Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.17 n.4 Pretoria Dec. 2023
http://dx.doi.org/10.7196/SAJCH.2023.v17i4.2004
ARTICLE
Variations in intravenous fluid management for paediatric hypernatraemia in South Africa: A survey of junior and senior South African paediatric doctors
M MilovanovicI; S OmarII; S G LalaIII, IV, *; Z DangorIII, IV, *
IMA Psych; Perinatal HIV Research Unit, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IICert Critical Care; Department of Critical Care, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIPhD; Paediatric Education and Research Ladder, Department of Paediatrics, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVPhD; Department of Paediatrics and Child Health, Chris Hani Baragwanath Academic Hospital, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Paediatric hypernatraemia is a severe and life-threatening electrolyte abnormality that is associated with considerable morbidity and mortality. Although intravenous (IV) fluid therapy is a crucial component of management, there are no management guidelines, and varying approaches to IV fluid therapy are commonplace in clinical practice.
OBJECTIVES: To determine the variance in IV fluid therapy in the management of paediatric hypernatraemia among paediatric registrars and consultants in South Africa.
METHODS: A self-administered online survey was conducted from November 2020 to February 2021. The survey assessed paediatricians' management of three typical clinical scenarios of community-acquired hypernatraemia seen in South Africa. Descriptive results were presented as proportions, frequencies and medians with interquartile ranges. Comparisons were done using contingency tables.
RESULTS: Responses from 119 participants were analysed. Most respondents worked in the state sector (69.8%), and were based mainly in Gauteng (46.2%) or Western Cape (25.2%) province. Most (60.2%) respondents considered a serum sodium level >146 mmol/L indicative of hypernatraemia, and 43.6% (n=51/117) reported seeing >10 cases of paediatric hypernatraemia in 2019. For all three cases, at least eight different types of infusate (of varying sodium concentrations) were chosen as maintenance fluids. Fluid deficits were calculated using either the free water method or based on the perceived degree/percentage of clinical dehydration.
CONCLUSION: There is considerable variability in the management of hypernatraemia among paediatricians in South Africa. There is an urgent need to develop a standardised guideline for the treatment of paediatric hypernatraemia.
Paediatric hypernatraemia is a severe and life-threatening electrolyte abnormality that occurs as a consequence of inadequate fluid intake,[1] the loss of hypotonic water from diarrhoeal disease, or rarely from excessive sodium intake.[2-4] Hypernatraemia occurs in ~10 - 20% of children with dehydrating diarrhoeal disease.[5,6] Furthermore, hypernatraemia is associated with high mortality (12 - 19%) and adverse neurodevelopmental outcomes.[4,7] In South Africa, the prevalence of hypernatraemic dehydration among hospitalised children with diarrhoeal disease varies from 12.3 - 41%.[8-10] In a recent South African study, the prevalence of hypernatraemia among all hospitalised children was 5.3%, with mortality rates of 28.0% in children with serum sodium levels >180 mmol/L.[11]
Appropriate intravenous fluid administration is a crucial component of therapy that reduces morbidity and mortality from hypernatraemia.[1] The selection of an appropriate intravenous fluid solution (infusate), the total volume of infusate administered, the rate of infusate administration, as well as the administration of intravenous fluid boluses are important therapeutic choices that a paediatrician must make to optimise treatment of hypernatraemia;[12] inappropriate infusate prescriptions (selection, rates and volume of administration) are associated with increased mortality and morbidity rates.[13,14] However, there is a dearth of high-quality studies about fluid and electrolyte management in children with hypernatraemia, and to date there are no national or international consensus management guidelines. Despite this limitation, the overarching principle of management is the gradual reduction of serum sodium levels in children with hypernatraemia. Our anecdotal experience suggests that South African doctors struggle with choosing an appropriate intravenous solution, as well as the rate and total volume of the infusate fluid, especially in severely ill children. We therefore conducted an online survey of South African paediatric registrars and consultants in state and private practice to determine the extent of variance in the management of paediatric hypernatraemia. This information is needed to develop a clinical practice guideline for paediatric hypernatraemia, which is a common and serious condition in South African children.
Methods
From November 2020 to February 2021, we conducted a self-administered online survey (in English) with paediatric consultants and registrars across South Africa regarding the management of hypernatraemia in children. There are approximately 1 400 registered paediatric clinicians (1 000 consultants and 400 registrars) in South Africa.[15] Paediatricians in private practice, and paediatrics registrars and consultants working in state hospitals, were invited to participate in the survey through an email invitation sent to the following networks: (i) the Paediatric Management Group, (ii) the South African Paediatric Association, and (iii) the academic Heads of Department of Paediatrics at all South African medical schools. Those receiving the communication were also encouraged to share the study details with others they deemed eligible for participation. Monthly follow-up communications were sent to the paediatric networks to encourage participation. Medical officers and interns were not eligible for inclusion in the study.
The survey, which took approximately 15 minutes to complete, was constructed as single-answer multiple choice questions with an option to provide additional or other information where necessary (full survey available as supplementary material, https://www.samedical.org/file/2091). The demographic section collected information on current position, province where currently working, years of experience, and medical school where postgraduate training was undertaken. We also collected data determining the approximate number of cases of hypernatraemia that the clinician managed in the previous year. In the survey, we developed three hypothetical clinical scenarios (Box 1) that mimic typical presentations of community-acquired (and not hospital-acquired) hypernatraemia in South African children. Case 1 represents a septic neonate who was severely dehydrated with a sodium concentration of 155 mmol/L; Case 2 represents a severely ill hypotensive six-week-old infant with a sodium concentration of 180 mmol/L; and Case 3 represents a moderately dehydrated six-month-old infant who tolerated oral feeds and had a sodium concentration of 165 mmol/L. A series of questions, regarding the intravenous fluid management of hypernatraemic children, then followed each clinical scenario.
Statistical analysis
All data were abstracted from the online platform into MS Excel, and analysed using Excel and Stata, version 13. Descriptive results were presented as proportions, frequencies and medians with interquartile ranges. Comparisons were done using contingency tables (either chi-square or Fisher's exact test); a p-value <0.05 was considered significant. Paediatric consultants were categorised into two groups: those with <10 years' experience compared with those with >10 years' experience. Fluids were classified as either hypotonic (sodium content <77 mmol/L) or isotonic (sodium content >77 mmol/L). We also categorised responses based on where most participants were registered or completed their postgraduate training, namely: University of the Witwatersrand (Wits), University of Cape Town (UCT), University of Pretoria (UP) and University of the Free State (UFS).
Ethics approval
Prior to starting the survey, interested members were requested to read through the detailed information page. By agreeing to 'continue', interested members were, by proxy, consenting to participate in the online survey and provided permission for their responses to be used for research purposes. This study was approved by the University of the Witwatersrand Human Research Ethics Committee (Medical) (ref no. M200923).
Results
A total of 121 survey responses were collected, from which two were removed from the final analysis owing to missing information. Of the total number analysed (N=119), 85 (71.4%) were consultants, with a median of 9 (interquartile range (IQR) 3 - 16) years of work experience. The majority of respondents worked in the public sector (n=83/119, 69.8%), with most based in either Gauteng (n=55/119, 46.2%) or Western Cape (n=30/119, 25.2%) province. A third of respondents (n=41/119, 34.8%) completed their postgraduate paediatric training at the University of the Witwatersrand (Table 1).
Regarding hypernatraemia, 71/118 (60.2%) respondents considered a serum sodium level >146 mmol/L as indicative of hypernatraemia while 43/118 (36.4%) regarded a serum sodium level >150 mmol/L as indicative of hypernatraemia. While a majority (n=91/117, 77.8%) of respondents indicated that serum sodium was the single most important clinical or laboratory parameter guiding the management of hypernatraemia, a fifth of respondents (n=26/117, 22.2%) used another clinical or biochemical parameter. In assessing paediatricians' exposure to children with hypernatraemia, 43.6% (n=51/117) of respondents reported seeing >10 cases of paediatric hypernatraemia in 2019 (Table 1).
Interpretation and management of case scenarios
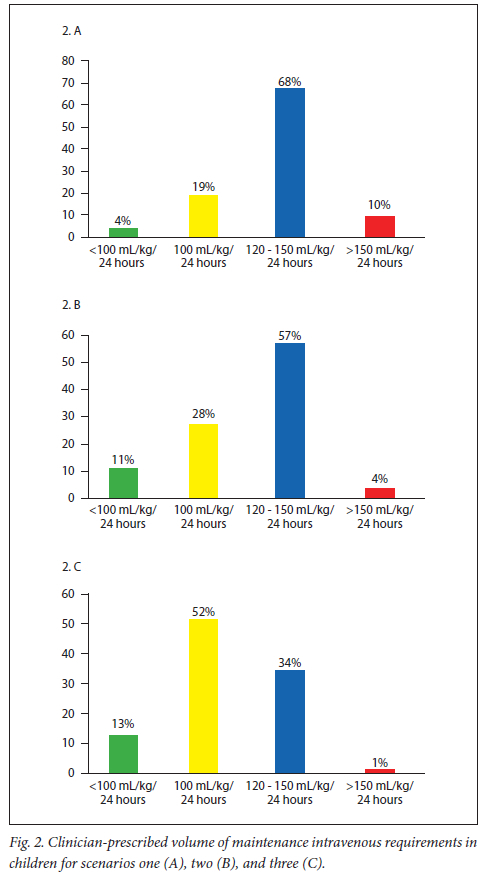
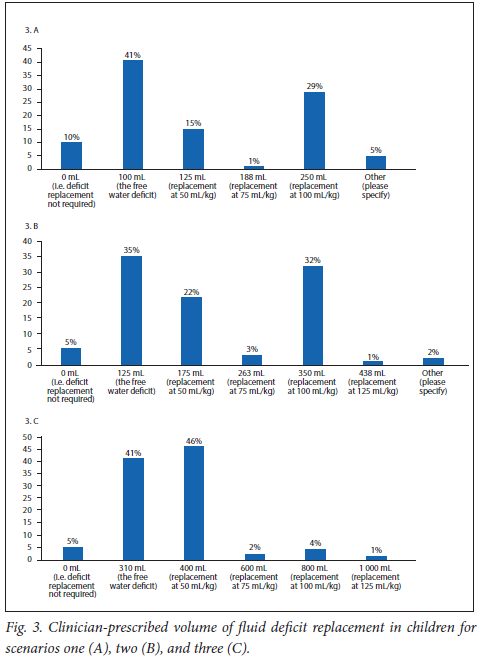
In general, for all three cases, at least eight different types of infusate, with varying sodium concentrations (nil to >154 mmol/L), were chosen as maintenance fluids (Fig. 1.A - C). This difference was significantly associated with the university at which postgraduate paediatric training occurred (Case 1, p)=0.011; Case 2, p=0.026; Case 3, p=0.018; Supplementary Tables 1 - 3, https://www.samedical.org/file/2090). There was no significant difference in prescribing practice between paediatricians working in the private or state sector, or between paediatric registrars and paediatricians (data not shown). Senior paediatricians (>10 years in practice) prescribed half-strength Darrow's dextrose solution more frequently than did their junior counterparts. Regarding the total volume of infusate fluid used to correct fluid deficit, some paediatricians calculated the deficit by estimating the amount of free water needed to correct the sodium whereas other paediatricians calculated the deficit based on the perceived degree/percentage of clinical dehydration (Fig. 2.A - C and Supplementary Tables 1 - 3, https://www.samedical.org/file/2090).
Case 1 specific findings
The most common type of prescribed infusate for maintenance requirements was Neonatalyte (27.6%), half-normal saline with 5% dextrose (19.1%) and half-strength Darrow's dextrose solution (16.2%) (Fig. 1.A). Clinicians trained at UCT were less likely to prescribe Neonatalyte as compared with Wits, UP or UFS. About 15% of paediatricians prescribed a modified infusate adding either sodium bicarbonate or hypertonic sodium chloride (Supplementary Table 1, https://www.samedical.org/file/2090). Where specified, 78.8% (n=67/85) of responders prescribed hypotonic fluids for maintenance.
Regarding the volume of infusate prescribed as maintenance requirements, 80.9% of responders (Fig. 2.A) did not prescribe maintenance intravenous fluids using the well-described Holliday-Segar formula.[16]
Case 2 specific findings
Normal (0.9%) saline (48.5%) and Ringer's lactate (29.9%) were the most common infusates used for fluid boluses (Supplementary Table 2). The majority of clinicians who trained at UCT and UFS used Ringer's lactate as the bolus fluid. As compared with Case 1, a larger proportion of clinicians (22.5%) prescribed a modified infúsate (adding either sodium bicarbonate or hypertonic sodium; Supplementary Table 2, https://www.samedical.org/file/2090). Where specified, 45.2% (n=33/73) of responders prescribed hypotonic fluids for maintenance.
Case 3 specific findings
For Case 3, which specifically enquired about the administration of oral fluids, 49.5% (n=47/95) of clinicians chose to rehydrate using only oral therapy, 48.4% (n=46/95) chose to rehydrate using a combination of oral and intravenous therapy, and 2.1% (n=2/95) chose to rehydrate using intravenous therapy only (Supplementary Table 3, https://www.samedical.org/file/2090). There were large variations in the type of infusate chosen for maintenance fluid; this difference was mainly associated with the postgraduate training institute.
Discussion
The present study, which sought to determine the extent of variance in the management of paediatric hypernatraemia by state and private practice clinicians highlighted a few important findings: (i) there are significant geographic differences in the choice and volume of infusate used by clinicians and this is most likely dependent on the postgraduate training institution; (ii) there is no single IV maintenance fluid that is preferred by clinicians: at least eight different types of infusate of varying sodium concentrations (nil to >154 mmol/L) and tonicity were prescribed; and (iii) 22% of responders do not use the drop in sodium concentration as the most important marker in the management of hypernatraemia. Our findings suggest that clinicians may struggle to select appropriate intravenous therapy, including the rate and volume of administered infusate fluid, in severely ill children with hypernatraemia. Importantly, inappropriate fluid therapy is associated with higher mortality in children with hypernatraemia.[1] Hence, a clinical practice guideline for paediatric hypernatraemia is urgently warranted in South Africa,[17,18] and even though this study was undertaken in South Africa, these challenges are likely to be present in other low- and middle-income countries.
Our questionnaire included case descriptions that typically mimic common clinical presentations of hypernatraemia in children, and we therefore expected registrars and consultants to be familiar with the management of these cases. This consideration allowed us to assess knowledge transfer, case management based on the severity of clinical presentation, the level of dehydration, the degree of shock, the child's ability to tolerate oral fluids (widely accepted as a safer option than using intravenous fluids), as well as the gradual reduction of serum sodium levels. Regarding the two major postgraduate teaching institutions, we found that clinicians who trained at UCT were more likely to base their fluid deficit calculations on the percentage of dehydration in the child as compared with clinicians who trained at Wits, who favoured the free water deficit calculation.
Our results indicate that South African paediatricians demonstrate little consistency in managing a serious, and not uncommonly encountered, medical condition. This is very likely to be influenced by their personal experiences and the application of general, rather than specific, fluid management principles that are taught at their training institute. This variability in judgement (referred to as 'noise' in cognitive psychology; our study is an example of a 'noise audit') almost always contributes to poorer outcomes.[19] The high level of variability in management implies that a clinical guideline must be developed for paediatricians who treat children with hypernatraemia. Even in the absence of high-quality evidence to inform practice (and it is not pragmatic to conduct such high-quality clinical trials in low- or middle-income settings in the near future), a team of experienced clinicians can use clinical reasoning to develop protocols that allow for a gradual and safe reduction in serum sodium levels.[17,18,20] Standardised treatment approaches also make it easier to identify and correct biases or errors that contribute to poor outcomes in hypernatraemia.
Our study has limitations. Owing to the impact of the COVID-19 pandemic, our survey response rate was lower than anticipated. By utilising existing networks, we hoped to access departments and hospitals across varying sectors and provinces in South Africa, which would have allowed us to explore differences and similarities in management protocols. However, our sample was not representative of the smaller universities in South Africa and featured responses from clinicians mostly from Gauteng and the Western Cape. Furthermore, our response rate for case 3 was lower than the other cases - we suspect that this was either due to the difficulty of the case or more likely survey fatigue. Although very unlikely, it is possible that participants discussed cases with each other before submitting responses.
Conclusion
In conclusion, we found high variability in the management of hypernatraemia that was mainly influenced by the institution at which postgraduate training was undertaken. By appreciating the varying strategies used by paediatric registrars and consultants in South Africa, this study highlights the need to develop a standardised guideline for the treatment of paediatric hypernatraemia.
Declaration. None.
Acknowledgements. We would like to acknowledge all the participants who took the time to answer the online survey.
Author contributions. MM, SO, SGL and ZD conceptualised the study. MM collected data. MM and ZD undertook the data analysis. MM, SGL and ZD wrote the manuscript. All authors read and approved the final manuscript.
Funding. No funding was secured for this study.
Conflict of interest. The authors have no conflict of interest to disclose. The authors have no financial relationship relevant to this article to disclose.
References
1. Moritz ML, Ayus JC. The changing pattern of hypernatremia in hospitalised children. Pediatrics 1999;104(3 Pt 1):435-439. https://doi.org/10.1542/peds.104.3.435 [ Links ]
2. Koklu E, Gunes T, Ozturk M, et al. A review of 116 cases of breastfeeding associated hypernatremia in a rural area of central Turkey. J Trop Pediatr 2007;53:347-350. [ Links ]
3. Ben-Shalom E, Toker O, Schwartz S. Hypernatremic dehydration in young children: Is there a solution? Isr Med Assoc J 2016;18:95-99. [ Links ]
4. Chisti MJ, Ahmed T, Ahmed AM, et al. Hypernatremia in children with diarrhea: Presenting features, management, outcome, and risk factors for death. Clin Pediatr (Phila) 2016;55(7):654-663. [ Links ]
5. Pettifor JM, Lala SG. Hypernatraemic dehydration - do we have consensus on its management. [Editorial] S Afr J Child Health 2018;12(1):2. [ Links ]
6. Anigilaje EA. Management of diarrhoeal dehydration in childhood: A review for clinicians in developing countries. Front Pediatr 2018;6:28. https://doi.org/10.3389/fped.2018.00028 [ Links ]
7. Shahrin L, Chisti MJ, Huq S, et al. Clinical manifestations of hyponatremia and hypernatremia in under-five diarrheal children in a diarrhea hospital. J Trop Pediatr 2016;62(3):206-212. [ Links ]
8. Hariram T, Naidoo K, Ramji S. Hypernatraemic dehydration in infants with acute gastroenteritis at King Edward VIII Hospital. S Afr J Child Health 2018;12(1):10-14. https://doi.org/10.7196/SAJCH.2018.v12i1.1424 [ Links ]
9. Cooke ML, Nel ED, Cotton MF. Pre-hospital management and risk factors in children with acute diarrhoea admitted to a short-stay ward in an urban South African hospital with a high HIV burden. S Afr J Child Health 2013;7(3):84-87. https://doi.org/10.7196/SAJCH.2013.v7i3.472 [ Links ]
10. Hoosain SBG. Hypernatraemic dehydration in acute gastroenteritis - a descriptive audit of prehospital management and predisposing factors. wiredspace.wits.ac.za/jspu/bitstream/1053 9/23167/1/Research%20 report%20final.pdf (accessed 9 April 2018). [ Links ]
11. Naka N, Solomon F, Madhi SA, et al. Borderline hypernatraemia and mortality rates in South African infants: A single-centre observational study. S Afr J Child Health 2023. Forthcoming issue 4 of 2023. https://samajournals.co.za/index.php/sajch/article/view/1449 [ Links ]
12. Maitland K, Kiguli S, Opoka RO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med 2011;364(26):2483-2495. https://doi.org/10.1056/NEJMoa1101549 [ Links ]
13. Regina GC. Hypo versus isotonic solutions in intravenous fluid maintenance of acutelly ill pediatric patients. J Anesth Intensive Care Med 2017;2(3):555589. https://doi.org/10.19080/JAICM.2017.02.555589 [ Links ]
14. Fang C, Mao J, Dai Y, et al. Fluid management of hypernatraemic dehydration to prevent cerebral oedema: A retrospective case control study of 97 children in China. J Paediatr Child Health 2010;46(6):301-303. https://doi.org/10.1111/j.1440-1754.2010.01712.x [ Links ]
15. Health Professions Council of South Africa. Annual Report 2020/2021. https://www.hpcsa.co.za/Uploads/Publications/2021/Annual%20Report/HPCSA%20FY2020-21%20Annual%20Report%20Approved%20Final.pdf [ Links ]
16. Holliday MA, Segar WE. The maintenance need for water in parenteral fluid therapy. Pediatrics 1957;19(5):823-832. [ Links ]
17. Murad MH. Clinical practice guidelines: A primer on development and dissemination. Mayo Clin Proc 2017;92(3):423-433. https://doi.org/10.1016/j.mayocp.2017.01.001 [ Links ]
18. Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: Potential benefits, limitations, and harms of clinical guidelines. BMJ 1999;318(7182):527-530. https://doi.org/10.1136/bmj.318.7182.527 [ Links ]
19. Kahneman D, Sibony O, Sunstein CR. Noise: A flaw in human judgement. 1st ed. New York: Little Brown Spark; 2021. [ Links ]
20. Graham ID, Harrison MB. Evaluation and adaptation of clinical practice guidelines. Evid Based Nurs 2005;8(3):68-72. https://doi.org/10.1136/ebn.8.3.68 [ Links ]
 Correspondence:
Correspondence:
Z Dangor
ziyaad.dangor@wits.ac.za
Accepted 3 August 2023
* Joint senior authorship














