations between the expectations and experiences in community pharmacy. This population understands the terminology used (d = 0.34), they are told how to take the medicine they receive (d = 0.61) and they know who to ask if they have questions regarding medicines (d = 0.38). Kaae, Traulsen, and N0rgaard (2012) interviewed customers at retail pharmacies in Denmark and found that only 42.9% of them expected to be questioned when purchasing medicine. In Nigeria (Oparah & Kikanme, 2006), consumers were satisfied with their pharmacists' professional and counselling service but not satisfied with the provision of the other services in community pharmacy. This South African study indicates that the medicine-related expectations of this specific study population were not met and highlights an opportunity for the community pharmacist to explore new and existing services to enhance consumer health-related quality of life.
The healthcare-related experiences and expectations, as reported by the study population, are reflected in Table 6 and shows that there were statistically significant differences in most of the pharmacy healthcare-related needs. The only statistically significant association was their willingness to pay for healthcare services at the pharmacy (p = 0.201) and that they regard the pharmacist as their partner in health (p = 0.784). Cohen's d-value indicates practically significant associations between most of the healthcare services offered: Blood pressure monitoring (d = 0.67); Peak flow measurement (d = 0.74); immunisation services (d = 0.37); the need for a call-out service (d = 0.58); pharmacist-initiated therapy (d = 0.35); urine analysis (d = 0.33); liaison with other healthcare professionals (d = 0.64); medicine management (d = 0.69); the pharmacist as a partner in health (d = 0.13) and the participant being willing to pay for healthcare services (d = 0.03). This correlates with a study in Texas, USA (Xu, 2002), where elderly patients, using community pharmacy, showed a high rate of satisfaction with pharmaceutical services. In Australia (Peterson, Jackson, Hughes, Fitzmaurice, & Murphy, 2010) and in Oman (Jose, Al Shukili, & Jimmy, 2015), patients expected community pharmacy to offer healthcare services.
The pharmacist experiences several barriers in the supply of pharmaceutical services. Pharmacists are trained to provide pharmaceutical services, yet they are mainly remunerated on product sales rather than services (SAPC, 2010). In 2012, only 25% of the healthcare funders in South Africa considered the pharmacist as a valuable member of the healthcare professional team (Mayosi et al., 2012).
The root of the discrepancies between patient experience and expectations for a pharmacist may well be pharmacists themselves. New attitudes, confidence in their abilities and the understanding of their role in patient care can restore the professional image of the pharmacist in the eyes of the community and motivate the pharmacist to be an active member of the healthcare team (Shu Chuen Li, 2003).
8. Conclusions, limitations & recommendations for future research
Pharmacy, and specifically community pharmacy, is a dynamic profession. It has developed from a medicine-selling, compounding, advisory profession to an interactive, individual-patient focused service industry. The community pharmacist should focus on the health-related quality of life of the individual patient (Kelly, 2012). Pharmacists need to identify the immediate healthcare needs of their specific community, with specific reference to vulnerable populations like the elderly. The pharmacist should be able to address these needs and become the go-to healthcare professional.
This study population was a high-income elderly population. The study can therefore not be generalised to the general elderly population in South Africa. The study cannot be generalised across all the language groups as the participants in this population could all speak English fluently, even though some spoke Afrikaans or Portuguese as a home language. There was no need for a translator while conducting this study. The population included only ambulatory participants, which prevents generalisation across the frail and handicapped elderly. The ambulatory patients could relay their personal experiences and expectations for the past year. The researcher depended on the perception of the participant with respect to their experiences and expectations of pharmaceutical care, which may have introduced recall bias.
Further studies amongst all language groups will be more generalisable. Other urban, independent and/or inner city old-age home studies will provide an interesting comparison in terms of pharmaceutical care needs and expectations. The research can also be extended to elderly, living independently in a rural environment.
This study should serve as a guideline for community pharmacists to enhance their services to patients. If patient expectations are met, customer satisfaction and retention will increase.
REFERENCES
Al Shaqua, M., & Zairi, M. (2001). Pharmaceutical care management: A modern approach to providing seamless and integrated health care. International Journal of Health Care Quality Assurance, 14, 282-301. [ Links ]
Anderson, S. (Ed.). (2005). Making medicines: A brief history of pharmacy and pharmaceuticals. Grayslake, Illinois: Pharmaceutical Press. [ Links ]
Benjamin, R. (2010). Multiple chronic conditions: A public health challenge. Public Health Report, 125(5), 626-627. [ Links ]
Blignault, S. M. (2010). Audit ofcommunity pharmacy activities (PhD thesis). Port Elizabeth: Nelson Mandela Metropolitan University. [ Links ]
FIP (Fédération Internationale Pharmaceutique). (1998). FIP statement ofpolicy: The role ofthe pharmacist in pharmacovigilance. http://fip.org/www/uploads/database_file.php?id=273&table_id=. Date of access: 3 October 2015. [ Links ]
Gous, A. (2011). Remuneration for clinical services. In Presentation at the South African society ofclinical pharmacy conference, Pretoria, RSA, 3 June. http://www.sasocp.co.za/downloads/conference/D2-P9-%20Remuneration%20for%20clinical%20services.pdf. Date of access: 15 August 2015. [ Links ]
Gray, A. L., Khan, R., & Sallet, J. P. (2002). Community-level model of pharmaceutical care: Pointers from South Africa. International Pharmaceutical Federation World Congress, 62, 111. [ Links ]
Hepler, C. D., & Strand, L. M. (1990). Opportunities and responsibilities in pharmaceutical care. American Journal of Hospital Pharmacy, 47, 533-543. [ Links ]
IBM. (2013). IBM SPSS statistics for Windows, version 22.0. Armonk, New York: IBM. [ Links ]
Jacobzone, S., Cambois, E., & Robine, J. M. (2001). Is the health of older persons in OECD countries improving fast enough to compensate for population ageing? OECD Economic Studies, 30(151). http://78.41.128.130/dataoecd/31/20/2732545.pdf. Date of access: 14 August 2014. [ Links ]
Jose, J., Al Shukili, M. N., & Jimmy, B. (2015). Public's perception and satisfaction on the roles and services provided by pharmacists - cross sectional survey in Sultanate of Oman. Saudi Pharmaceutical Journal, 23(6), 635-641. [ Links ]
Joubert, G., & Ehrlich, R. (2012). Epidemiology, a research manual for South Africa. Cape Town: Oxford. [ Links ]
Kaae, S., Traulsen, J. M., & N0rgaard, L. S. (2012). Customer interest in and experience with various types of pharmacy counselling - a qualitative study. Health Expectations, 17(6), 852-862. [ Links ]
Kelly, W. N. (2012). Pharmacy: What it is and how it works. Boca Raton, FL: CRC Press. [ Links ]
Malan, S. (2015). It's all about doing the right thing, in the right way, at the right time and for the right reason. South African Pharmaceutical Journal, 82(6), 6. [ Links ]
Mangoni, A. A., & Jackson, S. H. D. (2004). Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications. British Journal of Clinical Pharmacology, 57(1), 6-14. [ Links ]
Maree, K. (Ed.). (2012). First steps in research. Pretoria: Van Schaik. [ Links ]
Mayosi, B. M., Lawn, J. E., Van Niekerk, A., Bradshaw, D., Abdool Karim, S. S., & Coovadia, H. M. (2012). Health in South Africa: Changes and challenges since 2009. The Lancet, 380(9858), 2029-2043. [ Links ]
McGann, E. (2012). Pharmacists' role critical to patient safety. Medscape Medical News. http://www.medscape.com/viewarticle/756506. Date of access: 6 January 2012. [ Links ]
Modig, S., Kristensson, J., Troein, M., Brorsson, A., & Midlov, P. (2012). Frail elderly patients' experiences of information on medication. A qualitative study. BMC Geriatrics, 22(12), 46-48. [ Links ]
Nagashekara, M., Sze-Nee, N., David, M., D'Souza, U. J. A., & Rathakrishnan, B. (2012). Patient satisfaction in general, intervention and cognitive services among retail pharmacies in Kota Kinabalu, Malaysia. International Research Journal of Pharmacy, 3(8), 141-144. [ Links ]
Nobili, A., Garanttini, S., & Mannucci, P. M. (2011). Multiple diseases and polypharmacy in the elderly: Challenges for the internist of the third millennium. Journal of Comorbidity, 1,28-44. [ Links ]
Oakley, N. (2015). Need health advice? Why you should make your pharmacy your first port of call before trying a GP. Daily Record and Sunday Mail. http://www.dailyrecord.co.uk/special-features/need-health-advice-you-should-6394329. Date ofaccess: 25 September 2015. [ Links ]
Oparah, A. C., & Kikanme, L. C. (2006). Consumer satisfaction with community pharmacies in Warri, Nigeria. Research in Social & Administrative Pharmacy, 2(4), 499-511. [ Links ]
Peterson, G., Jackson, S., Hughes, J., Fitzmaurice, K., & Murphy, L. (2010). Public perceptions of the role of Australian pharmacists in cardiovascular disease. Journal of Clinical Pharmacy and Therapeutics, 35(6), 671-677. [ Links ]
Phaswana-Mafuya, N., Peltzer, K., Chirinda, W., Musekiwa, A., Kose, Z., Hoosain, E., et al. (2013). Self-reported prevalence of chronic non-communicable diseases and associated factors among older adults in South Africa. Global Health Action, 6. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3779355/. Date of access: 4 June 2014. [ Links ]
SAPC (South African Pharmacy Council). (2010). Good pharmacy practice manual. Official website http://www.pharmcouncil.co.za/. Date of access: 16 June 2015. [ Links ]
SAPC (South African Pharmacy Council). (2010a). Rules regulating to the services for which pharmacist may levy a fee and guidelines for levying such a fee or fees. Official website http://www.mm3admin.co.za/documents/docmanager/0C43CA52-121E-4F58-B8F6-81F656F2FD17/00010779.pdf. Date of access: 16 June 2015. [ Links ]
SAPC (South African Pharmacy Council). (2010b). Board notice no 193 of 2010, rules relating to the services for which a pharmacist may levy a fee and guidelines for levying such a fee or fees. http://www.mm3admin.co.za/documents/docmanager/0C43CA52-121E-4F58-B8F6-81F656F2FD17Z00010779.pdf Accessed 12 October 2016. [ Links ]
SAPC (South African Pharmacy Council). (2015). Official website. http://www.pharmcouncil.co.za/. Date of access: 16 June 2015. [ Links ]
Shu Chuen Li, L. (2003). An overview of community pharmacist interventions: Assessing cost-effectiveness and patients' willingness to pay. Disease Management and Health Outcomes, 11,95-106. [ Links ]
Smith, C. (Ed.). (2011). Shortage ofpharmacists a global problem. Medical chronicle: The doctors' newspaper, June 2011:3. [ Links ]
Sonnedekker, G. (Ed.). (1976). Kremer and Urdang's history of pharmacy (4th ed.). Madison, WI: American Institute of the History of Pharmacy. [ Links ]
South Africa. (1995). Pharmacy Act 53 of 1974, as amended by section 4 of Act 6 of 1995. [ Links ]
South Africa. (2006). Older persons' Act 13 of 2006. [ Links ]
Statistics South Africa.(2011). http://beta2.statssa.gov.za/?page_id=1021&id=city-of-johannesburg-municipality. Date of access: 13 March 2014. [ Links ]
Statistics South Africa. (2014). Midyear population estimates. http://www.statssa.gov.za/publications/P0302/P03022014.pdf. Date of access: 15 February 2015. [ Links ]
Steyn, K., Fourie, J., & Temple, N. (Eds.). (2006). Chronic diseases of lifestyle in South Africa: 1995-2005. Cape Town: South African Medical Research Council. [ Links ]
Strand, L. M., Cipolle, R. J., Morley, P. C., & Frakes, M. J. (2004). The impact of pharmaceutical care practice on the practitioner and the patient in the ambulatory practice setting: Twenty- five years of experience. Current Pharmaceutical Design, 10(31), 3987-4001. [ Links ]
Vaupel, J. W. (2010). Biodemography of human ageing. Nature, 464(7288), 536-542. [ Links ]
Volume, C. I., Farris, K. B., Kassam, R., Cox, C. E., & Cave, A. (2001). Pharmaceutical care research and education project: Patient outcomes. Journal of the American pharmaceutical Association, 41(3), 411-420. [ Links ]
WHO (World Health Organization). (1997). Measuring quality of life. The World Health Organization quality of life instruments (the WHOQOL-100 and the WHOQOL-BREF). http://www.who.int/mental_health/media/68.pdf. Date of access: 3 October 2015. [ Links ]
Wiedenmayer, K., Summers, R. S., Mackie, C. A., Gous, A. G. S., & Everard, M. (2006). Developing pharmacy practice: A focus on patient care. Geneva: World Health Organization. http://www.fip.org/files/fip/publications/DevelopingPharmacyPractice/DevelopingPharmacyPracticeEN.pdf. Date of access: 15 December 2014. [ Links ]
Wooten, J. M. (2012). Pharmacotherapy considerations in elderly adults. Southern Medical Journal, 105(8), 437-445. [ Links ]
Xu, K. T. (2002). Choice of overall satisfaction with pharmacies among a community-dwelling elderly population. Medical Care, 40(12), 1283-1293. [ Links ]
Received 29 April 2016
Accepted 8 December 2016
* Corresponding author. Private bag X6001, Potchefstroom Campus, North West University, Potchefstroom, 2520, South Africa. Fax: +27 18 299 4303.
E-mail address: Irma.Kotze@nwu.ac.za (I. Kotze). Peer review under responsibility of Johannesburg University.














