Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Health SA Gesondheid (Online)
versión On-line ISSN 2071-9736
versión impresa ISSN 1025-9848
Health SA Gesondheid (Online) vol.21 no.1 Cape Town 2016
http://dx.doi.org/10.1016/j.hsag.2016.04.001
FULL LENGTH ARTICLE
Professional nurses' understanding of clinical judgement: A contextual inquiry
Anna C. van GraanI, *; Martha J.S. WilliamsI; Magdalena P. KoenII
ISchool of Nursing Science, North-West University (Potchefstroom Campus), South Africa
IISchool of Nursing Science, North-West University (Mafikeng Campus), South Africa
ABSTRACT
Higher cognitive skills are essential competencies for nurses joining the technologically and increasingly complex health care environment to provide safe and effective nursing care. Educators and clinical facilitators have recognised that newly qualified nurses do not meet the expectations for entry level clinical judgement and are held accountable for finding adequate learning experiences as preparation for such practice demands. An explorative and descriptive qualitative design was followed in this study to reach an understanding of clinical judgement in the clinical nursing environment from the perspective of professional nurses. Eleven professional nurses (n = 11) working at primary health care clinics, public and private hospitals participated voluntarily. Data was collected by means of the "World Café" method, incorporating a combination of techniques such as interviewing, discussions, drawings, narratives and reflection. The focus was on professional nurses' knowledge of the meaning of clinical judgement and factors influencing the development of clinical judgement in the clinical environment. Qualitative thematic content analysis principles were applied during data analysis. The findings were integrated with the relevant literature to culminate in conclusions that should add to the knowledge base of clinical judgement as an essential skill for improving autonomous and accountable nursing care.
Keywords: Clinical nursing environment; Cognitive reasoning skills; Quality nursing care; Nursing student
1. Introduction
People frequently get sick and everybody has experienced nursing care at some stage, and yet in the 21st century Nursing is still difficult to describe and poorly understood. Some people associate nursing with the physical tasks concerned with keeping the sick person safe, comfortable, nourished and clean. Some view nursing as assisting the doctor by carrying out tasks associated with medical treatment. These descriptions are indeed part of nursing practice today. Sound research evidence demonstrates that skilled nursing care makes the difference from early versions of nursing (Royal College of Nursing, 2003:4) The more experienced a nurse is in what she does the less likely the patient may be to recognize what specific interventions been done. There for nursing care provided by skilled professional nurses be different from that of non-professional care givers.
The distinction of nursing care by professional nurses lies in the clinical judgement inherent in the processes of assessment, diagnosis, implementation and evaluation. Knowledge forms the basis of the patient needs assessment and determines the action to meet these needs; professional accountability for decisions and actions, including the decision to delegate to co-workers and the structured nurse-patient relationship, which incorporates the professional code of ethics and SANC regulation's (RCN, 2003:4-6).
2. Focus and background of the study
Today's clinical nursing environment is more complex than ever before. As a rapidly advancing profession, nursing demands higher cognitive skills from nurses. Critical creative thinking and clinical judgement is viewed as essential skills for every health professional (Potgieter, 2012:4). Nighthingale (1992) firmly established observations and its interpretation as hallmarks for trained nursing practice (Lin, Hsu, & Tasy, 2003:159). In recent years, clinical judgement in nursing has become synonymous with the nursing process model of practice viewed as a problem solving activity. The nursing process has dominated nursing education since the 1960's as theorists tried to link their theories with the clinical judgement process and to link nursing theory with clinical practice. Studies by Tanner (2006:205) and Higuchi and Donald (2002:146) indicate that teaching only one type of problem solving, such as the nursing process, fails to adequately describe the process needed for nursing judgement and to account for the complexity of factors influencing clinical judgement.
The mentioned need for thinking skills in nursing has been accentuated in response to the constantly and rapidly changing health care environments. As the acuity of hospitalised patients and the prevalence of chronic illnesses increase, the length of hospital stay shortens. The increased patient-nurse ratios, limited clinical facilities and shortage of nurse educators are common factors that contribute to the above mentioned (Potgieter, 2012:4).
Recent literature indicates that most newly qualified nurses do not meet the expectations for entry level clinical judgement (Pongmarutai, 2010:1). Health care institutions expect professional nurses joining the workforce to be highly competent and prepared to function in a technologically sophisticated and increasingly complex health care arena. According to (Australian Nursing and Midwifery Council, 2005 and Hammond, 1996:218) the changing demands of practice is characterised by uncertainty and despite this uncertainty, nurses still have to make clinical decisions and clinical judgements. Simply following the process, analysing the data like a computer and performing prescribed techniques cannot guarantee good clinical judgement that will solve the patient's problems (Pongmarutai, 2010:1). Clinical judgement has been recognised as a vital skill that enables nurses to determine the appropriate nursing interventions when planning patient care, especially the ability to manage rapidly deteriorating patients (Lindsey & Jenkins, 2013:64). This has produced an atmosphere in which the nurse is required to make sound accurate clinical judgements that support the complex health care and patient's needs and that contribute to optimal patient outcomes (Clark, Owen, & Tolken, 2004:550).
The remunerated community services year for newly qualified SA nurses, implemented in 2006 (SANC, 2005) led to the provision of comprehensive health care services. However, clinical educators and professional nurses have recognised that new graduates often lack the knowledge and ability to make sound clinical judgements (Tanner, 2006:207) as they have not been clinically or educationally fully prepared for the demand for health care and the greater accountability, which increases continuously (South Africa. Department of Health, 2013 and Geyer et al., 2002:11; Simpson & Courtney, 2002: 91).
Nurse educators recognise the increased demand for competent nurses in the current health care environment, and find it increasingly challenging. They are held accountable to find adequate clinical experiences to prepare students to meet the demand for the ever-changing and more acute clinical environment (Tanner, 2006:206). Limited exposure to real life patients during the education and training period leads to limited clinical practice for role taking. The newly approved nursing curriculum scheduled for implementation at all SA nursing education institutions (NEI) from 2016, reduces the minimum exposure to clinical nursing practice from 4000 to 3000 clinical hours (Department of Health, 2011).
Tanner (2006:205) accentuates the inefficient use of time in clinical teaching as one of the problems of current clinical education models. Teacher-student time is consumed by performing routine tasks, checking preparation/doing assessments and to assure that students are safe in the clinical environment. Time for more meaningful interaction to discuss students' observation of the underlying pathophysiology is limited (Randall, Tate, & Lougheed, 2007:61; Tanner, 2006:205). Students should be guided to understand patient needs, develop appropriate responses and adjust care plans on the basis of clinical reasoning and judgement. Nursing students should be able to go beyond the protocols, standards and formal rules to arrive at safe patient care that should not be entirely protocol driven (SmithBattle & Diekemper, 2001:403). Clinical decision making is facilitated when students have an opportunity to integrate scientific knowledge, experiences and clinical judgement in a specific situation (Benner, Tanner, & Chesla, 2009). Such opportunities guide nursing students to a deeper understanding of the clinical situation and allow them to progress from reliance on abstract knowledge and context free formal rules for nursing care to deep knowledge. They then learn to rely on past personal experiences as basis for clinical decision making and notice unique aspects that reflect understanding of salience, as well as the influence of the clinical context (Benner, 2001:210; Tanner, 2006:206). Potgieter (2012:5) adds to the above that didactic lectures, memorisation and simulation of demonstrations may lead to mastery, but they do not stimulate the development of critical thinking skills and ethical values for care. Frith and Clark (2013:7), as well as Maskey (2008:12) accentuate the fact that a student's performance depends on the knowledge, skills and attitudes accumulated during their training and the student's ethics and value system can only be assessed on observable behaviours.
Chisari (2009:18) and SANC (2005) indicate that collaborative dialogue between students, educators and clinical mentors as role models during nurse-patient interaction is a powerful learning tool in facilitating clinical judgement. The mentioned action can help students to move from dependence to self-direction (Bruce, Klopper, & Mellish, 2011:97, 365; Chan, 2004:665) within the clinical environment as ideal for active student learning (Quinn & Hughes, 2009:341). Nurses need to think critically, self-critique, synthesise information, link concepts and become self-directed, reflective, life-long learners (Facione, 2006:10; Potgieter, 2012:5). Nursing education curricula therefore have to change from a content focus to a concept based focus.
The importance and need for an increased attempt to facilitate clinical judgement is evident.
2.1. Central theoretical statement
This study explores the clarity on the meaning of the concept clinical judgement within the South African nursing environment in two phases. The first phase of this study comprised a concept analysis of the concept clinical judgement. This second phase explores clinical judgement from the perspective of professional nurses within a specific contextual, clinical nursing environment where undergraduate nursing students are placed for clinical experience. The following objectives guided this study:
The aim of this study was to explore clinical judgement from the perspective of professional nurses within a specific, clinical nursing environment where undergraduate nursing students are placed for clinical experience.
3. Research methods
3.1. Research approach
An explorative, descriptive qualitative design was followed to gain an understanding of the participants' (professional nurses) perception of clinical judgement within the South African clinical nursing environment.
3.2. Population, sampling and research setting
The population comprised of professional nurses who complied with the selection criteria working at eight primary health care clinics, three public and two private hospitals in the Matlosana and Tlokwe sub-districts of the Dr. Kenneth Kaunda district, North-West Province, where undergraduate nursing students are placed during practice for role taking.
A purposive sampling method was used in this qualitative research because the participants were selected to fit particular features of interest to the research study ( Bothma, Greeff, Malaudzi, & Wright, 2010:201; Burns & Grove, 2009:344). Eleven professional nurses voluntarily took part in data collection (n = 11).
The "World Café" method was used to collect data from the participating professional nurses (The World Café, 2008). The method employs seven design principles namely setting the context, creating a hospitable space, exploring questions that matter, encouraging everyone's participation, connecting diverse perspectives, listening together for patterns and insights and sharing collective discoveries (Du Plessis, Koen, & Bester, 2012). The World Café method is a combination of qualitative data collection techniques, such as interviewing, discussion, drawings and narratives, and allows time for reflection (Du Plessis et al., 2012). This method is a brainstorming tool to generate ideas and comments, a living network of conversations used for leading collaborative dialogue, sharing knowledge and creating possibilities for action (Brown, 2005:2). As qualitative data collection technique this method was appropriate and effective to collect a large quantity of rich data about clinical judgement as specific topic in this research within a short period of time.
At each table an experienced researcher acted as table host and facilitator. Participants were welcomed and a question was introduced for exploration and discussion. Questioning centred on the following phrases:
• Explore and describe the meaning, characteristics and process of clinical judgement; and
• Explore and describe factors that influence the development of clinical judgement within the clinical nursing environment.
Facilitation strategies were applied to stimulate discussion and achieve the set objectives. After 15 min the session was concluded and the participants moved to the next table. The facilitators took notes of what was said by the previous group and shared it with the new group for participants to relate to the ideas, add new ones and to prevent unnecessary repetition. The result is that each facilitator managed the exploration and discussion of a specific, predetermined question by all the participants. Data collection was concluded with a general discussion session during which the participants reflected on the process, uncertainties were clarified and findings were summarised on flip charts to serve as evidence and field notes to enrich the data.
The data collection process was voice recorded for transcription purposes and had a duration time of 3:30 h. It included obtaining informed consent, focused discussions as data collection and concluded with the general discussion and feedback session.
3.3. Data analysis
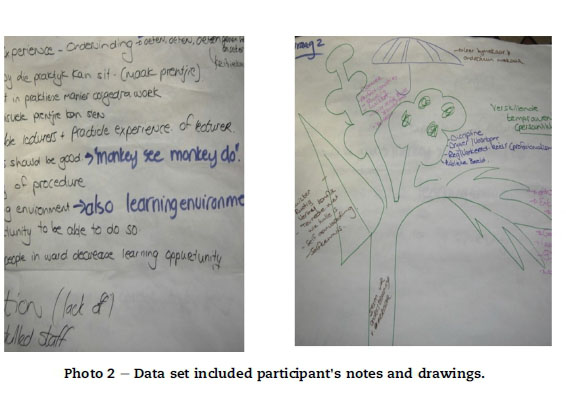
The data set included facilitators' notes, drawings by participants and the transcribed audio data of the actual discussions. Qualitative, thematic content analysis principles as described by Henning, Van Rensburg, and Smit (2004:127-129) and Du Plessis et al. (2012:770) were applied. The principles of document analysis as described by Blakeman, Samuelson, and McEvoy (2013:41) were useful during the analysis of the World Café data.
3.4. The process of data analysis
The data set was independently analysed by the researcher (coder) and a second researcher experienced in the analysis of qualitative data as co-coder. The analysis process started with a broad scanning of the data sheets for a general sense of the overall theme of clinical judgement. The data sheets were scanned a second time to identify broad themes from the main phrases. Keeping the broad themes in mind, data sheets and drawings were separately scrutinised, grouping similar words/phrases and comparing phrases with each other and with headings on the sheets to identify sub-themes. The coders engaged with the data by means of in-depth reflection not only on words, but also the use of colour and sketches (see Photo 2). The identified sub-themes were constantly compared with each other and with the main theme, clinical judgement. Related sub-themes were grouped together into themes. Data saturation was reached within each sheet as it represented the views of a group. A draft framework of themes and sub-themes was established from the data set after 3 sheets. The remaining sheets and field notes were studied to enrich and refine the themes and sub-themes.
After analysing the data separately, the researchers met to compare and discuss their findings. They reached consensus on two themes and associated sub-themes, which are discussed under Findings and Discussion.
3.5. Literature exploration and integration
The first phase of the research by Van Graan, Koen, and Williams (2014) comprised an extensive literature exploration to analyse the concept, clinical judgement in nursing. The second phase (focus of this manuscript) aimed to investigate professional nurses' understanding of clinical judgement and the factors that influences the development of clinical judgement within the clinical nursing environment. The qualitative nature of the study implies that the findings are related to and integrated with literature (Burns & Grove, 2009:12; De Vos, 2005:268) as executed under the heading Findings and Discussion.
4. Findings and discussions
The recorded data was transcribed, analysed and categorised into two (2) themes and associated sub-themes. These are described, supported by participants' responses and integrated with relevant literature to culminate in conclusions.
4.1. Theme 1: meaning of the concept clinical judgement
The participants' responses regarding the meaning of clinical judgement were categorised into sub-themes according to the four dimensions of Tanner's Clinical Judgment Model (Tanner, 2006). This model was used as framework to explain the attributes for this study as follows:
4.1.1. Effective noticing
Tanner (2006; 208) describes noticing as information gathering, which involves focused observation, searching for evidence by identifying relevant sources of patient data and recognising deviations from expected patterns, rooted in the nurse's integrated knowledge, experience, ethical perspectives and relationship with the patient.
Clinical judgement in nursing has become synonymous with the nursing process model of practice, viewed as a problem solving activity in which nurses use their critical and creative thinking skills to apply their nursing knowledge, attitudes, values and logic during patient assessment, utilising both deductive and inductive reasoning to express patient care (Chabeli, 2007:74; Mann, 2012:27; Ledesma-Delgado & Mendes, 2009:329 and Rivas, Garcia, Arenas, Lagos, & Lopez, 2012:18). Information collecting (Chitty & Black, 2011:177-179; Masters, 2005:80), involves observation and gathering of health history in evaluation of the health status of the patient and planning of holistic-prioritised care (Gotlieb, 2013:15; Pelzang, 2010:912). This assessment phase presents an opportunity for nurse-patient interaction and shared decision making to establish a therapeutic relationship (Benner et al., 2009:387; Gotlieb, 2013:205, 206; Higgs, Jones, Loftus, & Christen, 2008:27).
The participants in this study described the characteristics of clinical judgement as:
'Love and passion for the work; ...integrity; ...work to my best ability; ...decision to pull through...do the best for the patient... to walk the extra mile for your patient; ...identify a problem; ...have to listen; ...assessment of what is going on and what there is to do or manage in another way; ...use your brain to do the observations; ...use your intellect …stop to learn according the book; theory and practice needs to meet; ...experience...excellent care comes with experience; this patient has expectations... holistic approach'.
The participants' identified some of the characteristics of clinical judgement as identify a problem through assessment; to listen to the patient (patient interaction); to do the best for the patient (therapeutic relationship with the patient) and 'what there is to do or manage in another way" (planning prioritized care and problem solving); 'use your brain to do the observations' (use of knowledge and experience for observations). Evaluated against the quoted literature, the cornerstone concepts critical thinking, reasoning, values and ethical principles were omitted or not explicit mentioned. It seems as if the participants confused personal characteristics of the nurse as 'love and passion' and 'integrity' and 'excellent care' (skilled/experienced) with clinical judgement as concept.
4.1.2. Effective interpretation
Effective interpretation involves prioritising the most relevant data through reasoning, useful for explaining the patient's condition and making sense of the data by developing plans for interventions that can successfully meet the patient needs (coming to a conclusion) (Tanner, 2006). Mann (2012:27) and Benner, Hughes, and Sutphen (2008:89) view knowledge and experience as essential for interpretation and reasoning. Gerdeman, Lux, and Jacko (2013:15, 16) support Tanner's view of prioritising but accentuate the patient's condition at a given time. A few of the participants said:
'... I plan....then I implement; ...be able to anticipate what is going to happen...observe, re-assess, …prioritising of needs'
Participants didn't identify the essential meaning of effective interpretation as identification of patterns and critical thinking and the reasoning necessary to make sense of the patient's data. They viewed prioritising of patient needs and to anticipate the outcome as part of effective interpretation (Tanner, 2006 and Mann, 2012:27 and Benner et al., 2008:89).
4.1.3. Appropriate response
Tanner (2006:209) and Gerdeman et al. (2013:16) view effective responding as the process of intervening through confident and flexible decision making regarding nursing care. Lasater (2007:500, 501) and Tanner (2006:209) indicate it as interventions tailored for the individual patient, monitoring the patient's progress and adjusting treatment as indicated by the patient's response. Lasater (2007:500, 501) adds a demonstration of leadership, confidence and control over complex patient situations, delegation and direction of tasks, re-assessment and re-assurance of the patients and their families by use of effective communication.
The participants' perceptions are evident from the following quotations:
'… training and practical experience; ... give your solid ground; … you have to take charge of your patient; ... so you plan, implement,observe; ... manage according to your judgement;... professional judgement is developing with experience; ... difficult to integrate theory with practice; initiative; ...intuition.... the 'gut feeling'; ... need to look for that something extra;... the patientis the most important; ... use your knowledge; ...your decisions have to prioritise the patient's needs before other tasks; ... just two minutes you spend extra with the patient help to build a positive patient relationship, ... the patients' cooperation'.
Majority of participants view the patient him or herself and a positive relationship as important to gain the patient's cooperation in the delivering individualised nursing care. Experience and intuition flexible decision making and confident planning as indicated by ....your decisions have to prioritise the patient's needs before other tasks as indicated by their responses. No participants relate demonstration of leadership during patient care in any way to the appropriate response as revealed in literature ( Tanner, 2006:209; Gerdeman et al., 2013:16 and Lasater, 2007:500, 501).
4.1.4. Effective reflection
According to Tanner (2006:209) effective reflecting involves self-assessment of clinical performances, evaluating nursing experience and identification of strengths and weaknesses with commitment to improvement.
Several other studies (Gerdeman et al., 2013:16; Frith & Clark, 2013:112, 113; Alfaro-LeFevre, 2012:18) support reflection as the movement of thought from existing to emerging situations to gain a deeper understanding and therefore facilitate learning. Nielsen (2009:516) emphasise reflection as introspection regarding an experience. Literature identifies three types of reflection. Klopper (2009:28, 31) and Schön (1987:70) view reflection-in-action as an interactive sharing of experience and understanding (thinking while the action is taking place). Reflection-on-action refers to an evaluation of an experience ("cognitive post-mortem"), while reflection-with-action refers to interpersonal interaction to construct meaning. Klopper (2009:28) adds the making of inferences, generalisations, analogies, evaluations, problem-solving and discrimination as part of reflection. Critical thinking is therefore inherent to sound, clinical judgement.
Participants clarified their view by saying:
'You sit down and dissect the situation;.. can learn from the situation; ...after-event debriefing; ...discover how students experienced clinical learning; ...feedback help to identify misunderstandings; ...an assessment what is going on and what there is to do or manage in another way;… you as nurse will make decisions according to the patient;… decide to go on and always do the best for the patient;... you have to make an opinion; …respond according the important issues;...decide by yourself how to act; formulate outcomes and evaluate..'
Participants identified the patient and the prioritisation of his needs as the main focus. Decision-making is seen as patient-focused and not as an assessment of the strengths and weaknesses of interventions or the appropriateness of the treatment. Feedback refers to reflection as an evaluation of the situation and debriefing as an assessment of the students' experience of the clinical learning. Professional nurses see the above as a learning opportunity and problem solving activity as clarifying misunderstandings.
4.1.5. Conclusion theme 1
The participants verbalised a basic and simplistic understanding of the concept, clinical judgement in nursing. It seems as if clinical judgement is confused with good nursing care. The understanding of the relationship between a sound knowledge base, reasoning and critical thinking skills and its impact on effective interpretation and ultimately decision making, seems to be insufficient.
4.2. Theme 2: factors influencing the development of clinical judgement
The nursing practice is facing a multitude of issues that can either contribute to a positive or dysfunctional learning environment for the facilitation of clinical judgement in undergraduate students. The following factors were identified as dysfunctional for the development of clinical judgement.
4.2.1. Clinical accompaniment of nursing students
The participants describe clinical accompaniment of nursing students as problematic, inefficient and not conducive to the development and demonstration of clinical judgement.
They said: ' clinical and theory don't come together; ...practice it is not always happening as learned; ...not enough [staff] to do clinical guidance; ...no guidance; ...no time to train the juniors; ...we don't have the facts and knowledge to motivate'.
Accompaniment is described as the conscious, purposeful guidance and support of students in the clinical environment in an effort to empower them. It leads to the development of knowledge, competence and professional growth into active, critical thinkers and reflective practitioners in search of meaning (Grossman, 2007:28; Haghdoost & Shakibi, 2006:311 Quinn & Hughes, 2009:359). Meaning is described by Klopper (2009:32) as making sense of experiences within an interpersonal context. An important aspect of accompaniment is supervision, an interpersonal process during which a skilled/experienced individual (professional nurse) assists, educates and supports a less experienced person (student) to achieve professional abilities ( Carlson, Kotzé, & Van Rooyen, 2003:36). At the same time nursing students employ their newly acquired skills to the needs of patients (Cohen et al. 2007:14; Van Rooyen, Laing, & Kotzé, 2005:30). Quinn and Hughes (2009:341) accentuate learning that occurs in a real clinical setting as more meaningful than that acquired in the classroom. Nurse educators, clinical facilitators/preceptors and the professional nurses in the wards where students are placed during experiential learning should collaborate as role models to create an environment conducive to learning (Chisari, 2009:18). Students are exposed to learning opportunities (Jerlock, Falk, & Serverinsson, 2003:219), engaging in a respectful relationship grounded in ethical, personal and professional values (Beukes, Nolte, & Arries, 2010:3; Gagliardi et al., 2009:55; Straus, Chatur, & Taylor, 2009:135). Nurse educators rely greatly on professional nurses working in facilities to ensure that nursing students obtain the necessary clinical skills (Kanno & Koeske, 2010:355; Moscaritolo, 2009:19; Pinnock, Sharif, Hawke, Henning, & Jones, 2011:63). Bos, Alinaghizadeh, Saarikoski, and Kaila (2011:1785); Marshburn, Engelke and Swanson (2009:426) and Frankel (2009:5) report that financial constraints, the constant shortage of staff, heavy workloads and resources left staff frustrated and depressed, leaving them with inefficient energy and time to attend to the learning needs of students, thus affecting the motivation and quality of the clinical learning environment for undergraduate students. These authors add that professional nurses in the wards lack a qualification in education and feel that they are not paid to teach students. The effectiveness of the clinical learning environment is restricted and dysfunctional due to the unavailability and inaccessibility of clinical staff (Bezuidenhout, 2003:16; Carlson et al., 2003:33). Insufficient clinical accompaniment of nursing students further distorts and undermines the development of long-term ethical nursing skills and competencies, such as clinical judgement (Chan, 2004:665; Hartigan-Rogers, Cobbett, Amirault, & Muise-Davis, 2014:4).
4.2.2. Think critically
A nurse must be able to think critically in order to make sound clinical judgements in planning, managing and evaluating the health care of patients (Yildirim, 2011:258). The guidance from an experienced and knowledgeable clinical accompanist is essential for fostering critical thinking skills and ultimately, clinical judgement.
Participants said: '...give him an opportunity to think critical and make decisions; ...mastering of clinical skills and decision making has boost my confidence a lot; ...make decisions to better their ability to judge'.
With critical thinking being one of the primary expected competencies (Del Bueno, 2005:278), nurse educators are charged with the responsibility of designing clinical learning experiences that develop critical thinking skills along with nursing knowledge to meet expectations (Maskey, 2008:12). Students learn best by using the knowledge as they acquire it (Frith & Clark, 2013:7). The blending of knowledge acquisition and knowledge use facilitates students' understanding of practice and fosters clinical judgement. Students need to confront complex clinical situations that require them to think reflectively, link existing knowledge with the situation they are faced with to make sense under the guidance and support of clinical accompanists.
Yildirim (2011:258) describes the critical thinker as one who is habitually inquisitive, self-informed, trustful of reason, open-minded, fair-minded in evaluation, honest in facing personal biases, prudent in making judgments, willing to reconsider, clear about issues, orderly in complex matters, diligent in seeking relevant information, focused in inquiry and persistent in decisions. According to Facione (2011) "the critical thinking process is reflective and reasonable thinking about nursing problems without a single solution and is focused on deciding what to believe and do." Critical thinking is a complex, multidimensional cognitive process and is not bounded by predefined standards and outcomes dependent on reflective thought. It includes knowledge, skills and attitudes incorporated in the nursing process (Facione & Facione, 2008:3-4). While the nursing process demands linear thinking as part of problem solving, critical thinking compels nurses to challenge assumptions, question the context, look for new ways of doing and thinking, reconsider, sift and evaluate ideas for their worth and practicality (Yıldırım, 2011:258). A learning environment conducive to critical thinking provides opportunities for flexibility, creativity, support for change and risk taking. Interactive dialogue facilitates the building of connections to open up ideas, creates a way for thoughts and reflections to be made public and enables the dissemination of insight. Facilitators should not provide students with answers. A questioning attitude should be encouraged for students to develop interpretive, analytical, evaluative, inferential and explanatory skills to come to clinical judgement (Yıldırım, 2011:258).
4.2.3. The first clinical experience
The participants proposed that the first clinical experience of novice nursing students should be positive and an example of what nursing entails and not to be questionable, or a non-conducive environment for learning, as seems to be the case in some facilities. Participants experience the large first year intake and non-enabling environments for learning as an impending factor for the effective utilisation of clinical experiences and opportunity to develop clinical judgement. They said in this regard:
'...too many first years; …learn about basic patient care;… go on according that example for the rest of your life; ...clinical person should take student by hand; ... student to take ownership of learning; ...students need a safety net; ...trust the environment, people as family; ...sisters can support continuously, ...be approachable; ...questions to clarify'.
Clinical practice is a potentially stressful experience (Chan, 2004:665; Elliott, 2002:35); more so for a novice nurse. Levett-Jones, Lathlean, Higgins, and McMillan (2008:318) accentuate an educator's role to ensure clinical placements in positive learning environments to promote the personal and professional development of nursing students. A positive relationship between the ward staff and the nursing students is the single most crucial factor in creating a positive learning environment (Chesser-Smyth, 2005:324). Support and supervision leave nursing students more confident with their role during facilitation of learning (Landmark, Storm Hansen, Bjones, & Bøhler, 2003:836; Smith, Courtney, Finlayson, & Chapman, 2004:251) and contribute to their experiences of the clinical learning environment (Clark et al., 2004:109; Vallant & Neville, 2006:33; Zilembo & Monterosso, 2008:195). Ranse and Grealish (2007:173) view an unwelcoming environment as non-supportive and this contributes to students' fear of being overwhelmed by a lack of experience (Edwards, Smith et al., 2004:250; Pearcey & Elliott, 2004:385). A high level of anxiety can therefore lead to decreased learning as students focus on their feelings of anxiety and being accepted rather than on learning. This fear of making mistakes is according to Cheung (2011:287) the highest anxiety producing situation for all levels of students. Lambert and Glacken (2005:668) and Chan (2002:520) highlight the benefit of having a ward-based clinical facilitator for continuous access to someone who can concentrate solely on clinical education and support of students and who can attempt to narrow the theory-practice gap.
4.2.4. Nursing students are used as workforce
Nursing students are used as workforce (non-supernumerary status) to fill the gap in understaffed units. Tasks are allocated to permanent staff and students, resulting in limited learning opportunities for students and less guidance by experienced colleagues. Participants explained that:
'... students are supposed to be extra, not part of workforce; ...not too bad, it is a learning opportunity; ....they have to work under supervision;...no accompanist'.
McGowan (2006:1001) reports that using students as co-workers enables the clinical team to get through the work. On the other hand, a negative attitude to students' supernumerary status can negatively affect ward culture, resulting in both poor patient care and student learning, and ultimately, the facilitation of clinical judgement. Edelen (2009:3) and Koontz, Mallory, Burns, and Chapman (2010:242) found that during clinical practice, nursing students spent much time on menial tasks because registered nurses are not well acquainted with the learning outcomes of student nurses. The self-adopted task-oriented working system spontaneously acted as a barrier to effective relationships and participation in patient related decisions. In addition, students reported being used as workers to respond to staff shortages, at the expense of their role as learners. McGowan (2006:1001) found that a negative attitude to students' supernumerary status can negatively affect ward culture, resulting in both poor patient care and student learning and ultimately, the facilitation of clinical judgement.
Another obstacle for student accompaniment and the development of clinical judgement is the extensive use of nursing agencies to relieve the shortage of nurses in hospitals. It seems as if working for nursing agencies is popular due to the extra shifts to supplement income. Participants said:
'Agency personnel don't take ownership and accountability; ...some hospitals are running 80% on moonlighters"; …some of the training schools have no standards; …their nursing care is very poor'.
Storch (2013:1) and Jacobs (2011:3) support the finding that agency nurses often have conflicting schedules between primary and secondary jobs, they suffer from burn-out and exhaustion as a result of working excessive hours, have inadequate training, skills and experience, lack of knowledge of institution's procedures, policies and protocols. The severe shortage of nurses leave those in the system overworked, resulting in exhaustion as consequence of nurses working two jobs (Child, 2013). The training and subsequent qualifications offered by some training schools are questionable. Once the nurses' graduate from these institutions, they struggle to cope in the professional environment and need constant coaching and assistance from colleagues, putting additional strain on an under-resourced system. Nurses are sometimes employed in positions for which they are not qualified, but they accept the position for financial reasons. The inevitable result is a decline in the health of the overworked nurse, poor quality of care to patients, students receive questionable to no clinical accompaniment and are exposed to improper role modelling (ANON, 2014).
4.2.5. Role-modelling
Role-modelling, being a fundamental principle of learning in the clinical setting (Perry, 2009:38) impacts directly on patient care, as well as students' confidence and competence. SANC (2005:6) requires every professional nurse and midwife to create a learning environment and opportunities to foster professional growth and to actively engage in education and training of learners towards independence in the clinical nursing environment, thus being role models.
Participants reported:
'There are no role models; ...an imbalance …too many chiefs, less indians; ...the chiefs don't have sufficient knowledge; ...role model to be the sister working together with student; …facilitators need to be knowledgeable; ...evidence-based practice; …educators need to have experience, especially clinical experience; ...role models have to be there, ...identify learning opportunities; ...what monkey see, monkey do'.
The absence of role models in the clinical area and a reluctance by ward sisters to act as role models and mentors are confirmed by Mabuda, Potgieter, and Alberts (2008:23). Reports health personnel's antagonism towards students. Students' questions are not attended to and their knowledge is disregarded. Potgieter (2012:5); Bruce et al. (2011:228, 255) and Hayes (2001:112) highlight the importance of the learning accompanist as role model. It should be a subject expert with clinical experience, effective communication skills, a lifelong learner who is approachable, flexible, fair, cooperative with a positive attitude towards students and someone who demonstrates a sense of humour, warmth, empathy, good listening skills and someone who conveys enthusiasm in every contact during patient care (Lee, Cholowski & Williams, 2002:415). The clinical accompanist as role model facilitates learning within the prescribed ethical-legal parameters and delivers quality care under pressure (Bruce et al., 2011:228, 255). Dickson, Walker, and Bourgeois (2006:417) define facilitation as the technique by which one person makes challenges easier for others in an atmosphere of mutual respect and trust to cope with the purpose of co-creating new knowledge through a process of regular reflective interaction between learner and facilitator (Papastavrou, Lambrinou, Tsangari, Saarikoski, & Leino-Kilpi, 2010), providing constant feedback and support to facilitate clinical judgement (Burns, Beauchesne, Rayan-Krause, & Sawin, 2006:172,173; Hayes, 2001:112).
4.2.6. Communication
Communication in health care is in certain circumstances troublesome, but it is vital to ensure understanding in a culturally sensitive way to prevent misunderstandings. Good interpersonal relationships, communication and support between staff and students create an environment conducive to students' learning in the clinical environment. It results in a reduction in anxiety, positive socialisation, confidence and self-esteem, thus promoting learning.
Participants said: 'Precise language is an urgent thing; ...you don't have the ability to speak the languages; ...it influences the care; ...language is a barrier and we need to clarify understanding'.
Literature (Levett-Jones et al., 2008:321; Rosenstein & O'Daniel, 2006:88) confirms that effective communication and teamwork do not always occur in clinical settings. Anxiety is associated with a lack of confidence to ask questions and a fear of making mistakes (Levett-Jones et al., 2008:321). Sutcliffe, Lewton, and Rosenthal (2004:190); Flin, Fletcher, McGeorge, Sutherland and Patey, 2003: 135) reveal that social, relational and organizational structures contribute to inconsistent, conflicting communication failures that have been implicated as contributors to adverse clinical events and patient outcomes. Effective communication enhances employee morale and decreases the length of patient stay (Casey & Wallis, 2011:36; Chant, Jenkinson, Randle, & Russell, 2002:16).
Carlson et al. (2003:37) identify the discussion of information concerning the patients' condition and treatment plan during ward rounds and shifts changes as a vital learning opportunity for nursing students. Beukes et al. (2010:2) indicate that students should be able to use their developing communication skills to establish therapeutic nurse-patient relationships to evolve into competent practitioners. Communication appears therefore to be an obstacle in the process because professional nurses do not the take time to explain the patient treatment plan (Carlson et al., 2003:37) and valuable opportunities for the demonstration of and development of clinical judgement are lost. Bruce et al. (2011:256) accentuate the quality of clinical teaching as crucial to the professional development and facilitation of clinical judgement of undergraduate students.
4.2.7. Interpersonal relationships and professional conduct
Interpersonal relationships and professional conduct serve as facilitation for a trusting climate conducive to sharing understanding, critical thinking and clinical judgement attempts. The participants reported conflict with students:
'...students don't have respect, ...no discipline; ...staying home for minor ailments; ...private cell phone calls while on duty; ...transport is always the reason for late coming; ...discussing personal issues at the bedside; ...disrespectful attitudes; "...this have a ripple effect on the colleagues"; with doctors "...doctors can talk to you as if you are a dog"; with colleagues "...colleagues are bullying ye; ...sisters are all going on lunch and leave the students to solve the problem".
Lambert and Lambert (2008:40) state that nurses are frustrated with their work environment due to staff shortages, increased workloads, the critical nature of their patients and advances in technology. Relationships are stressed and problems are highlighted include unfriendly staff, hostile attitudes, students are denied opportunities to learn, students are isolated and ignored, negative remarks about becoming a nurse and being treated with hostility. Preceptors were noted for undervaluing students' efforts, placing students under undue pressure and setting impossible expectations. McKenna, Smith, Poole, and Coverdale (2003:92) report that classmates contribute to relationship problems by spreading rumours and acting in a nasty manner. Clarke (2012:270) view the consequences of bullying as numerous, including feelings of frustration, powerlessness, depression, fear, guilt, anger, anxiety, self-hatred, a decrease in confidence, morale and productivity (Celik & Bayraktar, 2004:232; Sofield & Salmond, 2003:276). Rosenstein and O'Daniel (2006:88) report that disruptive behaviour by physicians and nurses, staff satisfaction, turnover, patient outcomes, medical errors and compromises in patient safety can be traced back to poor communication and ineffective teamwork as a result of poor interpersonal relationships (Seago, 2008:1, 2). The impact of negative relationships leads to burn-out, apathy, passive anger and symptoms associated with post-traumatic stress disorder, resulting in nurses who distance themselves from colleagues and patients (Foster, Mackie, & Barnett, 2004:68; Randle, 2003:398) and an increase in errors (Rippon, 2000: 456). Due to the distressing nature of bullying, Randle (2003:398) reports an increase in absence from work, resulting in a negative effect on students' learning and progress to clinical judgment.
4.2.8. Conclusion theme 2
The clinical nursing environment is currently not conducive to the nurturing of nursing students' clinical judgement due to:
• Inadequate clinical accompaniment on account of staff shortages, insufficient role models, lack of motivation, knowledge and confidence of professional nurses for the task.
• The gap between theory and practice hampers critical thinking, an essential skill needed for clinical judgement.
• The large intake of first year nursing students is an obstacle for the clinical placement of nursing students to maximum exposure to appropriate learning opportunities.
• Nursing students are used as workforce for repetitive menial tasks to fill the gap in understaffed units, resulting in limited learning opportunities and a lack of guidance by experienced practitioners.
• Stressed interpersonal relationships and inadequate communication are obstacles for trust and confidence to seek clarity and share understanding.
5. Recommendations
Based on the research findings, the following recommendations are made in relation to nursing research, nursing education and nursing practice.
5.1. Nursing research
• Investigation of appropriate teaching-learning strategies to enhance critical thinking and the development of assessment instruments for assessment of clinical judgement as skill.
• Investigation of students' perspective on clinical judgement as well as the relationship between clinical guidance and clinical judgement.
5.2. Nursing education
• Varying teaching methodologies should be implemented to enhance problem solving skills such as explosion to clinical learning experiences accumulating in complexity for blending of knowledge acquisition and knowledge use to enhance higher order thinking skills and reflective interaction.
5.3. Nursing practice
In relation to nursing practice the following are recommended which can improve student development of clinical judgement:
5.3.1. Clinical educators
• All role players involved in the teaching-learning of nursing students should collaborate to find solutions for mutually experienced problems relating to clinical accompaniment and the fusion of theory and practice as follows:
○ Clinical nurse educators need to be clinically experienced and skilled for discipline of tutoring.
○ The clinical judgement process included as central aspect in the teaching-learning process.
○ Continuous guidance of especially first year nursing students by:
▪ Educators need to avail themselves of the clinical environment;
▪ Appointment of a full time clinical preceptor situated per clinical facility.
5.3.2. Student placement
• Criteria should be drafted for nursing students' clinical placement based on safety, learning opportunities, infrastructure, resources, role modelling and support.
The following aspects need attention:
○ Feedback from students should be attended to.
○ Allocation to a specific discipline for a reasonable period of time to allow students to participate as member of the multi-professional team and assure maximum exposure to learning opportunities.
○ Establish opportunities for reflection of all role players.
5.4. Limitations of the study
The following limitations were identified:
A rather small sample for a "World Café" was utilised. Limited voluntary participation of primary health care nurses could be seen as a limitation for the research but rich data and data saturation were obtained. The results of this research are therefore contextual, but they nonetheless provide food for thought.
6. Conclusion
The World Café method of data collection provided rich descriptions of professional nurses' understanding of the concept clinical judgement and factors hampering its development in the clinical environment. Nurses' understanding of the concept clinical judgement in nursing seems to be superficial and insufficient, especially regarding the relationship between a sound knowledge base, reasoning and critical thinking skills and its impact on effective interpretation, and ultimately decision making. This study revealed the complexity of theory-practice integration, clinical accompaniment and reflection as essential elements in the facilitation of clinical judgement and the need for a strategy to facilitate clinical judgement in the nursing environment. The recommendations should enhance the learning experiences in the development of thinking skills, attributes and knowledge of nursing students during their placement in the clinical learning environment.
References
Alfaro- LeFevre, R. (2012). Critical thinking, clinical reasoning, and clinical judgment: a practical approach (5th ed.). St. Louis, MO: Saunders Elsevier. [ Links ]
ANON. (2014). The South African nursing crisis Africa health placements (AHP). http://www.ahp.org.za/news-detail/104/thesouth Accessed 20.04.14. [ Links ]
Australian Nursing and Midwifery Council. (2005). National competency standards for the registered nurse. http://www.anmc.org.au/docs/Competency_standards_RN.pdf Accessed 09.07.12. [ Links ]
Benner, P. (2001). From novice to expert: Excellence and power in clinical nursing practice. Upper Saddle River, NJ: Prentice-Hall. [ Links ]
Benner, P., Hughes, R. G., & Sutphen, M. (2008). Chapter 6: clinical reasoning, decision making, and action: thinking critically and clinically. In R. G. Hughes (Ed.), Patient safety and quality: an evidence-based handbook for nurses (pp. 87e109). Rockville (MD): Agency for Healthcare Research and Quality (US). [ Links ]
Benner, P., Tanner, C., & Chesla, C. (2009). Expertise in nursing practice: Caring, clinical judgment and ethics (2nd ed.). , New York: Springer. [ Links ]
Beukes, S., Nolte, A. G. W., & Arries, E. (2010). Value-sensitive clinical accompaniment in community nursing science. Health SA Gesondheid, 15(1), 485e487. http://www.hsag.co.za/index.php/HSAG/article/view/485/539 Accessed 29.05.14. [ Links ]
Bezuidenhout, M. C. (2003). Guidelines for enhancing clinical supervision. Health SA Gesondheid, 8(4), 12e23. [ Links ]
Blakeman, J. R., Samuelson, S. J., & McEvoy, K. N. (2013). Analysis of a silent voice. A qualitative inquiry of embroidery created by a patient with schizophrenia. Journal of Psychosocial Nursing, 51(6), 38e45. [ Links ]
Bos, E., Alinaghizadeh, H., Saarikoski, M., & Kaila, P. (2011). Validating the 'clinical learning environment, supervision and nurse teacher' CLESþ T instrument in primary health care settings using confirmatory factor analysis. Journal of Clinical Nursing, 21, 1785e1788. [ Links ]
Botes, A. (2003). Validity, reliability and trustworthiness to sum up. In D. Rossouw (Ed.), Intellectual tools: Skills for the human sciences (2nd ed., pp. 176e184). Pretoria: Van Schaik. [ Links ]
Bothma, Y., Greeff, M., Malaudzi, F. M., & Wright, S. C. D. (2010). Research in health science. Cape Town: Heineman. [ Links ]
Brown, J. (2005). The world Cafe: Living knowledge through conversations that matter. Unpublished doctoral dissertation. The Fielding Institute. [ Links ]
Bruce, J. C., Klopper, H. C., & Mellish, J. M. (2011). Teaching and learning the practice of nursing (5th ed.). Cape Town: Heinemann Pearson. [ Links ]
Burns, C., Beauchesne, M., Rayan-Krause, P., & Sawin, K. (2006). Mastering the preceptor Role: challenges of clinical teaching. Journal of Pediatric Health Care, 20(3), 172e183. [ Links ]
Burns, N., & Grove, S. K. (2009). The practice of nursing research: Appraisal, synthesis, and generation of evidence (6th ed.). St. Louis: Saunders Elsevier. [ Links ]
Carlson, S., Kotze, W. J., & Van Rooyen, D. (2003). Enhancing support for nursing students in the clinical setting. Curationis, 26(2), 30e39. http://www.curationis.org.za/index.php/curationis/article/viewFile/778/715 Accessed 15.06.14. [ Links ]
Casey, A., & Wallis, A. (2011). Effective communication: principle of nursing practice E. Nursing Standard, 25(32), 35e37. [ Links ]
Celik, S. S., & Bayraktar, N. (2004). A study of nursing student abuse in Turkey. Journal of Nursing Education, 43, 330e336. [ Links ]
Chabeli, M. (2007). Facilitating critical thinking within the nursing process framework: a literature review. Health SA Gesondheid, 12(4), 69e89. [ Links ]
Chan, D. S. K. (2002). Associations between student learning outcomes from their clinical placement and their perceptions of the social climate of the clinical learning environment International. Journal of Nursing Studies, 39(5), 517e524. http://dx.doi.org/10.1016/S0020-7489(01)00057-8 Accessed 20.06.14. [ Links ]
Chan, D. S. K. (2004). Hong Kong nursing students' perception of the clinical environment: a questionnaire survey. International Journal of Nursing Studies, 42(6), 665e672. [ Links ]
Chant, S., Jenkinson, T., Randle, J., & Russell, G. (2002). Communication skills: some problems in nursing education and practice. Journal of Clinical Nursing, 11(1), 12e21. [ Links ]
Chesser-Smyth, P. A. (2005). The lived experiences of general students nurses on their first clinical placement: a phenomenological study. Nurse Education in Practice, 5, 320e327. [ Links ]
Cheung, R. (2011). Nursing students' anxiety and clinical performance. The Journal of Nursing Education, 50(5), 286e289. [ Links ]
Child, K. (2013). Nursing in SA is in crisis Accessed 15.07.14 http://www.timeslive.co.za/thetimes/2013/07/29/nursing-in-sa-isin-crisis. [ Links ]
Chisari, M. (2009). Redesigning the RN orientation program. http://www.massgeneral.org/pcs/CaringHeadlines Accessed 08.02.13. [ Links ]
Chitty, K. K., & Black, B. P. (2011). Professional nursing: Concepts and challenges (6th ed.). MO: Saunders. Elsevier Maryland Heights. [ Links ]
Clarke, C. (2012). The effects of bullying behaviours on student nurses in the clinical setting electronic theses and dissertations. Paper 372. University of Windsor http://scholar.uwindsor.ca/cgi/viewcontent.cgi?article=1371&context=etd Ontario, Canada Accessed 10.07.13. [ Links ]
Clark, M. C., Owen, S., & Tolken, M. A. (2004). Measuring student perceptions of clinical competence. Journal of Nursing Education, 42(12), 548e554. [ Links ]
Cohen, M. S., Jacobs, J. P., Quintessenza, J. A., Chai, P. J., Lindberg, H. L., Dickey, J., et al. (2007). Mentorship, learning curves, and balance. Cardiology in the Young, 17, 164e174. http://www.ncbi.nlm.nih.gov/pubmed/18039410?ordinalpos=1&itool=EntrezSystem2.PE (Accessed 08.02.10). [ Links ]
De Vos, A. S. (2005). Research at grass roots, 3rd Imp. Pretoria: Van Schaik Publishers. [ Links ]
Del Bueno, D. (2005). A crisis in critical thinking. Nursing Education Perspectives, 26(5), 278e282. http://dx.doi.org/10.1043/1536-5026(2005)026[0278:ACICT]2.0.CO;2 Accessed 25.03.14. [ Links ]
Dickson, C., Walker, J., & Bourgeois, S. (2006). Facilitating undergraduate nurses' clinical practicum, the lived experience of clinical facilitator. Nurse Education Today, 26(5), 416e422. [ Links ]
Du Plessis, E., Koen, M. P., & Bester, P. (2012). Exploring home visits in a faith community as a service-learning opportunity. Nurse Education Today, 33(8), 766e771. [ Links ]
Edelen, B.,G. (2009). Measuring and enhancing clinical decision making ability among students in an associate degree nursing program. PhD. University of Connecticut. [ Links ]
Edwards, H., Smith, S., Courtney, M., Finlayson, K., & Chapman, H. (2004). The impact of clinical placement location on nursing students' competence and preparedness for practice. Nurse Education Today, 24, 248e255. [ Links ]
Elliott, M. (2002). The clinical environment: a source for stress for undergraduate nurses. Australian Journal of Advanced Nursing, 20, 34e38. [ Links ]
Facione, P. (2006). Critical thinking: What it is and why it counts? (pp. 1e28) California: Academic press. http://www.student.uwa.edu.au/data/assets/pdf_file/0003/1922502/Critical-Thinking-What-it-is-and-why-it-counts.pdf Accessed 22.03.14. [ Links ]
Facione, P. A. (2011). Think critically. Englewood Cliffs, NJ: Pearson Education. [ Links ]
Facione, N. C., & Facione, P. A. (2008). "Critical Thinking and Clinical Judgment," from critical thinking and clinical reasoning in the health sciences: a teaching Anthology. Published by Insight Assessment/ The file:///C:/Users/10197869/Downloads/ CHþ1þCTþ&þCRþþ-þFacioneþ&þFacione%20(6).pdf, Accessed 25.03.14. [ Links ]
Flin, R., Fletcher, G., McGeorge, P., Sutherland, A., & Patey, R. (2003). Anaesthetists' attitudes to teamwork and safety. Anaesthesia, 58(3), 233e242. [ Links ]
Foster, B., Mackie, B., & Barnett, N. (2004). Bullying in the health sector: a study of bullying of nursing students. New Zealand Journal of Employment Relations, 29(2), 67e24. [ Links ]
Frankel, A. (2009). Nurses' learning styles: promoting better integration of theory into practice. Nursing times, 105, 1e7. [ Links ]
Frith, K. H., & Clark, D. J. (Eds.). (2013). Distance education in nursing (3rd ed.). New York: Springer. [ Links ]
Froneman, K (2013). Basic elements (Unpublished Masters dissertation). SA: North-West University Potchefstroom Campus. [ Links ]
Gagliardi, A. R., Perrier, L., Webster, F., Leslie, K., Bell, M., Levinson, W., et al. (2009). Exploring mentorship as a strategy to build capacity for knowledge translation research and practice: protocol for a qualitative study. Implementation Science, 4(55). http://www.ncbi.nlm.nih.gov/pubmed/19691833?ordinalpos¼1&itool¼EntrezSystem Accessed 15.07.14. [ Links ]
Gerdeman, J. L., Lux, K., & Jacko, J. (2013). Using concept mapping to build clinical judgement skills. Nurse Education in Practice, 13, 11e17. [ Links ]
Geyer, N., Naude, S., & Sithole, G. (2002). Legislative issues impacting on the practice of the South African nurse practitioner. Journal of the American Academy of Nurse Practitioners, 14(1), 11e15. [ Links ]
Gotlieb, L. N. (2013). Strengths-based nursing care. New York: Springer. [ Links ]
Grossman, S. C. (2007). Mentoring in nursing. A dynamic and collaborative process. Washington: Bang. [ Links ]
Haghdoost, A. A., & Shakibi, M. R. (2006). Medical student and academic staff perceptions of role models: an analytical cross sectional study. BMC Medical Education, 6(9). [ Links ]
Hammond, K. R. (1996). Reviewing intuitive decision making and uncertainty: the implications for medical education. Medical Education, 36(3), 216e234. [ Links ]
Hartigan-Rogers, J. A., Cobbett, S. L., Amirault, M. A., & Muise- Davis, M. E. (2014). Nursing graduates' perceptions of their undergraduate clinical placement. International Journal of Nursing Education Scholarship, 11(1). [ Links ]
Hayes, E. F. (2001). Factors that facilitate or hinder mentoring in the nurse practitioner preceptor/student relationship. Clinical Excellence for Nurse Practitioners, 5, 111e118. [ Links ]
Henning, E., Van Rensburg, W., & Smit, B. (2004). Finding your way in qualitative research. Pretoria SA: Van Schaik. [ Links ]
Higgs, J., Jones, M. A., Loftus, S., & Christen, N. (2008). Clinical reasoning in the health professionals (3rd ed.). Butterworth Heinemann Elsevier. [ Links ]
Higuchi, K. A. S., & Donald, J. G. (2002). Thinking processes used by nurses in clinical de decision making. Journal of Nursing Education, 41, 145e153. [ Links ]
Jacobs, M. (2011). Nursing agencies in the spotlight. ANASA NEWS FLASH http://www.mhr.co.za/IndustryRelatedInfo/ANASA%20News%20Flash%208%20Nursing Accessed 20.06.14. [ Links ]
Jerlock, M., Falk, K., & Serverinsson, E. (2003). Academic nursing education guidelines: tools for bridging the gap between theory, research and practice. Nursing and Health Sciences, 5(3), 219e228. [ Links ]
Kanno, H., & Koeske, G. (2010). MSW students' satisfaction with their field placements: the role of preparedness and supervision quality. Journal of Social Work Education, 46(1), 23e38. [ Links ]
Klopper, H. C. (2009). Nursing education: a reflection (2nd ed.). Potchefstroom: NWU. [ Links ]
Klopper, H. C., & Knobloch, S. (2010). Validity, reliability and trustworthiness. In K. Jooste (Ed.), The principles and practice of nursing and health care (pp. 317e325). Pretoria, Van Schaik, Pretoria. [ Links ]
Koen, M. P., Du Plessis, E., & Koen, V. (2012). Data analysis: the World Cafe. Springer (Unpublished). [ Links ]
Koontz, A., Mallory, J., Burns, J., & Chapman, S. (2010). Staff nurses and students: the good, the bad, and the ugly. Med-surg Nursing: Official Journal of the Academy of Medical-Surgical Nurses, 19(4), 240e246. [ Links ]
Lambert, V., & Glacken, M. (2005). Clinical education facilitators: a literature review. Journal of Clinical Nursing, 14(6), 664e673. [ Links ]
Lambert, V. A., & Lambert, C. E. (2008). 'Nurses' workplace stressors and coping strategies. Indian Journal of Palliative Care, 14(1), 38e44. [ Links ]
Landmark, B. T. H., Storm Hansen, G., Bjones, I., & Bøhler, A. (2003). Clinical supervision e factors defined by nurses as influential upon the development of competence and skills in supervision. Journal of Clinical Nursing, 12, 834e841. [ Links ]
Lasater, K. (2007). Clinical judgement development: using simulation to create and assessment rubric. Journal of Nursing Education, 45(11), 496e503. [ Links ]
Ledesma-Delgado, M. E., & Mendes, M. M. (2009). 'The nursing process presented as routine care actions: building its meaning in clinical nurses' perspective. Revista Latino- Americana de Enfermagem, 17(3), 328e334. [ Links ]
Lee, W., Cholowski, K., & Williams, A. K. (2002). Nursing students' and clinical educators' perceptions of characteristics of effective clinical educators in an Australian university school of nursing. Journal of Advanced Nursing, 39(5), 412e420. [ Links ]
Levett-Jones, T., Lathlean, J., Higgins, I., & McMillan, M. (2008). Staff-student relationships and their impact on nursing students' belongingness and learning. Journal of Advanced Nursing, 65(2), 316e324. [ Links ]
Lindsey, P. L., & Jenkins, S. (2013). 'Nursing Students' clinical judgement regarding rapid response: the influence of a clinical simulation education intervention. Nursing Forum, 48(1),61e70. [ Links ]
Lin, P., Hsu, M., & Tasy, S. (2003). Teaching clinical judgement in Taiwan. Journal of Nursing Research, 11(3), 159e166. [ Links ]
Mabuda, B. T., Potgieter, E., & Alberts, U. U. (2008). Student nurses' experiences during clinical practice in the Limpopo province. Curationis, 31(1), 19e27. [ Links ]
Marshburn, D. M., Engelke, M. K., & Swanson, M. S. (2009). Relationships of new nurses' perceptions and measured performance- based clinical competence. Journal of Continuing Education in Nursing, 9(40), 426e432. [ Links ]
Mann, J. (2012). Critical thinking and clinical judgment skill development in baccalaureate nursing students. Kansas Nurse, 87(1), 26e31. [ Links ]
Maskey, C. L. (2008). The coordination of clinical and didactic learning experiences to improve critical-thinking skills and academic performance. Teaching and learning in Nursing, 3, 11e15. [ Links ]
Masters, K. (2005). Role development in professional nursing practice. Sudbury, MA: Jones and Bartlett. [ Links ]
McGowan, B. (2006). Who do they think they are? Undergraduate perceptions of the definition of supernumerary status and how it works in practice. Journal Clinical Nursing, 15(9), 1099e1105. [ Links ]
McKenna, B. G., Smith, N. A., Poole, S. J., & Coverdale, J. H. (2003). Horizontal violence: experiences of registered nurses in their first year of practice. Journal of Advanced Nursing, 42(1), 90e96. [ Links ]
Moscaritolo, L. (2009). Interventional strategies to decrease nursing student anxiety in the clinical learning environment. The Journal of Nursing Education, 48(1), 17e23. [ Links ]
Nielsen, A. (2009). Concept- based activities using the clinical judgement model as a foundation for clinical learning. Journal of Nursing Education, 48(6), 350e354. [ Links ]
Nightingale, F. (1992). Notes on nursing: What it is, what it is not (Commemorative ed.). Philadelphia: Lippincott Williams & Wilkins (Original work published 1860). [ Links ]
Papastavrou, E., Lambrinou, E., Tsangari, H., Saarikoski, M., & Leino-Kilpi, H. (2010). Student nurses experience of learning in the clinical environment. Nurse Education in Practice, 10(3), 176e182. [ Links ]
Pearcey, P. A., & Elliott, B. E. (2004). Student impressions of clinical nursing. Nurse Education Today, 24, 382e387. [ Links ]
Pelzang, R. (2010). Time to learn: understanding patient-centred care British. Journal of Nursing, 19(14), 912e917. [ Links ]
Perry, B. (2009). Role modelling excellence in clinical nursing practice. Nurse Education in Practice, 6(1), 36e44. [ Links ]
Pinnock, R., Sharif, B., Hawke, S., Henning, M., & Jones, R. (2011). Students' and teachers' perceptions of the clinical learning environment in years 4 and 5 at the University of Auckland. The New Zealand Medical Journal, 124(134), 63. [ Links ]
Pongmarutai, T. (2010). Application of a judgement model toward measurement of clinical judgement in senior nursing students. Dissertation http://digitalscholarship.unlv.edu/thesesdissertations Accessed 15.07.14. [ Links ]
Potgieter, E. (2012). Clinical teaching: developing critical thinking in student nurses. Professional Nurse Today, 16(2), 4e8. [ Links ]
Quinn, F. M., & Hughes, S. J. (2009). Quinn's principles and practice of nurse education (5th ed.). London: Nelson Thorns. [ Links ]
Randall, C. E., Tate, B., & Lougheed, M. (2007). Emancipatory teaching-learning philosophy and practice education in acute care: navigating tensions. Journal of Nursing Education, 46, 60e64. [ Links ]
Randle, J. (2003). Bullying in the nursing profession. Journal of Advanced Nursing, 43(4), 395e401. [ Links ]
Ranse, K., & Grealish, L. (2007). 'Nursing students' perceptions of learning in the clinical setting of the dedicated education unit. Journal of Advanced Nursing, 58, 171e179. [ Links ]
RCN (Royal College of Nursing). (2003). Defining nursing. London: RCN. http://www.rcn.org.uk/data/assets/pdf_file/0008/78569/001998.pdf Accessed 10.08.12. [ Links ]
Rippon, T. J. (2000). Aggression and violence in health care professions. Journal of Advanced Nursing, 31(2), 452e460. [ Links ]
Rivas, F. J. P., Garcia, J. M. S., Arenas, C. M., Lagos, M. B., & Lopez, M. G. (2012). Implementation and evaluation of the nursing process in primary health care. International journal of knowledge, 23(1), 18e28. [ Links ]
Rosenstein, A., & O'Daniel, M. (2006). Addressing disruptive nurse-physician behaviors: developing programs and policies to improve outcomes of care. Harvard Health Policy Review Spring, 7, 86e91. Journal of the Scholarship of Teaching and Learning, 13(4), 21 e 35. [ Links ]
South African Nursing Council (SANC) Nursing Act, 2005 (Act no 33 of 2005) Regulation 786 Regulations regarding the scope of practice of Nurses and Midwifes, point 4.4 g-k page 6 No 38935 Government Gazette 15 October 2013. [ Links ]
Schön, D. (1987). Education the reflective practitioner. San Francisco: Jossey-Bass. [ Links ]
Seago, J. A. (2008). 'Professional communication': chapter 32. In R. G. Hughes (Ed.), Patient safety and quality: an evidence-based handbook for nurses (pp. 1e13). Rockville: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services. http://www.ahrq.gov/professionals/cliniciansproviders/resources/nursing/resources/ nurseshdbk/SeagoJ_PC.pdf. [ Links ]
Simpson, E., & Courtney, M. (2002). Critical thinking in nursing education: literature review. International Journal of Nursing Practice, 8(2), 89e98. [ Links ]
SmithBattle, L., & Diekemper, M. (2001). Promoting clinical practice knowledge in an age of taxonomies and protocols. Public Health Nursing, 18, 401e408. [ Links ]
Smith, E. H. S., Courtney, M., Finlayson, K., & Chapman, H. (2004). The impact of clinical placement location on nursing students' competence and preparedness for practice. Nurse Education Today, 24, 248e255. [ Links ]
Sofield, L., & Salmond, S. W. (2003). A focus on verbal abuse and intent to leave the organization. Orthopaedic Nursing, 22(4), 274e283. [ Links ]
South Africa Department of Health. (2011). Nursing Act (33/2005): regulations: approval of and the minimum requirements for the education and training of a nurse leading to registration as a professional nurse. (Notice1046). Government gazette, 34852:20, 14 December 2011. [ Links ]
South Africa Department of Health. (2013). Nursing strategy for South Africa. http://www.sanc.co.za/archive/archive2013/NursingStrategy2013.html Accessed 03.08.14. [ Links ]
Storch, C. (2013). Advantages and disadvantages of being an agency nurse. Horizon healthcare staffing: "Providing Quality staffing services since 1992". [ Links ]
Straus, S. E., Chatur, F., & Taylor, M. (2009). Issues in the mentormentee relationship in academic medicine: a qualitative study. Academic Medicine, 84(1), 135e139. http://www.ncbi.nlm.nih.gov/pubmed/19116493? ordinalpos=1&itoo=EntrezSystem Accessed 02.02.13. [ Links ]
Sutcliffe, K., Lewton, E., & Rosenthal, M. (2004). Communication failures: an insidious contributor to medical mishaps. Academic Medicine, 79, 186e194. [ Links ]
Tanner, C. A. (2006). Thinking like a nurse: a research-based model of clinical judgement in nursing. Journal of Nursing Education, 45(6), 204e211. [ Links ]
The World Cafe. (2008). The world cafe. Retrieved 19 June, 2013, from http://www.theworldcafe.com/pdfs/cafetogo.pdf. [ Links ]
Vallant, S., & Neville, S. (2006). The relationship between student nurse and nurse clinician: impact on student learners. Nurse Praxis in New Zealand, 22, 23e33. [ Links ]
Van Graan, A. C., Koen, M. P., & Williams, M. J. (2014). Clinical judgement in nursing: A conceptual analysis (Unpublished doctoral thesis). SA: North-West University, Potchefstroom Campus. [ Links ]
Van Rooyen, D., Laing, R., & Kotze, W. J. (2005). Accompaniment needs of nursing students related to the dying patient. Curationis, 28(4), 31e39. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16450557?ordinalpos¼1&itool¼EntrezSystem Accessed 02.02.13. [ Links ]
Yildirim, B. (2011). Critical thinking in nursing process and education. International Journal of Humanities and Social Science, 1(13), 257e262 [Special Issuee] www.mktudegy.hu/?q¼system/files/VargaJ.pdf Accessed 10.06.14. [ Links ]
Zilembo, M., & Monterosso, L. (2008). Nursing students' perceptions of desirable leadership qualities in nurse preceptors: a descriptive survey. Contemporary Nurse, 27, 194e206. [ Links ]
FURTHER READING
Creswell, J. W. (2009). Research design: Qualitative, quantitative, and mixed methods approaches (3rd ed.). Thousand Oaks, CA: Sage Publications. [ Links ]
Mochaki, N. W. (2012). Clinical accompaniment. Unpublished master's thesis www.edunurse.co.za/presentations/Clinical%20Accompaniment.ppt Accessed 20.06.14. [ Links ]
Jooste, K. (2009). Supervision in nursing practice. Cape Town: Juta. [ Links ]
Phaneuf, M. (2008). Clinical judgement e An essential tool in the nursing profession Accessed 17.07.12. from http://www.infiressources.ca/fer/Depotdocument_anglais/Clinical_Judgement%E2%80%9 3An_Essential_Tool_in_the_Nursing_Profession.pdf. [ Links ]
SANC. (1992). Philosophy and policy of the South African Nursing Council with regard to professional nursing education and training. Pretoria: SANC. [ Links ]
Turner, P. (2005). Critical thinking in nursing education and practice as Defined in the literature. Nursing Education Perspectives, 26(5), 272e277. http://dx.doi.org/10.1043/1536-5026(2005)026[0272:CTINEA]2.0.CO;2 Accessed 12.07.14. [ Links ]
Received 6 April 2015
Accepted 5 April 2016
Available online 8 August 2016
Peer review under responsibility of Johannesburg University.
* Corresponding author. School of Nursing Science, North-West University (Potchefstroom Campus), Private bag X6001, Potchefstroom, 2520, South Africa. Tel.: +27 082 6869659.
Annexure 1
Annexure 2
Annexure 3
















