Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Health SA Gesondheid (Online)
On-line version ISSN 2071-9736
Print version ISSN 1025-9848
Health SA Gesondheid (Online) vol.21 n.1 Cape Town 2016
http://dx.doi.org/10.1016/j.hsag.2016.05.003
SPECIAL EDITION 2016
Primary health care management challenges for childhood atopic eczema as experienced by the parents in a Gauteng district in South Africa
Kaarina Frieda Meintjes*; Anna Getruida Wilhelmina Nolte1
University of Johannesburg, P.O. Box 524, Auckland Park, Johannesburg, 2006, South Africa
ABSTRACT
The goal of this study was to explore and describe the experience of parents regarding the primary health care (PHC) management of their children's atopic eczema in a Gauteng district. A qualitative, explorative, descriptive, contextual embedded single case study design was employed. Data were collected through semi-structured individual interviews, field notes and direct observation until saturation occurred; analysed according to Tesch's steps of descriptive data analysis. Trustworthiness and ethical measures were used and were employed.
Three themes were identified. Management challenges, the second theme with sub-themes: drug management, knowledge levels of PHC clinicians, health education and financial challenges, will be discussed.
Keywords: Primary health care clinicians; Childhood atopic eczema; Parents; Experience
1. Introduction
1.1. Background
Atopic eczema (AE) is a common disease in most countries (Odhiambo et al., 2009). According to the World Allergy Organization (WAO), allergic diseases, of which AE is one, are on the rise worldwide and 20-30% of the world's population suffers from an allergic disease (Manjra et al., 2005 and Pawankar et al., 2008). There is not much data on AE prevalence in South Africa. Two South African studies, one in Cape Town and one in Limpopo Province, indicated a prevalence of AE in adolescents at around 19.5% (Wichmann et al., 2007 and Zar et al., 2004). Neither South African statistics for younger children (0-14 years) with atopic eczema nor Gauteng statistics for this condition are available.
Allergies can manifest in different ways and at any age. The most common allergic diseases are AE, asthma, allergic rhinitis and allergic conjunctivitis. During the first years of life, eczematous and gastrointestinal symptoms usually predominate in a typical atopic child. Asthma and allergic rhinitis and/or allergic conjunctivitis tend to develop later. This is the so-called 'atopic march' (Johansson et al., 2001 and Manjra et al., 2005).
There are different criteria that could indicate a child has atopic eczema. The PHCC should suspect AE if the child presents with the features of atopy, using one of the available sets of criteria, such as Hanifin and Rajka (1980) or the UK working party diagnostic criteria for AE (Williams et al., 1994).
1.2. Problem statement
Childhood atopic eczema has a significant effect on the patient and family. The physical and emotional effect that CAE has on the well-being of the patient and the family has been widely researched (Barnetson and Rogers, 2002, Carr, 2009, Lewis-Jones, 2006, Meintjes and Nolte, 2015, Su et al., 1997 and Van Onselen, 2009). Further AE is often undertreated, despite the disabling effect it has on the quality of life of the patient (Carr, 2009 and Manjra et al., 2005). In a survey done by Oilatum®Junior in the United Kingdom for the national Eczema Society (NES) it became clear that parents of children with AE suffered due to too little information, treatment and support received from the PHCC (Spink, 2009). In her practice as specialist dermatology nurse in the United Kingdom, Van Onselen (2009) found that parents were frustrated during their first appointment with her, because they have not previously been accorded the time for support and information. There is no study found on how PHC management of CAE is experienced by parents in Gauteng. Although AE is a condition that is regularly seen in PHC facilities in Gauteng, there are no statistics kept on the number of patients seen with atopic eczema (children and adults).
There are many treatment guidelines for CAE in the world. In South Africa there is a management guideline for the management of atopic dermatitis available that mainly focuses on medical doctors (Green & Sinclair, 2014) and a consensus document on CAE that provides management guidelines (Manjra et al., 2005). The Standard Treatment Guidelines and Essential Drug List (EDL) (Department of Health, 2008) is the protocol that needs to be followed by the PHCC in the public sector in treating patients for various conditions, including AE. The treatment protocol in the EDL gives limited guidance on management of CAE to the PHCC, especially when compared to the CAE consensus document for South Africa. The question arose: How do parents experience the PHC management of CAE?
1.3. Research objective
The objective was to explore and describe how parents experience the PHC management of CAE in the public sector of a district in Gauteng.
1.4. Definition of key concepts
Atopy: The WAO defines atopy as "a personal and/or familial tendency, usually in childhood or adolescence, to become sensitized and produce IgE antibodies in response to ordinary exposure to allergens, usually proteins. As a consequence, these persons can develop typical symptoms of asthma, rhinoconjunctivitis, or eczema" (Johansson et al., 2004).
Eczema is a chronic inflammatory skin disorder that develops mainly in early childhood (Hofer & Leung, 2002; National Institute for Health and Clinical Excellence (NICE), 2007), but could also develop in adulthood for the first time (Heyl & Swart, 1990)
Childhood: According to the Children's Act no 38 of 2005 (Department of Health, 2006), a child is a person under the age of 18. In this study, childhood will refer to children 0-14 years of age.
Primary health care: PHC in South Africa is the first level of health care. According to the African National Congress' National Health Plan for South Africa (ANC, 1994) PHC forms the central focus for health services. In the public health sector of a district of Gauteng, PHC is mainly rendered at clinics or community health centres by PHCCs.
Primary health care clinician (PHCC): In the context of this study, a PHCC is a nurse registered with the South African Nursing Council (SANC) as a general nurse, as well as a community health nurse, who is preferably also registered with an additional qualification in Clinical Nursing Science, Health Assessment, Treatment and Care (South African Nursing Council, 1997: Regulation 48). This group of PHCCs was the focus of the study, although medical practitioners who hold a Bachelor's qualification in Medicine and Surgery (MBChB) and work full or part-time in a PHC facility could also be part of the research as they follow the same treatment guidelines as the nurse PHCCs.
Parent: "A father or mother, one who begets or one who gives birth to or nurtures and raises a child"(The Free Dictionary, http://www.thefreedictionary.com/parent). The parent in this study is the mother or father of a child with AE.
Experience: "An event or a series of events participated in or lived through."(The Free Dictionary, http://www.thefreedictionary.com/experience). The lived experience of parents with a child suffering from AE is explored.
Management: "Coordinated care and advocating for specified individuals and patient populations across settings to reduce costs, reduce resource use, improve quality of health care and achieve desired outcomes". (The Free Dictionary, http://medical-dictionary.thefreedictionary.com/management). In this study management refers to the way a child with AE is treated on the PHC level.
1.5. Contribution to the field
One of the rationales for this study was to provide parents an opportunity to describe how they experience the PHC management of CAE. In exploring the phenomenon in this case study, insight was gained on how parents experience PHC management of CAE in the public health system of South Africa.
2. Research design and methods
2.1. Design
The study was qualitative, explorative and descriptive with the aim to explore and describe the experience of parents of the public sector PHC management of CAE in a district in Gauteng.
2.2. Method
A single embedded case study method was employed. This study had as the case (population) PHC management of CAE in the public sector of a district of Gauteng, within the wider context of the public health care system. The embedded units (samples) of this single case were the parents of children 0-14 years suffering from AE, the PHCC and the doctors and specialist. This article focuses on embedded unit one, namely the parents.
Embedded unit one: Parents of children 0-14 years of age suffering from AE. The inclusion criteria were: the parents must have visited a PHC facility with their child who has AE; they must be able to speak Afrikaans, English, Setswana or Zulu, as these are the languages the skilled interviewer, who holds a Doctor Curationis degree in psychiatric nursing can speak. These parents were purposively selected as they were information rich participants of the phenomenon under study. The selection was done as follows: the researcher explained the research to the people in the waiting room and parents who were willing to be interviewed were purposively selected from the waiting room if they met the inclusion criteria.
2.3. Data collection
Different methods of data collection were used: semi-structured individual interviews, direct observation and field notes.
2.3.1. Semi-structured interviews
Semi-structured individual interviews were held with parents from October to December 2010. A skilled interviewer, who holds a Doctor Curationis degree in psychiatric nursing and has conducted many interviews, conducted the parent interviews in the parent's language of the choice, in a private room. The researcher kept field notes during the interviews. The interviews were audio-taped as this assisted the interviewer and researcher to focus on the interview and not to lose any important verbal and non-verbal information from the participant. The participants had to give written consent to be interviewed and audio-taped. The researcher co-signed the consent document. The questions asked to the participants were: Parents: 'How is it for you living with a child who suffers from atopic eczema?' and 'How do you see the role of primary health care clinicians regarding the management of childhood atopic eczema?'
An initial pilot interview was conducted to test the questions. It was transcribed and analysed and found to be suitable and therefore was included as part of the findings. Interviews were done until data saturation occurred, that is no new information emerged.
2.3.2. Direct observation
The researcher utilised open-ended direct observation to observe the physical environment of the unit, as well as the provincial and local authority PHC clinics. Data were collected during the visits to the clinics and the unit during interviews, but also on days set aside specifically for direct observation. In order to minimise the Hawthorne effect, the researcher spent some time in the settings so that the participants could get used to her presence. She also placed herself among the patients in the waiting room, where she could observe what was happening in the waiting room as well as in the consultation rooms, without intruding in the space of the health care workers. The researcher recorded the observations: the way patients moved in the queue to be seen; how the consultation rooms were utilised. With every new consultation the number of people in the room and who they were; as well as the type of verbal and non-verbal communication between the doctor, PHCC and parent were observed and recorded. Actions such as weighing and height measuring of the child, physical examination; health education and recording of information in the patient's file, was also observed and recorded. The time a patient spent in the consultation room with the doctor or PHCC was also observed and recorded. Data were collected until data saturation occurred, that is no new observations were made.
2.4. Data analysis
All data collected were converted into a written format. The interviews were transcribed verbatim. The interviews in languages other than English were transcribed in their original language to keep the meaning intact and then translated into English for analysis by the researcher. The data collected through direct observation was put into text form. Data from all the collection methods were analysed using Tesch's eight steps of the descriptive method of data analysis, as reflected in Creswell (2014). Themes, categories and sub-categories were identified by the researcher and two independent coders. Consensus discussions were held to refine the themes, categories and sub-categories. The findings are supported by direct quotations by the participants, field notes and notes from the direct observation. The findings were re-contextualised by means of a literature review.
Theme two: PHC management challenges of CAE as experienced by the parents will be discussed in this article.
3. Ethical considerations
The four ethical principles - autonomy, beneficence, non-maleficence and justice - as endorsed by the Medical Research Council of South Africa (2001) were followed. Participation was voluntarily and the participants' information is only known to the researcher and the skilled interviewer. Raw data are kept under lock and key and will be destroyed two (2) years after publication of the research. The risk for the participants was negligible, but if debriefing was needed, it was provided by the researcher as part of the professional and ethical responsibility. Ethical clearance was received from the University of Johannesburg Higher Science and Ethical Committee (AEC 24/01-2010), as well as from the relevant organisations.
4. Trustworthiness
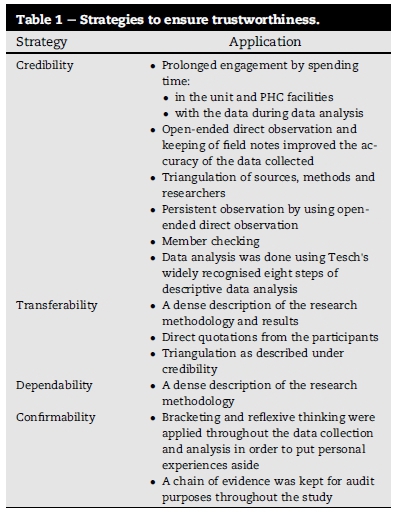
The Guba model of trustworthiness (Lincoln & Guba, 1985) was used throughout the research study: credibility, transferability, dependability and confirmability as summarised in Table 1.
5. Results and discussion
5.1. Demographics
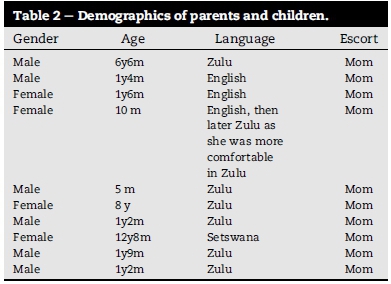
The demographics of the parents and children are reflected in Table 2.
5.2. Results
The categories identified under theme two are: drug management, knowledge levels of PHCC, health education and financial challenges.
5.2.1. Drug management
The sub-categories identified were: the ineffective and/or insufficient quantities of drug management on PHC level; inconsistent, but effective drug management on tertiary level; the defaulting of treatment and alternative treatment that seemed to help. All of this affected the physical, emotional and social wellbeing of the child and/or the parent.
Ineffective and/or insufficient quantities of drugs: The PHCC dispensed drug treatment for eczema, but often it was not effective, because it is not the preferred drug treatment for atopic eczema and thus did not really help for many of the patients. The quantity of drug treatment dispensed to the patients was often not enough and added to the physical discomfort of the children and the frustration and stress levels of the parents. This could be due to some of the treatments not forming part of the EDL for the PHC level or due to ordering issues, because PHCC tended to dispense very limited drug treatment at a time:
◦"Banginika (clinic) imedication but azange ingisize"
(They (clinic) gave me medication, but it never helped.)
◦ "ok the clinic has given me … ehh … just a little bit of a …. .emulsifying ointment, they have put it inside a …. ehh … a plastic of pills, so it was very small"
Effective drug management on tertiary level: The parents felt that drug treatment at the tertiary hospital was effective, as opposed to the drug treatment received from the PHC clinics. The effectiveness of the treatment caused a feeling of satisfaction to the parents. The availability of the hospital drug treatment was, however, inconsistent.
◦ "… because I can see that it is working … it is better. It is better than the medication that they give at the clinic."
◦ "uma uza la (name) bakunika izinto one by one, uma ufika izinto awuzitholi zonke. Mhlawumbe bakunika ngabo 2 by 2 and lezi bebakunikeza zona zonke zizamnceda umntwana."
(And when you come here at (name) they give you things one by one, when you arrive here, you don't get everything. Maybe they give you two by two and where else, the ones you were getting, they all help the child).
Defaulting of treatment: Parents indicated that they sometimes did not have the money for transport to go to the clinic, resulting in them defaulting treatment.
"Ngoba ngesinye isikhathi uma ngithi imali iyiproblem enkulu, kwesinye isikhathi uthole idate yakhe yokuza ize nginganamali, ngiyayijampa ngempela."
(Sometimes money is the biggest problem of all, sometimes you'll find that with the follow-up date of the child there is no money. I am really struggling.)
Alternative treatment that helps: Some parents mentioned alternative treatments they have tried that seemed to have helped. Alternative treatment here means treatment not received from the PHC clinic. The alternative treatments mentioned in the interviews were: Cuticura, Epimax (which is an emollient, but different from the emollient dispensed by the PHC clinics or hospital pharmacy) and a Disprin and lemon juice solution.
◦ "And iCuticura ngiyithenga ngoba ibhaliwe nokuthi noma une rash or ieczema but, yona ayisusi leskin iyapholisa nje ukuthi kuphele lokukuluma iphinde iqale futhi bese uyamgcobisa futhi."
(I buy Cuticura because it is written that it helps with rash or eczema, but it does not remove that skin, it only makes it better so that the itchiness can become better. When it comes back you use it.) ◦
"Then … omunye … ngahlangana nomunye usisi eClicks wangi adviser ukuthi ngisebenzise iepimax at least yaba better unlike before."
(I met a woman at Clicks and she advised me to use Epimax and at least it was better than before.)
◦ "Uma ngimgcobisa kuma pores, ububovu sebuyaziphumela, budonswa yi Disprin nale lemoen. Uma uqala umfaka kuyababa then after 5 minutes sekupholile buphumile, until lobovu buphuma bonke lwase laphuma lonke, after kwamila izinwele. So, mina bengiqabanga ukuthi, mhlawumbe sivumele nabanye abantwana ngoba abanye iliquid paraffin ayiba sizi. Mhlawumbe abo soscience bangazama ukuyenza le mixture yami le bangayibona ukuthi ingaba siza abanye, ngoba mina ayizange, iyizange bekanganazinwele uS, ngibele ngiyigcobisa."
(When I applied on the pores, the redness will come up, the Disprin and lemon juice will bring it up on top. When I applied it, it was itchy, but after 5 min it gets better, the redness came out and after her hair started growing. So, I was thinking that, maybe we should allow other kids to use this, because this liquid paraffin is not working. Maybe science people they can try to make this mixture of mine to see if it cannot help others, it helped S because she did not have hair, I am still applying it.)
5.2.2. Knowledge levels of PHCC
Parents felt the PHCCs had limited knowledge of CAE, its causes, the clinical presentation and its treatment. The PHCCs often confused eczema with other skin conditions, such as heat rash or tinea corporis. The PHCCs had some idea that allergens could be the reason for the eczema.
◦ "Then they did not notice … then I said to the nurse: My child is having some problem. Can you see the skin is not … she said no it is heat rash, don't mind that one …"
◦ "Azange basho ukuthi une eczema, like bathi unama ringworms uyabona."
(They have never told me that s/he has eczema. They told that s/he has ringworms.)
◦ "when I apply the medication that they gave me, because … the nurses, they don't know exactly which medication to give the child, it made him more worse."
◦ "Ba ile ba re a tlogele dijo tsa lebese, o mongwe o tla go bolela gore re tlhwatse dikobo tsa rona, e ne rona re tla tshwa … ba re ditlhwatse, re dibeye mo letsatsing e ne rona ra e ira ntho eo. O mongwe o tla go bolela … ko re ba sele, ba sele …"
(They just said we should omit dairy products, one will say we should wash our blankets. And we do wash our blankets, they say we should wash them and put them in the sun. Another one will tell this and that, I find some of them being silly … silly.)
5.2.3. Health education
Parents received some health education from PHCCs, mainly on food and soap. One parent said that she did not receive any health education. The parents expressed the need for more knowledge regarding the condition and what to do.
◦ "motho o dutseng fatshe a be a tlhalosetsa this thing ke kliniki yako ya (name of clinic)"
(The person who really told me about this thing, is at the clinic at (name of clinic))
◦ "angikaze mina mhlawumbe bayabanika kodwa, mina akaze ngahlangana nabo angikaze."
(I don't know, maybe they (PHCC) do it (health education), but I have never seen it, so I don't know.)
◦ "Hayi kuyasebenza, ngoba cause bokuthi uma kuqala adle idairy product uyabona uzozinwaya uyabona at least manje kungcono."
(It (diet) is working, because when it starts s/he used to eat dairy products, you see s/he will scratch, you see. At least now it is better.)
◦ "… cause bathi ngingasebenzisi insipho uallergic uyabona …"
(… because they said I must not use soap to bath … allergic …)
◦ "Anginayo ngazi nje ukuthi umntwana une eczema engingayazi ukuthi imean ini"
(I do not have, all that I know is that the child has eczema, something that I do not even know what it means.)
◦ "I was just concerned ukuthi lesifo siphuma kuphi? … ngoba ngesintu bazokutshela kuthiwa igazi elingcolile."
(I am just concerned about where does this illness come from? … because in African terms they will tell you that her blood is dirty.)
◦ "… ngifanele ngenze njani ukuthi umntwana wami abe right uyabona into leyo"
(… what am I supposed to do for my child to be alright, you see things like that).
5.2.4. Financial challenges
Parents expressed the financial challenges in managing their children with AE. Parents sometimes had to buy treatment from pharmacies when they did not get effective or sufficient treatment from the PHC clinics. The treatment is expensive to buy.
◦ "Ngi feela bad ngoba like ngimlethile and imithi yakhe echemist iexpensive"
(I feel bad because like I brought my child to the clinic and at the chemist the medication is very expensive) (field note: got very little treatment from the clinic).
Parents also found it expensive to see private doctors in their search for effective treatment for their children:
◦ "I must just go back to him (doctor), so I can't afford, so now … so I decided I'll come back to the clinic … (sighs)"
Parents often had to implement additional measures in the management of the children with AE. These measures, involving additional treatment, food choices and hygiene, cost money.
◦ "And then vele sengiyazi, sengivela ngiyilande eClicks ngecard uma kuthi bengine mali"
(I just simply go to buy the medication at Clicks with the card and that's if I have money)
◦ "I strive hard just to give the child food with … ehh … supplement of vitamin A, like … ehh … try spinach …" "So I … I give him a lot of vegetables and … and I normally stick to Purity, because they … I know that it is ehh … that there is no air that is entered … that it is not contaminated and everything … so I try to … I ehh … watch the diet very carefully."
◦ "phela go tlhatswa dikobo goseng every morning, re bile ra reka washing machine e kgolo re bona gore ga re kgone dikobo every morning re tshwanetse go di tlhwatsa ra reka top loader ke tsena … ke tlhatswa dikobo, dibijama tsa gage,"
(You know I have to wash every morning her blankets, we had to buy a big washing machine, seeing that so that we should wash her blankets every morning that is why we bought a top-loader … I have to wash her blankets, pyjamas).
The discussed findings were re-contextualised by means of a literature control.
5.3. Literature control
Drug management and knowledge levels: Hay (2005) stated in the editorial that skin conditions are often not well managed on PHC level. According to Hay (2005) two of the main factors that play a role, are poor knowledge levels of PHCCs, leading to poor disease recognition and management, and the unavailability of treatment. Van Deventer (2007) found that some of the factors that led to poor outcomes in chronically ill patients in primary and rural care in South Africa were the lack of appropriate drugs and equipment and/or lack of knowledge and/or clinical rigour of health care workers, lack of money to return for follow-up visits, which then led to defaulting on the treatment and a denial by patients of the seriousness of their chronic condition and its possible complications. In a study conducted by The World Allergy Organization Speciality and Training Council (Warner et al., 2006) it was found that the majority of allergic patients were seen by non-allergy-trained health workers. This situation is also true for South Africa (Pawankar et al., 2008 and Potter et al., 2009). The allergy clinic at Red Cross Children's Hospital was the first of its kind in Southern Africa to provide postgraduate allergy training to senior paediatric registrars (Weinberg, Potter, & Motala, 2006), but there is no specialised allergy training for nurses.
Health education: In their study on the effect of consultation in a dermatology clinic on CAE, where management issues, such as optimising of treatment, diet, bathing and keeping a child cool were discussed and reinforced later by a specialist nurse, Beattie and Lewis-Jones (2006), found that these actions had a positive impact on the quality of life of the child and the family. The French consensus document on management of AE (Stalder et al., 2005) stated that health education forms the focus for treating the patient, as it improves the cooperation of the patient and parent and improves management outcomes. There is consensus among allergy experts that educational interventions should form part of the management of AE (Stalder et al., 2013). Time spent on the educational intervention is an important factor which impacts on the success of educating the parents (Moore, Williams, Manias, & Varigos, 2006).
Alternative treatment: In a South African study by Stear (2011) it was found that more than half of the participants (general practitioners, specialists and dieticians) indicated that their patients were using complementary and alternative therapy before seeking conventional medical care, and that 43% were using this together with the medical treatment received from the participants. The most common complementary and alternative therapies identified were homoeopathy, kinesiology and traditional African herbal remedies. Herselman (2007) gives reasons why South African patients seek alternative trans-cultural treatment, including the fact that treatment from one health care option seems slower than an option from another. A systematic review on alternative treatments and atopic diseases concluded that, although there are some promising studies, results are not conclusive and more research is needed to identify the mechanisms of actions of these therapies and whether the clinical effects are true and not linked to any placebo effects (Pfab et al., 2013).
Financial challenges: There are direct and indirect costs involved in the management of children with AE. The direct costs related to treatment issues and indirect costs to loss of working time. The cost of managing moderate to severe CAE was found to be higher than that of childhood asthma, but similar to the cost for managing childhood diabetes (Su et al., 1997). Financial constraints for many of the patients and the generally expensive alternatives to food allergies are some of the areas of concern for allergy care in South Africa (Stear, 2011).
6. Conclusion
The research objective to explore parents' experience of the PHC management of their children with AE was addressed. The findings indicated that they experienced challenges regarding the drug management prescribed and received on PHC level, the health education received and the knowledge levels of PHCCs, as well as financial challenges related to the treatment. Some recommendations to address these challenges will be discussed next.
7. Recommendations
The findings discussed clearly indicate that parents experienced challenges regarding the PHC management of their children with AE. In addressing these management challenges the first recommendation is to develop a PHC management guideline for CAE. This guide can help PHCCs to prescribe the correct drug management in sufficient quantities. It can also help to give evidence-based health education to the parents.
The second recommendation is to enhance the knowledge levels of PHCCs on CAE. This can be done by incorporating allergy and allergic diseases in more depth into the basic nursing curriculum and the curriculum for the SANC Regulation 48: Clinical assessment, diagnosis, treatment and care. In-service training and workshops on CAE for PHCCs could also enhance the knowledge levels. Developing a short course for nurses on CAE and possibly other allergic diseases could be one of the strategies to improve the knowledge basis on CAE.
Author's contribution
Dr Meintjes - researcher (then PhD student).
Prof. AGW Nolte - supervisor.
Acknowledgement
Dr. A. Temane and Dr. C. Dörfling were the independent coders. Prof E.G. Weinberg was the consultant regarding allergy matters.
References
African National Congress. (1994). A national health plan for South Africa. Available from: http://www.anc.org.za/ancdocs/policy/health.html. [ Links ]
Barnetson, R. S. C., & Rogers, M. (2002). Childhood atopic eczema. British Medical Journal, 324(7350), 1376e1379. [ Links ]
Beattie, P. E., & Lewis-Jones, M. S. (2006). An audit of the impact of a consultation with a paediatric dermatology team on quality of life in infants with atopic eczema and their families: further validation of the infants' dermatitis quality of life index and dermatitis family impact score. British Journal of Dermatology, 155(6), 1249e1255. [ Links ]
Carr, J. D. (2009). Evidence-based management of childhood atopic eczema. British Journal of Nursing, 18(10), 603e604, 606, 608. [ Links ]
Creswell, J. (2014). Research design: Qualitative, quantitative and mixed methods approaches. Los Angeles: Sage. [ Links ]
Department of Health Republic of South Africa. (2006). Children's Act 38 of 2005. Pretoria: Government Printer. [ Links ]
Department of Health Republic of South Africa. (2008). Standard treatment guidelines and essential medicines list for South Africa. Primary health care level (4th ed.). Pretoria: The National Department of Health. [ Links ]
Free Online Dictionary, Thesaurus and encyclopaedia. Available from: http://www.thefreedictionary.com/experience [ Links ]
Free Online Dictionary, Thesaurus and encyclopaedia. Available from: http://medical-dictionary.thefreedictionary.com/management [ Links ]
Free Online Dictionary, Thesaurus and encyclopaedia. Available from:: http://www.thefreedictionary.com/parent [ Links ]
Green, R. J., & Sinclair, W. (2014). General approach to and summary of the guideline for the management of atopic dermatitis. South African medical Journal, 104(10), 720e721. [ Links ]
Hanifin, J. M., & Rajka, G. (1980). Diagnostic features of atopic dermatitis. Acta Dermatovenereol, 92, 44e47. [ Links ]
Hay, R. J. (2005). Editorial: public health and skin disease. Community Dermatology, 2, 1e2. [ Links ]
Herselman, S. (2007). 'Health care through a cultural lens': insights from medical anthropology. Current Allergy & Clinical Immunology, 20(2), 62e65. [ Links ]
Heyl, T., & Swart, E. (1990). Dermatologie vir suider-afrika. Butterworth: Durban. [ Links ]
Hofer, M. F., & Leung, D. Y. M. (2002). Anti-IgE and allergic skin diseases. In R. B. Fick, Jr., & P. M. Jardieu (Eds.), IgE and anti-IgE therapy in asthma and allergic diseases. New York: Marcel Dekker Inc. [ Links ]
Johansson, S. G. O., Bieber, B., Dahl, R., Friedmann, P. S., Lanier, B. Q., Lockey, R. F., et al. (2004). Revised nomenclature for allergy for global use: report of the nomenclature review committee of the world allergy organization, October 2003. Journal of Allergy Clinical Immunology, 113, 832e836. [ Links ]
Johansson, S. G. O., Hourihane, J. O. B., Bousquet, J., Bruijnzeel- Koomen, C., Dreborg, S., Haahtela, T., et al. (2001). A revised nomenclature for allergy: an EAACI position statement from the EAACI nomenclature task force. Allergy, 56(9), 813e824. [ Links ]
Lewis-Jones, S. (2006). Quality of life and childhood atopic dermatitis: the misery of living with childhood eczema.International Journal of Clinical Practice, 60(8), 984e992. [ Links ]
Lincoln, Y. S., & Guba, E. G. (1985). Naturalistic inquiry. Newbury Park: Sage. [ Links ]
Manjra, A. I., du Plessis, P., Weiss, R., Motala, C. M., Potter, P. C., Raboobee, N., et al. (2005). Childhood atopic eczema consensus document. South African Medical Journal, 95(6), 435e440. [ Links ]
Medical Research Council of South Africa. (2001). Guidelines on ethics for medical research: General principles (4th ed.). Tygerberg: Medical Research Council. [ Links ]
Meintjes, K. F., & Nolte, A. G. W. (2015). Parents' experience of childhood atopic eczema in the public health sector of Gauteng. Curationis, 38(1), 9. http://dx.doi.org/10.4102/curationis.v38i1.1215. [ Links ]
Moore, E., Williams, A., Manias, E., & Varigos, A. (2006). Nurse-led clinics reduce severity of childhood atopic eczema: a review of the literature. British Journal of Dermatology, 155(6), 1242e1248. [ Links ]
Odhiambo, J. A., Williams, H. C., Clayton, T. O., Robertson, C. F., Asher, M. I., & ISAAC Phase Three Study Group. (2009). Global variations in prevalence of eczema symptoms in children from ISAAC phase three. Journal of Allergy and Clinical Immunology, 124(6), 1251e1258. http://dx.doi.org/10.1016/j.jaci.2009.10.009. [ Links ]
Pawankar, R., Baena-Cagnani, C. E., Bousquet, J., Canonica, G. W., Cruz, A. A., Kaliner, M. A., et al. (2008). State of world allergy report 2008: allergy and chronic respiratory diseases. World Allergy Organisation Journal, S4eS17. June 2008: Supplement 1. [ Links ]
Pfab, F., Schalok, P. C., Napadow, V., Athanasiadis, G. I., Ring, J., & Huss-Mapp, J. (2013). Contemporary integrative medicine in atopic diseases e an overview. Focus on Alternative and Complementary Therapies, 18(2), 77e84. [ Links ]
Potter, P. C., Warner, J. O., Pawankar, R., Kaliner, M. A., Del Giacco, S., & Rosenwasser, L. (2009). Recommendations for competency in allergy training for undergraduates qualifying as medical practitioners: a position paper of the World Allergy Organization. World Allergy Organization Journal, 2(8), 150e154. [ Links ]
South African Nursing Council (SANC). (1997). Regulations for the diploma in clinical nursing science, health assessment, treatment and care. Government Notice No. R. 48. Available from: http://www.sanc.co.za/regulat/Reg-cht.html. [ Links ]
Spink, P. R. (2009). New research show's GPs struggle to offer recommended levels of care to children with eczema sourcewire news distribution. Available from: http://www.responsesource.com/releases/rel_display.php?relid=46909&ptint=true. [ Links ]
Stalder, J. F., Armingaud, P., Aulanier, S., Bourrier, T., Castanet, J., Celerien, P., et al. (2005). Consensus conference management of atopic dermatitis in children. Recommendations (Short version). European Journal of Dermatology, 15(4), 215e223. [ Links ]
Stalder, J. F., Bernier, C. D., de Raeve, L., Gieler, U., Deleuran, M., Marcoux, D., et al. (2013). Therapeutic patient education in atopic dermatitis: worldwide experiences. Pediatric Dermatology, 30(3), 329e334. [ Links ]
Stear, G. I. J. (2011). Management of food allergies in children in South Africa: Determining aspects of the knowledge and practices of dieticians and medical doctors. Available from: http://scholar.sun.ac.za/handle/10019.1/6765. [ Links ]
Su, J. C., Kemp, A. S., Varigos, G. A., & Nolan, T. M. (1997). Atopic eczema: its impact on the family and financial cost. Archives of Disease in Childhood, 76(2), 159e162. [ Links ]
Van Deventer, C. (2007). Asthma: an approach to some barriers to practice in primary and rural care. Current Allergy and Clinical Immunology, 20(2), 56e60. [ Links ]
Van Onselen, J. (2009). Unlocking the misery of childhood atopic eczema. British Journal of Nursing, 18(10), 590. [ Links ]
Warner, J. O., Kaliner, M. A., Crisci, C. D., Del Giacco, S., Frew, A. J., Lui, G., et al. (2006). Allergy practice worldwide: a report by the world allergy organization specialty and training Council. International Archives of Allergy and Immunology, 139(2), 166e174. [ Links ]
Weinberg, E. G., Potter, P. C., & Motala, C. (2006). Practice review: the allergy clinic: 50 years. South African Medical Journal, 96(9), 902e904. [ Links ]
Wichmann, J., Wolvaardt, J. E., Maritz, C., & Voyi, K. V. V. (2007). Household conditions, eczema symptoms and rhinitis symptoms: relationship with wheeze and severe wheeze in children living in the Polokwane area, South Africa. Maternal Child Health Journal, 13, 107e118. [ Links ]
Williams, H., Burney, P. G., Hay, R. J., Archer, C. B., Shipley, M. J., Hunter, J. J., et al. (1994). The UK working party's diagnostic criteria for atopic dermatitis: derivation of a minimum set of discriminators for atopic dermatitis. British Journal of Dermatology, 131(3), 383e396. [ Links ]
Zar, H. J., Ehrlich, R. I., & Weinberg, E. G. (2004). The prevalence of asthma, allergic rhinitis and atopic eczema (ISAAC phase 3 study) in adolescents in Cape Town and comparison with ISAAC 1. Current Allergy and Clinical Immunology, 17(3), 140. [ Links ]
Received 26 October 2015
Accepted 6 May 2016
Abbreviations: PHC, primary health care; PHCC, primary health care clinician; CAE, childhood atopic eczema; AE, atopic eczema; WAO, World Allergy Organisation
Peer review under responsibility of Johannesburg University.
* Corresponding author. Tel.: +27 011 559 6894, +27 072 66 11 691 (mobile).
1 Tel.: +27 011 559 6922, +27 082 804 1916 (mobile).














