Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
African Journal of Primary Health Care & Family Medicine
versão On-line ISSN 2071-2936
versão impressa ISSN 2071-2928
Afr. j. prim. health care fam. med. (Online) vol.15 no.1 Cape Town 2023
http://dx.doi.org/10.4102/phcfm.v15i1.4216
SHORT REPORT
School-based healthcare services in Cape Town, South Africa: When there's a will, there's a way
Nadia AhmedI, II; Carey PikeII; Jessica LeeII, III; Colleen WagnerII, IV; Linda-Gail BekkerII
IMortimer Market Centre, Central North West London NHS Trust, London, United Kingdom
IIDesmond Tutu HIV Centre, Faculty of Health Sciences, University of Cape Town, Cape Town, South Africa
IIIGeisel School of Medicine, Dartmouth College, Hanover, New Hampshire, United States of America
IVNetworking HIV and AIDS Community of South Africa (NACOSA), Cape Town, South Africa
ABSTRACT
South African secondary schools do not deliver school-based healthcare services despite high rates of human immunodeficiency virus (HIV) infection, sexually transmitted infections, and unplanned pregnancies among adolescents, ongoing sub-optimal uptake of healthcare services from public healthcare facilities by adolescents, and national policy support for such services. A pilot school health nursing programme (SHNP) was offered to 44 secondary schools in a single health sub-district within the Western Cape, South Africa. The programme included fortnightly nurse visits that offered a standard package of healthcare services, including sexual and reproductive health services tailored according to school preference.
Of the 44 schools, 42 gave permission for the SHNP to operate, with the majority of schools selecting the full comprehensive package of services. Programme implementation was truncated such that delivery only occurred over two school terms (20 weeks); however, 344 students attended the service. The majority of service users were female with a median age of 16 years, and over a half attended the service for sexual and reproductive health services.
CONTRIBUTION: A key challenge to school-based health service delivery arose from inadequate stakeholder support and differential views of adolescent healthcare needs among government officials, parents, guardians, school staff and governing bodies. These findings motivate for ongoing multi-level stakeholder engagement around the reality of adolescent healthcare needs and further opportunities to deliver school health services for longer time periods such that their feasibility, acceptability, and potential to impact healthcare outcomes can be assessed in this setting
Keywords: school health services; adolescent health; HIV prevention; adolescent pregnancy; sexual and reproductive health; South Africa; school health nursing.
Adolescents spend approximately one third of their time in school, a setting where healthy lifestyles and healthcare can be promoted and provided through interventions and direct service delivery.1,2 School health services are used in 102 countries, through school-based or school-linked provision, with evidence showing that such services provide accessible, efficient, effective and safe management of the healthcare needs of adolescents.1,2 South Africa (SA) has a high rate of human immunodeficiency virus (HIV) incidence, sexually transmitted infections (STIs), and unplanned pregnancies among adolescents, indicating unmet health needs by the current facilities and interventions.3 While recommended in national policy,4 in practice they are not delivered as a standard in South African secondary schools, with limited data to guide effective implementation. Implementation challenges have been attributed to managerial variation in the value attached to health promotion, insufficient collaboration between the departments of health (DOH) and education (DOE), and inadequate stakeholder integration.5,6 While deemed acceptable by school staff, previous attempts to implement school health services have been sub-optimal, with infrequent nurse visits (up to once a year), a lack of basic resources (staff, equipment and space), poor referral systems, and greater challenges in rural environments.4,7
Design and delivery
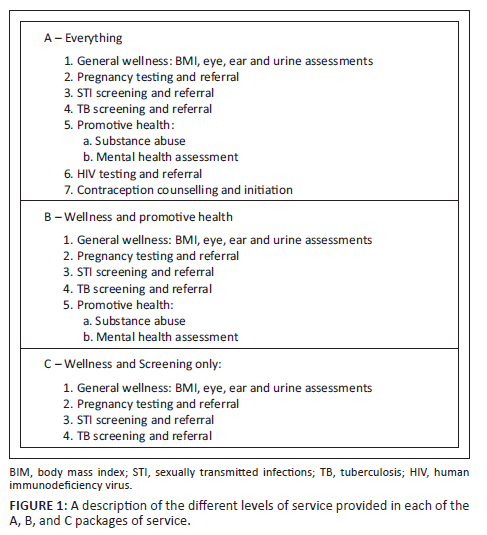
During the implementation of the South African National Young Women and Girls (YWG) Programme, funded by the Global Fund to Fight AIDS, Tuberculosis, and Malaria, a school health nursing programme (SHNP) was offered to 44 secondary schools in a single health sub-district within the Western Cape, SA.8 The primary objective was to pilot a potential model of school health delivery to inform the design of future large-scale trial, to provide guidance for implementation. The SHNP involved fortnightly school visits by registered nurses (RNs), offering a range of healthcare services (Figure 1) and urgent advice within school hours. Clinical practice was conducted according to standard practice, with onward referral to other services as needed.9 Data on school and learner characteristics were collected routinely as part of the broader YWG programme. Programme records included basic demographics and medical records (reason for visit, test results, administration of referrals).
Implementation
Of the 45 schools, 42 participated. Reasons for decline amongst the remaining three schools included: commitment to other programmes, local safety concerns, and school governing body opposition. Forty per cent (n = 17) of schools opted for package A, 43% (n = 18) for B and 17% (n = 7) for C. Schools of a lower socioeconomic status, larger size, higher HIV and tuberculosis (TB) burden, tended to opt for package A. Schools with higher socioeconomic status and performance, lower HIV and TB disease burdens but higher pregnancy prevalence and substance use, opted for package B, C, or declined altogether. The SHNP was scheduled for 12 months; however, a communication change from district education officials led to early termination, limiting the delivery period to two of the four school terms (20 weeks).
A total of 344 school learners were seen, and the majority of them were female (n = 258, 81%), with a median age of 16 years (IQR 14-17). Over a half attended for sexual reproductive health (SRH) related matters (55%, n = 189), including STIs, contraception, menstruation issues and circumcision requests. Fifty per cent (173/344) of the learners received an HIV test; 4% (5/138) had genital symptoms requiring onward referral for management; 9% (24/258) requested pregnancy tests; and 12 males enquired about circumcision following an educational session on HIV prevention. Contraception was used by 16% (41/258) of females, and 61% (131/344) never used condoms. The most common HIV risk factor reported was not knowing their partner's HIV status. Eight per cent (17/203) of those screened, reported a history of sexual and/or physical abuse. Depression was indicated in 11% of learners through the Patient Health Questionnaire 9 screening tool. Other minor ailments seen required simple reassurance, advice or management.
Thirteen per cent (44/344) in total required onward referral to another service. Healthcare facility referrals were needed for 57% (25/44), social services for 43% (19/44), with the remainder having their presenting complaint resolved on-site.
Discussion
The key challenge to the SHNP pilot in secondary school health service delivery came from inadequate stakeholder support and differential views of adolescent healthcare needs among government officials, parents, guardians, school staff and governing bodies. The package of healthcare services designed for the pilot, package A, met resistance in a subset of participating schools that necessitated the re-design of the package into two reduced offerings, further evidencing divergent views of needs across schools. Different opinions from district education officials however ultimately led to early termination, despite best efforts to reach effective solutions. The DOE has traditionally worried about activities that are not directly related to education and curricula. It is incumbent upon us to show that benefits outweigh any perceived risks and that this can be performed efficiently, minimising time that learners may take from school-related activities rather than increasing that time.
While the sample size was low overall, this reflects a short pilot period for reasons aforementioned. Furthermore, fortnightly RN visits might have further impacted the low sample size; had the RN visits been more frequent, more learners may have had the opportunity to be seen. Increased familiarity with the service over an extended period could have increased uptake, especially among traditionally difficult-to-engage male users, given that adolescents find services more confidential, reliable and consistent when there is time to develop rapport with healthcare providers.9,10
Learner enquiries into circumcision additionally support the ability of the SHNP to provide an immediate link for applying learning into practice. The need for health education and/or empowerment interventions in tandem with health services was further evident from the sexual risk profiles of learners. Risk factors among adolescents are chronically under-reported, for reasons including social desirability bias and confidentiality concerns, and as such the figures reported here are likely underestimates. More time to build rapport and trust with the RNs may have reduced underreporting bias, as well as led to opportunities to manage sexual reproductive health presentations but more importantly screening and prevention of these issues and others.
Approximately one third required external referrals, while the majority had the potential to be dealt with on-site, but was limited by specialisation (e.g. prescribing) and/or permissions (e.g. contraception provision). This supports the potential for school health services to, at a minimum, effectively increase access to healthcare for adolescents and to decongest health facilities.
Despite these challenges and limitations, there were encouraging and frequent reports of positive feedback that the SHNP was acceptable among learners, school staff, local DOE officials, and the RNs. No formal feedback was obtained; however, learners participating in focus group discussions linked to the broader YWG programme evaluation reported finding the SHNP acceptable; 'We go to the clinic and it's already packed … here it's never packed' and 'clinic nurses are rude … Here, the nurse doesn't shout, she just helps'.8
Findings from this SHNP provide the beginning of a successful model of care for delivering healthcare in secondary schools in SA. The delivery and implementation successes and challenges further motivate multilevel stakeholder engagement around the reality of adolescent healthcare needs and a potential solution to support and complement existing healthcare through the delivery of school health services. Longer implementation is needed to refine the model, and assess its impact, feasibility and cost-effectiveness.
Acknowledgements
The authors would like to thank the Research Nurses who carried out this School Health Nursing Programme, Sisters Boneta Smitsdorff, Beulah Classen, Miriam Gqiza, and Phindile Matshini. The authors would also like to thank the learners and school staff for their participation and support of this programme.
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
N.A., C.W., and L.G.B. conceptualised and designed the study, and along with J.L. were involved in the implementation of the study and the collection and analysis of the data. N.A., C.P., and L.G.B. drafted and critically revised the manuscript. All authors have given final approval of the manuscript for publication.
Ethical considerations
This article followed all ethical standards for research without direct contact with human or animal subjects.
Funding information
This school health nursing programme was a component of a large South African National Women and Girls Programme, funded by the Global Fund to Fight AIDS, Tuberculosis, and Malaria.
Data availability
The data that support the findings of this study are available from the corresponding author, C.P., upon reasonable request.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1.World Health Organisation. WHO guideline on school health services [homepage on the Internet]. Geneva: World Health Organization; 2021. [cited 01 June 2020]. Available from: https://www.who.int/publications/i/item/9789240029392 [ Links ]
2.Mason-Jones AJ, Crisp C, Momberg M, Koech J, De Koker P, Mathews C. A systematic review of the role of school-based healthcare in adolescent sexual, reproductive, and mental health. Syst Rev. 2012;1:49. https://doi.org/10.1186/2046-4053-1-49 [ Links ]
3.Mabaso M, Maseko G, Sewpaul R, et al. Trends and correlates of HIV prevalence among adolescents in South Africa: Evidence from the 2008, 2012 and 2017 South African National HIV Prevalence, Incidence and Behaviour surveys. AIDS Res Ther. 2021;18:97. https://doi.org/10.1186/s12981-021-00422-3 [ Links ]
4.Health Basic Education. Integrated school policy [homepage on the Internet]. 2012 [cited 2022 Jun 29]. Available from: https://www.education.gov.za/Portals/0/Documents/Policies/INTEGRATED%20SCHOOL%20HEALTH%20POLICYB-W_1.pdf?ver=2014-06-14-172322-000 [ Links ]
5.Rasesemola RM, Matshoge GP, Ramukumba TS. Compliance to the integrated school health policy: Intersectoral and multisectoral collaboration. Curations. 2019;42(1):1912. https://doi.org/10.4102/curationis.v42i1.1912 [ Links ]
6.Shung-King M. From 'stepchild of primary healthcare' to priority programme: Lessons for the implementation of the National Integrated School Health Policy in South Africa. S Afr Med J. 2013;103(12):895-898. https://doi.org/10.7196/SAMJ.7550 [ Links ]
7.Dibakwane ST, Peu MD. Experiences of school health nurses regarding the provision of the school health service delivery in the Tshwane district. Afr J Prim Health Care Fam Med. 2018;10(1):e1-e8. https://doi.org/10.4102/phcfm.v10i1.1807 [ Links ]
8.Desmond Tutu HIV Foundation. The Zimele project appraisal 2016-2019 [homepage on the Internet]. Cape Town; 2021 [cited 2021 May 26]. Available from: https://desmondtutuhealthfoundation.org.za/wp-content/uploads/2020/12/Zimele-16.11.pdf [ Links ]
9.South African National Department of Health. National consolidated guidelines for the prevention of mother to child transmission of HIV (PMTCT) and the management of HIV in children, adolescents and adults. [homepage on the Internet]. 2014 [cited 01 June 2020]. Available from http://www.kznhealth.gov.za/family/hiv-guidelines-jan2015.pdf. [ Links ]
10.Smith P, Marcus R, Bennie T, et al. What do South African adolescents want in a sexual health service? Evidence from the South African studies on HIV in adolescents (SASHA) project. S Afr Med J. 2018;108(8):677-681. https://doi.org/10.7196/SAMJ.2018.v108i8.13013 [ Links ]
 Correspondence:
Correspondence:
Carey Pike
Carey.Pike@hiv-research.org.za
Received: 28 June 2023
Accepted: 07 Sept. 2023
Published: 27 Oct. 2023














