Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
African Journal of Primary Health Care & Family Medicine
On-line version ISSN 2071-2936
Print version ISSN 2071-2928
Afr. j. prim. health care fam. med. (Online) vol.9 n.1 Cape Town 2017
http://dx.doi.org/10.4102/phcfm.v9i1.1441
ORIGINAL RESEARCH
Perceptions of health care professionals on the safety and security at Odi District Hospital, Gauteng, South Africa
Sunday O. Okeke; Langalibalele H. Mabuza
Department of Family Medicine & Primary Health Care, Sefako Makgatho Health Sciences University, South Africa
ABSTRACT
BACKGROUND: For optimum delivery of service, an establishment needs to ensure a safe and secure environment. In 2011, the South African government promulgated the National Core Standards for Health Establishments for safety and security for all employees in all establishments. Little is known about whether these standards are being complied to.
AIM AND SETTING: To assess the perceptions of health care professionals (HCPs) on safety and security at Odi District Hospital.
METHODOLOGY: A sample of 181 out of a total of 341 HCPs was drawn through a systematic sampling method from each HCP category. Data were collected through a self-administered questionnaire. The SPSS® statistical software version 22 was used for data analysis. The level of statistical significance was set at < 0.05.
RESULTS: There were more female respondents than male respondents (136; 75.10%). The dominant age group was 28-47 years (114; 57.46%). Perceptions on security personnel, their efficiency and the security system were significantly affirmed (p = 0.0001). The hospital infrastructure, surroundings and plan in emergencies were perceived to be safe (p < 0.0001). The hospital lighting system was perceived as inadequate (p = 0.0041). Only 36 (20.2%) HCPs perceived that hospital authorities were concerned about employees' safety (p < 0.0001).
CONCLUSION: HCPs had positive perceptions regarding the hospital's security system. Except for the negative perceptions of the lighting system and the perceived lack of hospital authorities' concern for staff safety, perceptions of the HCPs on the hospital working environment were positive. The hospital authorities need to establish the basis of negative perceptions and enforce remedial measures to redress them.
Background
Health care institutions are meant to provide a safe and secure environment for all users of the facilities.1 Yet threats to the safety and security of patients and hospital staff continue to affect the physician's oath to 'do no harm',2 in the sense that patient care may be compromised where health care professionals (HCPs) become hesitant to offer help for fear of endangering their own lives.
In British Columbia (BC), the health care sector accounted for more injuries and time loss than any other sector until 2003. However, according to the Workers Compensation Board (WCB) of BC, the injury rate in the BC health care sector has declined dramatically since 1998.3 The WCB examined how this was accomplished and linked it to the manner in which occupational health and safety measures were introduced through implementation of safety protocols in the interests of patient safety4; Kjellén defined 'safety' as protection against hazards, whereas security is protection against threats.5 The New Oxford Dictionary of English6 describes safety and security in the following ways: 'safety' is a condition of being protected from risk or injury, denoting something designed to prevent injury or damage, for example, safety barriers. 'Security' is a state of being free from danger or threat, for example, procedures followed or measures taken to ensure that state of feeling stable and free from fear or anxiety.7
From the above narrative, it becomes clear that the difference between security and safety is not remarkably sharp. Both are conditions where one is well protected and without risks. However, the condition of safety is about being protected, while the condition of security is about being free from danger.7
Therefore, according to the aforesaid explanations, it can be said that 'security' entails the systems, personnel and processes employed to impart the feeling of 'being secure' in an establishment, whereas 'safety' refers mainly to the physical infrastructure, surroundings, installations, plans and protocols put in place to eliminate threats or dangers, for example, 'being put in a place of safety'. Nevertheless, it must also be noted that safety cannot exist without security, and vice versa.
The South African Medical Research Council (MRC) reported that crime and violence impacted on health care service delivery in the Western Cape where it was found that 60% of the HCPs had to deal frequently with workplace crime and violence, with 92.3% reporting verbal abuse and 36.4% threats of assault.8
In 2001, a hospital ethics audit was conducted at Chris Hani Baragwanath Hospital (CHBH) one of the objectives of which was to assess its general working environment and the possible effects that the environment might have on personal and interpersonal behaviour of the employees. It found that workplace violence was rife; two-thirds of the staff affirmed that the number of security staff was inadequate and 76% felt that the security personnel were poorly equipped to do their job. A total of 57% believed that the screening of visitors was deficient and that, in general, there was a huge lack of confidence in the capacity and ability of security staff to ensure a safe environment.9
The South African situation discussed above has indicated that the country is faced with a high violence rate from which health care institutions are not exempt. However, the perceptions of the HCPs who are frequently at the receiving end of violence threatening their security and safety is unknown in their places of work. There is a scarcity of literature information relating to perceptions of HCPs about safety and security in health care institutions within South Africa and beyond. Studies on some aspects of safety and security have been conducted abroad.3,10,11,12,13 Notably, most of these studies assessed the safety and security in health care institutions indirectly, for example, assessing workplace violence against health workers.14,15,16,17 This study is conducted with the hope of gaining deep insight into the perception of HCPs regarding their security and safety in a typical district hospital in South Africa.
Research methods and design
Study setting
The study was conducted among HCPs at Odi District Hospital, Gauteng Province.
Study design
This was a descriptive cross-sectional study
Study population
All the 341 HCPs working at Odi District Hospital at the time of the study constituted the study population. They included 23 full-time and 9 part-time doctors, 7 family medicine registrars, 266 nurses, 12 pharmacists, 12 radiographers, 2 physiotherapists, 2 social workers, 2 clinical associates, 2 dieticians, 1 speech therapist, 1 occupational therapist and 2 clinical psychologists.
Sampling procedure
At the confidence level of 95%, confidence interval of 5% and a target population of 341, the sample size worked out to be 181. To obtain a representative sample from each category of HCPs, a pro rata number for the particular category was used. Therefore, each category group was represented by 181/341 (0.53) used to systematically select the individual respondents. However, where a category was represented by only one individual that individual was included in the sample. In summary, the sample included 12 full-time doctors, 5 part-time doctors, 4 family medicine registrars, 141 nurses, 6 pharmacists, 6 radiographers, 1 physiotherapist, 1 social worker, 1 clinical associate, 1 dietician, 1 speech therapist, 1 occupational therapist and 1 clinical psychologist - a total of 181 health care professionals (Table 3).
Data collection
Section 7.3 of the National Core Standards for Health Establishments in South Africa deals with the safety and security of establishments. Subsection 7.3.1 states that 'People and property should be actively protected to minimise safety and security risks'.18 Seven criteria are stipulated for the achievement of this ideal, namely:
-
Security systems to safeguard the building, patients, visitors and staff.
-
The layout and security systems for the protection of vulnerable patients.
-
Internal and external lighting to be adequate to protect patients, visitors and staff.
-
All security incidents to be reported and addressed accordingly.
-
Awareness of safety and security issues to be promoted to the staff.
-
There should be an up-to-date documented certification from the local fire authority which verifies that the health establishment complies with relevant fire safety regulations.
-
An emergency plan is to be made available indicating that patient well-being is at all times protected.
In keeping with Section 7.3 of the National Core Standards for Health Establishments in South Africa, the above-mentioned definitions and explanations, assessment of HCPs' perceptions on security and safety can be categorised according to the following parameters:6,7
-
Parameters on security:
■ presence of security personnel
■ security personnel efficiency
■ the security system (including incident reporting and processing of reported incidents).
-
Parameters on safety:
■ hospital infrastructure and surroundings
■ safety from fire
■ the hospital lighting system
■ the emergency evacuation plan (and staff confidence to follow it)
■ safety from possible harm from patients and their visitors
■ the protocol on violence prevention in the hospital
■ the hospital authorities' concern for employees' safety.
A pilot study was conducted at another district hospital (Jubilee Hospital in Hammanskraal) where 15 HCPs completed the questionnaire. This was done to refine the questionnaire and eliminate possible ambiguities in the questions. The self-administered questionnaire was created de novo by the research team, with the assistance of a statistician, and was distributed by the researcher and two trained research assistants to a consenting respondent. All completed questionnaires were collected for analysis. As respondents of each category were determined by the pro rata percentage, randomisation in each category was achieved by systematic sampling whereby respondents were selected from a sample of numbers allocated to each HCP in that category - as described in the sampling procedure above.
Data analysis
Descriptive data were presented as frequencies, tables and bar diagrams where applicable. Analysis was done using SPSS® statistical software version 22. Univariate analyses of the baseline characteristics and bivariate statistical analyses of dependent and independent variables for associations using the chi-square test, where applicable, were done. The statistical level of significance was set at < 0.05.
Ethical considerations
Ethical clearance for the study was obtained from Medunsa Research Ethics Committee (MREC) of the University of Limpopo, now Sefako Makgatho Health Sciences University (SMU). The clearance certificate number is MREC/M/19/2014:PG. The senior clinical manager of Odi District Hospital, Gauteng Province, gave permission for the study to be conducted at that hospital. Written informed consent was obtained from all the respondents using the University of Limpopo (Medunsa campus) consent forms before participation. Respondents were informed of their right to withdraw from the study at any stage. Confidentiality and anonymity of the respondents were maintained during and after the study. Data were analysed as group data and no personal identifiers were reflected in the data collection forms.
Results
Baseline characteristics
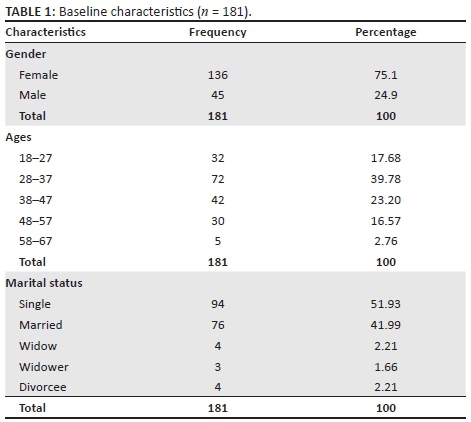
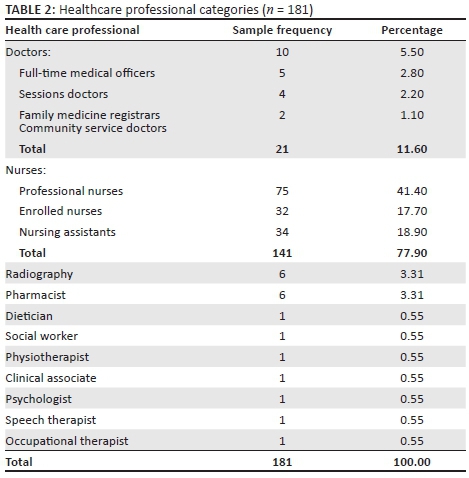
Table 1 shows the participants' baseline characteristics. Of the 181 participants, there were more females (136; 75.1%) than males (45; 24.9%). Most of the participants (63%) were aged between 28 and 47 years. Approximately 3% were above 58 years. The majority were single (94; 51.90%). Table 2 outlines the HCPs' professional categories. The majority were nurses (141; 77.9%) followed by doctors (21; 11.6%).
Perceptions on security
Table 3 shows that perceptions on security conferred by security personnel presence, efficiency of security personnel and efficiency of the security system were significantly affirmed (p = 0.0001). However, there was no difference between those affirming versus those dissenting regarding the incident reporting system to the relevant hospital authorities and the efficiency of the authorities (in dealing with reported security incident): p = 0.2086 and p = 0.2740 respectively.
Perceptions on security - Further analysis
Perceptions on efficiency of security personnel
The analysis was expanded to investigate possible differences in the main HCPs categories (doctors and nurses) and gender differences.
Table 3 has shown that the perceptions of all HCPs on the efficiency of hospital security personnel yielded a statistically significant difference between those who agreed and those who disagreed (p < 0.0001). However, when the perceptions of the main categories of HCPs (doctor and nurse) on the efficiency of hospital security personnel were compared, there was no significant difference among those who affirmed and those who did not, between the two groups (p > 0.05). However, more doctors (6; 28.6%) than nurses (14; 10.1%) indicated that they did not know about the efficiency of the hospital security system (p = 0.0174). Comparison of the perceptions of HCPs on the efficiency of the hospital security personnel by gender did not yield a statistically significant difference (p > 0.1000) in all the options (Box 1).
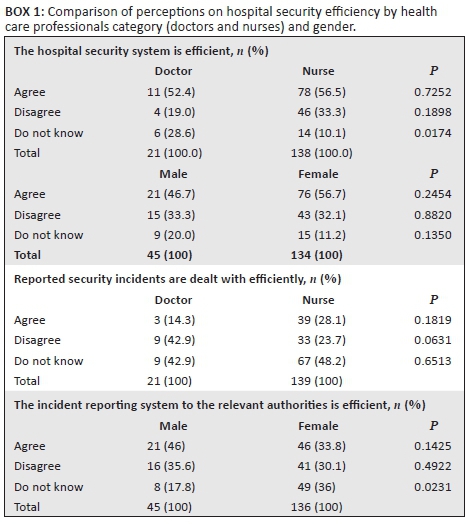
There was no significant difference between the perceptions of doctors and nurses regarding the efficiency in which reported security incidents were attended to (p > 0.05; Box 1). Although there was also no significant difference in the perceptions of male and female HCPs on the efficiency of the incident reporting system to the relevant authorities, there were significantly more female HCPs who indicated that they did not know about this efficiency (p = 0.0231; Box 1).
Perceptions on safety
Table 4 shows that the hospital infrastructure, surroundings, safety from fire hazards, emergency evacuation plan and confidence to follow the latter were perceived as safe (p < 0.0001). The hospital lighting system was perceived as inadequate (p = 0.0041). Almost an equal proportion of HCPs had affirmative and dissenting perceptions on their safety from possible harm from patients (81; 45.5% vs. 89; 50.0%; p = 0.4614) and their visitors (78; 43.8% vs. 85; 47.8%; p = 0.4708). It is noteworthy that 59.0% of HCPs were not aware of the protocol on violence prevention in the hospital and that among those who were aware of it there was a significant difference between those with a negative perception (49; 28.3%) versus those with a positive perception (22; 12.7%), p = 0.0008. Only 36 (20.2%) HCPs had the perception that the hospital authorities cared about their safety, which was significantly different from those who had the opposite perception (p < 0.0001).
Perceptions on safety - Further analysis
As was done with respect to security matters, further analysis was also conducted on safety matters to investigate possible differences in the main HCPs categories (doctors and nurses) as well as gender differences.
There was a statistically significant difference on perceptions between the proportions of male and female HCPs who disagreed that they were safe from patients as well as the patients' visitors, with proportionately more males disagreeing in each case (Box 2).
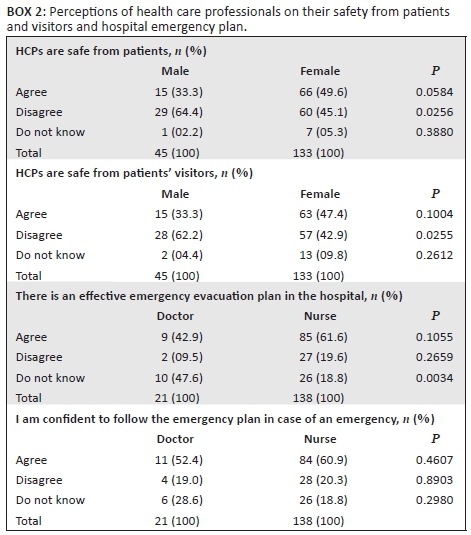
Regarding the perception on procedures to be followed in an emergency situation, there were significantly more doctors than nurses who did not know about the emergency evacuation plan (p = 0.0034; Box 2). Evaluation of confidence to follow the emergency plan in case of an emergency yielded no difference between doctors and nurses (p > 0.05; Box 2).
Discussion
This study describes the perceptions of HCPs on security in the district hospital, focussing on security personnel and their efficiency. It also assessed the HCPs' perceptions on their safety with respect to the hospital infrastructure and surroundings, including available measures in case of emergencies, as well as perceptions on the hospital authorities' care about the safety of the hospital staff in general. The majority of respondents were nurses (77.9%), a figure consistent with most articles related to perceptions of HCPs and HCWs.3,12,18 This is as a result of the dominant number of the nursing fraternity personnel in health care institutions - globally.19
Perceptions on security
On the statement on whether the presence of security personnel made HCPs feel secure, this study showed that more than half of the respondents (101; 58%) affirmed that they felt secure, which is consistent with the study by Shaw in Cincinnati Children's Hospital Medical Centre in the United States, where over half (101, 55.5%) of the respondents indicated that they experienced a sense of security when there were more hospital security personnel on duty.17 Slightly more than half of the respondents (54.2%) had a positive perception on the efficiency of the security personnel at the hospital. They indicated that the efficiency of the security personnel made them feel secure.17 This response could translate into the HCPs themselves rendering an efficient service in an environment where they feel secure.20 The hospital management should therefore maintain the security personnel presence and their operations in the hospital premises as these seem to engender the necessary perception of security among the HCPs.
There was no significant difference in the perceptions of doctors (52.4%) and nurses (56.5%) on the efficiency of the security system. Regarding the nurse proportion, our findings were similar to those by Rodriguez et al.,12 where about 54% of the nurses had trust in the efficacy of the security systems in comparison with other professionals in a Level III Hospital in Bogota, Colombia. The sex of the respondents did not influence their perceptions on the efficiency of the security personnel as the males (46.7%) and females (56.7%) affirmed this efficiency. These findings could not be compared with other studies because of paucity of research work on this topic. This means that nurses and doctors regardless of their sex had similar perceptions on the efficiency of the security personnel.
Almost one-third (31.5%) of the respondents indicated that they did not know about the security reporting system of the hospital. According to the study by Abdullah et al.,10 safety reporting was perceived as the most important element in employees' occupational health safety practices. In combating workplace violence, Gillespie et al.,21 also emphasised the importance of a universal violence incident reporting system in a given institution. Therefore, this could be an indication of neglect by the hospital authorities to raise awareness among the staff on the reporting system for safety and security in the hospital.
The finding that close to about one-in-two (47.8%) HCPs indicated that they did not know whether security incidents in the hospital were dealt with efficiently, and that only about one-quarter (23.9%) held the perception that reported incidents were dealt with efficiently, that is, to their logical conclusion raises a red flag for the hospital management. Literature has shown that poor perception on how reported incidents of unsafety are dealt with leads to reluctance from staff to even initiate the process of incident reporting.14 The hospital authorities need to improve on this aspect by involving the HCPs' leaders to ensure that proper feedback is given to the HCPs.
Perceptions on safety
The majority of the respondents (63.0%) agreed with the statement that the hospital infrastructure and surroundings were a safe place to work in and that the environment was safe from fire (55.4%). None of these items could be compared with other studies because of scarcity of research in this field. One study conducted by Rodriguez et al.12 showed different results in that, among the nursing and administrative personnel, only 2.71% and 2.77%, respectively, trusted the safety of the hospital surroundings. Just above the average number of respondents (51.4%) indicated that the hospital lighting system was inadequate to ensure safety. Safety conferred by the lighting system in an establishment has been demonstrated by the study by Steinman which showed over 50% of respondents affirming that providing adequate lighting of a hospital had increased the feeling of safety among the staff members.9 The authorities should attend to the lighting system of the hospital to enhance infrastructural feelings of safety and security.
Less than half of the respondents indicated some concern about their safety from the patients utilising the hospital (45.5%) or from the hospital visitors, including the relatives (43.8%). However, neither result showed a statistically significant difference between those affirming and negating the statement. The study by Shaw demonstrated fewer respondents (26.8%) who were concerned or fearful of patients that could turn violent, with about the same number (26.8%) concerned about visitors who could turn violent.17 This implies that in the majority of cases, patients and their visitor were not perceived as posing a safety threat to the HCPs.
More than half of the HCPs did not know that there was a written workplace violence prevention protocol in the hospital (59.0%). This might indicate the need to raise awareness among the HPCs about the existence of a written workplace violence prevention protocol in the hospital. The Centres for Diseases Control and Prevention (CDC) advocated for the availability of administrative responsibility on occupational safety in institutions, with a safety committee and education programmes, protocols, training, immunisation and prevention of health-related hazards.22 Most of the respondents (55.9%) indicated that they knew about the procedure to be followed in the case of emergency evacuation in the hospital, and almost the same percentage of respondents (57.0%) affirmed the existence of the emergency evacuation plan. Gillespie et al.21 have shown that individual knowledge and skills in universal precautions is important in the prevention and reduction of health care workplace violence. The hospital authorities should take note and follow up the finding that significantly more nurses than doctors had a negative perception about the effectiveness of the emergency evacuation plan in the hospital.
More than half of the HCPs (51.1%) were of the perception that the hospital authorities were not concerned about their emotional health and physical well-being. According to Erickson, when management blames the employee for injuries and accidents, occupational health safety performance decreases.23 For that reason, organisational culture on safety and security is vital in determining the level at which employers and employees pitch the implementation of the best practice on health safety. One in two of the HCPs had the perception that the hospital authorities cared about their safety (51.1%). This could be an indictment which needs to be corrected by the hospital management because it has been shown that in institutions with a strong safety climate, workers suffer fewer accidents - not only because of the implementation of the safety programmes, but also because the very existence of these programmes indicates to employees the commitment of the authorities about the former's safety.24,25 Efforts to curb workplace violence include policy, process and environmental changes and these should be routinely communicated to staff so that workers are always kept informed and develop the sense that they are valued by the employer.17
Strengths and limitations
To our knowledge, this study is the first to investigate the perceptions of HCPs on their safety and security according to the National Core Standards for Health Establishments in South Africa. Although the study was a cross-sectional study in design which could not establish causal relationships, its findings could be used to generate hypotheses which, in turn could be tested through larger sample studies involving a number of settings. The measuring tool used in this study was created de novo by the research team with the assistance of a statistician. The pilot study that was conducted helped to reduce possible ambiguities of the questions. Self-reports and perceptions do not necessarily reflect the true state of affairs in an institution and may be prone to information bias. However, this assessment offers a premise upon which implementation of policies can be based when working towards the realisation of the national core standards in a health care establishment. This study employed a quantitative method and could not provide in-depth understanding of the HCPs' views. In addition, the study was conducted in only one of the district hospitals in Gauteng and may not be a true representation of the perceptions of the entire health care workforce in all the district hospitals in the Gauteng province of South Africa. Future studies from more representative sites and employing qualitative methods are needed to fully investigate this topic.
Conclusion
This study shows that perceptions of HCPs on security conferred by security personnel presence, efficiency of security personnel and efficiency of the security system were significantly affirmed. HCPs perceptions were positive but varied on issues of security personnel, security infrastructure, safety around patients, reporting system, emergency and evacuation plans. Negative perceptions regarding lighting in the hospital premises and management's lack of concern for HCPs safety underscore the need for interventions to address these negative perceptions.
Acknowledgements
The researchers are grateful for the contributions of Prof. H.S. Schoeman towards the study data analyses. This study was conducted in partial fulfilment of the requirements for the awarding of the Master of Medicine (Family Medicine) degree for the first author at the University of Limpopo, Medunsa Campus, Pretoria, South Africa (now known as Sefako Makgatho Health Sciences University [SMU]).
Competing interests
The authors declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
Authors' contributions
S.O.O. conceptualised the research idea. L.H.M. supervised the Master of Medicine (Family Medicine) registrar. L.H.M. drafted the manuscript. S.O.O. reviewed the draft manuscript. Both authors approved the final manuscript.
References
1.State of Victoria. 2016. Security and safety at hospital - Better health channel [homepage on the Internet]. [cited 2016 Aug 1]. Available from: https://www.betterhealth.vic.gov.au/health/…/security-and-safety-at-hospital?viewAs [ Links ]
2. Sullivan M, Robertson G, Nibbelink S, Stieva G, Roberts C, Neave G. How an intelligent infrastructure can help optimize hospital safety and security [homepage on the Internet]. July 2011 / White paper. [cited 2017 Feb 14] Available from: http://docplayer.net/11496629-How-an-intelligent-infrastructure-can-help-optimize-hospital-safety-and-security.html [ Links ]
3. OHSAH, 2004. Trends in workplace injuries, illnesses, and policies in healthcare across Canada, March 31, 2004 Report [homepage on the Internet]. [cited 2017 Feb 14]. Available from: http://www.phsa.ca/Documents/Occupational-Health-Safety/ReportTrendsinWorkplaceInjuriesIllnessandPolicies.pdf [ Links ]
4. Yassi A, Hancock T. Patient safety - worker safety: Building a culture of safety to improve healthcare worker and patient well-being. Healthc Q. 2005;8:32-38. https://doi.org/10.12927/hcq..17659 [ Links ]
5. Kjellen U. Prevention of accidents through experience feedback. 6th ed. London: Taylor and Francis; 2000. [ Links ]
6. Pearsall J, Hanks P, editors. The new Oxford dictionary of English. UK: Oxford University Press; 2001. [ Links ]
7. Albrechtsen E. A generic comparison of industrial safety and information security. Term paper in the PhD course 'Risk and vulnerability', 2002 [homepage on the Internet]. [cited 2017 Jan 25]. Available from: www.iot.ntnu.no/~albrecht [ Links ]
8. Medical Research Council. The impact of crime and violence on the delivery of State Health Care Services in the Western Cape. Presented by Sandra Marais, 2001 Oct 18; Unisa Institute, Lenasia. [ Links ]
9. Steinman S. Work place violence in the health sector. Geneva: World Health Organization; 2002. [ Links ]
10. Abdullah NAC, Spicket JT, Rumchev KB, Dhaliwal SS. Assessing employees perception on health and safety management in public hospital. IJBR 2009;5(4):54-72. [ Links ]
11. Etukumana EA, Orie JB. Health workers' perception on the safety and security policy of a tertiary hospital in Nigeria. Ibom Med J. 2014;7(1):8-12. [ Links ]
12. Rodriguez MH, Rodriguez MEH, Lozano EMM, Rodriguez CDH. Perception of workers about the workplace health and safety system in a level III Hospital, Bogota-Colombia. GJRA 2015;4(10):89-92. [ Links ]
13. Senthil1 A, Anandh B, Jayachandran P, et al. Perception and prevalence of work-related health hazards among health care workers in public health facilities in southern India. Int J Occup Med Environ Health. 2015;21(1):74-81. https://doi.org/10.1179/2049396714Y.0000000096 [ Links ]
14. Carmi-Iluz T, Peleg R, Freud T, Shvartzman P. Verbal and physical violence towards hospital and community-based physicians in the Negev: An observational study. BMC Health Serv Res. 2005;5(1):54. https://doi.org/10.1186/1472-6963-5-54 [ Links ]
15. Franz S, Zeh A, Schablon A, Kuhnert S, Nienhaus A. Aggression and violence against health care workers in Germany - a cross sectional retrospective survey. BMC Health Serv Res. 2010;10:51. http://www.biomedcentral.com/1472-6963/10/51 [ Links ]
16. Ogbonnaya GU, Ukegbu AU, Aguwa EN, Emma-Ukaegbu U. A study on workplace violence against health workers in a Nigerian tertiary hospital. Niger J Med. 2012;21(2):174-179. [ Links ]
17. Shaw J. Staff perceptions of workplace violence in a pediatric emergency department. Work. 2015;51(1);39-49. https://doi.org/10.3233/WOR-141895 [ Links ]
18. National Department of Health. National core standards for health establishments in South Africa, Republic of South Africa, 2011: Published Tshwane, South Africa [homepage on the Internet]. [cited 2016 Dec 27]. Available from: http://national-department-health-national-core-standards-health-establishments-south-africa-0 [ Links ]
19. Zurn P, Dal Poz MR, Stilwell B, Adams O. Imbalance in the health workforce. Human Hum Resour Health. 2004;2:13. https://doi.org/10.1186/1478-4491-2-13 [ Links ]
20. Houle J. Health and safety survey. American Nurses Association, Nursing World. 2001;32(1): 1-32. [cited 2017 February 13]. Available from: http://www.nursingworld.org/DocumentVault/HealthSafetySurvey-2011.pdf [ Links ]
21. Gillespie GL, Gates DM, Miller M, Howard PK. Workplace violence in healthcare settings. Rehabil Nurs. 2015;35(5):177-184. https://doi.org/10.1002/j.2048-7940.2010.tb00045.x [ Links ]
22. Siegel JD, Rhinehart, E, Jackson, M, Chiarello L. The healthcare infection control practices advisory committee. 2007 Guideline for isolation precautions: Preventing transmission of infectious agents in healthcare settings infection control, Atlanta: Center for Disease Control and Prevention. [cited 2017 Feb 14]. Available from: https://www.cdc.gov/hicpac/pdf/isolation/isolation2007.pdf [ Links ]
23. Erickson JA. Corporate culture: The key to safety performance. Occup Hazards. 2000;62(4):45-50. [cited 2017 February 14] Available from: http://connection.ebscohost.com/c/articles/2993772/corporate-culture-key-safety-performance [ Links ]
24. Gershon RR, Stone PW, Zeltser M, Faucett J, MacDavitt K, Chou SS. Organizational climate and nurse health outcome in United State: A systematic review. Ind Health. 2007;45(5):622-636. https://doi.org/10.2486/indhealth.45.622 [ Links ]
25. Ribeiro PHV, Brevidelli MM, Tipple AFV, Ribeiro RP, Gir E. Organizational safety climate and adherence to standard precautions among dentists. Acta Paul Enferm. 2013;26(2):192-197. https://doi.org/10.1590/S0103-21002013000200014 [ Links ]
 Correspondence:
Correspondence:
Langalibalele Mabuza
honeymanyosi@gmail.com
Received: 18 Feb. 2017
Accepted: 10 Sept. 2017
Published: 27 Oct. 2017














