Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Health SA Gesondheid (Online)
On-line version ISSN 2071-9736
Print version ISSN 1025-9848
Health SA Gesondheid (Online) vol.21 n.1 Cape Town 2016
http://dx.doi.org/10.1016/j.hsag.2016.06.006
SPECIAL EDITION 2016
Case studies on the homeopathic treatment of binge eating in adult males
Radmila Razlog; Janice Pellow; Reshma Patel*; Marelize Caminsky; Hertzog Johannes van Heerden
Department of Homoeopathy, University of Johannesburg, Doornfontein Campus, P.O. Box 17011, Doornfontein, Gauteng 2028, South Africa
ABSTRACT
BACKGROUND: Homeopathy seeks to treat holistically. The role of homeopathy for treating binge eating however remains poorly explored.
OBJECTIVE: To determine the efficacy of individualized homeopathic treatment on binge eating.
METHOD: This was a nine-week pilot study using a case study design. Individualized homeopathic remedies were prescribed to each participant for six weeks and case analysis evaluated changes over time.
RESULTS: All participants reported a decrease in the severity and frequency of binging behaviour; concurrent improvements in general health were also noted.
CONCLUSION: This pilot study shows the potential benefits of individualized homeopathic treatment in binge eating in males.
Keywords: Homeopathy; Binge eating; Case studies
1. Introduction
1.1. Problem statement
Binge eating is a common symptom associated with eating disorders such as bulimia nervosa (BN) and binge eating disorder (BED). Binge eating is often accompanied by gastrointestinal discomfort, constipation, and abdominal distention which contributes to a poor quality of life. Eating disorders are often associated with underlying disturbances in emotional regulation and body image which leads to poor self-esteem and social isolation. Furthermore eating disorders can result in medical complications such as electrolyte abnormalities, oedema, cardiac conduction abnormalities and gastrointestinal complications (Colton, Rodin, Bergenstal, & Parkin, 2009). Obesity is the biggest complication of binge eating, which in turn may lead to associated health risks and complications, such as cardiovascular disease, gastro-esophageal reflux disease (GERD), sleep related breathing disorders and type II diabetes mellitus (Herrin, 2003). Binge eaters with an underlying eating disorder typically have psychological, social and medical co-morbidities resulting in a reduced quality of life (Hilbert, 2013). Current conventional treatment options for eating disorders include cognitive behavioural therapy (CBT), interpersonal psychotherapy (ITP), and selective serotonin reuptake inhibitors (SSRIs). It is difficult to assess the individual success rates of these treatments as they are often used in combination (McElroy, Guerdjikova, Mori, & O'Melia, 2012). Despite these treatment options, less than half of chronic cases seek treatment (Kessler et al., 2013). Treatment resistance in eating disorders is a common feature and is usually predicted by the severity of the core eating disorder psychopathology - this resistance complicates the disorder and is documented by poor response rates in many treatment trials (Halmi, 2013). The role of homeopathic treatment for eating disorders remains unknown. However, in certain isolated case studies, findings showed favourable results (Feingold, 2005, Feingold, 2006, Fixsen, 2006 and Tree, 2007) adding an increased interest in the field of treating eating disorders with homeopathy (Maslan, 2006 and Traub, 2006). There has been no research conducted to date evaluating the efficacy of homeopathic treatment for binge eating.
1.2. Aim of the study
The aim of this pilot study was to evaluate the efficacy of individualised homeopathic treatment on males with binge eating by means of detailed case studies.
1.3. Definition of key concepts
The concepts that are central to this study are defined as follows.
Binge eating: Binge eating is a common phenomenon associated with eating disorders such as bulimia nervosa (BN) and binge eating disorder (BED). It is defined as consuming a large quantity of food in a short period of time, with a subjective "sense of loss of control" (American Psychiatric Association, 2013).
Case study: A case study is an empirical inquiry that investigates a contemporary phenomenon (the "case") in depth and within its real-world context. This is especially done when the boundaries between phenomena and context may not be clearly evident (Yin, 2014).
Homeopathy: Homeopathy is a system of medicine founded by Dr Hahnemann which makes use of potentised remedies to stimulate the body's innate healing mechanisms (De Schepper, 2011).
Homeopathic principles: The Law of Similars is the principle on which the practice of homoeopathy is based. When ingested by a healthy individual, a substance produces a set of symptoms - this substance used as a homeopathic remedy will cure a disease which has the same symptoms in an unhealthy individual (De Schepper, 2010 and Kayne, 2008).
Homeopathic simillimum: The homeopathic simillimum refers to the unique, fundamental homeopathic remedy that covers the totality of symptoms experienced by the individual being treated (De Schepper, 2011).
Individualised homeopathic treatment: The individualised homeopathic remedy (also known as the similimum) is a single, unique remedy selected according to specific principles that most closely matches the total symptom picture of the patient (De Schepper, 2011). This includes their presenting symptoms, as well as generalized symptoms such as energy, appetite, sleep and perspiration.
Potentisation: The combination of the processes of diluting and succussing (shaking) a substance, is termed potentisation or dynamisation (Bloch & Lewis, 2003).
LM: LM potencies are made by diluting the medicinal substance in a ratio of one to fifty thousand, during every step of the remedy manufacturing process, instead of one part medicinal substance to ninety-nine parts solvent (centesimal) or to nine parts (decimal) (De Schepper, 2010).
Materia medica: A Materia Medica is a reference book that contains information of each remedy's symptom picture as researched (Owen, 2015).
Repertory: A repertory is an index of symptoms; each symptom has a corresponding list of remedies indicated for that symptom (Kayne & Kayne, 2007).
Repertorisation: Repertorisation is the process of using a repertory in order to find the remedy which best suits a patient's case (Bloch & Lewis, 2003).
Purposive sampling: Purposive sampling is selected based on the knowledge of a population and purpose of the study. The researcher selects participants that have a particular characteristic or fit a specific description. This technique carefully selects subjects based on study purpose with the expectation that each participant will provide unique and rich information of value to the study (Lee-Jen Wu, Hui-Man, & Hao-Hsien, 2012).
2. Materials and methods
2.1. Design
This pilot study used a nine-week case study design, consisting of ten male participants between the ages of 18 and 45 years. Participants were recruited by means of purposive sampling, using community forum postings and online social network sites. Potential candidates were screened telephonically for the following inclusion criteria: males aged 18-45 years, eating a large volume of food in a short span of time, a sense of lack of control over eating, and at least three of the following - eating at an accelerated pace, eating to physical discomfort, eating large volumes of food without being prompted by hunger, solitary eating behaviour stemming from embarrassment and/or feelings of guilt, and disgust or depression after eating. Exclusion criteria included: a previous diagnosis of anorexia nervosa, bulimia nervosa, diabetes mellitus, gallbladder disease, heart disease or cancer, any current use of allopathic medication (if a baseline treatment of six months had not been reached), and/or any homeopathic medication taken within the previous two-week period.
2.2. Research procedure
Participants attended four consultations, scheduled three weeks apart, and all consultations took place at the UJ Homeopathy Health Training Centre. At the initial consultation, each participant was interviewed around their dietary habits, including pertinent history or concurrent symptoms experienced. A more general assessment of health by system, including their current emotional state, personal and family histories, lifestyle, and a general physical examination completed the first consultation. Each case was then hand-repertorised using Murphy (1998), and the similimum remedy was determined by referring to the appropriate Materia Medica. The participants did not receive any treatment at the first consultation in order to establish a three-week treatment-free baseline with which to compare treatment intervals. Participants completed a binge eating scale (BES) to assess the severity of their binging at each consultation, and a self-monitoring binge-eating calendar each day for the duration of the study to track the number of binging episodes. They received their remedy at the second consultation. At the second, third and fourth consultations, the participants again participated in an interview in which the researcher documented any changes to previous symptoms.
Each participant was dispensed an individually selected remedy at their second and third consultations. Where possible, the researcher strived to not deviate from the initially selected remedy. In addition, the researcher did not include any other treatment regimes, and did not provide any advice regarding dietary habits or lifestyle changes. The potency of the remedies were universally selected at LM1 as the LM potency is best suited for chronic cases and those with underlying psychological co-morbidities as noted in binge eating (De Schepper, 2010). Various potencies are known to have different effects, therefore the LM potency was selected to minimise any variables to the treatment. Each participant was instructed to take their remedy daily, following eight succussions. Instructions on taking the remedy were given both verbally and in writing, and the researcher confirmed each participant's comprehension of the instructions via demonstration.
2.3. Validity and reliability
Quantitative and qualitative data each have their own strengths and weaknesses in validly describing the world. However, qualitative and quantitative research methods should be viewed in equal regard in order to realise their unique research contribution. The categorisation of case study research is nested under qualitative research (Fishman, 2012 and Verhoef et al., 2005).
Four tests have been commonly used to establish the quality of empirical case study research: construct validity, internal validity, external validity and reliability. External validity evaluates whether a study's findings are generalisable beyond the immediate study, regardless of the research method utilised. This study is exploratory in nature and therefore does not intend to produce generalisable information. Similarly, internal validity, which seeks to associate cause and effect, is not applicable to this study as this is a descriptive study that does not aim to establish a relationship between cause and effect. Construct validity is the accuracy with which a case study's measures reflect the concepts being studied. This is evident by the in-depth interviews done by the researcher which measured the severity and frequency of binge eating. The measurements of these items are included in order for the study to have validity and the research design has ensured measurement in these areas. The last test to establish the quality of case study research is reliability. Although the study of binge eating disorder using the homeopathic similimum is limited, a previous study conducted on females yielded good results (Jacobs, Mistry, & Henn, 2002). This contributes to the external reliability of this type of study (Yin, 2014). Descriptive studies, like case studies and case series, help to generate hypotheses and therefore larger case studies need to be conducted in order to assure reliability (Saxena, Prakash, Acharya, & Nigam, 2013).
With regard to internal reliability, the same researcher conducted all interviews and the same protocol was followed for each interview, thus preventing bias. All cases were also overseen by the same supervising clinician to ensure reliability. In addition, the researcher did not include any other treatment regimes, including the omittance of any advice regarding dietary habit or lifestyle changes.
2.4. Data analysis
The data gathered from the binge-eating scale (BES), was evaluated alongside the self-monitoring binge-eating calendar. This was used in conjunction with the observational qualitative data gained from the consultations to assess each participant's progress over the course of the nine-week study.
2.5. Ethical considerations
This research study was given clearance by both the University of Johannesburg (UJ) Faculty of Health Sciences Higher Degrees committee (HDC05/02-10) and the Academic Ethics Committee (AEC05/02-10), who report to the National Health Research Ethics Council of South Africa. The study was conducted at the Homeopathy Health Training Centre, Doornfontein campus, University of Johannesburg (UJ), South Africa. There were no anticipated risks to the study. All participants were assured of privacy, confidentiality and anonymity, and were informed of their right to withdraw from the study at any time.
3. Theory
3.1. Binge eating
Patients with eating disorders typically experience subjective distress regarding their eating patterns (American Psychiatric Association, 2013), and body image (Hay, 2013). To date, BN is more commonly seen in females, whereas BED is equally prevalent in both genders (Hay, 2013). The diagnostic criteria for eating disorders has recently been updated in the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (American Psychiatric Association, 2013), providing more sex-neutral diagnostic criteria for eating disorders (Raevuori, Keski-Rahkonen, & Hoek, 2014).
Risk factors for developing an eating disorder are diverse, and include hereditary psychological factors (such as negative affect, disturbances in mood, body dissatisfaction, and compulsive and impulsive behaviours), physical characteristics (obesity) and environmental factors such as adverse life experiences (trauma, abuse) (Andrés and Saldaña, 2014, Bello et al., 2014 and Hay, 2013). Stressful life situations also contribute to cravings for highly palatable foods; these foods reduce perceived feelings of stress and elevate mood by blunting the response of the hypothalamo-pituitary-adrenal (HPA) axis to stress (Bello et al., 2014, Dallman, 2010 and Rosenberg et al., 2013). "Food addiction" is another common feature related to disordered eating and obesity. Addictive-like eating is associated with elevated body mass index (BMI), weight fluctuation, and disordered eating patterns (Gearhardt, Boswell, & White, 2014). Indulging in these "comfort" foods results in the formation of compulsive stress-induced feeding behaviours; susceptible patients then learn to "self soothe" with food rather than develop problem-solving skills and strategies to cope with daily stressors (Dallman, 2010). Dieting, due to dissatisfaction in body weight and shape, is also a risk factor for the development of binge eating and can result in obesity and eating disorders (Andrés & Saldaña, 2014).
Currently, it is estimated that males make up roughly 10% of all clinical cases of established eating disturbances, with epidemiological studies suggesting as high a ratio as one case in six being male. BED differs in this respect, in that the male to female ratio approaches one-to-one (Fairburn and Brownell, 2002 and Striegel-Moore and Smolak, 2002). The similarities of symptoms between male and female sufferers of disordered eating run a close parallel, but one major difference is the shift of emphasis in males from body weight to body shape. In this regard, men can be considered to be more at risk of atypical eating disorders, as diagnostic criteria of established eating disorders favours an emphasis on body weight, so that the diagnosis of eating disorders may currently be skewed towards identifying female sufferers. Complicating the scenario is the likely reluctance of men to seek out help for what is traditionally viewed as a female problem (Birmingham and Treasure, 2010 and Palmer, 2000).
Current conventional treatment options for eating disorders include cognitive behavioural therapy (CBT), interpersonal psychotherapy (ITP), and selective serotonin reuptake inhibitors (SSRIs). Cognitive behavioural therapy and ITP have been found to assist in reducing binge eating episodes and improve psychosocial symptoms, however have little effect on reducing weight (Hay, 2013, Wilson, 2011 and Wilson et al., 2007). SSRIs, such as fluoxetine, have been investigated as adjunctive and stand-alone therapies. Randomised controlled trials (RCTs) have produced mixed results (Reas & Grilo, 2008), and there have also been no long-term studies evaluating the safety and efficacy of these drugs (Wilson, 2011). No single medication has received approval from a regulatory body for use in binge eating. The studies around binging have many limitations. SSRIs have shown greater rates of reduction in targeting binge eating, psychiatric, and weight symptoms than placebo; however, most weight reductions would not be considered clinically significant (McElroy et al., 2012). Despite these treatment options, less than half of chronic cases seek treatment (Kessler et al., 2013). Complicating the scenario is that treatment resistance is a common feature of eating disorders, as documented by poor response rates in many treatment trials (Halmi, 2013).
3.2. Individualised homeopathic treatment
Individualised homeopathic treatment starts with an in-depth case taking interview with the patient taking into consideration physical, mental and emotional symptoms - in-depth case taking is an integral part of homoeopathic practice and is the method of data collection from which a prescription can be made (De Schepper, 2010). The detail of the case assists the practitioner in finding the similimum remedy, while the patient-centered nature of the consultation validates and empowers patients. This tends to have therapeutic and positive effects on subjective outcome measures, as does disclosure of emotional experiences by the patient themselves. The positive outcomes of homeopathic treatment are proposed to be due to the synergistic combination of the remedy and the consultation itself (Eyles et al., 2011, Van Dulmen and Bensing, 2002 and Verhoef et al., 2005). This complex interaction would ideally be assessed best using Whole Systems Research, which equally values both subjective and objective measures, as was used in the current study, because no one method can fully evaluate the outcomes of homeopathic treatment (Verhoef et al., 2005).
Case taking is followed by case analysis and repertorisation, by either a manual book repertory or a computer repertory (Bloch and Lewis, 2003, De Schepper, 2010 and Subramanian and Subramanian, 2004). Repertorisation yields a variety of remedy options. The remedy which is most common throughout the selected repertory symptoms, suits the patient the best, and encompasses all of the patient's symptoms, is then prescribed (Bloch and Lewis, 2003 and Watson, 2009). This is the similimum remedy for the patient and the presenting case.
In a qualitative study conducted on the use of homeopathy in eating disorders, homeopathic practitioners showed that patients with long-standing subclinical eating disorders were more difficult to treat and required more rigorous management than patients with eating disorders that were of recent onset. Homeopathic treatment was also demonstrated to prevent the development of eating disorders in other cases (Dehn, 2012). In addition to the remedy that is given, the extended benefits of homeopathy as a treatment option for binge eaters may include the following: (i) the nature of the homeopathic consultation is therapeutic in itself (Brien, Lachance, Prescott, McDermott, & Lewith, 2011); (ii) the relationship that develops between a doctor and a patient may assist in encouraging and empowering patients to continue with the treatment; and (iii) the aim of homoeopathic treatment is to treat patients holistically, on a mental, emotional and physical level, while also taking contributing factors and the aetiology of the condition into account (Dehn, 2012).
4. Results and findings
There were 15 initial candidates, of which four were excluded on the basis of gender, age or not meeting the minimum inclusion criteria. One of the 11 remaining participants elected to leave the study after the first interview, citing the location as inconvenient. Ten Caucasian male participants between the ages of 23 and 42 years participated in this study. Presented here are four of the ten case histories to illustrate the diversity of symptom presentation in binge eating. It is noteworthy that case analysis and repertorising was based on the entire symptom picture in each case, and not limited to only the participant's binge eating symptoms.
4.1. Case one
A 28-year-old musician presented with irregular eating and sleeping patterns.
He has a history of eating beyond satiety reaching back to his childhood memories, and has a habit of eating at an accelerated pace, sometimes reaching a "frenzy" of eating. The participant expresses late-night cravings for sweet, rich foods. He experiences hunger pangs, increased salivation and slight nervousness in his chest region preceding a meal, a sensation of being bloated after eating. He describes himself as a highly strung, nervous person, and boredom often leads to eating.
On further questioning, the participant revealed a long-standing history of erratic sleeping patterns. He sleeps for approximately nine hours, consisting of a deep, heavy sleep. His sleep is characterised by a tendency to frequently change positions, and he will often feel tired for hours after waking from an extended period of rest. The participant has some residual anxiety over sleep, and he perceives it as a major problem.
He sometimes experiences slight dizziness, accompanied by a hot, flushed sensation and the feeling that his body is pushing out of his skin. He also complains of an occasional burning sensation when passing stool, and has a history of rectal spasms. The participant also complains of an itching of the skin around his buttocks. On examination, he presented with fine, visible tremors of the hands.
4.1.1. Repertorisation
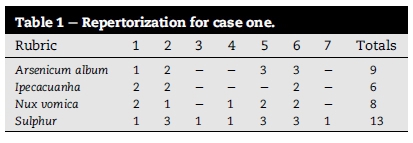
The following rubrics were used in the repertorization for case one (refer to Table 1): Rubrics (Murphy, 1998).
1. Food, eating, fast (Eliminator)
2. Food, sweets, desires (Eliminator)
3. Food, appetite, increased at night
4. Sleep, heavy sleep
5. Nerves, trembling, external
6. Skin, itching
7. Mouth, salivation, eating on, beginning,
4.1.2. Prescription
Sulphur LM1, taken once daily, was prescribed.
4.1.3. Motivation for remedy selection
The following symptoms indicate the remedy Sulphur in the Materia Medica: accelerated pace of eating, increased appetite at night, intense desire for sweets, anxious sensation in the chest, a sensation of tension and fullness in the abdomen, burning pain when passing stool, itchy skin, and sleepiness during the day with an increased alertness at night ( Vermeulen, 2000).
4.1.4. Follow up consultations
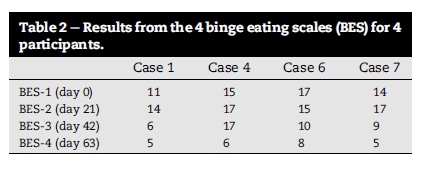
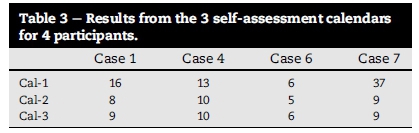
At the follow up consultations, the participant reported a spreading rash from the nates, which subsequently cleared up. His eating pace stabilised, and he no longer experienced the sensation of rushing his meal down. His binge eating severity, as measured by the BES, also decreased from 11 to 14 at the initial and second consultations (during the baseline period), to 6 and 5 at the third and fourth consultations (Table 2). His cravings decreased, he ate less and felt that he had a healthy appetite. There was a decreasing trend in his self-monitored binging frequency from 16 at baseline, to 8 and 9 at the third and fourth consultations respectively (Table 3). In addition, his quality of sleep improved, and the intensity of his rectal spasm decreased. The participant's eating patterns remained improved for the duration of the study and there was a decreasing trend in both his binging frequency as well severity, as measured by the BES.
4.2. Case four
A 35-year-old consultant presented with a history of periodically feeling out of control over his eating habits.
Since his childhood he has associated food with a sense of consolation and comfort, and he used to have a tendency to snack regularly throughout the day. He leads a sedentary lifestyle and feels overweight. His binges are preceded by a hollow sensation in the stomach, and a tickling sensation in his throat, with a feeling that he needs to experience interesting and satisfying textures while swallowing. He will seldom eat to physical discomfort, but will experience sleepiness afterwards. He rarely feels guilt after binging, but will experience a sense of regret prior to and after binging, and is consciously aware that his eating pattern or time of eating is inappropriate. He considers his diet as healthy overall, except for his late night binges. He has cravings for bread, starchy foods and salt, and is averse to offal; and generally he is feels better for eating.
The participant also revealed a proclivity for mountainous regions; he dislikes the heat, and avoids the sun, preferring cold, cloudy weather. He also has a suppressed libido, melancholy and an emotional attachment to romantic relationships that have ended. The participant is concerned over some hair loss on his head during the last two years.
4.2.1. Repertorisation
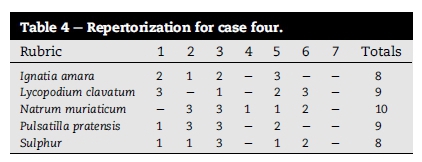
The following rubrics were used in the repertorization for case four (refer to Table 4): Rubrics (Murphy, 1998).
1. Food, appetite, hunger, at night (Eliminator)
2. Environment, sunlight, aggravates (Eliminator)
3. Mind, melancholy
4. Mind, objective, reasonable
5. Food, eating, ameliorates
6. Food, starchy food, desires
7. Constitution, hair loss, from head
4.2.2. Prescription
Natrum muriaticum LM1, taken once daily, was prescribed.
4.2.3. Motivation for remedy selection
The following symptoms indicate the remedy N. muriaticum in the Materia Medica: sensitivity to the sun, a craving for salt and farinaceous foods with an aversion to meat, a melancholic disposition and ailments from disappointed love ( Murphy, 1998).
4.2.4. Follow up consultations
After prescribing a daily dose of N. muriaticum LM1, the participant experienced a marked decrease in his late night eating. He was eating more regular meals, his appetite sated earlier, and he was able to decline second helpings of food. The frequency and intensity of his craving decreased, as seen in both the BES, where scores changed from 15 to 17 at baseline to 6 at the final consultation ( Table 2), and the self-assessment calendar, where his scores changed from 13 at baseline to 10 at the final consultation (Table 3). In general, he reported sleeping better, a return of his libido, and a lightening of his emotional state - he felt more assertive and confident in his professional and personal capacity.
4.3. Case six
A 23-year-old journalist presented with a dietary habit of eating the majority of his food at night. The participant's appetite is very low in the mornings, and only increases during the day as a result of boredom, without the physical sensation of hunger. At night, he tend to be hungrier, and after eating a meal, becomes even hungrier. He especially craves pasta. During a binging episode, he would binge throughout the day, leaving him with physical discomfort and regret afterwards.
He describes himself as a thirsty person, and avoids the sun whenever possible. His sleeping is erratic, and he often wakes up unrefreshed. Over the weekends he tends to indulge in inordinate amounts of alcohol. He has a history of recurring sinusitis with accompanying headaches extending to his right eye.
It is noteworthy that the participant seemed reticent to disclose information freely, and asked many questions about the prescribed remedy and its possible side effects.
4.3.1. Repertorisation
The following rubrics were used in the repertorization for case six (refer to Table 5): Rubrics (Murphy, 1998).
1. Food, appetite, hunger, at night (Eliminator)
2. Food, farinaceous, desires
3. Food, alcohol, desires
4. Mind, indolence, eating, after
5. Food, appetite, loss, morning
6. Environment, sunlight, aggravates
7. Skin, rough skin (as noted on physical examination)
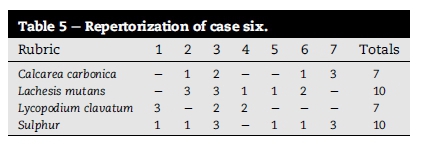
4.3.2. Prescription
Lachesis mutans LM1, taken once daily, was prescribed.
4.3.3. Motivation for remedy selection
The following symptoms indicate the remedy L. mutans in the Materia Medica: a craving for farinaceous foods, alcohol and narcotics, a loss of appetite in the mornings, restless sleep with difficulty waking, a general aggravation from sunlight and a characteristic right-sided headache ( Murphy, 1998;Vermeulen, 2000).
4.3.4. Follow up consultations
After a daily prescription of L. mutans LM1, the participant spontaneously decided to incorporate breakfast to his routine. His appetite had stabilised, and he felt that he was able to control his urges to overeat more easily. The score for the BES remained constant at 17 and 15 during the baseline period ( Table 2), and then decreased to 6 at the final consultation. The binges remained relatively unchanged in number as reported in the self-assessment calendars where his scores were 6, 5 and 6 at baseline, and the third and fourth consultations respectively (Table 3). Although his frequency of binging didn't improve, the severity of his binging episodes showed a marked improvement. The participant reported an increase in the quality of his sleep, allowing him to wake refreshed in the mornings. He also reported a decreased sensitivity to the sun.
4.4. Case seven
A 29-year-old editor presented with erratic eating patterns. He says that he finds eating boring, and dislikes it. The participant often skips breakfast, and opts for convenient options, such as toasted sandwiches or pizza. The participant drinks ten to fourteen cups of coffee or cola per day, and his coffee has to be very milky. He loves drinking milk and will consume two liters of milk in two days. If a cup of cooling, milky coffee or tea is not nearby, he feels that something is missing. He drinks his milk cold, and finds that it relaxes him. When he binges, it is usually in the afternoon after work. He eats on average two boxes of chocolate biscuits and three slabs of milk chocolate per week. He feels that he would be "physically incapable" of drinking water. He prefers bland food, and dislikes spicy, salty, exotic or slimy textured food.
The participant has a good level of energy, depending on how engaged he is with work. He easily perspires on his head, sides and back, on slight exertion. He is industrious in his free time and pursues many creative hobbies such as writing, painting and playing games with his friends. He dislikes being unproductive.
4.4.1. Repertorisation
The following rubrics were used in the repertorization for case seven (refer to Table 6): Rubrics (Murphy, 1998).
1. Food, milk, desires (Eliminator)
2. Food, appetite, relish, without
3. Perspiration, exertion, during slight
4. Food, salt, aversion to
5. Food, coffee, desires
6. Food, drinks, water, aggravates
7. Food, cold drinks, desires
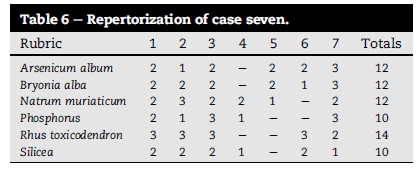
4.4.2. Prescription
Rhus toxicodendron LM1, taken once daily, was prescribed.
4.4.3. Motivation for remedy selection
The following symptoms indicate the remedy R. toxicodendron in the Materia Medica: industrious nature, a strong desire for cold milk, a want of appetite and an aversion to drinking water ( Murphy, 1998).
4.4.4. Follow up consultations
After prescribing a daily dose of R. toxicodendron LM1, the participant reported that his cravings had decreased by the third consultation, and disappeared at the final consultation, and he had stopped his milk intake. He was also able to resist his urges to binge and slowed his eating pace. The results of the BES showed a decrease in the intensity of binging from 14 to 17 at baseline, to 5 at the final consultation ( Table 2). The self-assessment calendar showed a dramatic improvement from 37 at baseline, to 9 at the end of the study (Table 3). He has spontaneously adopted a healthy dietary regime. Additionally, he reported an improved quality of sleep, a decrease in excessive levels of perspiration, and a new awareness and appreciation of his thirst sensation.
5. Discussion
It was hypothesised the individualised homeopathic treatment would have a beneficial effect on reducing the frequency and severity of bingeing episodes. In this study, participants exhibiting binge eating symptoms were recruited. The case study design allowed for qualitative data to be collected. It is noteworthy that all of the participants involved in the study were Caucasian, from similar socio-economic backgrounds, and in close proximity to each other. In many of the cases there was a concurrent disturbance in the participant's sleeping patterns. The diagnosis of an eating disorder was beyond the scope of this study, but it was interesting to note the overlap of symptoms from binge eating disorder (BED) and night eating syndrome (NES). Where possible, the researcher endeavoured to maintain the remedy initially prescribed, but in two of the cases (cases two and eight), there was a change in prescription at the third consultation in an attempt to best match the participants' total symptom picture at that time.
This study has contributed to our knowledge on the use of individualised homeopathic treatment for binge eating in adults. It serves to open up the field for further studies to be conducted on patients suffering from eating disorders characterised by binge eating. This research highlights the potential therapeutic benefits of homeopathy as an adjunctive or complementary treatment option, which may be of great value to health practitioners, caregivers and eating disorder sufferers. In total, eight different remedies were prescribed, of which three remedies were prescribed twice (N. muriaticum, Phosphorus, and Sulphur), and five remedies were prescribed once (Arsenicum album, Aurum metallicum, Delphinium staphysagria, L. mutans and R. toxicodendron). At the study's conclusion, all of the participants reported a decrease in the frequency and severity of their binge eating to a greater or lesser extent. Most participants experienced a concurrent improvement in other aspects of their health, such as their sleeping habits, libido, blood pressure, their level of confidence, and/or an overall sense of wellbeing. Statistical analysis of the participants' measured results confirms a significant improvement in both binging frequency and severity after similimum treatment.
5.1. Limitations of the study and recommendations
This small-scale, single group study had many limitations, mainly related to the small sample size, sample diversity and the duration of the study. In order to evaluate the long-term efficacy and sustainability of homeopathic treatment for this condition, double-blind, placebo-controlled trials should be conducted, with a larger sample group and over an extended time period. Future research may also assess the efficacy of homeopathic treatment in a more diverse population sample which includes both males and females, and people of different races and social-economic backgrounds, to assess differences in the response to treatment, if any. Comparing the overall efficacy of homeopathic similimum treatment on binge eating to that of counselling, and to that of a combination of both homeopathy and counselling in tandem, would also be of value. In an attempt to minimise treatment variables, only one potency of treatment was selected in this study. A true similimum prescription should also consider the selection of the most appropriate potency as well as the frequency of administration of the remedy when matching the totality of the case. It is also recommended that future studies assess body weight and body mass index of participants, before and after treatment, as this will allow for a more objective analysis of the treatment.
6. Conclusion
This study shows the potential benefits of individualised homeopathic treatment in binge eating in males which lead to a decrease in both the frequency and severity of binging episodes. The varied nature of the prescriptions indicates the highly individual manifestation of binge eating. Follow-up studies are recommended to explore this treatment modality as a complementary therapeutic option in eating disorders characterised by binge eating.
Acknowledgements
This work was financed and supported by the University of Johannesburg. The contents of this work are solely the responsibility of the authors and do not represent the official views of UJ.
References
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.) Washington, DC.: Author. [ Links ]
Andrés, A., & Saldaña, C. (2014). Body dissatisfaction and dietary restraint influence binge eating behavior. Nutrition Research. http://dx.doi.org/10.1016/j.nutres.2014.09.003. Advance online publication. 16(ii), S0271e5317(14) 00173-0. [ Links ]
Bello, N. T., Yeh, C. Y., Verpeut, J. L., & Walters, A. L. (2014). Bingelike eating attenuates Nisoxetine feeding suppression, stress activation, and brain norepinephrine activity. PLoS ONE, 9(4), e93610. [ Links ]
Birmingham, C. L., & Treasure, J. (2010). Medical management of eating disorders (2nd ed.). UK: Cambridge University Press. pp. 4, 99, 173, 183, 187. [ Links ]
Bloch, R., & Lewis, B. (2003). Homoeopathy for the home. Cape Town: Struik Publishers. [ Links ]
Brien, S., Lachance, L., Prescott, P., McDermott, C., & Lewith, G. (2011). Homeopathy has clinical benefits in rheumatoid arthritis patients that are attributable to the consultation process but not the homeopathic remedy: A randomized controlled clinical trial. Rheumatology, 50(6), 1070-1082. [ Links ]
Colton, P., Rodin, G., Bergenstal, R., & Parkin, C. (2009). Eating disorders and diabetes: Introduction and overview. Diabetes Spectrum, 22(3), 138-142. [ Links ]
Dallman, M. F. (2010). Stress-induced obesity and the emotional nervous system. Trends Endocrinology Metabolism, 21(3), 159-165. [ Links ]
De Schepper, L. (2010). Hahnemannian textbook of classical homeopathy for the professional. India: B. Jain. [ Links ]
De Schepper, L. (2011). Achieving and maintaining the similimum (4th ed.). India: B. Jain. [ Links ]
Dehn, K. (2012). A qualitative enquiry into the use of homeopathy for eating disorders: The homeopath's perspective. Hpathy Ezine. Retrieved from: http://hpathy.com/homeopathy-papers/a-qualitative-enquiry-into-the-use-of-homeopathy-foreating-disorders-the-homeopaths-perspective/. [ Links ] [ Links ]
Fairburn, C. G., & Brownell, K. D. (2002). Eating disorders and obesity. USA: The Guilford Press. pp. 99-101, 142, 160, 172-176, 178-181, 189/190, 249, 254, 350-352, 354-356. [ Links ]
Feingold, E. (2005). Treating people with eating disorders with homeopathy. American Journal of Homeopathic Medicine, 98(3), 174-178. [ Links ]
Feingold, E. (2006). Treating obesity with homeopathy. American Journal of Homeopathic Medicine, 99(2), 138-143. [ Links ]
Fishman, D. B. (2012). The pragmatic case study method for creating rigorous and systematic, practitioner-friendly research. Pragmatic Case Studies in Psychotherapy, 9(4), 403-425. [ Links ]
Fixsen, A. (2006). My parents weren't interested in what I felt. The Homeopath, 25(1), 27-31. [ Links ]
Gearhardt, A. N., Boswell, R. G., & White, M. A. (2014). The association of "food addiction" with disordered eating and body mass index. Eating Behaviours, 15(3), 427-433. http://dx.doi.org/10.1016/j.eatbeh.2014.05.001. [ Links ]
Halmi, K. A. (2013). Perplexities of treatment resistance in eating disorders. BMC Psychiatry, 13, 292. [ Links ]
Hay, P. J. (2013). Assessment and management of eating disorders: An update. Australian Prescriber, 36, 154-157. [ Links ]
Herrin, M. (2003). Nutrition counseling in the treatment of eating disorders. USA: Brunner-Routledge. [ Links ]
Hilbert, A. (2013). Cognitive-behavioral therapy for binge eating disorder in adolescents: Study protocol for a randomized controlled trial. Trials, 14, 312. [ Links ]
Jacobs, T., Mistry, R., & Henn, C. (2002). The effect of the homoeopathic similimum in binge eating disorder. South Africa: The Technikon Witwatersrand (Unpublished dissertation), pp 49, 50, 137-139. [ Links ]
Kayne, S. B. (Ed.). (2008). Homeopathic practice. London: Pharmaceutical Press. pp. 1-5, 63-73, 124. [ Links ]
Kayne, L. R., & Kayne, S. B. (2007). Homeopathic prescribing. London: Pharmaceutical Press. pp. 3e8, 11-31. [ Links ]
Kessler, R. C., Berglund, P. A., Chiu, W. T., Deitz, A. C., Hudson, J. I., Shahly, V., et al. (2013). The prevalence and correlates of binge eating disorder in the world health organization world mental health surveys. Biological Psychiatry, 73(9), 904-914. [ Links ]
Lee-Jen Wu, S., Hui-Man, H., & Hao-Hsien, L. (2012). A comparison of convenience sampling and purposive sampling. Journal of Nursing, 59(2), 105-111. [ Links ]
Maslan, A. (2006). The homeopathic treatment of eating disorders. Retrieved from: http://www.homeopathicwellness.com/articles/article1.html. [ Links ]
McElroy, S. L., Guerdjikova, A. I., Mori, N., & O'Melia, A. M. (2012). Current pharmacotherapy options for bulimianervosaand binge eating disorder. ExpertOpinion on Pharmacotherapy, 13, 2015e2026. [ Links ]
Murphy, R. (1998). Homoeopathic medical repertory. India: B Jain. [ Links ]
Owen, D. K. (2015). Local prescribing and repertorisation. London: Singing Dragon. [ Links ]
Palmer, B. (2000). Helping people with eating disorders. UK: Wiley & Sons, Ltd. [ Links ]
Raevuori, A. I., Keski-Rahkonen, A., & Hoek, H. W. (2014). A review of eating disorders in males. Current Opinion Psychiatry, 27(6), 426-430. [ Links ]
Reas, D. L., & Grilo, C. M. (2008). Review and meta-analysis of pharmacotherapy for binge-eating disorder. Obesity, 16, 2024-2038. [ Links ]
Rosenberg, N., Bloch, M., Ben Avi, I., Rouach, V., Schreiber, S., Stern, N., et al. (2013). Cortisol response and desire to binge following psychological stress: Comparison between obese subjects with and without binge eating disorder. Psychiatry Research, 208(2), 156-161. [ Links ]
Saxena, P., Prakash, A., Acharya, A. S., & Nigam, A. (2013). Selecting a study design for research. Indian Journal of Medical Specialities, 4(2), 334-339. [ Links ]
Striegel-Moore, R. H., & Smolak, L. (2002). Eating disorders e Innovative directions in research and practice. USA: American Psychological Association. pp. 38/39, 53-59, 92-92, 203. [ Links ]
Subramanian, R., & Subramanian, R. (2004). Textbook of homeopathic philosophy. India: B. Jain. [ Links ]
Traub, G. (2006). Eating disorders. Retrieved from: http://www.homeopathycenter.org/homeopathy-today/novemberdecember-2006/denver-host-joint-homeopathicconference. [ Links ]
Tree, J. (2007). The empty addict: Eating disorders in children. The Homeopath, 26(1), 21-24. [ Links ]
Van Dulmen, A. M., & Bensing, J. M. (2002). Health promoting effects of the physician-patient encounter. Psychology, Health & Medicine, 7(3), 289-300. [ Links ]
Verhoef, M. J., Lewith, G., Ritenbaugh, C., Boon, H., Fleishman, S., & Leis, A. (2005). Complementary and alternative medicine whole systems research: Beyond identification of inadequacies of the RCT. Complementary Therapies Medicine, 13, 206-212. [ Links ]
Vermeulen, F. (2000). Concordant materia medica. Netherlands: Emryss. [ Links ]
Watson, I. (2009). Repertorisation. Retrieved from: http://hpathy.com/homeopathy-repertory/repertorisation/. [ Links ]
Wilson, G. T. (2011). Treatment of binge eating disorder. Psychiatric Clinics of North America, 34(4), 773-783. [ Links ]
Wilson, G. T., Grilo, C. M., & Vitousek, K. M. (2007). Psychological treatments of eating disorders. American Psychologist, 62, 199-216. [ Links ]
Yin, R. (2014). Case study research: Design and methods (5th ed.). Los Angeles: Sage. [ Links ]
Received 7 August 2015
Accepted 30 June 2016
Available online 12 August 2016
* Corresponding author. Department of Homoeopathy, University of Johannesburg, P.O. Box 17011, Doornfontein, Johannesburg, Gauteng 2028, South Africa. Fax: +27 11 559 6117.
E-mail addresses: radmilar@uj.ac.za (R. Razlog), jpellow@uj.ac.za (J. Pellow), rpatel@uj.ac.za (R. Patel), mcaminsky@uj.ac.za
Peer review under responsibility of Johannesburg University.














