Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
African Journal of Primary Health Care & Family Medicine
versão On-line ISSN 2071-2936
versão impressa ISSN 2071-2928
Afr. j. prim. health care fam. med. (Online) vol.12 no.1 Cape Town 2020
http://dx.doi.org/10.4102/phcfm.v12i1.2155
ORIGINAL RESEARCH
Peer-learning reviews to improve Gauteng community-oriented primary care: Findings from AitaHealth™-enabled ward-based outreach teams
Tessa S. MarcusI; Elizabeth RejiII, III; Sanele NgcoboIV
IDepartment of Family Medicine, School of Medicine, Faculty of Health Sciences, University of Pretoria, City of Tshwane, South Africa
IIDepartment of Family Medicine, School of Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIDepartment of Family Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IVClinical Associate Programme, Department of Family Medicine, School of Medicine, Faculty of Health Sciences, University of Pretoria, City of Tshwane, South Africa
ABSTRACT
BACKGROUND: In 2016 the Gauteng Department of Health engaged University of Pretoria Family Medicine to provide` education, training and information and communication technology support for the phased scale-up of ward-based outreach teams (WBOTs) through community-oriented primary care (ICT-enabled COPC). As in all service delivery, quality assurance is essential. In contemporary best practice, it brings together peer-to-peer learning and quality improvement (QI) in what is termed here as peer-learning reviews (PLRs
AIM: To assess implementation fidelity and assure the quality of community-based healthcare services
SETTING: This study was conducted in two districts of Gauteng province, South Africa
METHODS: A 3-day PLR of paired WBOTs was conducted by multi-disciplinary teams of academics, partners and site-selected healthcare practitioners. Guided by a benchmark survey distilled from the seven COPC practice elements, they conducted individual interviews, accompanied WBOT members in field and facilitated solution-focused peer exchange workshops with all participants
RESULTS: At all sites there was clear evidence of achievements and practical challenges with respect to mapping; support, networks and partnerships; infrastructure and functional equipment; work integrated learning; data and service activities; and performance status and management. Methodologically, PLRs supported inclusive, context-specific learning for all along the healthcare service pathway. They generated action plans derived from shared understanding and joint decision-making
CONCLUSION: The PLRs and the implementation results demonstrate the importance of structuring learning into service and research. Both helped develop participants' abilities to understand what they do, do their work, grow their sense of self-worth and improve their relationship with others
Keywords: Peer learning; Quality improvement; ICT-enabled community-oriented primary care; Community healthcare; Primary health re-engineering.
Background
The success of healthcare reform in South Africa1 hinges on services that can respond to the complexity of health in context.1,2 A system that is functional, provides quality care and is universally accessible needs to integrate healthcare from the home to and from health facilities through levels of services and across public, private, non-governmental and traditional sectors.3 Guided by community-oriented primary care (COPC), services should be rendered by multi-disciplinary teams of healthcare professionals and workers informed by the best available practices and knowledge. Delivery should be geographically focused, person- and family-centred, comprehensive, generalist and equitable.4
In COPC, the community-based service delivery pathway involves identifying the community, defining a team's collective and individual practice boundaries, identifying the population as well as the resource asset base within it and then providing services. Workplace learning is structured into the service pathway through information technology (IT) as well as organised curriculation in order to continuously develop the individual and collective capacity of healthcare providers.
As in all service delivery, quality assurance is essential. In the health setting, quality improvement (QI) usually focuses on aspects of clinical care and system performance.5 Methodologically, QI initiatives are professional and researcher-led projects that are commonly conducted internally within units, components or teams. In COPC, a quality assurance peer-learning review (PLR) process has been developed. Informed by peer-to-peer learning initiatives,6 peer and learning are explicitly included in the terminology. Peer-learning reviews are processes and activities that bring learning and QI together around areas of service practice to support implementation fidelity and improve service quality. Peer-learning reviews also respond to the need to make the process internally productive, to encourage QI as ongoing and integral to performance rather than as stand-alone, once-off activities and to remove any audit or inspection connotations.
At the end of 2016, the Gauteng Department of Health engaged the University of Pretoria's Department of Family Medicine (UP-DFM) to provide education, training and IT support for the phased scale-up of ward-based outreach teams (WBOTs) through information and communication technology-enabled community-oriented primary care (ICT-enabled COPC).7 Envisaged as the first of several waves, implementation began in 2017 with a cohort of up to 40 teams (eight teams per district) selected from existing functioning WBOTs where community health workers (CHWs) had completed the national Department of Health's 10-day Phase 1 CHW training programme.
AitaHealth™ is a custom-built, gadget and web electronic data and human resource management support IT platform. It enables information, service and relationship continuity, as well as service and performance management.9
This article presents the results of PLRs of ICT-enabled COPC implementation in two districts of Gauteng province. The PLRs were undertaken between 03-05 October 2017 (Site 1) and 12-14 October 2017 (Site 2) with 16 WBOTs using AitaHealth™. They had been operational for between 6 and 3 months (Site 1: April-September; Site 2: July-September), during which time they had registered 5208 and 2096 households and 17 420 and 6312 individuals, respectively.
Methods
Study design
The PLR process is a structured undertaking designed to develop individual, team and management ability to self-assess and improve the quality of their practice. The purpose of PLRs is to monitor the fidelity of implementation of community-based services in a systematic way, identify best practices and critical challenges, and develop adaptive action plans through reflection to improve practice. The methodology has been developed and extensively tested by the 'Cities exchanging on local energy leadership' (CASCADE) and several other European Union projects, as well as in South Africa.6
Setting
The study was conducted in West Rand and Ekurhuleni districts of Gauteng province, South Africa. The districts differ significantly in population size and density (Ekurhuleni 1609/km2 and West Rand 200/km2) although their demographic characteristics are similar. In 2016, Ekurhuleni had a population of some 3.38 million people, with 52% of 1.3 million households having two or fewer inhabitants. West Rand had an estimated population of 838 600 people living in 330 572 households, with 51% having two or fewer inhabitants.8 Neither site has the requisite organisational arrangements to support fully functional community-based service delivery.
Selection of participants
The data reported in this article come from a PLR of 16 teams made up of 16 enrolled or professional nurse team leaders (eight outreach team leaders [OTLs] per site) and 139 CHWs (71 at Site 1 and 68 at Site 2) Table 1 describes the field work process.
At Site 1, 12 participants completed the benchmark guide as a survey: five CHWs, three facility managers and four OTLs. There were 31 participants in the peer exchange workshop: nine CHWs, one family physician, 10 OTLs, two WBOT coordinators and nine members of the University of Pretoria/International Training and Education Center for Health (UP-I-TECH) team. At Site 2, 11 participants completed the benchmark guide as a survey: four CHWs, two facility managers, four OTLs and one WBOT coordinator. There were 33 participants in the peer exchange workshop: 13 CHWs, one family physician, nine OTLs, three WBOT coordinators and seven UP-I-Tech team members.
Data collection
To understand the practices and assess progress in WBOT implementation, key elements of the COPC pathway were translated into seven COPC practice benchmarks. These are (1) mapping; (2) support, networks and partnerships; (3) infrastructure and functional equipment; (4) work integrated learning; (5) data; (6) service tasks and activities; and (7) performance status and management approach. The benchmarks were developed into an interview guide, which was used as a tool to collect the data.
The PLR was conducted by multi-disciplinary teams of academics (UP-DFM), partners (I-Tech-South Africa) and site-selected healthcare practitioners (district/subdistrict/facility managers, clinicians, team leaders and CHWs).
Data were collected by using the benchmark interview guide. It was completed individually as a survey (face-to-face or self administered) by up to three people per team on the day of the site visit, either prior to or after going out into the field. The benchmark guide was also used to direct field visit interactions and observations. Field notes were taken by reviewers, collated, shared and cross-referenced with the team, and developed into presentations for discussion at the peer-learning exchange workshop. At the workshop, feedback was noted and incorporated into the data where it was used to support reflection and planning. A report was prepared for and shared with the WBOT coordinators of the respective sites.
Data analysis
The results of the PLR were collated and analysed using the benchmark guide as an analytic framework. The framework is organised thematically. Data recorded on paper were captured electronically on Microsoft Word or on Qualtrics® survey and analytic software.
Ethical considerations
Informed consent was obtained from all participants involved in the benchmark surveys, field work and peer exchange workshops. Confidentiality and privacy were strictly adhered to and no names of individuals were recorded or made known in the collection or reporting of information. Data analysis was performed during and after collection. The study did not involve patients. The study was granted ethical clearance by the Research Ethics Committee of the Faculty of Health Sciences, University of Pretoria (Ethics reference number: 102/2011).
Results
Drawing on the benchmarks in the guide, the results are presented thematically as follows: mapping; support, networking and partnerships; infrastructure and functional equipment; learning in the workplace; activities, service organisation and supervision; and recommendations and forward planning.
Mapping
In the implementation of COPC, mapping is used to identify WBOT community practice areas, allocate CHWs to households and identify local organisations and institutions within them.
Community healthcare practice areas and households
In terms of mapping community healthcare practice areas, teams all indicated that they used and created maps of their areas and households both as a desktop activity and through physical mapping. They used maps to allocate teams and CHWs to physical areas and households. The mapping of CHW practice area households itself was mostly done using hand-drawn maps. Mapping was used to verify available settlement information, while maps were used to support in-field service management (Table 2).
Ward-based outreach teams encountered several mapping and household verification challenges. Through the process of mapping the teams found the numbers attributed to stands on municipal maps to be non-sequential and almost always out of date. They found buildings were put to multipurpose use. A team leader at Site 1 said they found tuckshops converted to rooms to accommodate tenants, for example. They discovered that people migrate into areas as well as in and out of households after CHWs have physically verified households and tenants. Community health workers also had problems of access, particularly locked gates, dogs in yards and people away at work during the week, as well as security guards.
Amongst the teams there was some variation in terms of where maps were stored and displayed. Cadastral maps were either kept at the facility or returned when they had been borrowed. Hand-drawn maps were sometimes kept by the CHWs who created them. Otherwise, these too were kept by OTLs at facilities, either in files or, more rarely, on display on the facility office wall.
Mapping organisations and institutions
The mapping of organisations in communities is also part of initial operationalisation as well as the ongoing functioning of COPC. Organisational mapping was used to identify stakeholders and partners. As with households and individuals, CHWs found service providers also moved around and were not permanent.
Teams are expected to use the 'local institutional support assessment' (LISA) tool to help determine the institutional community asset base. However, most teams said that they either had not used the tool at all or had used it sporadically. This was partly because they did not have copies of the paper-based instrument or partly because they saw the tool as 'paperwork', a bureaucratic formality rather than as something useful to them. Those who had used the LISA tool said they found it useful.
Support, networking and partnerships
Creating and maintaining relationships are important for the establishment and ongoing practice of community-based service delivery. In the PLR, participants described their relationships with individuals, families and communities, as well as with healthcare and other service providers (Table 3).
Individuals, families and communities
Participants described their relationships with the individuals, families and communities as generally positive. These relationships, however, are not automatic or easy to achieve. When CHWs go to people's homes, they often have to manage negative attitudes and behaviour as well as general service expectations. Teams said that they tried to reduce resistance by working with local authorities and ward committees as well as the clinic committees, where they are represented usually by the WBOT coordinator or facility managers. They also said that they overcame barriers through perseverance and persuasion as well as by delivering services that people need.
Health and other service providers
In terms of WBOT functioning in the public healthcare service in Gauteng, WBOT coordinators provide direct active support to teams and team leaders. Teams reported that coordinators routinely assisted with service and training, as well as when they had challenges in their communities or in the workplace. As WBOTs are clinic based, their relationships with facility managers and staff are particularly important. Teams said that they were given equipment and participated in monthly facility meetings and training sessions.
However, they also faced several critical organisational and relationship challenges. Participants reported organisational tensions between clinic and community service priorities that influence their work. Multiple reporting lines meant that facility managers struggled with their dual responsibilities and some acknowledged that they were often not available. At the same time, team leaders and CHWs felt under-supported or, as one CHW put it, supported 'only for clinic responsibilities'.
Outreach team leaders and CHWs felt that facility management and staff failed to take account of their work. Their poor understanding of and disrespect for what WBOTs do were evident in practical interactions. Team leaders are expected to work in the clinic and with WBOTs in the community. Outreach team leaders and CHWs are often substituted willy-nilly for absent staff. At facilities, WBOT work is not fast-tracked, although OTLs said that they are helped with equipment and patient treatment and do not have to queue to collect medications. They also reported insufficient back referral and a lack of clarity on the referral flow. A facility manager (WR5, facility manager, female, 04 October 2017), for example, said she did not know 'which flow to use' to back refer to specific CHWs.
Organisational privileging of facilities over WBOTs is also expressed in OTL and CHW terms of employment. As part of clinic staff, OTLs said they interacted routinely with nurses and sporadically with family physicians at clinics or during training. By contrast, CHWs, who are not part of the clinic staff, said that they are treated differently and made to feel marginal even though many had good relationships with individual clinic personnel.
Within facility services, WBOTs have a strong, but fairly one-sided relationship with the human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS), sexually transmitted infection (STI) and tuberculosis (TB) (HAST) vertical program.
Outside of primary healthcare clinics, the WBOTs' strongest working relationships are with social development and related 'third sector' non-governmental organisation (NGO) and faith-based organisation (FBO) welfare partners. Social workers were described in the PLRs as key integrators. Through NGO and FBO partnerships, CHWs and OTLs said they help families and individuals get assistance with grants, blankets and food parcels. They also make and receive referrals and ensure clients get home-based and rehabilitative care. Partner organisations in some places also allow them to use their facilities to run support groups and training.
The study participants said that the relationship of WBOT with local businesses was limited. In Site 1, examples were given about local tuckshops that offered bread and other drinks during events, and an undertaker who allowed CHWs to use his or her venue to give health talks. In Site 2, WBOTs involved local tuckshops in condom distribution.
Infrastructure and functional equipment
All teams faced basic infrastructural and functional equipment constraints. Space was a major constraint everywhere. The lack of workspace affected the ability of teams to meet, supervise and support workplace learning. There were limited or no resources for photocopying and often they did not have filing and storage space.
The then Gauteng Department of Health requirement that CHWs clock in and out at facilities was a challenge. Participants said that daily they lost time walking to and from the facility. Their work was further disrupted when there were electricity outages because they had to wait to clock in, in order to be paid for the day's work.
In terms of equipment, all teams were equipped with tablets to support electronic data collection and service delivery. In field, however, it was observed that a number of CHWs did not have paper-based referral forms and had to verbally refer clients without supporting documentation (Peer Exchange Workshop, 12/10/2017). They lacked essential equipment needed to provide community-based healthcare, including blood pressure machines, masks, urine dipsticks, glucometers, gloves and information leaflets. They were also not provided by the system with uniforms, kitbags and name tags. At Site 2, these were eventually obtained by the WBOT coordinator through once-off assistance from a non-governmental partner working in the area.
Learning in the workplace
Continuous learning to support capacity development using a capability approach is structured into the routine of COPC. Learning sessions were routinised for all teams. They were held either weekly or fortnightly during their Friday management meetings and additionally when there was wet weather. They describe having covered a range of topics (Table 4).
There was a generally positive attitude to learning. Participants found learning personally rewarding and a source of pride. They said that the knowledge and skills they had gained made it easier for them to support households. They also said peer learning benefitted everyone. It had helped improve communication between team members, assisted them with their work and helped improve their tattitude towards one another. They also felt that it had helped them relate better to people in general.
Participants reported that IT gave them a better understanding of both service and learning needs. Facility managers and team leaders said they used screening data collected on AitaHealth™ to assist them in identifying the focus of training, while CHWs said the app helped them learn what to ask in different conditions. Teams described the technology as 'empowering' and that it had helped improve their individual and collective knowledge of diseases. Although the app guided practice, it was also recognised that team members needed to be supported to link new knowledge with the job process. As one facility manager observed (04.10/2017), 'things constantly change' and CHWs need to 'interpret how to intervene as most of it is not only health related'.
The participants pointed out several real learning challenges. In terms of content, it was generally recognised that more training is needed and that there is a need to provide teams with relevant equipment to practise skills that they are trained in. The participants said that they wanted OTLs to be upskilled, more topics to be covered and that topics should be covered in greater depth. In terms of communication, there was a language challenge that affected learning.
In the field, it was observed that CHWs' understanding of doing COPC through WBOTs needed to be deepened. Amongst other things, some found it difficult to explain why they register households and the informed consent process. They found it hard to ask some of the questions, for example, around HIV and AIDS and income, as well as to deal with refusals. They also were inclined to provide vertical rather than generalist services. And they needed more training on handling medications in the field to maintain the cold chain. Team leaders also needed timely preparation with new information in order for them to effectively support learning in their teams (Peer Exchange Workshops).
Other challenges in learning that participants identified relate to the absence of certification, the low 'levels of education' of some CHWs, unfamiliarity with technology and individual variation in motivation to learn.
Activities, service organisation and supervision
Activities
In a COPC approach, the purpose of the WBOTs is to provide comprehensive care appropriate to the level of service. Amongst the tasks required from CHWs is the registration of households and household triage, a screening process to engage with and respond to healthcare needs from the initiation of service contact.
Table 5 shows the extent of the community-based work collected on AitaHealth in the month preceding the peer review.
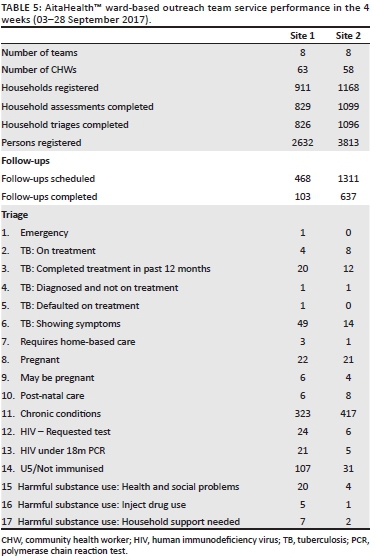
The participants said that in their community work they predominantly focus on health promotion and disease prevention, giving advice and making referrals to the clinics as needed. They also do treatment support and, to a lesser extent, palliative care. Team leaders and CHWs also worked at clinics. They said that they assist with triage, take vital signs and fetch files there. Teams also do clinic-related work in the community, particularly following up on patients who do not come for TB treatment.
Service organisation and supervision
Community health workers work in pairs for safety reasons. They are supervised and supported by OTLs. In turn, they and their teams are managed and supported by WBOT coordinators. Team leaders were described as being 'hands on'. They hold routine morning meetings. They accompany CHWs on supervised visits. They routinely run team management meetings, usually on Fridays. And they attend monthly team leader meetings with the WBOT coordinator (Table 6).
The participants reported that team leaders encouraged CHWs to have good work ethics and to work as a team, share responsibilities and build each other. Amongst other initiatives, OTLs rotate partners through teams to enable CHWs to share information, skills and experience. They also encourage CHWs to apply what they have learnt to themselves as well as to the people in the community.
Team members were actively made aware of possible future consequences of their practices, both through education and advice as well as through peer group pressure and formal disciplinary processes. When there are mistakes, CHWs said that they reported these to the OTLs. Team leaders either dealt with them directly or sought guidance from facility managers or WBOT coordinators.
Community health workers and OTLs are exposed routinely to distressing situations. In the field at both sites, it was observed that there was insufficient debriefing.
Recommendations and forward planning
In the peer review process, the purpose of the peer-learning exchange workshop is to generate a shared understanding of issues and to make recommendations and plans to improve practice. At both sites the teams generated practical recommendations that related to operational issues, work integrated learning and support (Table 7).
As part of forward planning, both sites then agreed on common tasks that all teams could action over the next 6 months. Site 1 WBOTs prioritised health promotion during service delivery and the improvement of LISA documentation, including the inclusion of LISA forms on AitaHealth™. Site 2 WBOTs prioritised strengthening relationships with all relevant local institutions, especially with the community policing forum in order to support CHWs working in dangerous areas, like hostels.
Discussion
As a methodology, PLRs apply participatory action research to understand and support implementation fidelity and encourage quality improvement processes. The results show that PLRs are able to generate a rich and multi-layered understanding of what it means to deliver healthcare services to people in their homes in the existing public primary health system. They are practically helpful for participants because they are structured to support inclusive, context-specific learning for everyone involved in the delivering of services, wherever they are located along the care pathway.
Peer-learning reviews are also of value to others. The benchmarks that guide the process are derived from assumptions about how WBOTs are expected to work and what they are supposed to do. The results show both the achievements and the challenges of making these assumptions reality. Particularly, they show how important context is to understanding why plans do not translate in linear and literal ways into practices. Thus, while mapping to define CHW and WBOT areas of practices may appear from above to be 'straightforward and once off', the view from below shows place and space as fluid, something to be navigated, something to be traversed many times. Similarly, the structural privileging of facility-based services in public primary healthcare organisationally marginalises CHWs and the work that WBOTs do. This is why it is possible for them to be taken out of the community to work in facilities and simultaneously not to be considered as facility staff, or to be expected to meet facility and patient needs without being properly equipped. The achievements of these teams show that the essential cooperation needed between levels of workers to ensure basic patient healthcare is hard won in a bureaucratised institutional hierarchy.
The PLR process and the implementation results demonstrate the importance of structuring learning into service and research. Both helped develop healthcare professionals' and workers' abilities to better understand what they do, do their work, grow their sense of self-worth and improve their relationship with others.
The study shows that PLRs make the practical issues and experiences of service delivery visible to all team members. And as elsewhere,10 the PLR processes of partnering and collectively reflecting on issues were found to be non-threatening, supportive of cooperation and encouraging of learning as an intrinsic part of doing. Individually and collectively they created an opportunity for participants to improve their own and others' healthcare abilities.
Limitations
The envisaged PLR process had to be modified because of meeting space and service demand constraints. These impacted inclusivity as not all facility managers and WBOT members were able to attend the peer exchange workshops. This may have led to the omission of some important issues or perspectives that would need to be picked up in future reviews. Also, although every effort was made to ensure that PLR teams included members with relevant experience and skills sets, practically variations in both these dimensions may have influenced the reporting and feedback received from each team. It is expected that individual and collective capacity to do PLR will improve with practice. The data presented reflect the outcome of the PLR process itself. Further research is needed to determine whether PLRs translate into improved practices. Lastly, doing ICT-enabled COPC is one of the many approaches to WBOT implementation in South Africa. This said, the principles, framework and processes of PLR can be applied to other applications and contexts in Africa and elsewhere.
Conclusion
The PLR methodology produces an intense experiential learning and self-monitoring process in which peers and colleagues engage with their work. As a facilitated process that is scaffolded by a benchmark guide that covers key deliverables as well as purposive interactions, it gives participants an overview of the work they do. They gain insight into their achievements and challenges and find possible solutions to improve their own well-being as well as their contribution to service delivery and individual, family and community health. As an 'own account', the PLR reveals the imperfect but substantial practice of community-based healthcare that can be achieved by ICT-enabled COPC delivered by WBOTS.
Amongst the lessons learnt from implementing the PLRs are that they need to accommodate local contexts, they should be scheduled into the annual district calendar at intervals of about 6 months and they need to be budgeted for financially and organisationally to ensure that venues, transport and refreshments enable inclusivity. In this way it is possible to maximise the benefits of PLRs without creating excessive demands on time and other resources.
Acknowledgements
The authors would like to thank Dr Leena Thomas, Site 1 and Site 2 clinicians, managers, trainers, team leaders and community health workers for their support. They would also like to thank the staff from I-TECH South Africa (Tshireletso Phatlhanyane, Nomkhosi Khoza, Sipho Mazibuko and Mary Jane Ratlhagana) and UP-DFM (Magdeline Maake, Pauline Matshego and Muzi Raseroka) for their assistance in the research.
Competing interests
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
T.S.M. declares that she was involved in the design, development and implementation of AitaHealth™ in the course of supporting service delivery. E.R. declares that she was involved in the implementation of AitaHealth™ in the course of supporting service delivery. S.N. declares that he was involved in the design and implementation of AitaHealth™ in the course of supporting service delivery.
Authors' contributions
T.S.M. was responsible for the conceptualisation and design of the study. Data collection and analysis were done by T.S.M., E.R. and S.N. T.S.M. and E.R. were responsible for interpretation framework. All authors contributed to the discussion and critical review of the article.
Funding information
The project was supported by the Health Resources and Services Administration (HRSA) Sub-Award (No. UWSC9688) to the University of Washington and the University of Pretoria Community-Oriented Primary Care Research Unit.
Data availability statement
Data sharing is not applicable for this study.
Disclaimer
The views expressed in this article are the authors' own and not the official position of the University of Pretoria, I-TECH South Africa, the University of Washington, HRSA, HHS or the US Government.
References
1. Schneider H, Okello D, Lehmann U. The global pendulum swing towards community health workers in low-and middle-income countries: A scoping review of trends, geographical distribution and programmatic orientations, 2005 to 2014. Hum Resour Health. 2016;14(1):65. https://doi.org/10.1186/s12960-016-0163-2 [ Links ]
2. Campbell J, Admasu K, Soucat A, Tlou S. Maximizing the impact of community-based practitioners in the quest for universal health coverage. Editorial. Bull World Health Organ. 2015;93(9):590-590A. https://doi.org/10.2471/BLT.15.162198 [ Links ]
3. Hugo J, Marcus T. Community-orientated primary care: Where there is a doctor. In: Mash B, editor. Handbook of family medicine. 4th ed. Cape Town: Oxford University Press Southern Africa, 2018; p. 334-359. [ Links ]
4. Marcus TS. COPC - A practical guide. Pretoria: Minuteman Press; 2018. [ Links ]
5. Van Deventer C, Mash B. African primary care research: Quality improvement cycles. Afr J Prim Health Care Fam Med. 2014;6(1):598. https://doi.org/10.4102/phcfm.v6i1.598 [ Links ]
6. EUROCITIES. CASCADE - Cities exchange on local energy leadership. Peer review manual V3, DeliverableNo3 [homepage on the Internet]. c2013 [cited 2019 May 21]. Available from: http://www.eurocities.eu/eurocities/projects/CASCADE-Cities-exchanging-on-local-energy-leadership&tpl=home [ Links ]
7. Gauteng Department of Health and University of Pretoria. GDoH and UP Service Level Agreement; 28092016 (Unpublished). [ Links ]
8. Marcus TS, Hugo J, Jinabhai CC. Which primary care model? A qualitative analysis of ward-based outreach teams in South Africa. Afr J Prim Health Care Fam Med. 2017;9(1):1252. [ Links ]
9. StatsSA Provincial Profile Community Survey 2016 [Homepage on the interrnet]. Report 03-01-09. [cited 2019 Oct 08]. Available from: http://www.statssa.gov.za/publications [ Links ]
10. Donnelly LF, Dorfman SR, Jones J, Bisset GS 3rd. Transition from peer review to peer learning: Experience in a radiology department. J Am Coll Radiol. 2018;15(8):1143-1149. https://doi.org/10.1016/j.jacr.2017.08.023 [ Links ]
 Correspondence:
Correspondence:
Tessa Marcus
tessa.marcus@up.ac.za
Received: 23 May 2019
Accepted: 17 Dec. 2019
Published: 05 Mar. 2020














