Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
Health SA Gesondheid (Online)
versão On-line ISSN 2071-9736
versão impressa ISSN 1025-9848
Health SA Gesondheid (Online) vol.22 Cape Town 2017
http://dx.doi.org/10.1016/j.hsag.2017.01.001
FULL LENGTH ARTICLE
Reported exposure to trauma among adult patients referred for psychological services at the Free State Psychiatric Complex, Bloemfontein
Laurisa van ZylI,; Carla NelI; Martie du ToitI; Gina JoubertII
IDepartment of Psychiatry, Faculty of Health Sciences, University of the Free State, PO Box 339, Bloemfontein, 9300, South Africa
IIDepartment of Biostatistics, Faculty of Health Sciences, University of the Free State, PO Box 339, Bloemfontein, 9300, South Africa
ABSTRACT
BACKGROUND: Information regarding lifetime exposure to potentially traumatic events is critical in the management of various psychiatric disorders. Recent South African research suggests high levels of trauma exposure in the general population, however, the prevalence and type of potentially traumatic events among tertiary psychiatric patients are unknown
OBJECTIVE: The study aimed to explore and describe the extent and nature of reported potentially traumatic events and associated variables in adult patients referred for psychological services at the Free State Psychiatric Complex (FSPC), Bloemfontein.
METHODS: In this cross-sectional study, demographic information, diagnostic morbidity and co-morbidity, and presence and type of reported trauma exposure reported by patients during the initial assessment were obtained from files of adult patients seen during a one-year period (2010) at the out-patient unit and the in-patient affective ward at the FSPC. Data were captured on data record forms by the researchers and analysed by means of descriptive statistics, univariate analysis and logistic regression (SAS version 9.1)
RESULTS: Of the 192 adults (71.9% White and 67.2% female) referred for psychological services, 75.5% were diagnosed with mood disorders, 17.2% with anxiety disorders, 22.4% with substance-related disorders and 20.9% with cluster B personality disorders or traits. A total of 145 (75.5%) reported past trauma exposure. The most frequently reported types of trauma exposure were traumatic death/injury of a loved one (37.0%), physical assault (24.5%), witnessed/threatened violence (19.3%), and sexual assault (17.7%). Women were more likely to have been exposed to trauma than men (OR 4.02, 95% CI 1.87-8.62), in particular to traumatic death of a loved one (OR 3.13), physical assault (OR 4.08), or sexual assault (OR 5.43).
CONCLUSIONS: The findings of this study contribute to current data regarding the prevalence of exposure to trauma and its possible association with mental illness. The importance of comprehensive trauma exposure screening in routine psychiatric interviewing practices is highlighted.
Keywords: Trauma exposure, Mental illness, Screening ,Post-traumatic stress disorder
1. Introduction
1.1. Background
South African society is faced with exceedingly high rates of interpersonal violence, with age-standardised mortality rates at seven times the global rate (Norman, Matzopoulos, Groenewald, & Bradshaw, 2007). South African research suggests high levels of trauma exposure, with a lifetime exposure to at least one potentially traumatic event (PTE) reported for 73.8% of the general population (Atwoli et al., 2013). An event is considered to be a PTE if it is characterised by the experience, witnessing, or confrontation with actual or threatened death, serious injury, or sexual violence (American Psychiatric Association, 2000; 2013). By analysing the South African Stress and Health Study, Atwoli et al. (2013) found that the unexpected death of a loved one and witnessing trauma occurring to others were the most common PTEs reported by a general population sample. However, the prevalence and type of PTEs among tertiary psychiatric patients are unknown.
Not only is the presence of previous trauma exposure relevant to clinical practice, but also the nature of the PTE. Different traumatic stressors have been associated with different response patterns; post-traumatic stress disorder (PTSD), for example, is diagnosed ten times more frequently following rape than after experiencing natural disaster (Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Kopel & Friedman, 1997). Williams et al. (2007) have also emphasised the importance of considering traumatic events in the context of other traumas, taking into account the cumulative effect of trauma exposure and the graded relationship between multiple traumatic events and distress. This is especially relevant in the South African setting, where the average person with a history of trauma exposure experienced 4.3 of such occurrences on average (Atwoli et al., 2013). Demographic variables may further influence both the degree of exposure to PTEs as well as the person's reaction to such events. It has been suggested that women not only have a greater risk of exposure to specific kinds of PTEs, such as sexual assault and childhood sexual abuse, but also have a greater risk of developing PTSD when exposed to such traumatic events (Tolin & Foa, 2006).
Apart from PTSD (a well-documented consequence of trauma exposure), previous trauma exposure has also been linked to an increased vulnerability to other forms of psy-chopathology, including depression, social anxiety, substance abuse, dissociative symptoms, personality disorders, aggressive behaviour, sexual dysfunction, self-mutilation and suicidal tendencies, as well as problems with self-esteem, parenting and an increased risk for later victimization (Allen & Lauterbach, 2007; Bandelow et al., 2004; Bedard-Gilligan et al., 2015; Bolton et al., 2004; Callahan, Price, & Hilsenroth, 2003; Fichter, Goldfeder, Conti, Rooney, & Demaria, 2011; Ford & Smith, 2008; Liebenberg & Papaikonomou, 2010; Munjiza, Law, & Crawford, 2014; Pine, Costello, & Masten, 2005; Seedat, Stein, & Carey, 2005; Stovall-McClough & Cloitre, 2006; Trickey & Black, 2000; Wolf, Reinhard, Cozolino, Caldwell, & Asamen, 2009). In a study conducted by Subramaney (2006) at a South African trauma clinic, it was found that other psychiatric disorders, in particular major depressive disorder, were more frequently diagnosed among patients reporting traumatic stress than PTSD.
In routine clinical practice, screening for past exposure to PTEs is mostly done during the completion of the semi-structured psychiatric intake interview. Other methods of assessment may include questionnaires such as the Traumatic Life Events Questionnaire (TLEQ) (Kubany et al., 2002), but these are not routinely used. Clinical practice, therefore, may potentially lead to the underdiagnosis of PTSD, and prevent appropriate management and assessment of outcomes (Mkize, 2008). Adequate screening for all forms of psychopa-thology, including PTSD, may be hindered by a high clinic workload, limitations placed on time for consultations, and working in a cross-cultural setting (Carey, Stein, Zungu-Dirwayi, & Seedat, 2003). The underdiagnosis of PTSD has been observed in an in-patient tertiary psychiatric setting in South Africa, where almost half of comorbid PTSD cases have been missed with standard assessments (Van Zyl, Oosthuizen, & Seedat, 2008). The absence of a thorough assessment into past trauma exposure may be due to an alarming trend in the training of mental health practitioners. McFarlane and Van Der Kolk (2007) warned that the study of trauma exposure and its role in the development of psycho-pathology is at risk of becoming marginalised. According to them, trauma-related disorders receive scant attention during the training of medical students and psychiatric residents. They comment that "... the need to ignore the reality of trauma in people's lives also pervades medical school departments of psychiatry, where the response to increasing levels of traumatisation in society has generally been to ignore it".
It is clear that trauma exposure is important in psychiatric settings, but currently no study has explored the extent and nature of exposure to PTEs or the variables associated with such exposure in psychiatric patient samples in South Africa.
1.2. Aim of study
This study investigated the extent of trauma exposure as reported by adult patients across all diagnostic categories referred for psychological services at the Free State Psychiatric Complex (FSPC), in Bloemfontein. This study, on a small scale, heeds the call by Williams et al. (2007) for a direct assessment of multiple traumas to elucidate the mental health burden of trauma exposure in South Africa. In order to meet these aims, the researchers posed the following research questions:
• What is the frequency with which the population report a history of trauma exposure?
• What is the reported frequency of different types of trauma exposure?
• What are the associations of diagnostic and demographic variables with the rate and nature of reported trauma exposure?
2. Research method and design
A cross-sectional study design was used. The study was conducted at the in-patient affective ward and adult out-patient unit at the FSPC, a specialist psychiatric facility in an urban setting where tertiary level care is provided. Routine diagnostic procedure at the study sites entails that all preliminary diagnoses made after the psychiatric intake are subject to review during multidisciplinary team rounds by consultant clinical psychologists and psychiatrists. These study sites were selected as they form part of the service delivery areas of the researchers, and are of the few facilities that provide mental healthcare users with psychotherapeutic services in the province. All 192 files of adult mental healthcare users who were referred by the multidisciplinary team and received psychological services during a one-year period (January 2010 to December 2010) at the FSPC were included. This included patients who had been referred by previous therapists at the units for continuation of psychological services.
2.1. Data collection
Demographic variables, diagnostic morbidity and co-morbidity, as well as presence and type of trauma exposure spontaneously reported by patients during the psychiatric intake interview were obtained from clinical files. Data collection took place during February and March 2011 at the study sites. The three principal researchers recorded this information on the data record forms. For the purpose of this study, the researchers designed the data record form to reflect an adapted classification of PTEs derived from the TLEQ (Kubany et al., 2002); a 23-item self-report measure of 22 types of potentially traumatic events, such as natural disasters, violent crime, and exposure to warfare. The researchers condensed the 22 items of the TLEQ to elicit 16 different types of trauma by grouping related individual items, such as Sexual abuse before age 13 by someone at least 5 years older, Sexual abuse before age 13 by someone close in age, and Sexual abuse during adolescence to the single category of Childhood sexual assault. The DSM-IV-TR was still in use during the time of data collection, and was therefore reflected in the data record form's diagnostic classification.
2.2. Pilot study
A pilot study (a standard practice in the Faculty of Health Sciences, University of the Free State), which included five patient files randomly selected, was conducted by the researchers during the first week in February 2011, after permission was obtained from the relevant Ethics Committees, for the purpose of verifying the design of the data record forms. No changes to the form were needed, and data from the pilot study were included in the research project.
2.3. Data analysis
Statistical analysis was done by the Department of Biostatis-tics, Faculty of Health Sciences, University of the Free State. Results were summarised by frequencies and percentages. To determine the association between demographic variables (age, gender and education level) and exposure to trauma and types of trauma exposure, logistic regression was performed utilising SAS version 9.1. From this analysis, odds ratios (ORs) with 95% confidence intervals (CIs) were obtained. Similarly, logistic regression was performed to assess the association between trauma exposure and psychiatric diagnoses (adjusted for the demographic variables).
2.4. Ethical considerations
The protocol was approved by the Ethics Committee of the Faculty of Health Sciences, University of the Free State (ECUFS 185/2010). Permission to conduct the study was obtained from the FSPC Clinical Ethics and Research Committee. All information was treated confidentially, clinical records were kept on site, and collected information was used only for the purpose of research. The database did not contain any identifying information of the participants.
3. Results
3.1. Demographic data
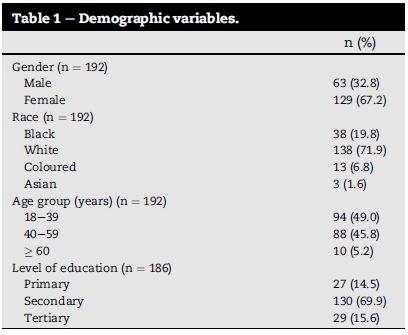
Of the 192 participants, most were White (71.9%) and female (67.2%) patients. Participants were mainly in the early adulthood and the middle adulthood age group (49.0% and 45.8%, respectively). Nearly 70 percent (69.9%) of participants had a secondary level of education (Table 1).
3.2. Diagnostic morbidity
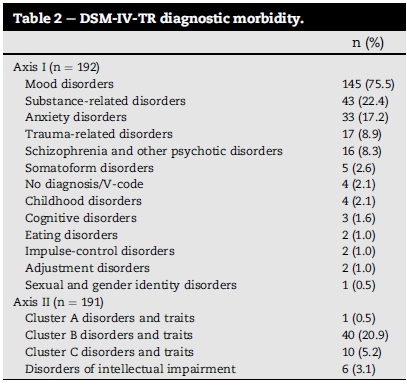
Data revealed that multiple psychiatric diagnoses were made for 108 (56.3%) participants. The majority of these participants (n = 73; 67.6%) had two diagnoses on record, 29 (26.8%) had three diagnoses and six (5.6%) had four or more. Post-traumatic stress disorder and acute stress disorder were diagnosed in 8.9% (n = 17). The most prevalent diagnoses were mood disorders (75.5%), substance-related disorders (22.4%), cluster B personality disorders or traits (20.9%), and anxiety disorders (17.2%) (Table 2).
3.3. Reported trauma exposure
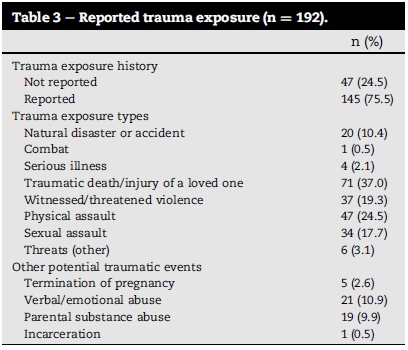
A total of 145 (75.5%) participants reported past trauma exposure during their initial assessment (Table 3). Of these, 61 (42.1%) reported exposure to a single trauma type and 84 (57.9%) exposure to multiple types of trauma. The most frequently reported types of trauma exposure were traumatic death/injury of a loved one (37.0%), physical assault (24.5%), witnessed/threatened violence (19.3%), and sexual assault (17.7%). The median number of trauma types for the total number of participants was one.
3.4. Logistic regression of variables
Logistic regression of demographic variables showed that women were more likely to report trauma exposure than men (OR 4.02; 95% CI 1.87-8.62); in particular traumatic, death/ injury of a loved one (OR 3.13; 95% CI 1.40-6.99), physical assault (OR 4.08; 95% CI 1.49-11.24), and sexual assault (OR 5.43; 95% CI 1.46-20.41). Participants with a primary education were more likely to have been exposed to sexual assault (OR 5.43; 95% CI 1.46-20.41) than participants with a tertiary education (OR 11.90; 95% CI 1.30-108.68).
The only other demographic association found with a specific trauma exposure was that participants in the age group 60 and older were more likely to have experienced traumatic death or injury of a loved one than patients in the age group 18-39 years (OR 11.24; 95% CI 1.92-66.67). The only significant association between trauma exposure and psychiatric diagnosis was for mood disorders (OR 2.79; 95% CI 1.19-6.53).
4. Discussion
The results of this study show that the majority of adult psychiatric patients referred for psychological services at the FSPC during the study period were white women. Most of the participants were under the age of 60 years and had completed secondary education. More than half of the group had multiple psychiatric disorders on record. The group presented with predominantly mood disorders, and the presence of diagnostic morbidities and co-morbidities of anxiety, personality pathology (cluster B disorders or traits) as well as substance-related disorders was also observed.
A high incidence of reported lifetime trauma exposure among psychiatric patients were seen, which correlates with findings at other South African study sites (Williams et al., 2007), and general population estimates (Atwoli et al., 2013). The nature of trauma exposure most frequently involved the traumatic death or injury of a loved one (37.0%), which correlates with the population-based exposure of 39.2% to this PTE (Atwoli et al., 2013). Other frequently reported PTEs included exposure to physical assault, witnessed/threatened violence and sexual assault. Multiple trauma exposure was found for 43.8% of the total number of study participants. This correlates with findings of Williams et al. (2007) noting that 55.6% of an South African sample reported multiple traumatic events.
Gender was a significant demographic variable relevant to trauma exposure, as women were more vulnerable than men to assault (sexual and physical) as well as traumatic grief. This is in contrast with findings by Carey et al. (2003) which reflected similar rates of exposure for both genders. Our results regarding sexual assault as a PTE reported more frequently by women correlate with internationally observed trends and local research (Carey et al., 2003; Tolin & Foa, 2006). The greater vulnerability of women to experience physical assault is, however, in contrast with the findings of a 25-year research review (Tolin & Foa, 2006). Results from a retrospective study in Brazil among female rape victims found that lower levels of education was associated with an increased risk for sexual assault (Souto, Araujo, Xavier, & Cavalcanti, 2015). Our study also showed that patients with primary education were more likely to be sexually assaulted than those with tertiary education.
The only diagnostic association with trauma exposure was found for mood disorders, reflecting the trend observed by other local researchers regarding the link between trauma exposure and non-trauma related psychiatric diagnoses, in particular unipolar depression (Subramaney, 2006; Van Zyl et al., 2008). Post-traumatic stress disorder and acute stress disorder were diagnosed in 8.9% of participants, which is higher than the South African lifetime prevalence of 2.3% in the general population (Atwoli et al., 2013). However, PTSD rates of 10.8% in the general population have also been observed (Topper, Van Rooyen, Grobler, Van Rooyen, & Andersson, 2015). Furthermore, PTSD rates of 22% among patients at a psychiatric out-patient clinic in Kwazulu-Natal have been suggested by Mkize (2008). The findings of this study may reflect the potential underdiagnosing of PTSD in a psychiatric setting where the trauma exposure did not necessarily form part of the presenting problem, as suggested by Mkize (2008). This may be due to the absence of traumasensitive questions during the standard psychiatric intake interview used at the study sites. This reflects the trend observed by the researchers in clinical practice that the diagnostic co-morbidities of PTSD often precipitate help-seeking behaviour and remain the only focus of clinical attention.
4.1. Study limitations
A limitation of the study is the lack of generalisability of the findings to other psychiatric settings due to the demographic profile of the participants. Due to the frequent exclusion of comprehensive assessment of trauma exposure from routine clinical practice at the FSPC, data in this study relied solely on the traumatic incidents reported voluntarily by mental healthcare users during their initial assessment, as the routine semi-structured psychiatric interview mainly elicits personal history and current mental status, which do not include trauma specific questions. This poses the potential problem: the reported exposure to traumatic events may represent an under-reporting of such events, as the mental healthcare practitioners may have failed to thoroughly explore the patient's trauma exposure history. Similarly, the participants were not re-diagnosed during the course of this study, which limits the study's ability to illuminate the potential issue of PTSD diagnosis in this population.
Future studies are needed to focus on the presence of PTSD symptomatology in the psychiatric population not presenting with direct trauma-related pathology. Furthermore, patients could have withheld such information upon questioning. This study may, therefore, illuminate potential problems regarding the possible current underestimation of past exposure to potential traumatic events.
5. Conclusion and recommendations
The findings of this study serve to enhance the current understanding of factors associated with rates and nature of trauma exposure in South African psychiatric patients in an urban tertiary setting. The high morbidity of mood, anxiety and substance-related disorders in this study population necessitates further inquiry regarding the spectrum of psychiatric sequelae of trauma exposure apart from trauma-related disorders.
The study highlights implications for the effective management of patients who may have been exposed to potentially traumatic incidents. Results from this study suggest a need for the incorporation of a specific focus on the assessment of trauma exposure. Special care needs to be taken in a psychiatric setting to obtain a clear and comprehensive assessment of past exposure to potentially traumatic events. Such an assessment should take into account the possibility that the association found between gender and PTE exposures in this study could have been related to under-reporting of trauma exposure by men. The psychiatric intake interview format may need to be adapted to include a specific set of questions regarding past exposure to previous potentially traumatic events, and to take into account the potential impact that the chronicity of PTSD may have on the clinical presentation of adult out-patient populations. Clinical practice may further benefit from the routine administration of screening tools, such as the TLEQ (Kubany et al., 2002).
Follow-up studies may focus on comparing the impact of the use of such structured assessment approaches on the phenomenology of trauma exposure as currently documented in clinical records.
Acknowledgement
Ms T. Mulder, Medical Editor, School of Medicine, University of the Free State, for technical and editorial preparation of the manuscript.
REFERENCES
Allen, B., & Lauterbach, D. (2007). Personality characteristics of adult survivors of childhood trauma. Journal of Traumatic Stress, 20(4), 587-595. http://dx.doi.org/10.1002/jts.20195. [ Links ]
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev). Washington, DC: APA. [ Links ]
American Psychiatric Association. (2013). Diagnostic and statistical manual ofmental disorders (5th ed.). Washington, DC: APA. [ Links ]
Atwoli, L., Stein, D. J., Williams, D. R., Mclaughlin, K. A., Petukhova, M., Kessler, R. C., et al. (2013). Trauma and posttraumatic stress disorder in South Africa: Analysis from the South African stress and health study. BMC Psychiatry, 13, 1-12. http://dx.doi.org/10.1186/1471-244X-13-182. [ Links ]
Bandelow, B., Charimo Torrente, A., Wedekind, D., Broocks, A., Hajak, G., & Rüther, E. (2004). Early traumatic life events, parental rearing styles, family history of mental disorders, and birth risk factors in patients with social anxiety disorder. European Archives of Psychiatry and Clinical Neuroscience, 254(6), 397-405. http://dx.doi.org/10.1007/s00406-004-0521-2. [ Links ]
Bedard-Gilligan, M., Duax Jakob, J. M., Doane, L. S., Jaeger, J., Eftekhari, A., Feeny, N., et al. (2015). An investigation of depression, trauma history, and symptom severity in individuals enrolled in a treatment trial for chronic PTSD. Journal of Clinical Psychology, 71(7), 725-740. http://dx.doi.org/10.1002/jclp.22163. [ Links ]
Bolton, D., Hill, J., O'Ryan, D., Udwin, O., Boyle, S., & Yule, W. (2004). Long-term effects of psychological trauma on psychosocial functioning. Journal of Child Psychology and Psychiatry, 45(5), 1007-1014. http://dx.doi.org/10.1111/j.1469-7610.2004.t01-1-00292.x. [ Links ]
Callahan, K. L., Price, J. L., & Hilsenroth, M.J. (2003). Psychological assessment of adult survivors of childhood sexual abuse within a naturalistic clinical sample. Journal of Personality Assessment, 80(2), 173-184. http://dx.doi.org/10.1207/S15327752JPA8002_06. [ Links ]
Carey, P. D., Stein, D. J., Zungu-Dirwayi, N., & Seedat, S. (2003). Trauma and posttraumtic stress disorder in an urban Xhosa primary care population: Prevalence, comorbidity, and service use patterns. Journal of Nervous and Mental Disease, 191 (4), 230-236. http://dx.doi.org/10.1097/01.NMD.0000061143.66146.A8. [ Links ]
Fichter, C., Goldfeder, C., Conti, M., Rooney, E., & Demaria, T. (2011). Clinical exposure with traumatized populations and the assessment of trauma during clinical practice. In Poster presented at the annual convention of the American Psychological Association. Washington, DC. Abstract retrieved from EBSCOHost. [ Links ]
Ford, J. D., & Smith, S. F. (2008). Complex posttraumatic stress disorder in trauma-exposed adults receiving public sector outpatient substance abuse disorder treatment. Addiction Research & Theory, 16(2), 193-203. http://dx.doi.org/10.1080/16066350701615078. [ Links ]
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., & Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry, 52(12), 1048-1060. http://dx.doi.org/10.1001/archpsyc.1995.03950240066012. [ Links ]
Kopel, H., & Friedman, M. (1997). Posttraumatic symptoms in South African police exposed to violence. Journal of Traumatic Stress, 10(2), 307-317. http://dx.doi.org/10.1002/jts.2490100211. [ Links ]
Kubany, E. S., Haynes, S. N., Leisen, M. B., Owens, J. A., Kaplan, A. S., Watson, S. B., et al. (2002). Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The traumatic life events questionnaire. Psychological Assessment, 12(2), 210-224. http://dx.doi.org/10.1037/1040-3590.12.2.210. [ Links ]
Liebenberg, H., & Papaikonomou, M. (2010). "Complex trauma": Reflections on the effect of early childhood abuse among a small adult group of bariatric patients. South African Journal of Psychology, 40(3), 327-337. http://dx.doi.org/10.1177/008124631004000311. [ Links ]
McFarlane, A. C., & Van Der Kolk, B. A. (2007). Trauma and its challenge to society. In B. A. Van der Kolk, A. C. McFarlane, & L. Weisaeth (Eds.), Traumatic stress: The effects ofoverwhelming experience on mind, body, and society (pp. 24-46). New York: Guilford Press. [ Links ]
Mkize, D. L. (2008). Post traumatic stress disorder symptoms in a psychiatric population not presenting with trauma: A preliminary study. African Journal of Psychiatry, 11(1), 51-53. http://dx.doi.org/10.4314/ajpsy.v11i1.30255. [ Links ]
Munjiza, J., Law, V., & Crawford, M. J. (2014). Lasting personality pathology following exposure to catastrophic trauma in adults: Systematic review. Personality and Mental Health, 8(4), 320-336. http://dx.doi.org/10.1002/pmh.1271. [ Links ]
Norman, R., Matzopoulos, R., Groenewald, P., & Bradshaw, D. (2007). The high burden of injuries in South Africa. Bulletin of the World Health Organisation, 85(9), 695-702. http://dx.doi.org/10.2471/BLT.06.037184. [ Links ]
Pine, D. S., Costello, J., & Masten, A. (2005). Trauma, proximity, and developmental psychopathology: The effects of war and terrorism on children. Neuropsychopharmacology, 30(10), 1781-1792. http://dx.doi.org/10.1038/sj.npp.1300814. [ Links ]
Seedat, S., Stein, D. J., & Carey, P. D. (2005). Post-traumatic stress disorder in women: Epidemiological and treatment issues. CNS Drugs, 19(5), 411-427. http://dx.doi.org/10.2165/00023210-200519050-00004. [ Links ]
Souto, R. Q., Araujo, F. K., Xavier, A. F., & Cavalcanti, A. L. (2015). Rape against Brazilian women: Characteristics of victims and sex offenders. Iranian Journal of Public Health, 44(12), 1613-1619. [ Links ]
Stovall-McClough, K. C., & Cloitre, M. (2006). Unresolved attachment, PTSD, and dissociation in women with childhood abuse histories. Journal of Consulting and Clinical Psychology, 74(2), 219-228. http://dx.doi.org/10.1037/0022-006X.74.2.219. [ Links ]
Subramaney, U. (2006). Traumatic stress and psychopathology: Experiences of a trauma clinic. South African Psychiatry Review, 9, 105-107. [ Links ]
Tolin, D. F., & Foa, E. B. (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959-992. http://dx.doi.org/10.1037/0033-2909.132.6.959. [ Links ]
Topper, K., Van Rooyen, K., Grobler, C., Van Rooyen, D., & Andersson, L. M. (2015). Posttraumatic stress disorder and barriers to care in Eastern Cape Province, South Africa. Journal of Traumatic Stress, 28(4), 375-379. http://dx.doi.org/10.1002/jts.22032. [ Links ]
Trickey, D., & Black, D. (2000). Long-term psychiatric effects of trauma on children. Trauma, 2(4), 261-268. http://dx.doi.org/10.1177/146040860000200403. [ Links ]
Van Zyl, M., Oosthuizen, P. P., & Seedat, S. (2008). Post traumatic stress disorder: Undiagnosed cases in a tertiary inpatient setting. African Journal of Psychiatry, 11(2), 119-122. http://dx.doi.org/10.4314/ajpsy.v11i2.30263. [ Links ]
Williams, S. L., Williams, D. R., Stein, D. J., Seedat, S., Jackson, P. B., & Moomal, H. (2007). Multiple traumatic events and psychological distress: the South African stress and health study. Journal of Traumatic Stress, 20(5), 845-855. http://dx.doi.org/10.1002/jts.20252. [ Links ]
Wolf, G. K., Reinhard, M., Cozolino, L. J., Caldwell, A., & Asamen, J. K. (2009). Neuropsychiatric symptoms of complex posttraumatic stress disorder: A preliminary Minnesota Multiphasic Personality Inventory Scale to identify adult survivors of childhood abuse. Psychological Trauma: Theory, Research, Practice, and Policy, 1(1), 49-64. http://dx.doi.org/10.1037/a0015162. [ Links ]
Received 11 March 2016
Accepted 10 January 2017
* Corresponding author. Department of Psychiatry (G66), Faculty of Health Sciences, University of the Free State, PO Box 339, Bloemfontein, 9300, South Africa. Fax: +27 (0)51 430 3834.
E-mail addresses: VanZylL@fshealth.gov.za (L. van Zyl), NelC@fshealth.gov.za (C. Nel), DuToi@fshealth.gov.za (M. du Toit), gnbsgj@ufs.ac.za (G. Joubert).














