Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.17 no.4 Pretoria dic. 2023
http://dx.doi.org/10.7196/SAJCH.2023.v17i4.1976
ARTICLE
The quality of life among children with epilepsy in resource-limited settings: A pilot study in a paediatric neurology clinic at a quaternary care teaching hospital
H HblousI; L MubaiwaII; R GovenderIII
IMMed, FCPaed; Department of Paediatrics and Child Health, Inkosi Albert Luthuli Central Hospital, University of KwaZulu-Natal, Durban, South Africa
IIMB ChB, MA (Child Development, Tufts University); Department of Paediatric Neurology, Inkosi Albert Luthuli Central Hospital, University of KwaZulu-Natal, Durban, South Africa
IIIMB ChB, MPhil; Department of Paediatric Neurology, Inkosi Albert Luthuli Central Hospital, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND: An important part of holistic care management of children with epilepsy (CWE) is measuring their health-related quality of life (HRQOL). However, little is known about the HRQOL of CWE who live in resource-limited settings, particularly in South Africa.
OBJECTIVES: To assess the HRQOL of CWE and to identify the possible factors that correlate with HRQOL including demographic variables and epilepsy health-related factors.
METHODS: A cross-sectional prospective quantitative study was undertaken at the paediatric neurology outpatient clinic at Inkosi Albert Luthuli Central Hospital (IALCH), a quaternary care teaching hospital in Durban, South Africa. Participants were recruited during the period between December 2019 and February 2020. CWE between 2 and 12 years old with no comorbid syndromic disorder or other chronic diseases, accompanied by English-speaking caregivers, were included in the study. We used the Pediatric Quality of Life Inventory 4.0 (PedsQL 4.0) generic core parent-proxy questionnaire modified with separate sociodemographic and epilepsy data collection sheets.
RESULTS: One hundred and twenty participants were recruited. The majority of patients (54.2%) had generalised epilepsy. The aetiology of epilepsy was unknown in 40.8% of patients. The most commonly used anti-seizure medication was sodium valproate (39.2%). The mean of the total score of HRQOL (SD) (coefficient of variation %) was 66.7 (24.1 (36.1)). School attendance p-value <0.001, financial aid for indigent families p<0.047, monotherapy p<0.001, absence of disability p<0.001 and absence of comorbidity p<0.001were strongly associated with good HRQOL total scores.
CONCLUSION: CWE attending IALCH in Durban, South Africa, have compromised HRQOL scores. The variables that significantly correlate with better HRQOL scores are school attendance, receiving financial aid for indigent families, monotherapy, and absence of disabilities and comorbidities. We recommend a multicentre study that involves a larger number of epileptic children with the employment of the epilepsy-specific PedsQL 4.0 module translated into local languages.
Health-related quality of life (HRQOL) is a concept which helps practitioners to understand the social, emotional and physical impact of chronic diseases and to assess healthcare outcome.[1,2] The Pediatric Quality of Life Inventory 4.0 (PedsQL) generic core score scale includes child-self and parent-proxy reports with coefficient of variation (COV). It has been used as a valid, reliable and feasible gauge for assessment of HRQOL of healthy and chronically ill paediatric populations. However, while the child-self report is the standard tool, parent-proxy reports in clinical practice and medical research are cited as important instruments to evaluate HRQOL of children between 2 and 16 years of age who are unable to complete the questionnaire owing to cognitive impairment, very young age or serious illness. In addition, the major advocate for better healthcare services in the paediatric population is the parent's perception and concern of their child's health.[1,3] A fundamental notion in the literature is that children with epilepsy (CWE) have a poorer quality of life.[4-8] There are a few studies that describe good HRQOL scores in children and adolescents with epilepsy[9,10] which could be related to different statistical methods used or different perceptions of health and satisfaction levels among communities. Furthermore, the factors that correlate with poor HRQOL in CWE have been identified in many studies and include epilepsy factors such as seizure frequency, polytherapy, adverse effects of anti-seizure medication and other comorbidities such as attention deficit hyperactivity disorder (ADHD), low intelligence quotient (IQ) and presence of additional disabilities. The social factors influencing HRQOL scores include unemployment of caregivers, poor family resources, higher family demands and parental anxiety.[6,11-15] We conducted the present study in Durban, South Africa, in order to assess parents' perceptions of HRQOL of CWE.
Material and methods
Study design and materials
A cross-sectional prospective descriptive quantitative study was undertaken at a paediatric neurology outpatient clinic at Inkosi Albert Luthuli Central Hospital (IALCH). This is a quaternary care teaching hospital in Durban, South Africa. The participants were recruited from the neurology clinics that were held twice weekly (Monday and Thursday) between December 2019 and February 2020. Patients included were the first 15 patients per clinic aged between 2 and 12 years accompanied by English-speaking caregivers with different educational backgrounds who understood the terminology used in the questionnaire. The caregivers answered questions about their child's health. The exclusion criteria were children who were less than 2 years or more than 12 years of age, caregivers who did not understand the terminology in the questionnaire, children accompanied by companions (not their caregivers) and children with comorbid syndromic disorders, or other chronic diseases such as diabetes, asthma, and cardiac and renal disease.
Measurement tool
We used the PedsQL 4.0 parents-proxy generic report to assess HRQOL. This questionnaire assesses problems experienced by the child in the previous month and noted by the caregiver. It consists of 23 items comprising Physical (8 items), Emotional (5 items), Social (5 items) and School functioning (5 items). The answers for each item are rated (0=never a problem; 1=almost never a problem; 2=sometimes a problem; 3=often a problem; 4=almost always a problem). Items are reverse-scored from a scale of 0 - 100 (4=0, 3= 25, 2=50, 1=75, 0=100). A higher score indicates a better HRQOL. The scale scores are calculated by dividing the sum of the items by the number of items answered. The scale scores were not computed if >50% of the items were missing.
Calculation of the physical health score comprises the physical functioning scale score, and the psychosocial health score is the sum of the emotional, social and school functioning scales over the number of answered items. The final step entails calculating the total health scale score by dividing the physical and psychosocial scores (which is the sum of all items) by the number of items answered on all scales.
We used sociodemographic and epilepsy data sheets to identify factors that correlated with HRQOL scores in CWE. This included personal data such as the child's age, gender, location of residence, caregiver type (parent or guardian), parental educational achievement, occupation, parental marital status and financial aid (grant). The last three factors were used as a proxy indicator of socioeeonomic status. The data collected also included seizure type, number of anti-seizure medications and concurrent disability or comorbidity.
Ethics and procedure
Written informed consent was obtained from the caregiver by the principal investigator. Questionnaires were administered to parents with no translation. Some parents were interviewed before and others were interviewed after the clinic consultation. The sample was classified into three age groups: 2 - 4 years, 5 - 7 years, and 8 - 12 years to be consistent with the questionnaire used.
The study was approved by the University of KwaZulu-Natal Bioethics Research Ethics Committe (ref. no. BREC bE246/19).
Statistical analysis
Statistical analysis was conducted by biostatistician Partson Tinarwo of the Department of Biostatistics, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa, using R-3.6.3 software. Data were summarised in numbers and percentages. While the PedsQL 4.0 scores were analysed, the mean, standard deviation and coefficient variables were calculated. The statistical methods used to analyse the data included mean bars with p-values, i-test, Wilcoxon test for comparing two means, and Kruskal-Wallis test for comparing multiple mean dependant variables on normality of measurements.
Results
Sample characteristics
There were 120 participants recruited, whose ages ranged between 2 and 12 years, with mean (SD) age 6.51 (3.15) years. (Supplementary Table 1, https://www.samedical.org/file/2092).
Fifty-five caregivers (45.8%) had no primary school education; 65 caregivers (54.2%) had secondary school education and above; 73.3% of the caregivers were unemployed (n=88/120); 12.5% had an elementary occupation (n=15/120); 10% were support workers (n=12 /120); and 4.2% were technicians or professionals (n=5/120).
Epilepsy and associated disabilities and comorbidities in CWE
The main seizure type was a generalised tonic-clonic (40% of participants). The aetiology of the epilepsy was unknown in 40.8% of children; 22.5% had a comorbid neuro-behavioural disorder; and 47.5% had a physical disability. Most of the children were on monotherapy (45.8%). The prescribed medications in our participants were sodium valproate (39.2%), a combination of sodium valproate and topiramate (17.5%), sodium valproate, topiramate and clonazepam (7.5%), sodium valproate and lamotrigine (6.7%).
HRQOL in CWE
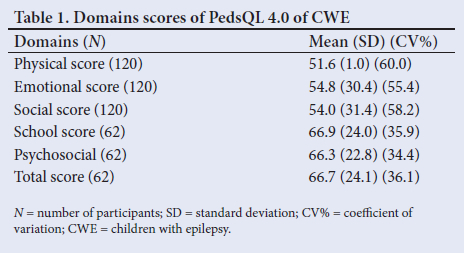
The mean of the total scale score of 62 participants was 66.7 (24.1%). Fifty-eight participants (48.3%) had missing data for the school domain. The mean of the total scale score indicates a compromised HRQOL among CWE attending IALCH in Durban, South Africa. Moreover, in our sample, the physical health scale score was significantly lower than for all the other domains of HRQOL. Table 1 shows the mean score of each domain of PedsQL 4.0.
Variables influencing HRQOL in CWE
Child self-characteristic and sociodemographic variables
Table 2 compares the demographic variables of the patients with the HRQOL domains. The means calculated for the physical, emotional and social health scores were derived from all of the study participants (N=120). The means calculated for the school, and the psychosocial and total HRQOL scores, were derived from the group of 62 children attending school. The apparent higher psychosocial health scores and total health scores in some instances are because these scores were only completed for the group of 62 children attending school.
There was a statistically significant negative effect of the absence of schooling (p-value <0.00) and receiving a care dependency grant (CDG) (p-value 0.05) on HRQOL scores of CWE (Table 2), which is expected, as epileptic children with multiple disabilities generally do not attend school.
There was no statistical significance in correlation between HRQOL scores and children's location, caregivers, marital status of caregiver, caregiver level of education and caregiver employment status. There was a tendency of males with epilepsy, age 2 - 4 years, CWE living in rural areas, and children whose caregivers were single parents or unemployed to have lower HRQOL scores than those with other variables. We omitted race because most of our population were of African indigenous ancestry (Table 2).
Epilepsy-specific variables
Monotherapy and absence of disabilities and comorbidities were associated with higher HRQOL scores of CWE (p-value <0.001) for each variable (Table 3).
The group of CWE and no disability had good scores with a minimum of 75.6 for emotional and a maximum of 89.2 for social scale. In addition, focal epilepsy was associated with better physical health (p-value 0.023), and emotional (p-value<0.00), social (p-value 0.04) and school scores (p-value 0.02).
Discussion
Our findings are consistent with data in existing literature that CWE have a compromised HRQOL.[4-8] Conversely, a few studies have also reported that adolescents and CWE have a good HRQOL.[9,10] This variation could be explained by the diversity of the tools used to measure HRQOL or because of different perceptions of communities towards the concept of health.
In our study, the mean of HRQOL total scale score was 66.7, which is similar to the mean of HRQOL total scale score of 67.21 in the private healthcare setting in the Indian study. The Indian study concluded that CWE have poorer HRQOL in both private and public care settings, with a mean of 67.21 for patients in the private sector and 78.66 for public care settings.[8]
Socio-economic and demographic variables including age, gender, location, caregiver either parents or guardian, marital state of caregiver, caregiver level of education, and caregiver employment state did not affect the HRQOL significantly in our study. In addition, our study showed that there was a significant influence of child support grant and school attendance on good HRQOL scores of CWE. However, male gender, age 2 - 4 years, residence in rural areas, guardian caregivers, single parents and unemployed caregivers correlated with lower HRQOL scores that were not statistically significant. These findings are similar to those in other studies.[11,14,15
Previous studies have reported that some socio-economic and demographic variables were significantly correlated with HRQOL.[8,1tU6,171 Older age of child and lower socioeconomic status,[16] younger age of child at onset of epilepsy,[8] male caregivers and lower level of education of caregivers[10] were associated with poorer HRQOL. Reinforcing these findings, high level of education and income of caregivers,[8] and more specifically higher maternal education and maternal employment,[17] were correlated with higher
HRQOL scores.
Regarding the epilepsy data, the present study showed that there was a statistically significant positive influence of monotherapy, absence of disabilities and comorbidities on HRQOL. Most studies in the literature mirrored these findings and emphasised the negative influence of early onset of epilepsy, higher seizure frequency, number and neurotoxic effect of anti-seizure medications, and presence of disabilities and comorbidities on HRQOL.[5,6,8,12,14,18] Furthermore, ADHD, particularly the combined hyperactive-inattentive subtype, was found to be associated with a compromised HRQOL.[19] An American study conducted in 2010 highlighted the relationship between common anti-seizure medication and longitudinal HRQOL of CWE aged 2 - 12 years across 7 months. Sodium valproate was associated with improvement in emotional HRQOL.[20] This was not assessed owing to the majority of our monotherapy children being on sodium valproate, and our study was a point prevalence assessment. In our study, there was no statistically significant correlation between seizure type and HRQOL. In the literature, two studies mentioned this correlation. However, one study found that partial seizure was correlated with a poorer HRQOL[21] while the other study found that generalised seizure disorder correlated with a poorer HRQOL.[4]
Limitations
We hope that the present study will assist future researchers in understanding the HRQOL of CWE in South Africa. However, the limitations of our study include:
1. The PedsQL4.0 instrument we used is a generic core proxy form and not an epilepsy-specific module.
2. Our study was conducted in a specialised epilepsy clinic in a quaternary referral centre in KwaZulu-Natal and therefore the patients recruited were not representative of CWE who attend lower levels of care. This selection bias will tend to skew the cohort to children with severe epilepsy and comorbidities and hence will be likely to score lower HRQOL scores.
3. Non-English-speaking caregivers were excluded because of the language barrier between the researcher and the patients.
4. The questionnaire was performed before the clinic visit in some cases and after in others. This might have caused a mild form of bias.
5. Lack of a control group.
Conclusion
CWE attending the paediatric neurology clinic at IALCH (a quaternary care teaching hospital) in Durban, South Africa, have compromised HRQOL scores in all the domains. Their physical health was significantly more affected than the psychosocial and total health scores, which is possibly because there were limited/ incomplete data on psychosocial and total health (58 caregivers did not complete this aspect of the questionnaire as these children were not at school).
The variables that significantly correlate with better HRQOL scores were school attendance, receiving financial aid for indigent families, monotherapy and absence of disabilities and comorbidities.
For the future, we recommend a multicentre study involving a larger number of children with epilepsy who are sub-classified by their levels of physical and cognitive ability and the use of an epilepsy-specific assessment tool that is translated to local languages. A control group of healthy children from similar socio-economic backgrounds would also improve the quality of comparison.
Recommendations
Systemic screening of CWE for disabilities and comorbidities, particularly ADHD.
1. Early referral of children with physical disability for rehabilitation.
2. Early school placement to promote better HRQOL.
3. Preferential use of appropriate monotherapy (dose and selection of anti-seizure medication) to treat epilepsy as far as possible.
4. Providing a clinical psychology service at the neurology clinic to assist young adolescents and single caregivers would be beneficial.
Declaration. None.
Acknowledgements. We thank Mr Partson Tinarwo (biostatistician, University of KwaZulu-Natal) for his help in analysis; nursing staff of the Paediatric Neurology Clinic of the Inkosi Albert Luthuli Central Hospital; and participating families/caregivers of children with epilepsy.
Author contributions. Conceptualisation: HH, LM, RG. Data collection: HH. Data analysis: HH, LM, PT. Writing of original draft: HH, LM, RG. Editing: HH, LM, RG. Supervision: LM, RG.
Funding. None.
Conflicts of interest. None.
References
1. Varni JW, Limbers CA, Burwinkle TM. Parent proxy-report of their children's health-related quality of life: An analysis of 13,878 parents' reliability and validity across age subgroups using the PedsQL 4.0 Generic Core Scales. Health Qual Life Out 2007;5:2. https://doi.org/10.1186/1477-7525-5-2 [ Links ]
2. Calman KC. Quality of life in cancer patients-an hypothesis. J Medical Ethics 1984;10 (3):124-127. https://doi.org/10.1136/jme.10.3.124 [ Links ]
3. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambulatory Pediatr 2003;3 (6):329-341.https://doi.org/10.1367/1539-4409(2003)003<0329:TPAAPP>2.0.CO;2 [ Links ]
4. Monir ZM, EL-Alameey IR, Eltahlawy E. Health related quality of life of children with epilepsy in Egypt. J Arab Soc Medical Res 2013;8(2):53. https://doi.org/10.4103/1687-4293.123787 [ Links ]
5. Miller V, Palermo TM, Grewe SD). Quality of life in pediatric epilepsy: Demographic and disease-related predictors and comparison with healthy controls. Epilepsy Behav 2003;4(1):36-42. https://doi.org/10.1016/s1525-5050(02)00601-7 [ Links ]
6. Malhi P, Singhi P. Correlates of quality of life with epilepsy. Indian J Pediatrics 2005;72(2):131-135. https://doi.org/10.1007/bf02760697 [ Links ]
7. Abbas Z, Elseed MA, Mohammed IN. The quality of life among Sudanese children with epilepsy and their care givers. Sudanese J Paediatrics 2014;14 (1):51 [ Links ]
8. Karnavat PK, Hegde AU, Kulkarni S. Quality of life in children with epilepsy in private and public tertiary care centers in India. Int J Epilepsy 2018;5(01):28-37. https://doi.org/10.1055/s-0038-1660774 [ Links ]
9. Siqueira NF, Oliveira FL, Siqueira JA, de Souza EAP. Quality of life in epilepsy: A study of Brazilian adolescents. PLoS ONE 2014;9(9):e106879. https://doi.org/10.1371/journal.pone.0106879 [ Links ]
10. Hussain SR, Orwa J, Sokhi DS, et al. Determining the quality of life of children living with epilepsy in Kenya-a cross-sectional study using the CHEQOL-25 tool. Seizure 2020;76:100-104. https://doi.org/10.1016/j.seizure.2020.01.00 [ Links ]
11. Conway L, Smith ML, Ferro MA, et al. Correlates of health-related quality of life in children with drug resistant epilepsy. Epilepsia 2016;57(8):1256-1264. https://doi.org/10.1111/epi.13441 [ Links ]
12. Hoare P, Mann H, Dunn S. Parental perception of the quality of life among children with epilepsy or diabetes with a new assessment questionnaire. Qual Res 2000;9 (6):637-644. https://doi.org/10.1023/a:1008980608568 [ Links ]
13. Ferro MA. Risk factors for health-related quality of life in children with epilepsy: A meta-analysis. Epilepsia 2014;55(11):1722-1731. https://doi.org/10.1111/epi.1277 [ Links ]
14. Adewuya AO, Oseni SB. Impact of psychiatric morbidity on parent-rated quality of life in Nigerian adolescents with epilepsy. Epilepsy Behav 2005;7 (3):497-501. https://doi.org/10.1016/j.yebeh.2005.07.011 [ Links ]
15. Sherman EM, Griffiths SY, Akdag S, Connolly MB, Slick DJ, Wiebe S. Sociodemographic correlates of health-related quality of life in pediatric epilepsy. Epilepsy Behav 2008;12(1):96-101. https://doi.org/10.1016/j.yebeh.2007.07.009 [ Links ]
16. Devinsky O, Westbrook L, Cramer J, Glassman M, Perrine K, Camfield C. Risk factors for poor health-related quality of life in adolescents with epilepsy. Epilepsia 1999;40(12):1715-1720. https://doi.org/10.1111/j.1528-1157.1999.tb01588.x [ Links ]
17. Hirfanoglu T, Serdaroglu A, Cansu A, Soysal AS, Derle E, Gucuyener K. Do knowledge of, perception of, and attitudes toward epilepsy affect the quality of life of Turkish children with epilepsy and their parents? Epilepsy Behav 2009;14(1):71-77. https://doi.org/10.1016/j.yebeh.2008.08.011 [ Links ]
18. Sabaz M, Cairns DR, Lawson JA, Bleasel AF, Bye AM. The health-related quality of life of children with refractory epilepsy: A comparison of those with and without intellectual disability. Epilepsia 2001;42(5):621-628. https://doi.org/10.1046/j.1528-1157.2001.25200. [ Links ]
19. Sherman EM, Slick DJ, Connolly MB, Eyrl KL. ADHD, neurological correlates and health-related quality of life in severe pediatric epilepsy. Epilepsia 2007;48 (6):1083-1091. https://doi.org/10.1111/j.1528-1167.2007.01028.x [ Links ]
20. Modi AC, Ingerski LM, Rausch JR, Glauser TA. Treatment factors affecting longitudinal quality of life in new onset pediatric epilepsy. J Pediatric Psychology 2011;36(4):466-475. https://doi.org/10.1093/jpepsy/jsq114 [ Links ]
21. Aggarwal A, Datta V, Thakur L. Quality of life in children with epilepsy. Indian Pediatrics 2011;48(11):893-896. https://doi.org/10.1007/s13312-011-0137-3 [ Links ]
 Correspondence:
Correspondence:
H Hblous
haifahblous@gmail.com
Accepted 5 July 2022














