Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.17 no.4 Pretoria dic. 2023
http://dx.doi.org/10.7196/SAJCH.2023.v17i4.2003
ARTICLE
An audit of electronic discharge summaries of neonates admitted with hypoxic ischaemic encephalopathy to tertiary hospitals in Bloemfontein in 2018 - 2019
K M AfolabiI; A van der BylII; G JoubertIII
IMB BS, MMed; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIMMed (Paeds), Cert Neonatol; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIBA, MSc; Department of Biostatistics, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: A discharge summary may be the only available health record for a patient, especially in resource-limited settings with suboptimal record-keeping. Considering the risk of adverse neurodevelopmental outcomes secondary to hypoxic ischaemic encephalopathy (HIE), as well as litigation, the quality of summaries for neonates with HIE is particularly important.
OBJECTIVES: To audit electronic discharge summaries of neonates admitted with HIE to two tertiary hospitals in Bloemfontein, South Africa.
METHODS: A retrospective, quantitative study was conducted. Electronic discharge summaries of late preterm and term neonates with HIE, admitted in 2018 and 2019, were audited for relevant information, including final diagnosis, birth history, clinical evaluation, management, investigations, plan at discharge, as well as counselling of parents.
RESULTS: Of the 165 identified cases, 34 (20.6%) were excluded. Ten patients did not have electronic discharge summaries. Admission register details were incomplete for the other 24 cases. The final diagnosis of HIE appeared in 87 of 131 (66.4%) audited summaries. More than half (52.7%) had incorrect ICD-10 coding for HIE. Information on foetal distress and sentinel events was absent in 61.1% and 42.0%. Requirement for resuscitation was recorded in 90.8% of summaries. Performance of cardiac compressions and adrenaline administration were not specified in 46.6% and 54.2%. Admission blood gas results, particularly base deficit, lactate and glucose, were absent in 42.7%, 63.4% and 90.8% of summaries. Eligibility for therapeutic hypothermia was not captured in 41.2%. Cranial ultrasound, neuroimaging, exclusion of meningitis, or multisystem involvement was not mentioned in 80.9%, 99.2%, 80.2% and 96.2%, respectively. Notes on counselling of parents were lacking (83.2%). Final cause of death was unspecified in 85.7% (n=12/14) of patients who died.
CONCLUSION: Discharge summaries of neonates at risk of adverse neurodevelopmental outcomes secondary to HIE lacked essential information. Quality improvement and regular auditing of patient records must be prioritised.
A comprehensive discharge summary is an essential part of a patient's medical record, as emphasised by the Health Professions Council of South Africa (HPCSA).[1] A high-quality summary contains particulars regarding a patient's most recent hospital admission and is beneficial as the first source of medical information.[2-4] In resource-limited settings, record-keeping and filing may be suboptimal, particularly for paper-based records. Electronic medical records may be the only accessible health record to ensure continuity of care.[5] Key elements for a high-quality summary include diagnosis, treatment received, results of investigations and need for follow-up.[2,3] Patient outcomes may be improved by discharge documentation of good quality, as suggested by a US study,[6] which reported a reduced risk for readmission in heart-failure patients for whom follow-up plans were well documented. A Nigerian study[7] identified the lack of will of clinicians to prepare comprehensive discharge summaries despite having the ability to do so. A similar study exploring a quality improvement initiative found that poor-quality discharge summaries could be addressed by training healthcare professionals.[4] There is a paucity of research on the quality of medical records in South Africa (SA). A local study in Limpopo Province showed that poor record-keeping/filing contributed to a delay in patients being assisted in the hospital.[8] Another recent study at a tertiary hospital in Gauteng[2] (2016) found that only four out of every five paediatric patients had a completed discharge summary.
Neonatal encephalopathy (NNE) is a 'clinically defined syndrome of disturbed neurological function in the earliest days of life in an infant born at or beyond 35 weeks' gestation, manifested by a subnormal level of consciousness or seizures, and often accompanied by difficulty with initiating and maintaining respiration and depression of tone and reflexes.[9] Asphyxia is impaired gaseous exchange leading to hypoxaemia, hypercapnia and metabolic acidosis, with reduced bicarbonate levels and increased base deficit.[10] Hypoxia is the decreased oxygenation of cells or organs. Ischaemia refers to blood flow to cells or organs that are inadequate to maintain physiological function.[11] Therefore, hypoxic ischaemic encephalopathy (HIE) in a newborn is encephalopathy owing to a hypoxic ischaemic event as defined by the American College of Obstetricians and Gynaecologists/American Academy of Paediatrics (ACOG/AAP).[9]
A discharge summary in the context of HIE is particularly important owing to the increased risk for morbidity and mortality associated with the diagnosis. Developed countries report an escalation in medical litigation cases, specifically for neonates with HIE and NNE. Most settlements are related to neurological impairment and cerebral palsy attributed to perinatal compromise and birth asphyxia.[12] In SA, medical negligence claims comprised almost a third of the health budget during 2016 and 2017. Detailed and accurate records are necessary in these high-risk cases to withstand scrutiny in a court of law should litigations arise, even years later.[13]
Ethics
Ethics approval was obtained from The Health Sciences Research Ethics Committee of the University of the Free State (UFS) (ref. no. UFS HSD2020/0047/2403). Permission to conduct the study was also obtained from the Free State Department of Health. Data were anonymised to maintain patients' and medical professionals' confidentiality.
Methods
Study design
A retrospective, quantitative study was conducted to audit electronic discharge summaries of neonates admitted with HIE to the neonatology units of Universitas Academic Hospital and Pelonomi Tertiary Hospital, Bloemfontein, over a 2-year period.
Standard of care at the study centres
At both hospitals, neonates admitted with suspected HIE could be inborn or referred from clinics or other hospitals for specialised care. On admission, patients are evaluated and classified as having mild, moderate or severe HIE. An arterial blood gas is done within the first hour according to international guidelines. Owing to limited resources and/or expertise, referring clinics or hospitals may not be able to perform a blood gas within this time frame and, therefore, it will be done on admission.
A cranial ultrasound is performed on admission and repeated on days 3 - 5 of admission.
Owing to resource constraints, magnetic resonance imaging (MRI) of the brain, which is the standard of care, is not routinely done. Patients are also screened for other conditions that could cause NNE. Parents of a neonate admitted with HIE are informed about the diagnosis, management plan and expected long-term prognosis. Trauma, infection, and coagulation disorders are routinely excluded as causes of NNE. Secondary causes, such as metabolic disorders and genetic causes, are investigated, if clinically indicated.
Therapeutic hypothermia/whole-body cooling was available at both hospitals, where local guidelines are informed by international consensus.[14,15] The inclusion criteria for therapeutic hypothermia are shown in Fig. 1 (Supplementary file: https://www.samedical.org/file/209). Exclusion criteria included: (i) inability to initiate therapeutic hypothermia by 6 hours after birth; and (ii) major congenital anomaly.[14,15]
Sample selection
Late-preterm and term neonates (>35 weeks' gestation) admitted with an HIE diagnosis from the 1 January 2018 to 31 December 2019 were identified by using admission registers, electronic statistics databases and therapeutic hypothermia registers at the two hospitals. Neonates with incomplete or missing admission records and missing discharge summaries were also noted in the study. Patients with other causes of NNE were excluded.
Data collection
The first author retrieved electronic discharge summaries from the Meditech database, a software programme which captures all relevant data of the patient from admission until discharge. Obligatory fields capture the birth parameters, mode of delivery and Apgar scores, dates of admission and discharge, and the final diagnosis by way of an ICD-10 code. Other information is typed into the system by approved users who receive unique usernames and passwords, ensuring confidentiality. Attending doctors, namely interns, registrars, and occasionally consultants, are tasked to complete these summaries before patient discharge. When an intern prepares the summary, it has to be reviewed by a medical officer or registrar before printing a copy for the parents/ guardians.
Variables were identified from the literature and used to audit each discharge summary, noting the presence or absence of information related to neonatal HIE. In total, 63 variables were assessed, based on the ACOG/AAP diagnosis of HIE.[16] Data were collected by means of a data collection sheet. Variables included diagnosis and ICD-10 codes, maternal parameters, birth and resuscitation history, details of clinical examination, treatment and management plan, special investigations, rehabilitation and follow-up, as well as notes on counselling of parents. A pilot study was conducted, and those results were included in the final analysis.
Data analysis
Data were transferred to a Microsoft Excel spreadsheet (Microsoft Corp., USA) and analysed by the Department of Biostatistics, Faculty of Health Sciences at UFS, using SAS version 9.4 (SAS Institute, USA). Results were summarised as frequencies and percentages.
Results
In total, 165 neonates with HIE were identified; 24 patients (14.5%) were excluded owing to missing or incorrect patient details in admission registers. The latter patients could not be matched with a maternal hospital number on Meditech, despite being noted as a patient with HIE in the admission register. In some cases, a maternal number was written, or no number was available. A further 10 patients (6.1%) did not have Meditech discharge summaries, therefore 131 (79.4%) electronic discharge summaries were retrieved and audited.
Of the 131 patients, 14 (10.7%) died and 97 (74.0%) were discharged. Transfers to other institutions were documented in 17 (13.0%) summaries; the outcomes of three (2.3%) patients were unknown. Date of discharge, death or transfer was not captured for 21 (16.0%) patients. The final diagnosis did not appear in 44 (33.6%) summaries, and the ICD-10 code, i.e. P91.6, was absent in more than half (n=69; 52.7%) of the summaries. The grading of HIE as mild, moderate or severe was not specified for 38 (29.0%) patients.
Basic maternal data regarding the current pregnancy were captured well, but the specification of risk factors related to birth asphyxia was absent in 54 (41.2%) summaries (Supplementary Table 1: https://www.samedical.org/file/2095).
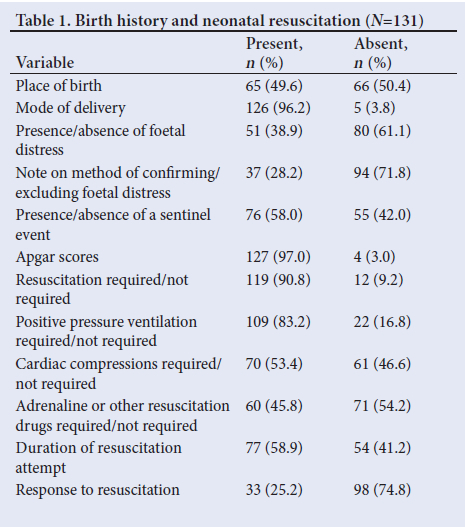
Information regarding perinatal factors is summarised in Table 1. Notably, the presence or absence of foetal distress and the method to confirm or exclude perinatal compromise were absent in 80 (61.1%) and 94 (71.8%) summaries, respectively. A sentinel event was not specified in 55 (42.0%) cases. Apgar scores were entered in all but 4 (3.0%) patients.
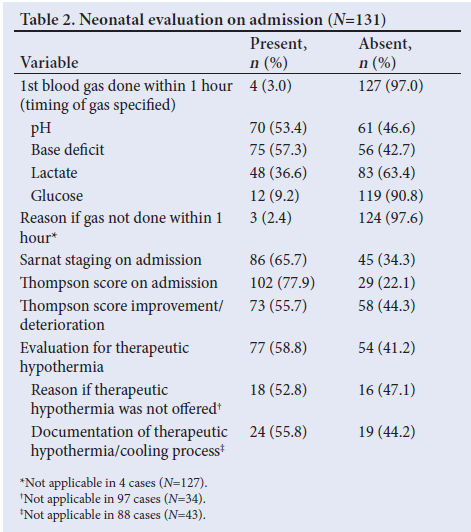
Timing of the first blood gas was not specified in 127 (97.0%) summaries. Admission gas results were inconsistently captured, with 56 (42.7%) and 83 (63.4%) summaries not specifying metabolic acidosis and hyperlactataemia, respectively. Information indicating the severity of HIE was not consistently captured; 45 (34.3%) summaries had no Sarnat staging, and 29 (22.1%) did not mention Thompson scores. Eligibility criteria for therapeutic hypothermia were noted to have been applied in 77 (58.8%) summaries. Only 43 (55.8%) of the 77 evaluated patients received targeted temperature management. No reasons were specified for withholding therapeutic hypothermia for 16 (47.1%) of the 34 patients who were not cooled (Table 2).
In the evaluation and monitoring of the central nervous system of an HIE patient, information on amplitude-integrated encephalogram (aEEG) monitoring was not available for 97 (74.0%) patients. Cranial ultrasound results were absent in 106 (80.9%) summaries. Only one patient had a documented brain MRI. The exclusion of meningitis was not mentioned in 105 (80.2%) summaries.
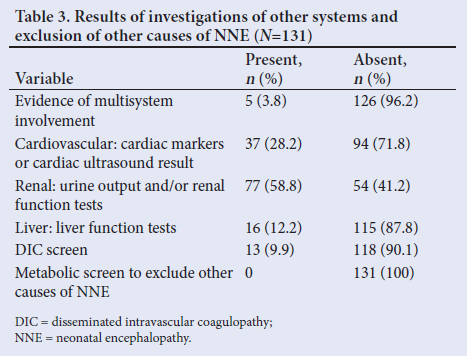
Table 3 refers to the exclusion of other causes of NNE. None of the summaries recorded metabolic screening investigations. Cardiac, renal, liver and haematological involvement were not described in 94 (71.8%), 54 (41.2%), 115 (87.8%) and 118 (90.1%) summaries, respectively.
Management was poorly captured (Supplementary Table 2: https://www.samedical.org/file/2095), with the need for respiratory and inotropic support not documented for 44 (33.6%) and 116 (88.6%) patients, respectively. The involvement of allied health services was not specified for 75 (64.1%) of the 117 survivors.
The final cause of death was not specified for 12 of the 14 (85.7%) patients who demised. Details on the neurological condition at discharge were absent in 84 (64.1%) summaries. Outpatient follow-up appointments for neurodevelopmental assessment were absent in 43 (36.7%) summaries. Most summaries did not specify dates for rehabilitation services (Supplementary Table 3: https://www.samedical.org/file/2095).
Most of the summaries did not capture the counselling of the parents or relatives regarding the condition and prognosis of their infants (83.2%). Information on a palliative care plan, which was indicated for 92 patients, was not seen in 76 (82.6%) summaries.
Discussion
In the present study, 34 (20.6%) patients were excluded owing to poor admission documentation and missing discharge summaries.
This value was close to the results of an SA study,[2] where 21.7% of paediatric admission files did not have a discharge summary. This is quite concerning, as the studies were conducted in tertiary academic settings.
The final diagnosis of HIE, absent in 44 (33.6%) summaries, was lower than the findings of a 2016 study in an SA paediatric population in which the principal diagnosis was missing in 56.2% of the population,[2] but higher than the 7.1%[17] and 30.9%[18] reported in two other studies, respectively. The absence of the ICD-10 coding in 52.7% of the summaries was more than reported in a 2016 study in Gauteng, where it was omitted in 32.8% of summaries,[2] but similar to a study in the Western Cape, with absent ICD-10 coding in 54.7% of electronic records.[19] This coding system will be essential for the future successful implementation of the National Health Insurance (NHI) policy in SA.[19] Poor documentation regarding the diagnosis may also negatively impact the quality, safety and efficacy of outpatient and long-term patient care and may increase medico-legal risk.[20]
Literature suggests a preceding risk factor in up to 65.0% of neonates born with HIE,[21,22] raising concerns about possible poor documentation and underreporting of known risk factors for HIE and identification of peripartum foetal distress, lacking in 41.2% and 61.1% of summaries, respectively. Donn et al.[l2] also postulated that a major obstetric factor that leads to malpractice claims is failure to diagnose foetal distress during labour. A sentinel event, such as cord prolapse, uterine rupture or abruptio placentae, is highly suggestive of asphyxia related to the birth[16,22] of a baby; however, a specific sentinel event was not mentioned in 42.0% of audited summaries. Under-reporting of known risk factors for HIE may bring into question the validity of the final diagnosis.
Details of the neonatal resuscitation attempt at birth were not captured optimally in the summaries. The extent of resuscitation will influence the subsequent management, as well as prognosis and expected long-term neurological sequelae of the patient. It is also likely to be critically evaluated during legal proceedings; hence, the clinician must fully document the resuscitation of infants with suspected HIE.[12,20]
The timing of the first blood gas sample, taken on admission, was absent in 97.0% of summaries, even though a blood gas within an hour of birth is one of the requirements to make the diagnosis of HIE.[10,23,24] Blood gas results on admission were inconsistently captured, with 42.7% and 63.4% of the summaries not specifying metabolic acidosis and hyperlactataemia, respectively. Both persistently high metabolic acidosis and lactate may indicate a fatty acid oxidation defect or an organic acidaemia as the cause of an NNE.[20] Staging HIE by the Thompson score was not captured in 22.1% of summaries, and the Sarnat staging even less frequently at 34.3%. Both scoring systems have implications for the management strategy and may aid in predicting long-term neurological outcomes.[25] However, further prospective studies are necessary to assess such outcomes and are beyond the scope of this study.
Evaluation for eligibility for therapeutic hypothermia was not captured in the summaries for 54 (41.2%) patients. The reason for not offering this standard of care was absent in 18 (52.9%) of the 34 patients who were considered for therapeutic hypothermia but not cooled. Treating patients with moderate HIE with therapeutic hypothermia has been shown to improve neurological outcomes.[20,26-28] The number needed to treat to get a beneficial outcome is seven patients, which means that, despite significant long-term benefits, it is still ineffective in some infants with HIE.[20,26] In a North African study,[28] 56% of the neonates who received therapeutic hypothermia had normal neurological outcomes at 18-month follow-up. Not clearly documenting decisions regarding management with what is now the standard of care, poses a medico-legal risk.[12,13]
Documentation regarding aEEG monitoring was lacking for 97 (74.0%) patients. As studies suggest that seizures may be wrongly diagnosed on clinical grounds alone in neonates with HIE, neurophysiological monitoring with aEEG is advised.[20,26] Not recognising convulsions may have implications for management and long-term prognosis.[20] Information on neuroimaging was also lacking, which was likely a reflection of the resource-constrained setting. Only one MRI scan and 25 cranial ultrasound results were noted. While there are no major limitations to doing cranial ultrasound scans at the study centres, the paucity of MRI information is most likely due to inaccessibility to this specialised investigation. A brain MRI is the most sensitive imaging modality in the diagnosis of HIE - it confirms the diagnosis as well as the extent and timing of cerebral injury.[16,20] It may also predict expected neurological outcomes.[10,16,20,23,29] If an MRI is unavailable, ultrasound may provide useful information by identifying echogenicity or echodensity 48 hours after an ischaemic cerebral injury.[16,20,27]
Cerebrospinal fluid analysis results were not documented, which may mean that meningitis was not excluded as a cause of NNE in most cases (80.2%). A metabolic screen was not mentioned in any of the summaries. The Vermont Oxford Network NNE Registry found that an asphyxia (i.e. HIE) event accounted for only 15% of all NNE cases.[30] Other causes identified in the literature include trauma, inflammatory disorders, coagulation disorders, infections, inborn errors of metabolism and genetic conditions, which should be excluded.[12, 29-31]
Most summaries did not note multiple system involvement (96.2%). Evaluation of injury to separate systems, typically affected by hypoxia and ischaemia, was inconsistently captured. Multisystem organ failure is required to diagnose HIE.[10,16,23,24,29] Documentation regarding hypoxic-ischaemic insults to other organ systems, therefore, needs to be prioritised.
Omission of the final cause of death in most of the audited discharge summaries also reflects poor documentation identified in this study. Lacking information on the neurological condition at death, discharge or transfer (64.1%) will make follow-up of survivors more difficult.[20,28] Rehabilitation and follow-up plans were poorly highlighted. Visual impairment, hearing loss and cognitive defects are common in survivors of HIE. Prompt and regular allied health follow-ups and interventions are therefore required to identify these defects on time, optimise treatment and improve the quality of life of affected children.[20-26]
Parental involvement through counselling and discussion of palliative care was also poorly documented. Efforts to improve this aspect of care are essential, as poor communication has been described as a major cause of patient dissatisfaction with increased risk for legal action against the healthcare, professional and facility. [13] Considering the resource-constrained setting and the ethical principle of distributive justice, proper documentation of redirection of care is also required to manage resources better.[32
Study limitations and strengths
The present study was retrospective in nature, with inherent limitations. Identifying discharge summaries for inclusion in the study may have been hampered by inaccurate information in admission registers. Clinical notes kept during admission, the patients' true clinical condition, and results of special investigations were not correlated with what was finally captured in the electronic discharge summary. It was also impossible to correlate the completeness of the electronic summaries with the knowledge of the attending physician(s). Minimising the risk of medico-legal action by improved quality of discharge documentation was only postulated in this study but cannot be proven.
However, the strength of this study was in its ability to give near-accurate results as data were easily obtained.
Conclusion and recommendations
Electronic discharge summaries of neonates at risk of adverse neurodevelopmental outcomes secondary to HIE lacked important information related to the condition. Regular auditing of patient records must be prioritised to improve the quality of discharge documents. We recommend the following:
• A standardised discharge summary template for neonates with HIE should be developed. The format of the template can either be paper-based or electronic (such as Meditech) depending on the resources and practices at the specific healthcare facility.
• Further research should be undertaken to audit all discharge summaries of neonatal patients managed at the study centres.
• Evaluation of barriers to accurate completion of discharge summaries, particularly in HIE patients, should be undertaken.
• Guidelines on avoiding legal pitfalls should be considered when documenting the course of HIE patients.
Declaration. This manuscript was submitted in partial fulfilment of the requirements for KMA's MMed degree in Paediatrics and Child Health at UFS.
Acknowledgements. Mrs A Bouwer, former research coordinator, Department of Paediatrics and Child Health, Faculty of Health Sciences, UFS, for her immense contribution towards the process of reviewing and modification of the final research topic and the design of the data collection sheet. Ms T Mulder, medical editor/writer, Faculty of Health Sciences, UFS, for technical and editorial preparation of the manuscript.
Author contributions. KMA was responsible for the study conception and design, acquisition of data, interpretation of data, compiling a report in partial fulfilment for his MMed (Paeds) degree and drafting of the final article. AvdB was the supervisor, and was involved in the study conception and design, as well as critical revision of clinical content. GJ provided methodological input during the planning of the project, performed the data analysis, assisted with data interpretation. All authors read and approved the final article.
Funding. None.
Conflicts of interest. None.
References
1. Health Professions Council of South Africa. Guidelines for good practice in the health care professions. Booklet 9: Guidelines on the keeping of patients' records. Pretoria: HPCSA, 2016. https://www.hpcsa.co.za/Uploads/professional_practice/ethics/Booklet_9_ Keeping_of_Patient_Records_Review%20Draft_vSept_2022.pdf (accessed 15 July 2019). [ Links ]
2. Singh S, Solomon F, Madhi SA, Dangor Z, Lala SG. An evaluation of the quality of discharge summaries from the general paediatric wards at Chris Hani Baragwanath Academic Hospital, Johannesburg, South Africa. S Afr Med J 2018;108(11):953-956. https://doi.org/10.7196/SAMJ.2018.v108i11.12966 [ Links ]
3. Wimsett J, Harper A, Jones P. Components of a good quality discharge summary: A systematic review. Emerg Med Australas 2014;26(5):430-438. https://doi.org/10.1111/1742-6723.12285 [ Links ]
4. Stein R, Neufeld D, Shwartz I, et al. Assessment of surgical discharge summaries and evaluation of a new quality improvement model. Isr Med Assoc J 2014;16(11):714-717. [ Links ]
5. Mostert-Phipps N, Pottas D, Korpela M. Improving continuity of care through the use of electronic records; a South African perspective. S Afr Fam Pract 2012;54(4):326-331. https://doi.org/10.1080/20786204.2012.10874244 [ Links ]
6. Salim Al-Damluji M, Dzara K, Hodshon B, et al. Association of discharge summary quality with readmission risk for patients hospitalised with heart failure exacerbation. Circ Cardiovasc Qual Outcomes 2015;8(1):109-111. https://doi.org/10.1161/CIRCOUTCOMES.114.001476 [ Links ]
7. Adeleke IT, Adekanye AO, Onawola KA, et al. Data quality assessment in healthcare: A 365-day chart review of inpatients' health records at a Nigerian tertiary hospital. J Am Med Inform Assoc 2012;19(6):1039-1042. https://doi.org/10.1136/amiajnl-2012-000823 [ Links ]
8. Marutha NS, Ngoepe M. The role of medical records in the provision of public healthcare services in the Limpopo province of South Africa. S Afr J Inf Manag 2017;19(1):a873. https://doi.org/10.4102/sajim.v19i1.873 [ Links ]
9. Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists' Task Force on neonatal encephalopathy. Pediatrics 2014;133(5):e1482-e1488. https://doi.org/10.1542/peds.2014-0724 [ Links ]
10. Shevell MI. The 'Bermuda triangle' of neonatal neurology: Cerebral palsy, neonatal encephalopathy, and intrapartum asphyxia. Semin Pediatr Neurol 2004;11(1):24-30. https://doi.org/10.1016/j.spen.2004.01.005 [ Links ]
11. Kliegman RM, St Geme J. Nelson Textbook of Pediatrics. 21st ed.:Merhar SL, Thomas CW, eds. Chapter 120: Nervous Systems Disorders.Amsterdam: Elsevier, 2019:918-923. [ Links ]
12. Donn SM, Chiswick ML, Fanaroff JM. Medico-legal implications of hypoxic-ischemic birth injury. Semin Fetal Neonatal Med 2014;19(5):317-321. https://doi.org/10.1016/j.siny.2014.08.005 [ Links ]
13. Taylor B, Van Waart J, Ranchod S, Taylor A. Medicolegal storm threatening maternal and child healthcare services. S Afr Med J 2018;108(3):149-150. https://doi.org/10.7196/SAMJ.2018.v108i3.13139 [ Links ]
14. Lemyre B, Chau V. Hypothermia for newborns with hypoxic-ischemic encephalopathy. Paediatr Child Health 2018;23(4):285-291. https://doi.org/10.1093/pch/pxy028. [ Links ]
15. Chiang MC, Jong YJ, Lin CH. Therapeutic hypothermia for neonates with hypoxic ischemic encephalopathy. Pediatr Neonatol 2017;58(6):475-483. https://doi.org/10.1016/j.pedneo.2016.11.001 [ Links ]
16. American College of Obstetricians and Gynecologists' Task Force on Neonatal Encephalopathy.Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Obstet Gynecol 2014;123(4):896-901. https://doi.org/10.1097/01.AOG.0000445580.65983.d2 [ Links ]
17. Oguego NC, Okoye O, Aghaji A, Maduka-Okafor FC, Okoye OI, Ezegwui IR. Audit of ophthalmology discharge summaries in a Nigerian Teaching Hospital. Niger J Clin Pract 2018;21(7):901-906. https://doi.org/10.4103/njcp.njcp_363_17 [ Links ]
18. Kazmi SM. Quality of electronic discharge summaries at Newham University Hospital: An audit. Br J Med Pract 2008;1(1):30-32. [ Links ]
19. Dyers RE, Evans J, Ward GA, Du Plooy S, Mahomed H. Are central hospitals ready for National Health Insurance? ICD coding quality from an electronic patient discharge record for clinicians. S Afr Med J 2016;106(2):181-185.https://doi.org/10.7196/SAMJ.2016.v106i2.10079 [ Links ]
20. Martinello K, Hart AR, Yap S, Mitra S, Robertson NJ. Management and investigation of neonatal encephalopathy: 2017 update. Arch Dis Child Fetal Neonatal Ed 2017;102(4):F346-F358. https://doi.org/10.1136/archdischild-2015-309639 [ Links ]
21. Bruwer DG. Are we doing better? Hypoxic ischemic encephalopathy in Pelonomi Hospital during two time periods. Masters dissertation (Paediatrics). Bloemfontein: University of the Free State, 2016:1-48. [ Links ]
22. Parker SJ, Kuzniewicz M, Niki H, Wu YW. Antenatal and intrapartum risk factors for hypoxic-ischemic encephalopathy in a US birth cohort. J Pediatr 2018;203:163-169. https://doi.org/10.1016/j.jpeds.2018.08.028 [ Links ]
23. MacLennan A. A template for defining a causal relation between acute intrapartum events and cerebral palsy: International consensus statement. BMJ 1999;319(7216):1054-1059. https://doi.org/10.1136/bmj.319.7216.1054 [ Links ]
24. Strijbis EM, Oudman I, van Essen P, MacLennan AH. Cerebral palsy and the application of the international criteria for acute intrapartum hypoxia. Obstet Gynecol 2006;107(6):1357-1365. https://doi.org/10.1097/01.AOG.0000220544.21316.80 [ Links ]
25. Mendler MR, Mendler I, Hassan MA, Mayer B, Bode H, Hummler HD. Predictive value of Thompson-Score for long-term neurological and cognitive outcome in term newborns with perinatal asphyxia and hypoxic-ischemic encephalopathy undergoing controlled hypothermia treatment. Neonatology 2018;114(4):341-347. https://doi.org/10.1159/000490721 [ Links ]
26. Lemyre B, Chau V. Hypothermia for newborns with hypoxic-ischemic encephalopathy. Paediatr Child Health 2018;23(4):285-291. https://doi.org/10.1093/pch/pxy028 [ Links ]
27. Chiang MC, Jong YJ, Lin CH. Therapeutic hypothermia for neonates with hypoxic ischemic encephalopathy. Pediatr Neonatol 2017;58(6):475-483. https://doi.org/10.1016/j.pedneo.2016.11.001 [ Links ]
28. Maoulainine FMR, Elbaz M, Elfaiq S, et al. Therapeutic hypothermia in asphyxiated neonates: Experience from neonatal intensive care unit of University Hospital of Marrakech. Int J Pediatr 2017;2017:3674140. https://doi.org/10.1155/2017/3674140 [ Links ]
29. Hankins GD, Speer M. Defining the pathogenesis and pathophysiology of neonatal encephalopathy and cerebral palsy. Obstet Gynecol 2003;102(3):628-636. https://doi.org/10.1016/s0029-7844(03)00574-x [ Links ]
30. Pfister RH, Bingham P, Edwards EM, et al. The Vermont Oxford Neonatal Encephalopathy Registry: Rationale, methods, and initial results. BMC Pediatr 2012;12:84. https://doi.org/10.1186/1471-2431-12-84 [ Links ]
31. Molloy EJ, Bearer C. Neonatal encephalopathy versus hypoxic-ischemic encephalopathy. Pediatr Res 2018;84(5):574. https://doi.org/10.1038/s41390-018-0169-7 [ Links ]
32. Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet 2009;373(9661):423-431. https://doi.org/10.1016/S0140-6736(09)60137-9 [ Links ]
 Correspondence:
Correspondence:
K M Afolabi
kashi4real@yahoo.com
Accepted 10 January 2023














