Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
Health SA Gesondheid (Online)
versión On-line ISSN 2071-9736
versión impresa ISSN 1025-9848
Health SA Gesondheid (Online) vol.21 no.1 Cape Town 2016
http://dx.doi.org/10.1016/j.hsag.2016.06.002
REVIEW ARTICLE
The bloody truth: Investigating nurse phlebotomy competencies at a private laboratory in Johannesburg, South Africa
Lizelle Crous1, * ; S.J. Armstrong2
University of the Witwatersrand, 7 York Road, Parktown, 2193, South Africa
ABSTRACT
BACKGROUND: With the introduction of the phlebotomist technician-certification programme in South Africa, nurses' phlebotomy competence, an acquired skill during basic training, was questioned. Various studies indicate that the majority of errors occur during the collection phase, causing negative outcomes for the patient.
OBJECTIVE: Despite in-service training, samples were rejected and linked to the nurse phlebotomist's sample collection technique. The purpose of this study was to establish if nurses' phlebotomy techniques could be improved through a workplace-training programme in the attempt to improve the quality of the test results.
METHOD: The methodology used was a quantitative, experimental, pilot intervention study, based on a one group pre-test - post-test design. Data was collected by means of peer video recordings of the nurses (n = 20) based at outpatient departments of the laboratory. Independent evaluators evaluated the recordings against criterion-based observational checklists.
RESULTS: Compliance to standards on the venepuncture procedure was identified during the pre-test, with an average score of 61.9%. The training programme, developed to address all deviations from the standards, proved to be effective as the post-test compliance score was 85%.
CONCLUSION: The reason for improving nurses' phlebotomy skills is to ensure accurate results that will assist clinicians caring for their patients. The results suggest that knowledge and skills were acquired, however further investigations are needed for guidance in the standardisation of training programmes and at what intervals should these training programmes be presented.
Keywords: Venepuncture technique; In-service training; Peer-evaluation
1. Introduction
In modern medicine, doctors rely heavily on diagnostic testing to assist them with patient management, making or excluding diagnosis and implementing an appropriate treatment plan. It is therefore important that the laboratory produces quality test results.
Phlebotomy is a neglected procedure in healthcare. Limited time is spent on training nurses and doctors on the procedures and yet it involves serious health risks, which could result from improper venepuncture technique impacting on the patient treatment outcomes. In European countries and the USA, specially trained phlebotomists perform phlebotomy procedures, whilst in most African countries medical professionals perform phlebotomy procedures. In South Africa, however, the situation is more complex as phlebotomy is performed by both health professionals and trained phlebotomists, with different competency requirements for both (Mbah, 2014). The phlebotomist technician qualification is an 18-month certificate and on completion thereof, a person registers with the Health Professions Council of South Africa (HPCSA). This programme focuses primarily on the venepuncture procedure and clear guidance is given with regard to the requirements of training and competence, which will lead to a person registering as a phlebotomist (Presley & Liotta, 2006). Unlike the phlebotomy technicians nursing staff do not need a certificate for phlebotomy and therefore training programmes vary in requirements and set outcomes.
In South Africa, phlebotomy is considered an acquired skill and not a discipline. With the increase in patient numbers, doctors realised they cannot keep up with providing all aspects of quality patient care and nurses were taught how to take blood at the patient's bedside. Nurses were available to patients around the clock and it seemed to be a practical and justifiable solution to a problem for nurses to take blood on the orders of a doctor. With the increase in laboratory tests ordered by doctors to make timeous diagnoses, and a growing shortage of registered nurses at the patient's bedside, laboratories started employing nurses to perform phlebotomy procedures in hospitals. Phlebotomy procedures were therefore included in the skills taught as part of the requirements of the qualifications of nurses, however teaching time spent on performing a venepuncture may vary from one institution to another. Due to limited opportunities nurses have to obtain phlebotomy skills in the hospital setting, the focus of training has shifted from the venepuncture technique to accessing a vein for intravenous therapy (IV). Even if the nurse has many years of experience in starting an IV, a different approach is involved to perform a successful venepuncture (Ernst, 1998). The assumption has been that nurses are trained on phlebotomy procedures during their basic training, and once employed as a phlebotomist, they only receive in-service training delivered by older, more experienced nurses working at the laboratory. This has led to technique variations and the lack of a standardised training programme for nurses performing a phlebotomy procedure that is impacting on the quality of the test outcomes (Lima-Oliveira et al., 2012). Due to the differences in training outcomes between nurses and the phlebotomist technician, the competence and skill of nurses working as phlebotomists in the laboratory was questioned, when considering employing new "phlebotomists".
The nurse (phlebotomist) is the person responsible for ensuring specimen quality in the pre-analytical phase of laboratory testing. The collection process forms part of the pre-analytical phase where 60-70% of errors occur (Green, 2008). Samples collected by a human, are prone to errors as humans can err. Errors in the pre-analytical phase, especially during the specimen-collection process, may cause negative outcomes for the patient which range from financial implications to death. Complications associated with the collection process are preventable and are directly linked to the technique of the nurse or phlebotomist. An opportunity for errors is created when nurses lack knowledge about laboratory practices or do not have the appropriate skill to perform the necessary procedures. Lack of quality control might also be an issue (Ernst & Ballance, 2006). Two of the major complications that can occur due to improper technique are haemolysis and haemoconcentration. An example would be prolonged tourniquet application will resulting in haemoconcentration, where blood plasma infiltrates the surrounding tissue causing an increased concentration of protein-based analytes in the blood. It will go unnoticed when tested and the clinician will diagnose the patient based on the erroneous results. A haemolysed sample, detected by visual inspection of the sample and may be caused by usage of the wrong needle size, is unacceptable and unsuitable for testing and will result in the patient being re-bled (Ernst & Ballance, 2006).
Previous studies (Green, 2008, Hawkins, 2012, Lippi, 2009 and Sharma, 2009) investigated the errors that can occur if the wrong technique has been followed and indicate that it is vital to improve the quality of the service being rendered. Although all studies indicate training is vital (Lippi, Salvagno, Montagnana, Franchini, & Guidi, 2006), South Africa doesn't have a standardised training programme for nurses performing phlebotomy procedures. Ernst (2011) indicated that phlebotomy training must be of good quality so that the phlebotomist understands the implications of the wrong technique and errors in the pre-analytical phase's impact on test result outcomes.
Ernst (1998) stated that one of the four indefensible errors in phlebotomy is inadequate training. In South Africa, nurses performing phlebotomy procedures in the laboratory setting receive only in-service training or on the job training. The training programmes are developed by phlebotomy experienced nurses and are specific to that laboratory's policies. Training programmes for nurses vary not only between the different private laboratories but also from one region to another within a specific private laboratory group. Training and assessment for competency is not standardised, the nurses are also not trained on specific tests, the requirements for the tests and what may influence the outcome of those tests.
The best way to improve the quality of the specimens and to reduce errors whilst performing the procedures is to observe staff while they perform a venepuncture and identify the mistakes they make, and more importantly test their understanding of the impact of that particular error has on the outcome of the test (Ernst, 2011).
There is a dearth of literature on the effectiveness of training and whether training ensures competent and skilled staff. In a special report (Ho, Purdy, Adrian, Higa, & Cembrowski, 2002), researchers observed trained phlebotomists, with an average of 10 years experience, on their performance of venepuncture and found that out of 38 parameters monitored, they were noncompliant in 13 of them. Not allowing sufficient drying time for the disinfectant was at the top of the noncompliance list followed by re-palpation of the puncture site; contamination of the site and not cleaning effectively was also at the top of noncompliance together with wrong needle angle. These technique errors result in haemolysis and haemoconcentration (Strasinger & Di Lorenzo, 2011).
Based on the results of this study, it is clear that a standardised training programme is needed as well as regular assessment of competence (Ernst, 2011).
By conducting this study, the author aimed to investigate the feasibility of in-service training, presented in the workplace, for nursing staff on the venepuncture procedure. This study was therefore significant to all persons performing venepuncture procedures, providing a method on improving their phlebotomy skills. The laboratory will benefit because of the improved specimen quality and reduced number of sample rejections which ultimately, will benefit the clients (doctors and patients) who will receive quality results timeously.
2. Methods
2.1. Setting
A natural setting was chosen to observe nurses' behaviour in the workplace. This environment was familiar to them and comfortable, thus minimising the stressors of being assessed. It is very difficult to replicate the workplace in a simulated situation as stressors that occur on a daily basis cannot be predicted and replicated. Therefore data was collected at outpatient departments (depots) of a private laboratory, which are based at three private hospitals in the Gauteng South Region. The laboratory, which is the preferred service provider at these hospitals, has a 24-h lab (STAT-lab) on site performing emergency tests, with a high demand for pathology testing requiring more phlebotomy staff.
2.2. Population
The population consisted of registered nurses employed as phlebotomists on a permanent basis, based at the chosen laboratories: N = 35.
2.3. Sample
A total sampling method was used due to the limited number of full time employed registered nurses working at the laboratory. The realised sample size was 20 (n), or 57% of the population. The nurses who were not included in the final sample were either unavailable or refused participation and therefore did not sign consent.
The outpatient numbers were large due to the convenience of having a laboratory on site and enabled random selection of patients on whom the nursing staff could perform the venepuncture procedure. Every third adult patient who visited the Depot of the STAT laboratory and who agreed to participate was included. Random selection of patients excluded biases and favouritism from the nursing staff, and prevented nurses pre-empting which patient they were about to bleed.
2.3.1. Inclusion criteria
Only registered nurses permanently employed at the laboratory were considered for inclusion.
2.3.2. Exclusion criteria
Phlebotomy technicians were excluded from the study because of their intensive training programme. Enrolled Nurses employed by the laboratories, according to their scope of practice work under the supervision of registered nurses and were also excluded from the study.
2.4. Design
A quantitative, experimental, pilot intervention study was used for the purpose of this study. This methodology was thought to provide the most suitable guidance for the research questions. It determined the methods of data collection as well as the techniques and principles to apply when analysing the data.
Quantitative research: "is a formal, objective, systematic process in which numerical data are used to obtain information about the world. This research method is used to describe variables, examine relationships among variables, and determine cause-and-effect interactions between variables." (Burns & Grove, 2009).
Experimental research: The idea of experimental research is to compare two things with one another. There are three main categories of experimental designs identified namely: pre-experimental, quasi-experimental and true experimental. Differences between the experimental designs are the degree of control of the variables and if a comparison group was used or not. Experimental research provides a platform to conduct intervention studies as it allows the researcher to determine what is known about the study, subjects or intervention and to determine if there is any difference between before and after (De Vos, Strydom, Fouche, & Delport, 2013).
The one-group pre-test - post-test design (Burns & Grove, 2009) was used, which enabled the researcher to test if in-service training, the intervention, had an effect on the current phlebotomy practices of registered nurses (the participants). The goal of practice is to achieve 100% compliance to the standards. However, if the intervention made the nurses aware of their training needs and enabled them to reflect on their own practice, a positive outcome would be reached.
A pilot study can be seen as a small-scale version of the complete project, before a researcher attempts to conduct the research mainly to establish and rectify any discrepancies and also to determine the feasibility of the study (De Vos et al., 2013). The reasons for using a pilot study were to determine the feasibility in terms of cost involvement and practicality of the implementation of the intervention. Secondly to design a protocol describing how to implement the intervention and still assure quality within the laboratory setup.
Finally, because of the small number of available participants, a pilot study is done to gather information to answer the research questions (Burns & Grove, 2009).
A pilot study only provides limited information, however it still allows for identification of deficiencies that can be addressed (Burns & Grove, 2009).
Interventions are treatments or programmes that are implemented that will result in change of behaviour to improve quality of care. Intervention research aims to provide a platform for the generation of knowledge, nurses' use as evidence for best practices. Burns and Grove (2009).
2.5. Data collection
For the pre-test, nursing staff were video recorded by their peers whilst performing a venepuncture. To overcome the Hawthorne effect, where people change their behaviour because they are aware of being video recorded, it was decided to ask their peers (colleagues) to do the recording. Video recordings of human behaviour have certain benefits over in-person observation, which directed the decision to use recordings. Recordings are less threatening to the participants and minimise change of daily routine and behaviour. An added benefit of reviewing recordings is that it allows the reviewer the opportunity to stop, replay and make notes without interrupting the process, enabling improved judgements that an in-person observer might have missed (Paterson, Bottorff, & Hewat, 2003). The recordings were then reviewed by independent evaluators and scored against a criterion-based checklist to identify pre-analytical technique errors made by the nursing staff.
2.6. Instrument
There was no tool available for the purpose to assess competence for nursing staff on phlebotomy procedures at the laboratory. Therefore the first step was to check the feasibility of using an existing procedure evaluation instrument as a research tool. This instrument is currently used as a competence assessment tool of the phlebotomist technician learning programme.
To ensure content validity the recommendations of the WHO were followed to identify factors that influence the procedural steps of the procedure, checked by experts in the phlebotomy field, who made judgements on the inclusion of the various criteria. The changes made to the checklist were broken into smaller steps and were added to the tool.
The intervention for this study consisted of a training programme, which addressed the errors identified during the pre-test and was presented in the workplace, as presented in Fig. 1.
The training programme focused on the following aspects:
• The correct steps in the venepuncture procedure.
• Implications of variations in the procedure.
• Complications of variations in the procedure.
• Variations in the procedure's influence on the quality of the test outcome.
The training methodology was a group (peer) learning approach. No conceptual framework was followed; however Benner's principles of moving from novice to expert and Ericsson's deliberate practice were applied (Bordage, 2009). The nursing staff watched a ten-minute training video developed by the researcher explaining the steps of a venepuncture procedure (Chan, 2010). The nursing staff then watched their own performances and had to evaluate the procedure, finally giving feedback on the implications of wrong technique applications. A group discussion was held to derive best practices based on the evidence. Colleagues captured the video recordings of the pre-test so they had the opportunity to view their peers in action and it was also covered in the discussion session. The advantage of this was the immediate feedback on performance from their colleagues, which gave valuable insight on the way forward for on the job training (Norcini & Burch, 2007).
The post-test was conducted one month after completion of the intervention. The same procedure was followed as during the pre-test. The score of the post-test indicated to what extent the errors identified during the pre-test were eradicated.
2.7. Data analysis
Descriptive statistics were used to describe the calculated results within the mean and standard deviation. The recordings were not linked to a specific nurse for confidentiality reasons therefore a before and after profile cannot be created.
Two independent evaluators used the same criterion based observational evaluation form for both pre- and post-tests, to evaluate the video recordings. The total scores indicated the compliance level to the procedure standards. Obtaining feedback from the performing laboratory on the sample quality of all specimens collected during the time period of the study provided additional quality control. According to the error log control form used by the laboratory to report on rejections there was a decline in the number of rejected samples during the time period of the study. The researcher fulfilled the role of moderator, and reviewed the data collected to ensure all problems were identified and addressed in the training programme and that the post-test results gave a true reflection of the effectiveness of such a training programme.
2.8. Quality assurance
During data collection all recordings were captured on SD memory cards, one dedicated for the pre-test recordings and one for the post-test recordings. The video recorder has allocated a unique number for each recording that was transcribed on to the checklists used by the assessors. The results were moderated by the researcher for inconsistencies and discrepancies.
Both assessors who entered their results onto an Excel spread sheet managed digitisation and data entry and data checking. The assessors co-checked each other's data sheets before the researcher moderated the sheets.
2.9. Validity and reliability
Instrument validity ensures the instrument measures the concept (venepuncture procedural steps) and that it is measured accurately (De Vos et al., 2013).
Content validity was established by looking at the WHO's procedural recommendations for a venepuncture (WHO, 2010). It was followed by a literature review (Green, 2008, Hawkins, 2012, Sharma, 2009 and Strasinger and Di Lorenzo, 2011) on factors that influence the various steps of the procedure. As this study only focused on the venepuncture technique of the nursing staff members, non-applicable criteria were omitted from the original tool.
Face validity and reliability were established by running an in-vivo session with phlebotomy technicians (excluded from the study). The assessors used the tool to identify any problems with the content and steps in the procedure. The assessors, experts in the phlebotomy field, made judgements on the criteria used in the checklist. Changes were made based on their feedback, before using the criterion checklist for the video recordings.
During the in-vivo sessions the instructions were standardised and the instrument checked for consistency. The assessors' feedback stated that the tool proved easy to use and scoring was consistent, not only from one observation to the next but also the scores of the evaluators were similar which assured inter-rater reliability.
2.10. Ethical considerations
Emanuel, Wendler, Killen, and Grady (2004) identified ethical principles to be followed for research which includes the following:
• Anonymity: No patient or nursing staff member was identifiable as the video recordings only displayed the ante Cubital fossa area of the patient and the hands of the nurse. No identifiable content was captured as the study excluded the patient identification and labelling of the samples procedures, so there was no risk of compromising anonymity.
• Permission was granted by the Wits Human Research Ethics Committee (M130466) and the CEO of the laboratory group used in the study.
• Consent: was obtained from all nursing staff participating in the study and the patients from whom they drew blood, who were first given an information letter to read. Consent was obtained for participation in the study and a separate form was signed permitting to be video recorded. Participation was voluntary and no staff member or patient was forced to take part. They could also withdraw at any stage without prejudice.
• Data management: the pre-test and post-test recordings are kept in a locked cupboard together with the observation checklists. It will be destroyed after 5 years.
• Possible harm to patients: In the event the evaluator observed procedures that might be harmful to the patients, it was reported to the nursing managers of all the participating departments to address the issue. Only one incident was observed on the recordings, where a tourniquet was placed too tight that it left an imprint on the patient's arm. This was reported to all managers to address with their staff.
• There was no conflict of interest between the researcher and the participants, as the researcher was not employed at the lab and therefore had no influence on the career pathway of any of the participants.
• The training department of the laboratory sponsored the video camera and the memory cards used for data collection were purchased by the researcher to ensure confidentiality.
3. Results
The laboratory work experience of nurses in the laboratory setting ranged from seven months to 15 years, with six participants indicating they had worked in this setting for between seven months and two years; nine participants reported having worked longer than five years at the laboratory. Of the 20 participants, only six indicated that they had not attended a five-day laboratory orientation programme thus revealing they were self-taught. The participants who indicated attendance of a five-day orientation programme reported they had not changed their venepuncture technique or deviated from what they had been taught. However the six participants who did not attend an orientation programme reported having adapted their venepuncture technique over the years.
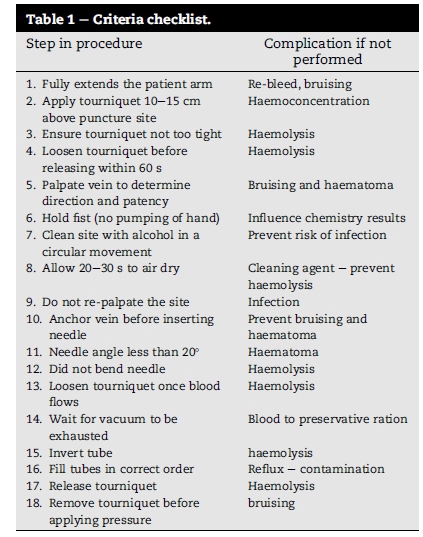
The pre-test and post-test consisted of video recordings which were measured against a criterion based checklist (Table 1). The checklist had 18 criteria, which the nursing staff had to perform during a venepuncture procedure. The performance of the participants during the pre-test averaged at 61.9%.
The participants' performance during the pre-test showed: the lowest performance by two participants who performed eight out of the 18 steps correctly and the highest performance by three participants performing 15 steps correctly (Refer to Fig. 2).
Less than 10 of the participants performed the following six steps correctly:
• Two participants anchored the vein correctly before needle entry preventing the vein to "roll" away and causing a possible haematoma.
• Five participants waited for the vacuum in the test tube to be exhausted and inverted the tube to mix the blood with the preservative, as per manufacturer instructions.
• Seven participants ensured that the tourniquet was not too tight around the patient's arm, preventing haemolysis.
• Eight participants waited for the cleaning agent to air dry before needle entry, limiting the risk for haemolysis.
• Eight participants did not re-palpate the area after cleaning the site preventing contamination and a possible infection.
• 9 Participants asked their patients to hold a fist and not to "pump the fist", preventing any erroneous chemistry results.
After the training programme was presented, the post-test was conducted. Performance of the participants during the post-test averaged at 85% and their performances in the post-test improved in all the steps when compared to the scores obtained in the pre-test (Refer to Fig. 3). One participant performed 12 steps correctly and had the lowest compliance score; on the highest compliance score, five participants performed 17 steps correctly.
The most significant improvement in performance of the individual steps was noted in the steps related to ensuring the tourniquet is not too tight and allowing time for the cleaning agent to air-dry. However re-palpating the site and anchoring the vein remained problematical.
Additional data received from the laboratory indicated there was a decline in sample rejection numbers from before the pre-test when a total number of 18 samples were rejected compared to the post-test period measured in October, when only six samples were rejected. In the month of November, a month after the intervention, only three samples were rejected. Unfortunately the total number of samples collected during this period is not available. However it would seem that the training programme had a positive effect on the efficiency of the laboratory testing process which relies on quality samples, with reasons for rejection being directly linked to sample quality.
4. Discussion
It was evident from participant responses that nurses with less than five years working experience had attended a more structured training programme than those working for more than five years. Underlining this statement is the nurses who attended a more structured training programme but did not change their technique from what they had been taught. The pre-test, with a low mean score of 61.9%, indicated that in-service training is required at regular intervals. Ernst (1998) reinforced this notion in his article "Four Indefensible Phlebotomy Errors and How to Prevent Them." As long ago as 1998 the importance of a good training programme in phlebotomy has been stressed. Despite this Ernst still remains the only author that addresses this issue. Ernst (1998) contends that training phlebotomy personnel is key to preventing mistakes and lawsuits, because ineffective training and evaluation of those performing venepunctures are indefensible in a court of law. Ernst also emphasised the importance of the regular evaluation of techniques in addition to well-designed and well-implemented training programmes. Ernst defines 'regularly' as within six months after completing a training programme and annually thereafter.
One of the objectives of this study was to determine the level of compliance of nurses working at the laboratory to the standard operating procedure of performing a venepuncture. The pre-test score of 61.9% indicates a deviation from the standard operating procedure on venepuncture and a third of the steps were performed poorly with anchoring the vein before needle insertion as the step least performed; only two participants stabilised the vein before needle insertion.
The post-test results show a different picture. With an average of 85% compliance it is clear the intervention had a positive influence on the nurses' performance. Although all steps of the procedure show an increase in frequency, there are still areas of concern. Some nurses are still re-palpating the puncture site after cleaning the area and the veins are still not anchored before needle entry.
Peer-assessment or evaluation allows the person to reflect on own practices and compare them to those of their colleagues, not only do they learn more about the task or skill, they learn about themselves which can lead to self-actualisation (Bothma, Brysiewicz, Chipps, Mthembu, & Phillips, 2014).
After the post-test, participants were given an evaluation form to complete and were asked three questions namely:
• What did you find valuable in the process?
• What changes are you planning to make as a result of this training?
• What have you learnt about yourself?
The feedback from the participants indicated that some valued this as a learning opportunity to improve their own performance as they observed the interaction with the patients as a complete entity. This is valuable as it shows reflection has taken place and assisted with acquiring practical knowledge and experiential reasoning (Barratt, 2010) internalising information and improving critical thinking.
In conclusion, the results from the pre-test compared to the post-test have improved however 100% compliance to the procedure was not reached. The short training programme given proved to have an effect as seen in the post-test results (85%). The steps in the procedure which were not performed might indicate that the participants still lack confidence in their own capabilities to access the vein with the first try. Confidence comes with experience and competence comes with practice. Having a system of regular observation of skill, even peer observation, can provide the platform to boost confidence as support and feedback are provided at the end of the performance (Barratt, 2010).
As phlebotomy is becoming a specialised skill, it is important to ensure nurses have the competence and the confidence to perform a venepuncture without hesitation. The training programme should therefore enhance skill and portray professionalism. This will motivate nurses working in the laboratory to become experts and specialists in their field, committing to life-long learning and caring for their patients by ensuring the best specimen is produced for testing.
4.1. Limitations of the study
This was a pilot study to test the feasibility and usefulness of the intervention. The following limitations were identified:
• Finding literature on nurses performing venepunctures proved difficult to find; research is done on the extra analytical phases of the laboratory process but not much is written on the collection process itself. Furthermore in the South African context no studies are done on the nurses' role in the laboratory.
• Due to policy changes in the laboratory during the study the number of nurses available to participate was limited.
• Difficulty was experienced in gaining cooperation from middle management at the beginning of the study managers were reluctant to permit access to the departments, but this was ultimately achieved.
• The study was conducted at three departments of one private laboratory group and is therefore contextual and limits generalisation of results.
4.2. Recommendations for research
To perform a longitudinal study to observe nursing and phlebotomy technicians over a period of time to determine to what extend techniques variations occur, and at what time interval in-service training should be attended to prevent technique variations which impact on sample quality.
Establish a standardised training programme within the field of pathology and to develop a practical and universal checklist for competence.
Investigations to determine to what extent the variations in technique impact on the quality of the specimen and ultimately the test results might be insightful to establish the compliance level to procedural instructions. Should it be 100% compliance to all steps, or can there be a difference in the weight each step carries when it comes to the influence they have on the test outcome?
5. Conclusion
Nurses traditionally formed the core of the phlebotomy services but have gradually been replaced by specially trained phlebotomy technicians. This study has shown that there are deficits in the skills of phlebotomy nurses but, as phlebotomy technicians were not included in the study, it is not known whether similar deficits exist amongst these specifically trained personnel. Current practice is that nurses provide training to the phlebotomy technicians so it is likely that if they, the nurses, are not 100% compliant with standards and criteria, phlebotomy technicians will follow suit.
This study has shown that peer teaching is effective and although the study was small, it gives a clear indication it is a useful and necessary way of improving competencies of nurse phlebotomists to ensure patient safety, cost-effective services and improved training of phlebotomy technicians.
References
Barratt, J. (2010). A focus group study of the use of video-recorded simulated objective structured clinical examinations in nurse practitioner education. Nurse Education in Practice, 10, 170e175. [ Links ]
Bordage, G. (2009). Conceptual frameworks to illuminate and magnify. Medical Education, 43, 312e319. [ Links ]
Bothma, Y., Brysiewicz, P., Chipps, J., Mthembu, S., & Phillips, M. (2014). Creating stimulating learning opportunities (pp. 175e176). Pearson. [ Links ]
Burns, N., & Grove, S. K. (2009). The practice of nursing research: Appraisal, synthesis, and generation of evidence (6th ed., p. 257).Elsevier. [ Links ]
Chan, Y. M. (2010). Video instructions as support for beyond classroom learning. Procedia Social and Behavioral Sciences, 9, 1313e1318. [ Links ]
De Vos, A. S., Strydom, H., Fouche, C. B., & Delport, C. S. L. (2013). Research at grass roots (4th ed., pp. 142e177). Van Schaick Publishers. [ Links ]
Emanuel, D. J., Wendler, D., Killen, J., & Grady, C. (2004). What makes clinical research in developing countries ethical? the benchmarks of ethical research. The Journal of Infectious Diseases, 189, 930e937. [ Links ]
Ernst, D. J. (1998). Four indefensible phlebotomy errors and how to prevent them. Journal of Healthcare Risk Management, 18(2), 41e46. [ Links ]
Ernst, C. (September 2011). Phlebotomy training: Does your program pass the test. Medical Observer Laboratory, 36e38. [ Links ]
Ernst, D. J., & Ballance, L. O. (2006). Quality collection: The phlebotomist's role in pre-analytical errors. Medical Observer Laboratory, 31e38. [ Links ]
Green, S. (2008). Improving the pre-analytical process: The focus on specimen quality. Journal of Medical Biochemistry, 27, 343e347. [ Links ]
Hawkins, R. (2012). Managing the pre- and post-analytical phases of the total testing process. Annals of Laboratory Medicine, 32, 5e16. [ Links ]
Ho, A., Purdy, L., Adrian, B., Higa, T., & Cembrowski, G. (2002). Measurement of variation in videotaped outpatient phlebotomies. Laboratory Medicine No 3, 33, 179e185. [ Links ]
Lima-Oliveira, G., Lippi, G., Salvagno, G., Montagnana, M., Picheth, G., & Guidi, G. (2012). Impact of the phlebotomy training based on CLSI/NCCLS H03-A6 e Procedures for the collection of diagnostic blood specimens by venipuncture. Biochemia Medica, 22(3). [ Links ]
Lippi, G. (March 2009). Governance of preanalytical variability: Travelling the right path to the bright side of the moon? Clinica Chimica Acta, 32e36. [ Links ]
Lippi, G., Salvagno, G., Montagnana, M., Franchini, M., & Guidi, G. (2006). Phlebotomy issues and quality improvement in results of laboratory testing. Clinical Laboratory, 52. [ Links ]
Mbah, H. A. (2014). Phlebotomy and quality in the African laboratory. African Journal of Laboratory Medicine, 3(1). Art.#132. [ Links ]
Norcini, P., & Burch, V. (2007). Workplace-based assessment as an educational tool: AMEE guide No. 31. Medical Teacher, 29, 855e871. [ Links ]
Paterson, B. L., Bottorff, J. L., & Hewat, R. (2003). Blending observational methods: Possibilities, strategies and challenges. International Journal of Qualitative Methods, 2(1), 29e38. [ Links ]
Presley, C. H., & Liotta, M. (August 2006). How and Why to start inhouse phlebotomy training. Medical Laboratory Observer, 48e49. [ Links ]
Sharma, P. (2009). Preanalytical variables and laboratory performance. Indian Journal of Clinical Biochemistr, 24(2), 109e110. [ Links ]
Strasinger, S., & Di Lorenzo, M. (2011). The phlebotomy textbook (3rd ed., pp. 187e334). Philadelphia: F.A. Davis Company. [ Links ]
WHO guidelines on drawing blood: Best practices in phlebotomy.(2010). [ Links ]
Received 18 February 2016
Accepted 30 June 2016
Available online 11 September 2016
E-mail addresses: Lizelle.Crous@wits.ac.za (L. Crous), Sue.Armstrong@wits.ac.za (S.J. Armstrong).
Peer review under responsibility of Johannesburg University.
* Corresponding author. Fax: +27 11 488 4195.
1 Contribution - 90% - writing up of research project.
2 Contribution - 10% - editing and writing of conclusion.














