Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Primary Health Care & Family Medicine
On-line version ISSN 2071-2936
Print version ISSN 2071-2928
Afr. j. prim. health care fam. med. (Online) vol.15 n.1 Cape Town 2023
http://dx.doi.org/10.4102/phcfm.v15i1.3688
ORIGINAL RESEARCH
Knowledge, attitude and practice on screening and early diagnosis of prostate cancer of primary health care providers in the Free State
Matthew O.A. BenedictI; Wilhelm J. SteinbergI; Frederik M. ClaassenII; Nathaniel MofoloIII; Cornel van RooyenIV
IDepartment of Family Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIDepartment of Urology, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIFaculty of Health Sciences, School of Clinical Medicine, University of the Free State, Bloemfontein, South Africa
IVDepartment of Biostatistics, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Prostate cancer is topmost in terms of incidence and mortality among men in sub-Saharan Africa, including South Africa. Prostate cancer screening is beneficial only to certain categories of men, making a rational screening approach necessary.
AIM: This study aimed to assess the knowledge, attitudes and practice (KAP) regarding prostate cancer screening among primary health care (PHC) providers in the Free State, South Africa.
SETTING: Selected district hospitals, local clinics and general practice rooms.
METHODS: This was a cross-sectional analytical survey. Participating nurses and community health workers (CHWs) were selected through stratified random sampling. All available medical doctors and clinical associates were approached to participate, totalling 548 participants. Relevant information was obtained from these PHC providers using self-administered questionnaires. Both descriptive and analytical statistics were computed using Statistical Analysis System (SAS) Version 9. A p-value < 0.05 was considered significant.
RESULTS: Most participants had poor knowledge (64.8%), neutral attitudes (58.6%) and poor practice (40.0%). Female PHC providers, lower cadre nurses and CHWs had lower mean knowledge scores. Not participating in prostate cancer-related continuing medical education was associated with poor knowledge (p < 0.001), negative attitudes (p = 0.047) and poor practice (p < 0.001.
CONCLUSION: This study established appreciable KAP gaps relating to prostate cancer screening among PHC providers. Identified gaps should be addressed through the preferred teaching and learning strategies suggested by the participants.
CONTRIBUTION: This study establishes the need to address KAP gaps regarding prostate cancer screening among PHC providers; therefore necessitating the capacity-building roles of district family physicians.
Keywords: Knowledge, attitude and practice; primary health care practitioners; primary health care providers; prostate cancer screening; early diagnosis.
Introduction
Noncommunicable diseases (cancers inclusive) are responsible for about 70% of all deaths worldwide, with the majority of these deaths occurring in the low- and middle-income countries.1 Hence, the Sustainable Developmental Goal 3.4 aims 'to reduce, by one third, premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being by 2030'.2
In sub-Saharan Africa, prostate cancer (PCa) is topmost in terms of incidence and mortality among men.3 Both foreign4,5 and local6,7 studies have shown racial disparities in PCa presentation, with men of African ancestry being mostly affected. In South Africa, black men often present late and with advanced disease, thus contributing to an increased mortality and morbidity. Poverty, poor socio-economic status, illiteracy and a lack of knowledge of the disease symptoms are some of the factors responsible for late presentation.8 Most South African indigenous languages do not even have translations for the term 'prostate'.8
The Free State has the lowest life expectancy (male 55 years; female 61 years) compared with the average figures for the other provinces in South Africa (male 62 years; female 68 years).9 The black race is mostly associated with poor socio-economic status and concomitant poor health outcomes. There is therefore the need to prioritise access to basic primary health care (PHC) services, such as screening, in the study setting.
Relevant international10 and local11 associations have recognised some benefits of PCa screening among certain categories of men and have therefore published guidelines for screening. Screening for PCa has been controversial because of over-diagnosis, overtreatment and certain accompanying side effects such as sexual and urinary dysfunction.12 However, a recent study on the harm-to-benefit of PCa screening showed that the potential for over-diagnosis and overtreatment notwithstanding, the net benefit of prostate-specific antigen (PSA) screening is greater for black men than the general population. This may indicate the need for race-specific screening guidelines.13 The United States Preventive Task Force (USPSTF) has reported a potential benefit of decreasing deaths from PCa in men aged 55-69 years with PSA screening; this is doubtful for men above 70 years of age.14
South African guidelines11 recommend that PCa screening (PSA and digital rectal examination [DRE]) be performed in all men from 45 years onwards in the absence of identifiable risk factors and from 40 years in black men, where there is a family history of PCa and other identifiable risk factors. Yet there is evidence that African men are less likely to participate in PCa screening with a view to making an early diagnosis, which may in part explain the disparity in PCa deaths.15 Poor adherence to screening guidelines among black men could indicate gaps in their knowledge, culture and beliefs regarding PCa and related aspects.15 In a review study, barriers related to PCa screening among men in sub-Saharan Africa were related to client, healthcare provider and healthcare systems factors.16 The influence of healthcare providers is an important factor associated with PCa screening uptake among men.17,18
According to the health belief model, individual beliefs and certain sociopolitical factors are strong determinants of health behaviours.19 Healthcare providers support users to make healthcare choices through shared decision-making (SDM).20 Guidelines of the American Cancer Society highlighted the following as vital information needed for men to make screening decisions: risks, potential benefits and uncertainties regarding PCa screening.21 Ng and Lee22 highlighted six steps in the practice of SDM: (1) identify the decision, (2) list the available options, (3) discuss the pros and cons of each option, (4) elicit patient values, (5) provide support and (6) make a decision. More so, it has been shown that healthcare users from socio-economically disadvantaged areas prefer SDM.20
In a European study that compared general practitioners (GPs) and urologists in their handling of PSA testing and guidelines on early detection of PCa, unlike the urologists, the GPs perceived the PSA test not to be useful. In addition, the GPs showed a less proactive approach to informing men about PSA and were less familiar with guidelines and recommendations on PSA testing.23 This might imply a knowledge gap among these GPs. A United States (U.S.) study showed a poor practice of SDM among some physicians involved with PCa screening with PSA.24 At the 8th International Prostate Cancer Congress, better education of primary care physicians on SDM was recommended to achieve an improved approach to PCa screening.25 In a Malaysian study, more than half of the GPs overestimated the positive predictive values of PCa screening tools. The same study also showed that GPs who would consider having a PSA test performed on themselves were more likely to screen asymptomatic men than GPs who would not have the test.26
In a study that assessed the knowledge and attitude of primary care physicians in Florida, U.S., regarding PCa screening, the mean knowledge score was 66%. More than 70% of the responders believed that screening was effective, and the attitude scores were associated with practice setting and the proportion of patients having medical aid.27 Primary health care providers' knowledge and attitudes towards PCa screening may affect their approach to the screening of men. Studies exploring this subject are, however, scarce in our study setting. Foreign studies28,29 have shown the roles of nurses and community healthcare workers in health promotion and SDM relating to PCa screening. These roles should be encouraged among these nonmedical PHC cadres, who are first-line PHC providers in South African local communities and clinics.
As explained here, the controversy associated with PCa screening may inform the varied attitude and practice of PHC providers. Studies have identified gaps in knowledge, attitude and practice (KAP) regarding PCa screening among men; however, there is a scarcity of local studies on this subject among PHC providers in South Africa.
Therefore, the aim of the study was to assess the KAP regarding PCa screening and early diagnosis among PHC providers in the Free State, South Africa. The objectives were to determine: (1) demographic details, (2) KAP on PCa screening and early diagnosis, (3) participants' perceived need for enhanced knowledge on PCa screening and their preferred learning methods and (4) factors associated with participants' KAP.
Research methods and design
Study design
This was a cross-sectional analytical survey carried out among PHC providers in the Free State, South Africa, over six months (01 January 2021 - 30 June 2021).
Study setting and rationale for this setting
The study setting chosen for this study was the Free State, which is geographically the third-largest province in South Africa, constituting 5.1% of the national population. The estimated population was 2 971 708 as of 2019. This province comprises Mangaung Metropolitan Municipality (MMM) and four district municipalities: Xhariep, Lejweleputswa, Thabo Mofutsanyana and Fezile Dabi. These district municipalities are subdivided into 19 local municipalities. The economy is dominated by agriculture, mining and manufacturing.30
The PHC facilities in the Free State include 231 PHC clinics, that is, local clinics and community health centres, and 24 district hospitals. Most of the population using public health services attend these healthcare facilities. Ward-Based Primary Health Care Outreach Teams (WBPHCOTs) are linked to the PHC facilities and consist of community health workers (CHWs) led by nurses. The WBPHCOTs undertake home visits, assess the health status of individuals in households and provide health education and promotion services; they identify and refer those in need of preventive, curative or rehabilitative services to relevant PHC facilities.
Mangaung Metropolitan Municipality of the Free State is one of the top populated black townships in South Africa.31 According to an unpublished retrospective cross-sectional study conducted in Bloemfontein, Free State, African men were shown to be at higher risk of having PCa of worse prognosis, that is, Gleason score ≥ 8, higher mean PSA levels and more advanced local staging, compared with their European counterparts.32
Target population
The target population comprised PHC workers (doctors, nurses, clinical associates and CHWs) in the Free State. The PHC workers include all cadres of state-employed medical doctors (interns in Family Medicine rotation, community service medical officers, medical officers, Family Medicine registrars and specialist family physicians) and GPs in private practice, nurses (professional, enrolled and enrolled nursing assistants), clinical associates and CHWs working in the PHC clinics. The majority of these PHC providers (especially the nurses and CHWs) work in the community and are not hospital-based. The subject of PCa screening, like any other screening, falls within PHC services and does not require specialised capabilities. Healthcare providers working in more specialised settings were excluded from this study.
Sample and sampling
Owing to the diversified cadres of the study population, multiple sampling methods were engaged to maximise the sample size per cadre of PHC provider while also minimising the risk of bias. The total number of PHC medical doctors in the Free State at the time of the study was less than 200; hence, they were all targeted without sampling. The same went for clinical associates, who are less than 20 in the province. On the other hand, the PHC nursing staffs and CHWs in the Free State were much more numerous; hence, a stratified sampling was engaged for these cadres.
All state-employed medical doctors and clinical associates were easily accessed through the corresponding PHC facilities in the Free State (i.e. district hospitals and PHC clinics). Therefore, they were all approached to participate. There were approximately four nurses per 231 fixed PHC clinics (total of about 924 nurses) and around two full-time CHWs per 231 fixed PHC clinics (a total of about 462 CHWs). With the aid of the Raosoft sample size calculator (Raosoft, Inc., Seattle, Washington, United States),33 setting the margin of error at 5%, confidence level at 95%, response distribution at 50% and with the population sizes of 924 and 462, the authors arrived at sample sizes of 272 and 210, respectively, for nurses and CHWs.
The list of the clinics was obtained from each district office. Through the stratified simple random sampling method, 105 clinics in total were selected from the five districts in the Free State, that is, 21 clinics per district. Three nurses and two CHWs were targeted from each of the 105 selected clinics.
Measurement, data collection and questionnaire
For the purpose of this study, data were obtained from primary sources, that is, the eligible PHC providers in the Free State. A self-administered questionnaire was used. The questionnaire was adapted from previous similar surveys26,34,35 aimed to understand the KAP of primary care physicians towards PCa and PCa screening. The researcher and his (research) assistant visited the selected PHC facilities and administered the questionnaires to consenting participants. An electronic version of the questionnaire was e-mailed to GPs in private practice.
The adapted questionnaire consisted of six sections. Section A dealt with the background information and demographics of the participants. Section B contained the knowledge items. This included 61-point knowledge-testing questions. Four of these questions were not applicable to the enrolled nurses, enrolled nursing assistants and CHWs; hence, these cadres responded to 57 knowledge-testing questions. The questions were mainly a combination of the following formats: single best answer; multiple choice; 'list' type; 'yes', 'no' or 'I don't know'; 'true', 'false' or 'I don't know'. The correct and incorrect responses were scored 1 and 0, respectively. The aspects of PCa knowledge tested included: function of the prostate, risk factors, symptoms, screening tests, screening test interpretation, diagnosis, staging, treatment and complications of treatment.
Bloom's cut-off points36 was used to categorise knowledge levels as follows:
•good knowledge (80% - 100% correct responses)
•moderate knowledge (60% - 79% correct responses)
•poor knowledge (< 60% correct responses).
Section C was the attitude section. Participants were requested to respond to 14 statements, through which their attitude towards PCa was measured on a 7-point Likert scale (1 = strongly disagree; 7 = strongly agree). The individual points per statement were summed up, and the possible obtainable scores ranged from 0 to 98.
Using Bloom's cut-off points,36 the scores were classified as follows:
•positive attitude (80% - 100% correct responses)
•neutral attitude (60% - 79% correct responses)
•negative attitude (< 60% correct responses).
In Section D, the participants' practices regarding PCa counselling and screening were measured on a 7-point Likert scale. An additional yes-or-no question asked the male participants if they would be willing to have a PCa screening.
The participants responded to nine practice statements. The enrolled nurses, enrolled nursing assistants and CHWs were exempted from three of these statements, which do not apply to them. The practice statements were graded on a 7-point Likert scale (1 = very untrue of me; 7 = very true of me). The individual points per statement were summed up, and the possible obtainable scores ranged from 0-63 (0-42 for enrolled nurses, enrolled nursing assistants and CHWs)
Using Bloom's cut-off points,36 the scores were classified as follows:
•good practice (80% - 100% of the possible obtainable scores)
•fair practice (60% - 79% of the possible obtainable scores)
•poor practice (< 60% of the possible obtainable scores).
Section E assessed participants' perceived barriers to PCa counselling and screening. This was measured on a 3-point scale (true, false, I don't know).
Finally, Section F checked the participants' perceived need for additional knowledge on PCa as well as their preferred method of knowledge transfer.
Content validity and reliability of the questionnaire
This original questionnaire was validated by experts specialising in urology, public health, health education and behavioural sciences in Saudi Arabia. Cronbach's reliability test was used to test the internal consistency of the different scales used (the scores were 0.75 for knowledge, 0.65 for attitude and 0.93 for self-efficacy and practice).34,35
Changes were made to the original questionnaire to adapt the questions to the study setting, for example, 'Saudi Arabian men' was changed to 'South African men'. The adapted questionnaire was reviewed and approved by a Health Sciences Faculty evaluation committee comprising consultant family physicians, a urologist, medical educators, a professional nurse and a biostatistician.
Pilot study
The adapted questionnaire was pretested in December 2020 on 22 participants, including two clinical associates and four from each of the other cadres of PHC workers. Participants were chosen in succession. The pilot study was to ensure that the questions were balanced and correctly constructed and that the crucial information was obtained. The 22 piloted questionnaires were included in the study because no significant changes arose from the pilot study.
Data analysis
The data were analysed by the Department of Biostatistics, Faculty of Health Sciences, University of the Free State (UFS), using Statistical Analysis System (SAS) version 9 (SAS Institute Inc., Cary, North Carolina, U.S.). Descriptive statistics (e.g. median and standard deviation [s.d.]) were used for continuous variables, while frequencies and percentages were calculated for categorical data. Association between variables were assessed using chi-square or Fisher's exact tests. A level of significance was set at p-value of < 0.05.
Ethical considerations
The permission to conduct the study was granted by the head of the Free State Department of Health. Ethical approval for the study was obtained from the Health Sciences Research Ethics Committee of the University of the Free State (ethical clearance number UFS-HSD2020/1481/2411).
Before study participation, each participant gave informed consent after being provided with a detailed description of the study. The voluntary nature of participation and the right to refuse participation or withdraw during the study was explained. The self-administered questionnaire was anonymous. The names of participants were not recorded on any of the documents.
Results
Sociodemographic characteristics of participants
Five hundred and forty-eight (n = 548) PHC providers participated out of the 763 eligible participants invited, giving a response rate of 71.8%. Table 1 summarises the participant characteristics.

The median age of the participants was 38 years (range 22-77 years). Of the 309 participants with a degree(s) (or equivalent), 110 (35.6%) had postgraduate qualifications, ranging from postgraduate certificates to PhD degrees. Forty-three (7.8%) participants had some training outside South Africa, while 39 (7.1%) had practised outside South Africa. Forty-one (7.5%) participants had held posts or worked in a urology unit, the duration of which was less than a year (n = 33, 80.5%). Most (n = 511, 93.2%) participants had never attended continuing medical education (CME) focusing on PCa. Only 28 (5.1%) worked in a facility that runs a men's health clinic. Sixty-nine (12.6%) participants were involved in the training of medical students.
Other prostate cancer-related background information
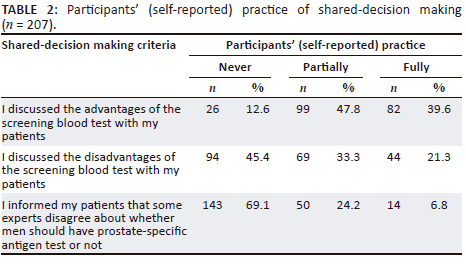
About a fifth (n = 117, 21.4%) of the participants had guidelines on PCa screening, and 192 (35.0%) were aware of the South African Prostate Diagnostic and Treatment Guidelines, 2017 (SAPDTG).11 A total of 207 (37.8%) participants had either given a health talk about PCa or conducted PCa screening with PSA in the past. These participants' (self-reported) practice of SDM is shown in Table 2.
Assessment of participants' knowledge about prostate cancer
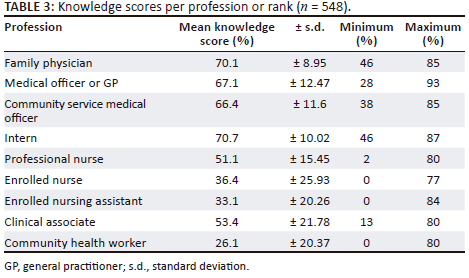
The majority (n = 355, 64.8%) of participants had poor knowledge (< 60%), 30.1% (n = 165) had moderate knowledge (60% - 79%), while 5.1% (n = 28) had good knowledge (80% - 100%). However, 274 (50.0%) participants had a score of ≥ 50%. The mean knowledge scores (± s.d.) per profession are shown in Table 3.
Comparison between different background characteristics and participants' knowledge
As shown in Table 6, compared with the male participants, more women had poor knowledge. Medical officers or GPs had better knowledge compared with other professions and ranks (p < 0.001). More state-employed participants had better knowledge than those in the private sector or both sectors (p < 0.001). Participants with over 10 years' working experience had better knowledge, although it was not statistically significant (p = 0.064).
Participants without prior working experience in urology had poor knowledge (p = 0.001). Participants who had never attended PCa-related CME or continuing professional development (CPD) had poor knowledge (p < 0.001). Running men's health clinics did not show any statistically significant association with the participants' knowledge (p = 0.062). Participants uninvolved with the training of medical students had poor knowledge compared with those involved in providing such training (p < 0.001).
Participants unaware of the SAPDTG11 had poor knowledge (p < 0.001). Participants without PCa screening guidelines in their practice had poor knowledge (p = 0.044). Participants who had previously conducted PCa screening or given relevant health talks had better knowledge than those who had not (p < 0.001).
Assessment of participants' attitudes towards prostate cancer screening
Most (n = 321, 58.6%) participants had a neutral attitude (60% - 79%), 40.7% (n = 223) had a negative attitude (< 60%), while 0.7% (n = 4) had a positive attitude (80% - 100%). Table 4 shows the level of agreement to the statements regarding attitude towards PCa.
Comparison between different background characteristics and participants' attitudes
The female participants were more uncomfortable with practice relating to men's health than their male counterparts (p = 0.003). Professional nurses and CHWs were more uncomfortable with practice pertaining to men's health compared with participants of other professions and ranks (p = 0.002). More CHWs had a negative attitude than participants of other professions or ranks (p < 0.001).
The bivariate analysis in Table 6 shows that more female participants had a negative attitude compared with their male counterparts. More state-employed participants had a positive attitude compared with those of other work sectors (p < 0.001). Participants with 1-5 years' working experience had a positive attitude compared with those with other years of experience (p = 0.014). Participants without additional postgraduate qualifications (compared with those who have) had a negative attitude, although this was not of statistical significance (p = 0.105).
Participants without previous work experience in urology had a negative attitude compared with those with prior urology work experience, although this association was not of statistical significance (p = 0.239). Participants who had never attended PCa-related CME or CPD had a negative attitude (p = 0.047).
More participants aware of the SAPDTG11 had a positive attitude than those unaware of the guidelines (p = 0.027). More participants with poor knowledge had a negative attitude than participants in the other knowledge categories (p < 0.001).
Assessment of participants' practice regarding prostate cancer screening and counselling
The majority (n = 219, 40.0%) of participants had poor practice (< 60%), 35.8% (n = 196) had fair practice (60% - 79%), while 24.3% (n = 133) had good practice (80% - 100%). Table 5 shows the participants' self-reported level of confidence regarding PCa screening and counselling practices.
Male participants tended to be more comfortable with DRE than their female counterparts (p < 0.001). Unlike the other professions or ranks, the professional nurses were less comfortable with DRE (p < 0.001) and felt less competent in detecting abnormalities on DRE (p < 0.001). Of the 130 male participants, 100 (75.8%) would consider having PCa screening on themselves.
Comparison between different background characteristics and participants' practices
As shown in Table 6, compared with their male counterparts, more female participants had poor practice (p < 0.001). Medical officers or GPs had good practice compared with the other professions or ranks (p < 0.001). State-employed participants had good practice in comparison to those of other work sectors (p < 0.001). Participants with 1-5 years' working experience had good practice compared with those with other years of experience (p = 0.019). Participants without additional postgraduate qualifications (compared with those who have) had poor practice (p = 0.041).
Participants who had never attended PCa-related CME or CPD had poor practice (p < 0.001). Participants without a men's clinic in their practice had poorer practice than those having such a clinic (p = 0.005). Participants uninvolved with training of medical students had poorer practice than those involved in giving such training (p < 0.001).
Participants aware of the SAPDTG11 had better practice than those unaware of the guidelines (p < 0.001). Participants without PCa screening guidelines in their practice had poorer practice than those with such guidelines (p < 0.001). Participants who had previously conducted PCa screening or given relevant health talks had good practice compared with those who had not (p < 0.001).
Overall comparison between knowledge, attitude and practice
Participants with poor knowledge had poor practice compared with other knowledge categories (p < 0.001). Participants who had a negative attitude had poor practice compared with other attitude categories (p < 0.001).
Perceived barriers to prostate cancer screening and counselling
Table 7 shows the participants' perceived barriers to PCa counselling and screening. Most participants reported a lack of knowledge among healthcare practitioners and men at risk as possible barriers.

Need for more knowledge relating to prostate cancer
The majority (n = 489, 89.4%) of participants felt they needed additional knowledge regarding PCa screening. These aspects included: treatment (n = 392, 80.2%), risk factors and counselling (n = 387, 79.1%), value of nutrients (n = 367, 75.1%), diagnosis (n = 351, 71.8%), symptoms (n = 345, 70.6%), value of PSA testing (n = 338, 69.1%) and value of DRE (n = 335, 68.5%).
The preferred methods of knowledge delivery were as follows: study material (n = 374, 76.5%), practical sessions (n = 312, 63.8%), simulated scenarios (n = 288, 58.9%), group tasks (n = 254, 51.9%), didactic lectures (n = 218, 44.6%) and other - online CPD (n = 8, 1.6%).
Discussion
Sociodemographic and background characteristics
The majority (76.3%) of the participants were women. This may be because PHC clinics in South Africa are nurse-driven. Most nurses and CHWs were women; these two cadres of PHC providers formed about 60% of the participants in this study. The majority of the participants were in the age group 31-40 years old, with a median age of 38 years. The majority (39.4%) had work experience of 1-5 years. Among the medical doctors in this study, the majority were medical officers. Similar demographic patterns were found in a study37 conducted among medical doctors and nurses in the Free State, where the majority were women and nurses, in the age group 30-39 with a mean age of 39 years, with between 1-5 years' experience, and the majority of the medical doctors were medical officers.
The majority of the participants had never worked in facilities running men's health clinics (94.9%). Most participants (93.2%) had never attended CME related to PCa. This may suggest that this subject and perhaps subjects relating to men's health have not been prioritised among some PHC providers in the study setting.38 This subject of men's health is also unlikely to have been prioritised when it comes to refresher courses considered for PHC providers.
About a fifth (21.4%) of the participants had guidelines on PCa screening at their practice, and 35% were aware of the SAPDTG.11 This approximately correlates with the 37.8% who had ever either given a health talk on PCa or conducted a PCa screening with PSA. However, as shown in Table 2, it is unlikely that the participants were aware of the proper conduct of SDM. There is therefore a need for PHC providers to be acquainted with the steps engaged in the conduct of SDM and be trained on how to practise them in sync with good consultation.22
Knowledge, attitude and practice of participants on prostate cancer screening and early diagnosis
Knowledge
Almost two-thirds (64.8%) of the participants in this study had poor knowledge. In a similar study35 among primary care physicians in Saudi Arabia, the mean knowledge score was 54.3%. The overall poor knowledge among the participants in the present study may be because of the varied cadre of PHC providers with varied levels of knowledge. As seen in Table 3, the mean knowledge score for family physicians was 70.1% compared with CHWs with 26.1%. Diverse questions may arise from patients during the process of SDM. Primary health care providers' sound knowledge of the screening tests (and their interpretations), diagnosis, investigations, treatment modalities, complications (of the disease and treatment), among others, is essential to conduct an efficient SDM process.
Good knowledge had a statistically significant association with the following factors: state-employed PHC providers (p < 0.001), being a GP or medical officer (p < 0.001) and having previously conducted PCa screening or given relevant health talks (p < 0.001). Reiterative education and practice of this subject is therefore important.
Poor knowledge, on the other hand, had a statistically significant association with the following factors: female PHC providers (p < 0.001), no previous CME on PCa topics (p < 0.001), uninvolved in medical student training (p < 0.001), unaware of the SAPDTG11 (p < 0.001) and no PCa screening guidelines at practice site (p = 0.044). The same explanation (as given) holds; a lack of opportunities and activities promoting reiterative education on this subject may gradually impact negatively on the knowledge.
Attitude
There was an overall prevalence of a neutral attitude (58.6%) among the participants. In a Saudi Arabian study,35 the mean total attitude score was greater than the midpoint. In the same Saudi Arabian study,35 most participants believed that early detection of PCa through screening could improve the survival of men. Similarly, the majority of the participants in this study believed there is value in early diagnosis through screening. However, about 40% of the participants felt specialists should perform PCa screening, as observed from their response to the following statement: 'It is more appropriate for specialists to screen for PCa'. This is unlike the finding in the Saudi Arabian study,35 where most of the participants accepted PCa screening as their role.
Participants' responses to the statements, 'I will conduct PCa screening on any man requesting it' and 'PCa screening is unnecessary in men > 70 years' could imply that some of them may engage in an irrational screening approach. Also, there seems to be an inadequate understanding of the use and interpretation of the screening tests, as the majority of the participants felt that PSA and DRE are accurate screening tests for PCa.
Most of the participants agreed to the following statements: 'There is evidence to support using DRE for PCa screening on asymptomatic men with no risk factors' and 'There is enough evidence to support using PSA for PCa screening on asymptomatic men with no risk factors'. This is in contrast to a study34 carried out among physicians, where only about a fifth agreed to these statements. Primary health care provider information provided to patients during SDM could therefore be questionable, in the study setting.
Over 40% of the participants were either neutral or agreed to the statement, 'DRE is unaccepted by South African men, so PHC practitioners should avoid it'. This belief might have informed their response to the statement, 'I am uncomfortable with practice relating to men's health', to which over 40% either agreed or were neutral. Being a female PHC provider was associated with being uncomfortable with practices relating to men's health (p = 0.003).
Factors found to be significantly associated with a positive attitude towards PCa screening include state-employed PHC providers (p < 0.001), 1-5 years' working experience (p = 0.014) and awareness of the SAPDTG11 (p = 0.027). Factors associated with a negative attitude towards PCa screening include being a female PHC provider (p = 0.029), no previous CME on PCa topic (p = 0.047) and poor knowledge of PCa screening (p < 0.001). As stated earlier, female PHC providers (mostly nurses) are gradually avoiding certain clinical functions relating to men's health. This may be because of certain perceptions and beliefs, particularly PHC provider and patient gender differences. This is further compromised by the scarcity of continued healthcare education on this subject. Knowledge was a top determinant of attitude towards PCa counselling and screening, as confirmed in a similar study by Arafa et al.35
Practice
There was an overall prevalence of poor practice (40%) among the participants. The responses of the participants to the following practice statements: 'I am able to counsel patients on the benefits of PSA testing', and 'I am able to discuss the various treatment modalities of PCa with my patients' could imply their inability to conduct an effective SDM process; this is also reflected in their self-reported practice on SDM (Table 2). In a similar study,26 60% of the primary care physicians would discuss the implication of an abnormal PSA test before performing it, and 20% would discuss the treatment modalities for PCa before screening. There may be the need to review the consultation styles of PHC providers in this setting.
Almost 60% of the participants responded positively to the practice statement, 'I am able to take a proper history in order to identify risk factors and symptoms of PCa from patients'; this is a reflection of their satisfactory knowledge on the risk factors and symptoms of PCa.
The majority of the participants who responded negatively to the practice statement 'I am able to examine the prostate by DRE' and 'I am able to detect palpable abnormalities on the prostate during DRE' were nurses. According to the former head, School of Nursing, UFS (Prof. Magda Mulder 2020, personal communication, June 13), nurses' practice of DRE is gradually fading, despite being within their scope of practice. Time constraints running busy clinics might hinder this practice in the study setting. With proper training of PHC providers (especially nurses) and time management, opportunistic screening in the form of annual DRE and PSA checks can be included in men's regular care.
More than three-quarters (75.8%) of the male participants in this study would consider having PCa screening on themselves. In a similar study,26 almost 90% of the participants would consider going for a PSA test. Factors found to be significantly associated with good practice of PCa screening include: being a state-employed PHC provider (p < 0.001), 1-5 years working experience (p < 0.001), being a medical officer or GP (private practice) (p < 0.001), having additional postgraduate qualifications (p = 0.041), awareness of the SAPDTG11 (p < 0.001) and previous conduct of PCa screening (p < 0.001).
Factors found to be significantly associated with poor practice include: no previous CME on the topic of PCa (p < 0.001), not having a men's clinic in practice (p = 0.005), being uninvolved with medical student training (p < 0.001), no PCa screening guidelines in the practice (p < 0.001), poor knowledge on PCa screening (p < 0.001) and a negative attitude towards PCa screening (p < 0.001). In a similar study,26 factors associated with an inclination of the primary care physician to screen men for PCa were the older age group, longer duration of practice and those who would consider having PSA conducted on themselves.
Barriers to prostate cancer counselling and screening
Top self-reported barriers to PCa counselling and screening were a lack of knowledge among healthcare practitioners and 'at risk' men and inadequate skills among healthcare practitioners. In a similar study,35 apart from the lack of skills and knowledge, refusal of patients and PCa not being viewed as a public health concern were the barriers to screening and counselling for the disease.
Need for additional learning
The majority of the participants felt the need for additional learning in the following topics relating to PCa: (1) risk factors and counselling, (2) symptoms, (3) the value of nutrients, (4) the value of PSA testing, (5) the value of DRE, (6) diagnosis and (7) treatment. The preferred methods of instruction suggested by the majority included study materials, practical sessions, simulated scenarios and group tasks.
Continuing professional development refers to the education that follows certification and licensure and has been shown to improve healthcare provider practice and, in some instances, healthcare outcomes.39 Experts suggest the need for the development of more effective courses for PHC providers (especially the nurses, clinical associates and CHWs) to enhance their educational background, thereby improving their collaborative functionality within the PHC system.40,41
While the importance of continued healthcare provider education has been described, there is a lack of research on the specific strategies to provide this education. The following have been shown as effective methods of instruction among CHWs: (1) role play, (2) case studies, (3) teach-back, (4) group presentation, (5) interactive didactic, (6) demonstration, (7) group assessment, (8) group discussion, (9) hands-on practice and (10) individual assessment.42 In the nursing profession, commonly used practices for continuing nursing education are short, repeated education; the use of interactive techniques, for example, simulation models; audio-visual learning modalities; teamwork in healthcare settings; use of cultural context; and the practice of assessment and feedback.43
To maximise the outcome of CPD activities, the preferred learning styles and methods of the targeted audience need to be considered. A survey among PHC physicians showed a higher preference for learning about cancer screening through the following educational formats: conferences; self-directed, small group workshops; hospital rounds; and online CME and CPD.39
Recommendations
The identified KAP gaps and the self-reported additional knowledge needs should be addressed in the medical undergraduate curriculum and CPD activities and refresher courses developed for practising PHC providers, bearing in mind their preferred learning methods. Women constitute the majority among the PHC providers in the study setting; measures should be put in place to improve their confidence during PCa counselling and screening and other practices relating to men's health.
Community health workers in conjunction with the Ward-Based Outreach Team (WBOT) provide PHC services (including health education and promotion) from household to household; there is therefore the need to channel adequate resources towards their proper training, mentoring and coordination. Family physicians who are champions of PHC should be saddled with the coordination and provision of these teaching and learning needs in the community.
Strengths and limitations
To the best of our knowledge, this is the first KAP study on PCa among a wide range of PHC providers in South Africa. This study offered the participants the opportunity to determine their learning needs as well as their preferred learning methods on the subject of PCa; the study's findings may therefore be a valuable tool in planning the needful intervention.
Study limitations include that the study was conducted among PHC providers in the Free State; therefore, it may not be generalised to other populations or other specialised healthcare providers in the country. The ongoing coronavirus disease 2019 (COVID-19) pandemic limited access to GPs in private practice. As a result of the diversified cadres of healthcare providers, multiple sampling methods were engaged in this study; some degree of selection bias is possible. Of note is the unequal gender distribution among participants in this study, with women dominating; this likely affected some of the bivariate analysis. Although the questionnaire items were basic and unambiguous, the possibility of information bias should be borne in mind because of the diverse scope of practice among various cadres of healthcare providers. Lastly, the use of self-reported data in some aspects of the study made it prone to recall bias.
Conclusions
Women, who constituted the majority of the participating PHC providers in this study, have appreciable KAP gaps relating to PCa screening. There is also a likelihood of poor knowledge on the proper conduct of SDM, which is an important subject and prerequisite, owing to the controversies regarding PCa screening; therefore, there is the likelihood of improper conduct of PCa screening. The participants' perceived need for additional knowledge on the subject and preferred learning methods were determined. Factors associated with their KAP were also identified, which indicated the need for reiterative learning and teaching on this subject.
Acknowledgements
The authors would like to thank the various cadres of primary health care providers who participated in this study. Thanks also go the departments of Family Medicine, Urology and Biostatistics for their support.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Authors' contributions
M.O.A.B. conceptualised the study with input from W.J.S., F.M.C. and N.M. M.O.A.B. collected the data. C.v.R. and M.O.A.B. conducted data analysis. M.O.A.B. wrote the manuscript. All authors reviewed the manuscript, gave critical input and approved the final version.
Funding information
The study was conducted with financial assistance from the Faculty of Health Sciences, University of the Free State, through the Three Schools of Medicine Research and Postgraduate Committee. The contents of this document are the sole responsibility of the authors.
Data availability
The data that support the findings of this study are available from the corresponding author, M.O.A.B., upon reasonable request.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of any affiliated agency of the authors.
References
1.World Health Organization. Non-communicable diseases [homepage on the Internet]. Geneva: World Health Organization; n.d. [cited 2021 Sep 09]. Available from: https://www.who.int/health-topics/noncommunicable-diseases#tab=tab_1 [ Links ]
2.World Health Organization (WHO) global meeting to accelerate progress on SDG target 3.4 on noncommunicable diseases and mental health. East Mediterr Health J. 2021;27(5):524-525. https://doi.org/10.26719/2021.27.5.524 [ Links ]
3.Seraphin TP, Joko-Fru WY, Kamaté B, et al. Rising prostate cancer incidence in Sub-Saharan Africa: A trend analysis of data from the African Cancer Registry Network. Cancer Epidemiol Biomarkers Prev. 2021;30(1):158-165. https://doi.org/10.1158/1055-9965.EPI-20-1005 [ Links ]
4.Siegel DA, O'Neil ME, Richards TB, Dowling NF, Weir HK. Prostate cancer incidence and survival, by stage and race/ethnicity - United States, 2001-2017. MMWR Morb Mortal Wkly Rep. 2020;69(41):1473-1480. https://doi.org/10.15585/mmwr.mm6941a1 [ Links ]
5.Jiang S, Narayan V, Warlick C. Racial disparities and considerations for active surveillance of prostate cancer. Transl Androl Urol. 2018;7(2):214-220. https://doi.org/10.21037/tau.2017.09.11 [ Links ]
6.Tindall EA, Monare LR, Petersen DC, et al. Clinical presentation of prostate cancer in black South Africans. Prostate. 2014;74(8):880-891. https://doi.org/10.1002/pros.22806 [ Links ]
7.Dewar M, Kaestner L, Zikhali Q, Jehle K, Sinha S, Lazarus J. Investigating racial differences in clinical and pathological features of prostate cancer in South African men. S Afr J Surg. 2018;56(2):54-58. https://doi.org/10.17159/2078-5151/2018/v56n2a2324 [ Links ]
8.Mofolo N, Betshu O, Kenna O, et al. Knowledge of prostate cancer among males attending a urology clinic, a South African study. Springerplus. 2015;4:67. https://doi.org/10.1186/s40064-015-0824-y [ Links ]
9.Free State Department of Health. Annual performance plan, Free State Department of Health 2020/21. Bloemfontein: Free State Department of Health; 2021. [ Links ]
10.Tracy CR, Brooks NA, Said M. Prostate cancer workup [homepage on the Internet]. Medscape; 2021 [updated 2021 Feb 02; cited 2021 Sep 09]. Available from: https://emedicine.medscape.com/article/1967731-workup#c7 [ Links ]
11.Segone AM, Haffejee M, Wentzel S, et al. Prostate cancer diagnostic and treatment guidelines [homepage on the Internet]. Johannesburg: The Prostate Cancer Foundation of South Africa; 2013 [cited 2019 Oct 03]. Available from: https://prostate-ca.co.za/wp-content/uploads/2017ProstateGuidelinesDraftVersion2016.pdf [ Links ]
12.Harvard Health Publishing. Harvard Medical School. PSA: Prostate-specific antigen, persisting scientific ambiguities [homepage on the Internet]. 2009 [cited 2019 Nov 30]. Available from: https://www.health.harvard.edu/newsletter_article/PSA-Prostate-Specific-Antigen-Persisting-Scientific-Ambiguities [ Links ]
13.Basourakos SP, Gulati R, Vince RA Jr, et al. Harm-to-benefit of three decades of prostate cancer screening in Black men. NEJM Evid. 2022;1(6):10.1056/evidoa2200031. https://doi.org/10.1056/evidoa2200031 [ Links ]
14.US Preventive Services Task Force, Grossman DC, Curry SJ, et al. Screening for prostate Cancer: US Preventive Services Task Force Recommendation Statement [published correction appears in JAMA. 2018;319(23):2443]. JAMA. 2018;319(18):1901-1913. https://doi.org/10.1001/jama.2018.3710 [ Links ]
15.Kinyao M, Kishoyian G. Attitude, perceived risk and intention to screen for prostate cancer by adult men in Kasikeu Sub Location, Makueni County, Kenya. Ann Med Health Sci Res. 2018;8:125-132. [ Links ]
16.Baratedi WM, Tshiamo WB, Mogobe KD, McFarland DM. Barriers to prostate cancer screening by men in Sub-Saharan Africa: An integrated review. J Nurs Scholarsh. 2020;52(1):85-94. https://doi.org/10.1111/jnu.12529 [ Links ]
17.Berglund G, Nilsson S, Nordin K. Intention to test for prostate cancer. Eur J Cancer. 2005;41(7):990-997. https://doi.org/10.1016/j.ejca.2005.01.011 [ Links ]
18.Weinrich SP. Prostate cancer screening in high-risk men: African American Hereditary Prostate Cancer Study Network. Cancer. 2006;106(4):796-803. https://doi.org/10.1002/cncr.21674 [ Links ]
19.Kalani L, Aghababaeian H, Nosratabadi M, et al. Prostate cancer screening behavior based on the Health Belief Model in men aged over 40 years. Trends Med Sci. 2022;2(2):e119524. https://doi.org/10.5812/tms-119524 [ Links ]
20.Eales OO, Smith S. Do socio-economically disadvantaged patients prefer shared decision-making?. S Afr Fam Pract. 2021;63(1):e1-e6. https://doi.org/10.4102/safp.v63i1.5293 [ Links ]
21.American Cancer Society. Cancer facts & figures 2019 [homepage on the Internet]. Atlanta, GA: American Cancer Society; 2019 [cited 2019 May 10]. Available from: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2019/cancer-facts-and-figures-2019.pdf [ Links ]
22.Ng CJ, Lee PY. Practising shared decision making in primary care. Malays Fam Physician. 2021;16(1):2-7. https://doi.org/10.51866/cm0001 [ Links ]
23.Kappen S, Jürgens V, Freitag MH, Winter A. Early detection of prostate cancer using prostate-specific antigen testing: An empirical evaluation among general practitioners and urologists. Cancer Manag Res. 2019;11:3079-3097. https://doi.org/10.2147/CMAR.S193325 [ Links ]
24.Leyva B, Persoskie A, Ottenbacher A, et al. Do men receive information required for shared decision making about PSA testing? Results from a national survey. J Cancer Educ. 2016;31(4):693-701. https://doi.org/10.1007/s13187-015-0870-8 [ Links ]
25.Berberabe T. 'Using common sense' in prostate cancer screening debate [homepage on the Internet]. Targeted Oncology; 2015 [cited 2019 Oct 03]. Available from: https://www.targetedonc.com/view/using-common-sense-in-prostate-cancer-screening-debate [ Links ]
26.Tun Firzara AM, Ng CJ. Knowledge and practice of prostate cancer screening among general practitioners in Malaysia: A cross-sectional study. BMJ Open. 2016;6(9):e011467. https://doi.org/10.1136/bmjopen-2016-011467 [ Links ]
27.Johnson K, Chang M, Sun Y, Miyake M, Rosser CJ. Attitudes and knowledge of primary care physicians regarding prostate cancer screening. J Cancer Educ. 2013;28(4):679-683. https://doi.org/10.1007/s13187-013-0533-6 [ Links ]
28.Mbugua RG, Karanja S, Oluchina S. Effectiveness of a community health worker-led intervention on knowledge, perception, and prostate cancer screening among men in rural Kenya. Adv Prev Med. 2022;2022:4621446. https://doi.org/10.1155/2022/4621446 [ Links ]
29.PedrosaTorres RL, Silva MH, Melo TR, Santos OC, Mendonça EF, Mota SM. Nursing role in promoting and prevention to prostate cancer. Glob J Nurs. 2018;1(2):1. https://doi.org/10.28933/GJON [ Links ]
30.Department of Health. Provincial guidelines for the implementation of three streams of PHC re-engineering. Pretoria: Department of Health; 2011. [ Links ]
31.StatsSA. Census 2011. 2011 [cited 2022 Apr 24]. Available from: https://www.statssa.gov.za/?page_id=993&id=mangaung-municipality [ Links ]
32.Myburgh JJ, Claassen FM. The association between increase in Gleason score, age and ethnicity in men with prostate cancer in central South Africa. Abstract presented at: South African Urological Association Conference; 2018 Sep 20-23; Stellenbosch (Unpublished) [ Links ]
33.Raosoft. Sample size calculator. 2004 [cited 2020 Mar 04]. Available from: http://www.raosoft.com/samplesize.html [ Links ]
34.Arafa MA, Rabah DM, Abdel-Gawad E, Ibrahim FK. Association of physicians' knowledge and behavior with prostate cancer counseling and screening in Saudi Arabia. Saudi Med J. 2010;31(11):1245-1250. [ Links ]
35.Arafa MA, Rabah DM, El-Nimr NA. Physicians' behavior and attitudes towards prostate cancer screening in Riyadh, Saudi Arabia. J Med Med Sci. 2012;3(1):43-48. [ Links ]
36.Yimer M, Abera B, Mulu W, Bezabih B. Knowledge, attitude and practices of high risk populations on louse-borne relapsing fever in Bahir Dar City, North-West Ethiopia. Sci J Public Health. 2014;2(1):15-22. https://doi.org/10.11648/j.sjph.20140201.13 [ Links ]
37.Benedict M, Steinberg WJ, Raubenheimer JE. Knowledge of the management of postpartum haemorrhage by doctors and midwives working in Free State district hospitals. Afr J Nurs Midwifery. 2016;18(2):146-161. https://doi.org/10.25159/2520-5293/812 [ Links ]
38.Houman JJ, Eleswarapu SV, Mills JN. Current and future trends in men's health clinics. Transl Androl Urol. 2020;9(Suppl 2):S116-S122. https://doi.org/10.21037/tau.2019.08.33 [ Links ]
39.Lynn B, Hatry A, Burnett C, Kan L, Olatunbosun T, Bluman B. Identifying primary care physicians continuing education needs by examining clinical practices, attitudes, and barriers to screening across multiple cancers. J Cancer Educ. 2018;33(6):1255-1262. https://doi.org/10.1007/s13187-017-1240-5 [ Links ]
40.Mash R, Blitz J. Overcoming challenges in primary care education in South Africa. Educ Prim Care. 2015;26(4):274-278. https://doi.org/10.1080/14739879.2015.11494355 [ Links ]
41.Snyman S, Von Pressentin KB, Clarke M. International classification of functioning, disability and health: Catalyst for interprofessional education and collaborative practice. J Interprof Care. 2015;29(4):313-319. https://doi.org/10.3109/13561820.2015.1004041 [ Links ]
42.Lightfoot M, Palazuelos D. Evaluating the teaching methods of a community health worker training curriculum in rural Guatemala. J Family Med Community Health. 2016;3(6):1096. [ Links ]
43.Azad A, Min JG, Syed S, Anderson S. Continued nursing education in low-income and middle-income countries: A narrative synthesis. BMJ Glob Health. 2020;5(2):e001981. https://doi.org/10.1136/bmjgh-2019-001981 [ Links ]
 Correspondence:
Correspondence:
Matthew Benedict
BenedictMA@ufs.ac.za
Received: 02 June 2022
Accepted: 12 Nov. 2022
Published: 28 Feb. 2023














