Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
Health SA Gesondheid (Online)
On-line version ISSN 2071-9736
Print version ISSN 1025-9848
Health SA Gesondheid (Online) vol.21 n.1 Cape Town 2016
http://dx.doi.org/10.1016/j.hsag.2015.08.001
Keep pushing! Limiting interruptions to CPR: bag-valve mask versus i-gel® airway ventilation
Craig Vincent-Lambert*; Andrew Makkink1; Fredrick Kloppers1
Department of Emergency Medical Care, Faculty of Health Sciences, University of Johannesburg, Doornfontein Campus, PO Box 17011, Doornfontein, 2028, South Africa
ABSTRACT
BACKGROUND: Recent recommendations made by ILCOR have de-emphasised the role of advanced airway management such as "endotracheal intubation" (ETI) during cardiac arrest in favour of maximising the number of chest compressions performed by rescuers. Maximising time available for compressions is achieved by minimising hands-off time (HOT). This has led to first responders and paramedics performing single rescuer CPR using a bag-valve-mask (BVM) device as opposed to the historical practice of intubating and ventilating via an endotracheal tube. Bag-valve-mask ventilations, especially during single rescuer CPR, are however associated with complications potentially resulting in increased ventilation times. More time spent on ventilations in the single rescuer scenario naturally leads to an increase in HOT and less time being available for compressions. It is postulated that the use of an appropriate supraglottic airway device (SAD) may decrease the time spent on the ventilation component of CPR and result in a decrease in HOT
OBJECTIVES: This pilot study evaluated how interruptions to chest compressions or hands-off time (HOT) are affected by the placement of an i-gel® airway vs. simple BVM ventilation during single rescuer CPR
METHOD: 16 participants performed two, ten-minute single rescuer CPR simulations, firstly using the BVM and later the i-gel® airway for ventilation. Data pertaining to ventilations and HOT in each scenario was statistically analysed and compared
RESULTS: The i-gel® airway demonstrated a superior ease of ventilation compared to BVM alone and resulted in a reduction of time spent on ventilations overall. The i-gel® however took a mean of 29 s, ± 10 s, to secure which contributes considerably to HOT
CONCLUSION: The use of the i-gel® airway resulted in a considerable decrease in the amount of time spent on ventilations and in more compressions being performed. The overall reduction in HOT was, however, offset by the time it took to secure the device. Further investigation into the use and securing of the i-gel® airway in single rescuer CPR is recommended
Keywords: CPR, Airway managment, Cardiac arrest
1. Introduction
This study compared differences in HOT between single rescuer CPR using a BVM and single rescuer CPR using the i-gel® airway with reference to a) chest compressions, b) cycles of CPR, and c) time taken to assess and secure the airway and ventilate using an i-gel® SAD.
1.1. Background
In South Africa, heart disease and sudden cardiac arrest is on the increase. When cardiac arrest occurs the prognosis is poor unless effective resuscitation measures are rapidly initiated. The International Liaison Committee on Resuscitation (ILCOR) strives to promote prompt and skilful responses to cardiac arrest that can make the difference between life and death. Every five years ILCOR convenes to review the latest literature and science regarding CPR and to reach consensus on treatment recommendations (Hazinski et al., 2010). Over the past five years, ILCOR has de-emphasised the role of endotracheal intubation (ETI) in CPR, and re-emphasised the importance of maximising the number of chest compressions and limiting sources of hands-off time (HOT) during CPR (Berg et al., 2010).
The above recommendations, however, assume that a single rescue scenario is unlikely to persist for a considerable length of time. The South African scenario is somewhat different to both the American and European models, in that many advanced life support (ALS) paramedics work alone on a primary response vehicle (PRV) and are therefore commonly required to manage cardiac arrest cases alone until the ambulance crew arrives. Taking the recent ILCOR recommendations into account, local ALS paramedics are performing single rescuer ventilations during CPR with a BVM apparatus as opposed to the historical practice of ETI which is seen to create an opportunity for significant HOT.
Having said this, bag-valve-mask (BVM) ventilations, especially those being performed during single rescuer CPR, are associated with many complications. These include gastric insufflation, aspiration and delays associated with repeated attempts at positioning and opening the airway together with difficulties in obtaining an appropriate face-mask seal. All of these complications may result in an increase in the time spent attempting to provide rescue breaths during CPR. More time spent on ventilations in the single rescuer scenario naturally leads to less time being available for compressions (Berg et al., 2010).
1.2. Problem statement
Evidence indicates that interruptions to chest compressions or hands-off time during single rescuer CPR are undesirable and negatively impact on cardiac output (Hazinski et al., 2010). The time spent securing the airway and providing ventilations during CPR serves as a source of interruption to chest compressions or HOT. Limited data currently exists to support one form of airway management above the other during CPR and that airway management strategies should be adapted to the specific circumstances surrounding CPR. Increases in HOT during CPR lowers the likelihood of achieving a return of spontaneous circulation (ROSC) and survival. CPR techniques where HOT is minimised are preferable and certain ventilation techniques may be beneficial to decreasing time spent on ventilations. Prior to this study no data existed comparing HOT during CPR with BVM ventilation to HOT during CPR using a supraglottic airway device.
1.3. Aim
The aim of this study was to determine whether or not the insertion of an i-gel® airway during single rescuer CPR would minimise HOT compared to single rescuer CPR using only a BVM.
1.4. Literature review
1.4.1. Hands-off time
Hands-off time is defined as any period of time during CPR that there is a cessation in the performance of chest compressions (Nolan et al., 2010). End organ perfusion pressure decreases with the cessation of chest compressions and it may take a significant number of compressions to regain adequate end organ perfusion after a period of HOT. Disruptions to chest compressions should therefore be limited as far as possible in order to promote blood flow and adequate end organ perfusion (Perkins, Brace, Smythe, Ong, & Gates, 2012).
A direct correlation exists between the fraction of each minute of CPR spent performing chest compressions and the incidence of ROSC (Christenson et al., 2009). Limiting the frequency and duration of interruptions in chest compressions may improve the incidence of ROSC and clinically meaningful outcomes in cardiac arrest patients (Abella et al., 2005; Christenson et al., 2009; Eftestol, 2002). Similarly, findings suggest that CPR should focus primarily on chest compressions and that time taken for airway management during CPR may have a negative effect on ROSC (Bobrow et al., 2008).
1.4.2. Airway management during CPR
Periodic ventilation during CPR is an important component of the resuscitation sequence as it brings about oxygenation of lung tissue (Perkins et al., 2012). However, during cardiac arrest, a lower minute volume is required to achieve normal oxygenation of organ tissues. This is based on the fact that pulmonary perfusion is only 25%-30% of normal during optimal CPR, resulting in oxygen uptake from the pulmonary circuit being significantly reduced (Perkins et al., 2012). A literature shift regarding the importance of ventilation in CPR has occurred, with the emphasis falling on the circulation component (Berg et al., 2010). Excessive ventilation during CPR has been proven to be detrimental to patients, resulting in poorer outcomes (Aufderheide et al., 2004). Another function of airway management during CPR is the protection of the airway against pulmonary aspiration of gastric contents. It has been reported that as many as 12% of patients aspirate at some point during the resuscitation effort (Berg et al., 2010; Stone, Chantler, & Baskett, 1998).
Preceding 2005, ETI was regarded as the gold standard for airway management during CPR (Zaritsky & Morley, 2005). The importance of ETI during CPR has, however, recently been deemphasised as it was not shown to improve outcome (Hazinski et al., 2010; Zaritsky & Morley, 2005). Endotracheal intubation performed during CPR is not associated with an improved outcome with regard to ROSC, and has been shown to increase HOT significantly (Don Michael, 1985; Wang, Simeone, Weaver, & Callaway, 2009). Today, airway devices such as SAD are viewed as acceptable alternatives to ETI during CPR, as they provide easy and rapid insertion with good seal pressures (Don Michael, 1985; Hazinski et al. 2010; Ruetzler et al. 2011; Yannopoulos & Aufderheide, 2007).
The NCBI database was searched using the terms "randomized" and "controlled" and "ventilation" and "CPR".No randomised trials could be found to support one form of airway management strategy above the other during patient CPR. The only clear recommendation made by ILCOR regarding airway management strategies during CPR is that these strategies should be adapted to the specific circumstances surrounding CPR, and that airway management should not prolong HOT (Hazinski et al., 2010).
1.4.3. Single rescuer CPR and HOT
Single rescuer CPR should be aimed at good quality CPR with minimal interruptions in chest compressions occurring (Abella et al., 2005; Bobrow et al., 2008; Eftestol, 2002; Hazinski et al., 2010). The 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardio-vascular Care highlight that the provision of quality compressions that are minimally interrupted remains the main objective of single rescuer CPR (Berg et al., 2010).
Kern, Hilwig, Berg, Sanders, and Ewy (2002) and Hilwig et al. (2002) conducted an animal study in order to assess the effect that interruptions in chest compressions had on the incidence of ROSC in chemically induced ventricular fibrillation. The incidence of ROSC and 24-h post-resuscitation survival was measured with the application of a conventional single rescuer CPR protocol involving periodic ventilations as well as a protocol focusing on compressions. The authors found that interruptions in chest compressions during single rescuer CPR were inversely related to the incidence of ROSC, and that the incidence of 24-h post-resuscitation survival was three times higher in the protocol focusing on compressions. The conclusion was that during single rescuer CPR, rescue breaths may be detrimental to the incidence of ROSC and 24-h survival, as the rescue breaths caused excessive HOT. The study concluded that any changes in CPR technique/sequence that minimised HOT in the first ten minutes of CPR, should be seriously considered, especially pertaining to airway management (Kern et al., 2002).
Through the use of a manikin-based study, Wiese and Bartels et al. measured the effect that an adaptation of airway management strategies had on HOT during single rescuer CPR (Wiese et al., 2008). Single rescuer CPR was performed using a BVM apparatus, and then again using a laryngeal tube. HOT was found to decrease by 30% through the insertion of a laryngeal tube during single rescuer CPR (Wiese et al., 2008). This was the only study encountered that provided data on HOT during an entire single rescuer CPR sequence (Wiese et al., 2008). Other studies only measured insertion time of airway devices during active compressions and extrapolated the data to HOT (Ruetzler et al., 2011).
1.4.4. Bag-ualue-masfe ventilations during CPR Bag-valve-mask ventilation is used to provide to provide positive pressure ventilation to a patient. Fig. 1 is an example of a typical BVM. BVM ventilation is associated with complications such as aspiration of gastric contents. Difficult mask ventilation (DVM) is described as "difficulty in finding an appropriate seal between the mask and the patient's face" (Kovacs & Law, 2007). During DMV, the rescuer has to repeatedly reposition the mask, hyperextend the patient's head (provided that there is no suspected neck injury) and adjust the pressure they apply to the facemask in order to provide an effective seal between the mask and the patient's face thereby assisting in the facilitation of effective ventilations. The incidence of DMV has been reported to be as high 5% in the general population undergoing routine anaesthesia in a controlled environment (Langeron, Masso, Huraux, & Guggiari, 2000). DMV is more likely in the case of a single person resuscitation, as it becomes increasingly difficult to achieve an adequate seal between the mask and the patient's face with one hand and squeeze the bag with the other (Dörges, Wenzel, Neubert, & Schmucker, 2000)(Yannopoulos & Aufderheide, 2007).
Bobrow and Ewy et al. found that positive pressure ventilations performed during out-of-hospital cardiac arrest may adversely affect outcome. In 1019 OHCA cases involving ventricular fibrillation, the authors found that CPR with passive oxygen insufflation had a 12.4% greater incidence of ROSC than a conventional CPR protocol involving periodic positive-pressure BVM ventilations (Bobrow et al., 2009).
1.4.5. CPR and supraglottic airway devices (SADs)
The use of SADs during CPR provides an alternative form of airway management to BVM, as BVM is known to be associated with many complications such as DMV (Doörges et al., 2000; Hazinski et al., 2010; Stone et al., 1998; Wiese et al., 2008; Yannopoulos & Aufderheide, 2007). Some of these SADs include the laryngeal mask airway (LMA) and the laryngeal tube (Doörges et al., 2000). These may serve as alternative means of providing ventilation, as they are associated with a lower incidence of complications such as DMV and gastric insufflation (Yannopoulos & Aufderheide, 2007). The i-gel is a type of SAD that was used in this study. Fig. 2 is a depiction of the i-gel.
In 2008 Wiese and Bartels measured the effect that the insertion of a laryngeal tube had on HOT during single rescuer CPR and found that BVM ventilations increased ventilation time and gastric insufflation compared to ventilations via the laryngeal tube during single rescuer CPR (Wiese et al., 2008).
Doörges and Wenzel et al. conducted a study aimed at determining the feasibility of alternative airway devices, including SAD, as well as ETI used during CPR. They concluded that ETI as well as SAD provided an acceptable alternative form of ventilation to BVM during CPR, based on the fact that SAD and ETI remove DMV and other complications such as gastric inflation. The study also concluded that ETI as well as SAD resulted in an overall decreased ventilation time by mitigating the effects of DMV (Doörges et al., 2000).
1.4.6. Insertion times of alternative airway devices and the endotracheal tube
In 2011, Ruetzler and Gruber et al. conducted a study to measure the insertion time of different SADs during on-going chest compressions performed on manikins. They compared the insertion times of ETI, the LMA, the Easy Tube®, the laryngeal tube as well as the i-gel® airway (Ruetzler et al., 2011). A measurement of the time taken to insert the various devices successfully during ongoing chest compressions was performed and the data was extrapolated to HOT occurring during CPR. The authors concluded that all SADs used in the study, including the i-gel® airway could be used as alternative forms of ventilation and that the i-gel® airway was inserted in a mean time of only 15.9 s, which was more or less the same time it took to insert the LMA (Ruetzler et al., 2011).
Castle and Owen et el conducted a manikin-based study in which they measured the insertion times of different SADs and found that the devices ranked from fastest to slowest insertion times in the following order: i-gel® airway, laryngeal tube airway and lastly LMA. The median insertion times for the devices were as follows: 12.3s (i-gel® airway), 23.4s (laryngeal tube airway), and 33.8.s (LMA). The study concluded that the i-gel® airway is an acceptable alternative to BVM during CPR. In an interview, participants commented on the fact that they were impressed by the ease and speed at which the insertion of the i-gel® airway occurred. During the interview of the participants, the i-gel® airway was found to be the favourite option with 63% of the participants finding it the easiest SAD to insert (Castle, Owen, Hann, Naidoo, & Reeves, 2010).
Gatward and Thomas et al. found similar results in a manikin-based study that measured insertion times of SADs during CPR in order to measure how airway placement is affected by active chest compressions. The insertion time for the i-gel® airway was found to be 50% shorter than that of an LMA Classic and the median insertion time for an i-gel® airway was found to be only 7 s. The study also commented on the importance of minimising insertion time in order to minimise HOT during CPR. The conclusion was that the i-gel® airway served as a viable alternative to BVM during CPR (Gatward et al., 2008).
1.4.6.1. The i-gel® airway. The above literature indicates that the i-gel® airway is associated with a significant ease of insertion and takes a significantly shorter time to insert compared to any other SAD (Castle et al., 2010; Gatward et al., 2008). The i-gel® airway is a single use SAD with a non-inflatable cuff, and a relatively new addition to the range of SAD available today (Asai & Liu, 2010; Jindal, Rizvi, & Sharma, 2009; Kannaujia et al., 2009; Levitan & Kinkle, 2005; Richez, Saltel, Banchereau, Torrielli, & Cros, 2008). The efficiency and safety of the i-gel® airway has been tested over the four years since its release onto the market (Richez et al., 2008). The i-gel® airway is made of a gel-like rubber compound that is designed to mold to the soft tissues of the perilaryngeal soft tissues in order to create an appropriate seal with the hypo-pharynx (Levitan & Kinkle, 2005). The gel-like material that it is composed of conforms well to the perilaryngeal soft tissues, producing appropriate device placement and seal (Jindal et al., 2009; Levitan & Kinkle, 2005). In a cadaver study, the i-gel® airway caused sufficient glottic opening in 83% of insertions and covered the laryngeal inlet in 100% of insertions performed (Levitan & Kinkle, 2005). The position of the i-gel® has also been found to be consistently stable during movement of the patient's head and neck (Kannaujia et al., 2009).
Kannaujia and Srivastava et al. found that in more than 100 cases of i-gel® airway insertion, successful first attempt insertion occurred in 90% of the cases and that in the other 10% of cases, only one more attempt was necessary for successful placement (Kannaujia et al., 2009).
Wharton and Gibbison also measured the safety and efficacy of the i-gel® airway and found that the i-gel® airway was inserted in manikins in a median time of 14 s with good peak airway and seal pressures. Moreover, the i-gel® airway was correctly placed within the first attempt in 88% of the participants. The study concluded that the i-gel® airway can safely be used as a SAD in patients but that its role in CPR requires further study (Levitan & Kinkle, 2005).
1.4.7. BVM versus i-gel airway ® during single rescuer CPR No literature could be found that compared BVM versus the i-gel® airway. The 2010 ILCOR treatment guidelines state the following regarding airway management during CPR: "There were no randomised trials that assessed the effect of airway management with bag valve mask versus any other form airway management including endotracheal intubation of adult victims in cardiac arrest" (Hazinski et al., 2010). This statement indicates a lacuna in the available literature on airway management as a whole during CPR. This research report aims to deal with this knowledge gap by providing new information regarding BVM versus the i-gel® airway and the effect that both techniques have on HOT during single recue CPR.
2. Research method and design
2.1. Design
The study was carried out as a prospective, non-randomised, paired design with self-controls. This particular design enabled each participant to act as their own control in two separate simulations. The design allowed the researcher to measure the difference in hands-off time (HOT) brought on by the insertion of the i-gel® airway, by comparing the HOT of each participant during two separate simulations.
2.2. Population and sample
The 16 participants were registered third- or fourth-year students in the Department of Emergency Medical Care who had been approached by the researcher to participate and had consented to involvement in the study. All participants were familiar with the SimMan 3G high fidelity manikin and its working and had been exposed to an i-gel® training video and had an opportunity to practice its insertion. First- and second-year students were purposefully excluded as proficiency in the application and use of the i-gel® airway is only expected from the third year of study.
The simulation containing single rescuer CPR with a BVM served as the control simulation. The simulation using the i-gel® airway was considered the experimental simulation. As rescuer fatigue may have influenced chest compression rate and quality, the control and experimental simulations were conducted on two separate days, at least one calendar week apart (Ashton, McCluskey, Gwinnutt, & Keenan, 2002; Heidenreich et al., 2006; Manders & Geijsel, 2009; Sugerman et al., 2009; Wharton et al., 2008). On the day of the experimental simulation, each participant was provided with a video tutorial on the use of the i-gel® airway. This video tutorial was by the manufacturer and was in accordance with manufacturer guidelines. After viewing the video footage, the participant was given an opportunity to practise the insertion of the i-gel® airway using Laerdal® airway trainers.
2.3. Materials
A camera was placed at the simulation manikin's (SimMan® 3Gs) feet to record video footage of the simulation for retrospective analysis. During the simulations, participants were provided with a medical jump bag containing an ECG, adult BVM, appropriately sized oropharyngeal tubes (OPT) and an i-gel® airway placed in its packaging. A one-meter segment of 1.5 cm thick, linen trachy tape and a tube of water-based lubricant were also provided to each of the participants.
2.4. Data collection
A personal computer was connected to the manikin. During the simulation, the SimMan® 3G software program provided the following information: a) the duration of the simulation, b) the number and quality of compressions completed, c) the number of ventilations provided, pulse checks, and d) the time that chest compressions were started and ended. Time from commencement to conclusion of each scenario was ten minutes.
2.5. Data analysis
Raw data was transferred onto Microsoft Excel® worksheets. The mean and standard deviation were calculated using the statistical functions of the Microsoft Excel program. The paired t-test was used to determine statistical significance as it was the most relevant test for the methodology of this study. A 95% confidence interval was used to determine the statistical value of the data.
2.6. Context of the study
The study was conducted in August 2012 at the University of Johannesburg in the clinical training facilities of the Department of Emergency Medical Care.
3. Results
3.1. Duration of various activities during control and experimental simulations
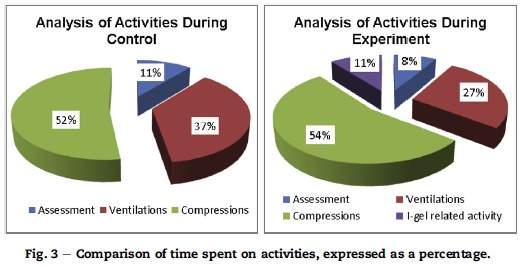
All participant data was combined and used to calculate a mean time spent on each activity. Each of the control simulations was divided into the activities of initial patient assessment, ventilations and compressions, while each of the experimental simulations was divided into initial patient assessment, ventilations, compressions and i-gel® related activities.
Fig. 3 shows the time spent on assessment of the patient and decreased from 11% of the total simulation time in the control, to 8% of the total simulation time in the experiment. The time spent on ventilations decreased from 37% of the simulation in the control, to 27% of the simulation in the experiment. The time spent on the performance of chest compressions increased from 52% of the simulation in the control to 54% of the simulation in the experiment. A mean of 63 s was used for i-gel® related activity in the experimental simulations. This correlates to 11% of experimental simulation time having been spent on preparing, inserting, securing and confirming the placement of the i-gel® airway device.
3.2. Overview of i-gel® related activity
Participants spent a mean of 63 s, ± 14 s, on i-gel® related activity. This translated to 11% of each experimental simulation involving some form of activity related to the i-gel® airway. All activity involving preparation, insertion, securing and confirmation of the i-gel® was also included in HOT, as it directly resulted in the cessation of the performance of chest compressions.
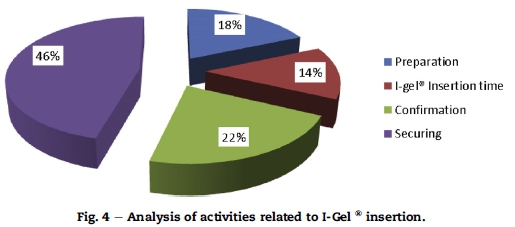
I-gel® related activity was divided into four categories, namely preparation of the device for insertion purposes, the actual insertion of the device, the securing of the device and confirmation of its correct anatomical placement via auscultation with a stethoscope.
Fig. 4 illustrates the percentage of time that each of the i-gel® related activities occupied within the overall i-gel® related activity. The percentage of the time used to prepare the device was calculated at 18%, with the percentage associated with device insertion, only totalling 14%. The percentage of the time associated with the confirmation of the device's placement was calculated at 22%. Almost half of the overall time associated with i-gel® related activity occurred as a result of securing the device (46%). Fig. 5.
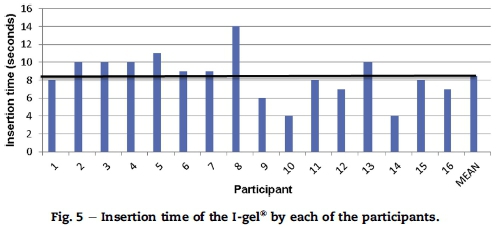
3.3. Insertion of the i-gel®
All participants (100%) inserted the i-gel® successfully on the first attempt. The mean insertion time for the i-gel® was found to be 8 s, ± 3s.
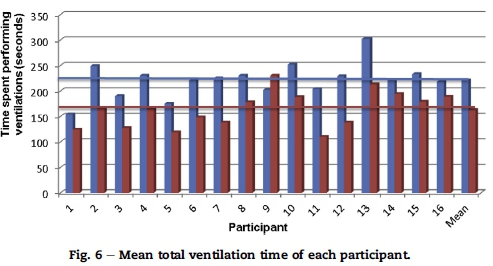
3.4. I-gel® airway and ventilation time
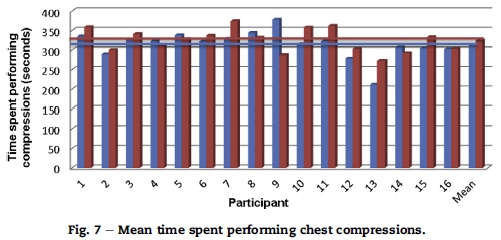
Fig. 6 illustrates the difference in time spent on ventilations during their control and experimental simulations. The time spent performing ventilations decreased by 10% from the control simulation using a bag-valve-mask BVM, to the experimental simulation using the i-gel®. With the insertion of the i-gel®, the total time spent performing ventilations decreased from 221 s, ± 34 s, in the control simulation, to 163 s, ± 35 s, in the experimental simulation, a decrease of 58 s. The mean time spent performing ventilations per cycle of CPR also decreased from 10 s, ±2 s, during the control simulation, to 7 s, ±2 s, as recorded during the experimental simulations (Fig. 7).
3.5. The i-gel® airway and compressions cycles
The results of the study indicated that during the control simulations, participants performed compressions for a mean of 313 s, ±36 s. During the experimental simulations, participants performed compressions for a mean of 324 s, ±30 s. The participants therefore performed compressions for a total of 11 s longer during the experimental simulations (2% of total simulation time). Fig. 8.
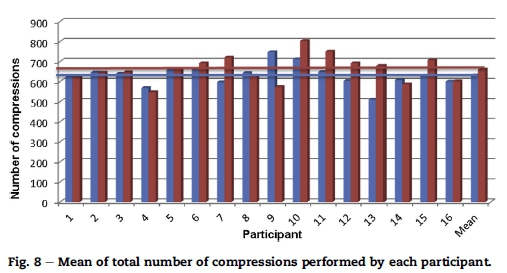
Participants performed a mean of 21, ±2, compressions cycles in the control, and a mean of 22, ±2, compression cycles during the experiment. Participants performed a greater number of compressions during the experimental simulations. They performed a mean of 631, ±54, compressions in the control and a mean of 660, ±67, compressions during the experiment.
3.6. Hands-off time
The values represented by the bars in Fig. 9, indicate the total HOT for each participant out of each of the ten-minute simulations. The mean HOT calculated from the individual HOT of all the different participants was calculated to be 286 s, ± 36 s, during the control simulations. The mean overall HOT for all the participants calculated during the experimental simulations was calculated to be 276 s, ± 30 s (difference in overall HOT of 10 s). The mean HOT per cycle of CPR was also calculated to have decreased from 13 s, ±3 s, in the control simulations to 12 s, ± 2 s, for the experimental simulations.
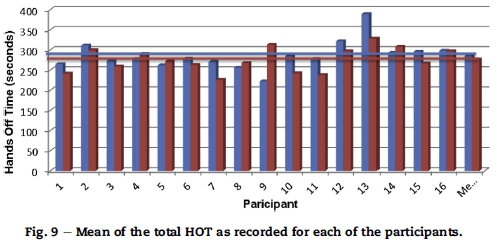
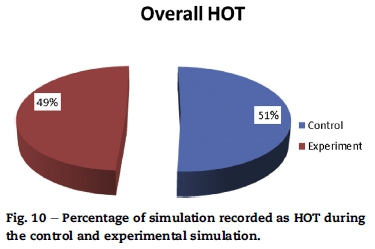
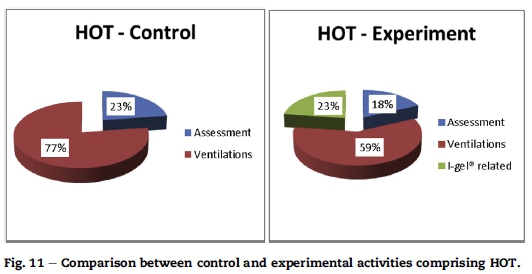
Fig. 10 illustrates the overall percentage of each of the simulations consisting of HOT. It indicates that the insertion of the i-gel® during the experimental simulations resulted in a decrease in overall HOT from 51% in the control simulations to of 49% in the experimental simulations. Although this may not seem significant, it is the reasons for this similarity that are significant, specifically those related to activities performed during the i-gel® insertion (Fig. 11).
3.7. I-gel® and HOT
Time spent performing ventilations decreased significantly during the experimental simulations. During the control simulations, 77% of HOT was attributed to the performance of ventilations. This is in comparison to the 59% of HOT that was attributed to the performance of ventilations during the experimental simulation.
The experimental simulation contained a segment of activity not contained within the control simulation. The experimental simulation contained a segment of activity that contributed to 23% of HOT which did not occur in the control simulations (i-gel® related HOT activity: 63 s, ± 14 s). This means that the use of the i-gel® airway during the experimental simulations resulted in significant decreases in ventilation time (thereby decreasing HOT), but at the same time introduced a new element of HOT in the form of i-gel® related HOT activity.
4. Discussion
4.1. The use of the i-gel® airway device introduced a new category of HOT during the experimental simulations
Participants spent a mean 63 s, ± 14 s, on i-gel® related activity. This translated to 11% of each experimental simulation involving some form of activity related to the preparation, insertion, securing and confirmation of the i-gel®. All these activities were included in hands-off time (HOT) as this was a single-rescuer scenario, and all activity involving the airway device directly resulted in a cessation in the performance of chest compressions. Participants took a mean of 12 s, ± 6 s, in order to prepare the device for insertion, whilst taking a mean time of 8 s, ± 3s,toinsert the device successfully. This translated to 18% of the overall i-gel® related HOT occurring as a result of preparation, with only 14% of the same total occurring as a result of the actual insertion of the device. Participants took a mean of 14 s, ± 5 s, to confirm the device's correct placement via auscultation (22% of overall i-gel® related HOT). A considerable amount of time was taken to secure the device using trachy tape (mean of 29 s, ± 10 s). The vast majority of HOT accumulated during i-gel® related activity was as a result of securing the airway device (46% of total i-gel® related HOT).
4.2. The use of the i-gel® airway changed the distribution oftime spent on the activities ofassessment, ventilations and compressions
The insertion of the i-gel® airway in the experimental simulations changed the mean distribution of time that each participant spent on the various activities of assessment, ventilations and compressions.
4.3. The use of the i-gel® airway decreased the time spent on ventilations
With the insertion of the i-gel®, the total time spent on ventilations decreased from a mean of 221 s, ± 34 s, in the control simulation, to 163 s, ± 35 s, in the experimental simulation, representing a decrease of 58 s overall. During each cycle of ventilations the i-gel® decreased time spent on ventilations per cycle of CPR by 3 s. Overall time spent on ventilations, as well as ventilation time per cycle of CPR, decreased quite considerably from the control to the experimental simulations. The total time spent performing ventilations decreased by 10% from the control simulation using a BVM to the experimental simulation using the i-gel®.
The above results indicate that the decrease in time spent performing ventilations was caused by the i-gel® removing difficulties related to BVM ventilations. From the video footage gathered during data collection, it could easily be seen that the i-gel® simplified ventilation cycles as the BVM was already attached to the airway device and did not have to be picked up off the floor. Also, no mask had to be positioned over that patient's face, due to the supraglottic placement of the airway device, further shortening ventilation time. No literature regarding the abovementioned inferences could be found, reinforcing the study's usefulness as a pilot study.
4.4. The use of the i-gel® airway resulted in a greater number of compressions being performed
The results indicate that the participants performed more compressions during the experimental simulation using the i-gel® airway. The latest international CPR guidelines have shifted their focus to the circulation component of the resuscitation sequence, placing an emphasis on the number of chest compressions performed (Hazinski et al., 2010). The use of the i-gel® thus supports latest CPR recommendations with regard to the number of compressions performed, as it resulted in more compressions being performed during the experimental simulations despite the delays associated with securing the i-gel®.
4.5. The impact ofthe i-gel® airway on overall HOT
Although the use of the i-gel® resulted in a decrease in time spent performing ventilations and HOT, the difference in overall HOT between the control and experiment groups over the 10-min simulation was only 2%. This is because, as mentioned above, the use of the i-gel® unexpectedly introduced a new category of HOT linked to the time taken to prepare, insert, secure and confirm placement of the i-gel® device. The benefits of i-gel® insertion and associated reduction in HOT, however, become greater as the length of resuscitation time increases.
In essence, over the 10-min period, the i-gel® took almost as long to prepare, insert, secure and confirm as the amount of time it removed from ventilation time and overall HOT. This study chose to use trachy tape as a means of securing the device as this is the most widely available and cost-effective airway-securing device available on the South African EMS market. It is possible that should a different (faster) means of securingthe i-gel® airway be used, HOTtimes mightbe further decreased.
4.6. Ethical considerations
Ethical clearance for this study was granted by the Higher Degree and Ethics Committees of the Faculty of Health Sciences at the University of Johannesburg (Ethical Clearance Number AEC01-73-2014).
4.7. Reliability
Raw data captured by the researcher was independently verified by a second party who was a registered emergency care practitioner, knowledgeable about the study and associated research processes. In addition, each simulation was audio- and video-recorded, and the recorded times were compared to the recording to further ensure they were accurately reflective of the participants' actions.
4.8. Validity
The times and compressions recorded from directobservation of each participant's actions by the researcher, second party and video recording were finally compared to those registered via the SimMan® 3G software package which accurately records interventions such as ventilation, compression and hands-off time. Data was analysed using standard formulae and functions available in Microsoft Excel®. Both of these packages have been commercially tested and are deemed to deliver valid results.
4.9. Limitations of the study
This manikin-based pilot study was conducted on a relatively small sample. Even though all steps possible were taken to ensure that the simulation represented as far as possible real-life CPR, the participant's familiarity with the manikin may have influenced the incidence of difficult mask ventilation (DMV) compared to what is experienced with real live patients. It is also possible that, as the manikin used is designed to create optimal conditions for airway management for training purposes, the insertion of the i-gel® airway may possibly have occurred with greater speed and ease than in real live patients.
5. Conclusion and recommendations
No studies have proven the benefit of a single form of airway management strategy over the other, instead, the literature indicates that airway management strategies in CPR should be adapted to the specific circumstances surrounding the CPR (Hazinski et al., 2010). In South Africa, ALS paramedics often have to perform single rescuer CPR on the scene for several minutes. The latest ILCOR guidelines recommend that ALS practitioners should not perform ETI when alone with a patient in OHCA, and that BVM ventilations should rather be performed as ETI is not associated with improved outcomes (Hazinski et al., 2010). Single rescuer CPR using a BVM is associated with DMV which leads to increased ventilation time and increased HOT (Doörges et al., 2000; Kovacs & Law, 2007).
SADs provide acceptable alternatives to BVM as they mitigate the effects of DMV by removing complications associated with finding an appropriate seal between the mask and the patient's face (Dörges et al., 2000; Kovacs & Law, 2007). The i-gel® airway has been proven to be a safe addition to the range of SAD and is known to conform to the perilaryngeal soft tissues well, resulting in an appropriate placement and good seal pressures (Abraham et al., 2012; Jindal et al., 2009). The i-gel® airway is associated with short insertion time and significant ease of insertion and could provide a valid alternative to BVM ventilations during single rescuer CPR by mitigating the effect of DMV on HOT (Castle et al., 2010; Gatward et al., 2008).
As this study revealed that use of the i-gel® airway in single rescuer CPR can reduce overall ventilation time and decrease HOT, the authors recommend healthcare professionals consider the use of the i-gel® airway during single rescuer CPR as opposed to bag valve mask ventilation. Further research should be considered focusing on evaluating the impact of advanced airway management on HOT during CPR in the real clinical setting.
6. Significance of work
This article deals with how interruptions to chest compressions or "Hands Off Time" (HOT) are affected by the placement of an i-gel® airway vs. simple BVM ventilation during single rescuer CPR. An article such as this serves to draw the attention of all health care professionals to the importance of limiting interruptions to compressions when performing CPR.
REFERENCES
Abella, B. S., Alvarado, J. P., Myklebust, H., Barry, A., Hearn, N. O., Vanden Hoek, T. L., et al. (2005). Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA, 293(3), 305-310. [ Links ]
Abraham, J., Kannampallil, T., Patel, B., Almoosa, K., Patel, V. L., Medicine, A., et al. (2012). Ensuring patient safety in care transitions: an empirical evaluation of a Handoff Intervention Tool. Center for Cognitive Studies in Medicine and Public Health, The New York AMIA Annual Symposium Proceedings, 2012,17-26. [ Links ]
Asai, T., & Liu, E. (2010). The i-gel, a new supraglottic airway. Masui, 59(6), 794-797 (Article in Japanese). [ Links ]
Ashton, A., McCluskey, A., Gwinnutt, C., & Keenan, A. (2002). Effect of rescuer fatigue on performance of continuous external chest compressions over 3 min. Resuscitation, 55(2), 151-155. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/12413752. [ Links ]
Aufderheide, T. P., Sigurdsson, G., Pirrallo, R. G., Yannopoulos, D., McKnite, S., von Briesen, C.... Lurie, K. G. (2004). Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation, 109(16), 1960-1965. http://dx.doi.org/10.1161/01.CIR.0000126594.79136.61. [ Links ]
Berg, R. A., Hemphill, R., Abella, B. S., Aufderheide, T. P., Cave, D. M., Hazinski, M. F. . Swor, R. A. (2010). Part 5: adult basic life support: 2010 American heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 122(Suppl. 3), S685-S705. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.970939. [ Links ]
Bobrow, B. J., Clark, L. L., Ewy, G. A., Sanders, A. B., Berg, R. A., Richman, P. B., et al. (2008). Minimally interrupted cardiac resuscitation by emergency medical services for out-of-hospital cardiac arrest. JAMA, 299(10), 1158-1165. [ Links ]
Bobrow, B. J., Ewy, G. A., Clark, L., Chikani, V., Berg, R. A., Sanders, A. B...Kern, K. B. (2009). Passive oxygen insufflation is superior to bag-valve-mask ventilation for witnessed ventricular fibrillation out-of-hospital cardiac arrest. Annals of Emergency Medicine, 54(5), 656-662.e1. http://dx.doi.org/10.1016/j.annemergmed.2009.06.011. [ Links ]
Castle, N., Owen, R., Hann, M., Naidoo, R., & Reeves, D. (2010). Assessment of the speed and ease of insertion of three supraglottic airway devices by paramedics: a manikin study. Emergency Medicine Journal: EMJ, 27, 860-863. http://dx.doi.org/10.1136/emj.2009.084343. [ Links ]
Christenson, J., Andrusiek, D., Everson-Stewart, S., Kudenchuk, P., Hostler, D., Powell, J. . Berg, R. (2009). Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation, 120(13), 1241-1247. http://dx.doi.org/10.1161/CIRCULATIONAHA.109.852202. [ Links ]
Don Michael, T. (1985). Comparison of the esophageal obturator airway and endotracheal intubation in prehospital ventilation during CPR. Chest, 87(6), 814-819. [ Links ]
Dörges, V., Wenzel, V., Neubert, E., & Schmucker, P. (2000). Emergency airway management by intensive care unit nurses with the intubating laryngeal mask airway and the laryngeal tube. Critical Care, 4(6), 369-376. [ Links ]
Eftestol, T. (2002). Effects of interrupting precordial compressions on the calculated probability of defibrillation success during out-of-hospital cardiac arrest. Circulation, 105(19), 2270-2273. http://dx.doi.org/10.1161/01.CIR.0000016362.42586.FE. [ Links ]
Gatward, J. J., Thomas, M. J. C., Nolan, J. P., Cook, T. M., Hospital, R. U., Park, C., et al. (2008). Critical care effect of chest compressions on the time taken to insert airway devices in a manikin. British Journal ofAnaesthesia, 100(3), 351-356. http://dx.doi.org/10.1093/bja/aem364. [ Links ]
Hazinski, M. F., Nolan, J. P., Billi, J. E., Boöttiger, B. W., Bossaert, L., de Caen, A. R. . Zideman, D. (2010). Part 1: executive summary: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation, 122(Suppl. 2), S250-S275. http://dx.doi.org/10.1161/CIRCULATIONAHA.110.970897. [ Links ]
Heidenreich, J., von Briesen, C., Berg, R. A., Higdon, T. A., Ewy, G. A., Kern, K. B., et al. (2006). Rescuer fatigue: standard versus continuous chest-compression cardiopulmonary resuscitation. Academic Emergency Medicine, 13(10), 1020-1026. http://dx.doi.org/10.1197/j.aem.2006.06.049. [ Links ]
Jindal, P., Rizvi, A., & Sharma, J. (2009). Is i-Gel a new revolution among supraglottic airway devices? Middle East Journal of Anesthesiology, 20(1), 53-58. [ Links ]
Kannaujia, A., Srivastava, U., Saraswat, N., Mishra, A., Kumar, A., & Saxena, S. (2009). A preliminary study of i-gel: a new supraglottic airway device. Indian Journal ofAnaesthesia, 53(1), 52-56. [ Links ]
Kern, K., Hilwig, R., Berg, R., Sanders, A., & Ewy, G. (2002). Importance of continuous chest compressions during cardiopulmonary resuscitation: Improved outcome during a simulated single lay-rescuer scenario. Circulation, 105(5), 645-649. http://dx.doi.org/10.1161/hc0502.102963. [ Links ]
Kovacs, G., & Law, J. A. (2007). Airway management in emergencies. Chicago: McGraw-Hill Companies. [ Links ]
Langeron, O., Masso, E., Huraux, C., & Guggiari, M. (2000). Prediction of difficult mask ventilation. Anesthesiology, 92(5), 1229-1236. [ Links ]
Levitan, R. M., & Kinkle, W. C. (2005). Initial anatomic investigations of the I-gel airway: a novel supraglottic airway without inflatable cuff. Anaesthesia, 60(10), 1022-1026. http://dx.doi.org/10.1111/j.1365-2044.2005.04258.x. [ Links ]
Manders, S., & Geijsel, F. E. C. (2009). Alternating providers during continuous chest compressions for cardiac arrest: every minute or every two minutes? Resuscitation, 80(9), 1015-1018. http://dx.doi.org/10.1016/j.resuscitation.2009.05.014. [ Links ]
Nolan, J. P., Soar, J., Zideman, D. A., Biarent, D., Bossaert, L. L., Deakin, C. . Boöttiger, B. (2010). European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation, 81(10), 1219-1276. http://dx.doi.org/10.1016/j.resuscitation.2010.08.021. [ Links ]
Perkins, G. D., Brace, S. J., Smythe, M., Ong, G., & Gates, S. (2012). Out-of-hospital cardiac arrest: recent advances in resuscitation and effects on outcome. Heart, 98, 529-535. http://dx.doi.org/10.1136/heartjnl-2011-300802. [ Links ]
Richez, B., Saltel, L., Banchereau, F., Torrielli, R., & Cros, A. (2008). A new single use supraglottic airway device with a noninflatable cuff and an esophageal vent: an observational study of the i-gel. Anesthesia and Analgesia, 106(4), 1137-1139. http://dx.doi.org/10.1213/ane.0b013e318164f062. [ Links ]
Ruetzler, K., Gruber, C., Nabecker, S., Wohlfarth, P., Priemayr, A., Frass, M...Roessler, B. (2011). Hands-off time during insertion of six airway devices during cardiopulmonary resuscitation: a randomised manikin trial. Resuscitation, 82(8), 1060-1063. http://dx.doi.org/10.1016/j.resuscitation.2011.03.027. [ Links ]
Stone, B. J., Chantler, P. J., & Baskett, P. J. (1998). The incidence of regurgitation during cardiopulmonary resuscitation: a comparison between the bag valve mask and laryngeal mask airway. Resuscitation, 38(1), 3-6. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/9783502. [ Links ]
Sugerman, N. T., Edelson, D. P., Leary, M., Weidman, E. K., Herzberg, D. L., Vanden Hoek, T. L.... Abella, B. S. (2009). Rescuer fatigue during actual in-hospital cardiopulmonary resuscitation with audiovisual feedback: a prospective multicenter study. Resuscitation, 80(9), 981-984. http://dx.doi.org/10.1016/j.resuscitation.2009.06.002. [ Links ]
Wang, H. E., Simeone, S. J., Weaver, M. D., & Callaway, C. W. (2009). Interruptions in cardiopulmonary resuscitation from paramedic endotracheal intubation. Annals of Emergency Medicine, 54(5), 645-652.e1. http://dx.doi.org/10.1016/j.annemergmed.2009.05.024. [ Links ]
Wharton, N. M., Gibbison, B., Gabbott, D. A., Haslam, G. M., Muchatuta, N., & Cook, T. M. (2008). I-gel insertion by novices in manikins and patients. Anaesthesia, 63(9), 991-995. http://dx.doi.org/10.1111/j.1365-2044.2008.05542.x. [ Links ]
Wiese, C. H. R., Bartels, U., Schultens, A., Steffen, T., Torney, A., Bahr, J., et al. (2008). Influence of airway management strategy on "no-flow-time" during an "advanced life support course" for intensive care nurses - a single rescuer resuscitation manikin study. BMC Emergency Medicine, 8(4), 1-7. http://dx.doi.org/10.1186/1471-227X-8-4. [ Links ]
Yannopoulos, D., & Aufderheide, T. (2007). Acute management of sudden cardiac death in adults based upon the new CPR guidelines. Europace: European Pacing, Arrhythmias, and Cardiac Electrophysiology: Journal of the Working Groups on Cardiac Pacing, Arrhythmias, and Cardiac Cellular Electrophysiology of the European Society of Cardiology, 9(1), 2-9. http://dx.doi.org/10.1093/europace/eul126. [ Links ]
Zaritsky, A., & Morley, P. T. (2005). The evidence evaluation process for the 2005 international consensus conference on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation, 112. http://dx.doi.org/10.1161/CIRCULATIONAHA.105.170812. III-128-III-130. [ Links ]
Received 3 August 2015
Accepted 5 August 2015
* Corresponding author. Tel.: +27 11 559 6257, +27 082 653 2125 (mobile). E-mail address: clambert@uj.ac.za (C. Vincent-Lambert).
1 Tel.: +27 11 559 6257.














