Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.17 n.4 Pretoria Dec. 2023
http://dx.doi.org/10.7196/SAJCH.2023.v17i3.1994
ARTICLE
An analytical investigation into noise levels in public health sector neonatal intensive care units in the eThekwini District
S Ismail; S Panday
MA; Discipline of Audiology, School of Health Sciences, University of KwaZulu-Natal, South Africa
ABSTRACT
BACKGROUND: Noise is a known environmental stressor in the neonatal intensive care unit (NICU), as it may result in adverse effects on preterm neonates because of the unique vulnerability and physiological immaturity of their central nervous systems.
OBJECTIVE: To investigate noise levels in public sector NICUs in the eThekwini District, KwaZulu-Natal Province, South Africa. Methods. An analytical observational study design with purposive sampling of public sector hospitals was used. Noise was continuously measured with a sound level meter in a central location for 48 hours on 2 consecutive days (Sunday and Monday) in the four NICUs. A sample of noise sources, as well as their frequency of occurrence, was identified through direct observation and a frequency spectrum analysis using one-third octave bands. Data were analysed using descriptive and inferential statistics.
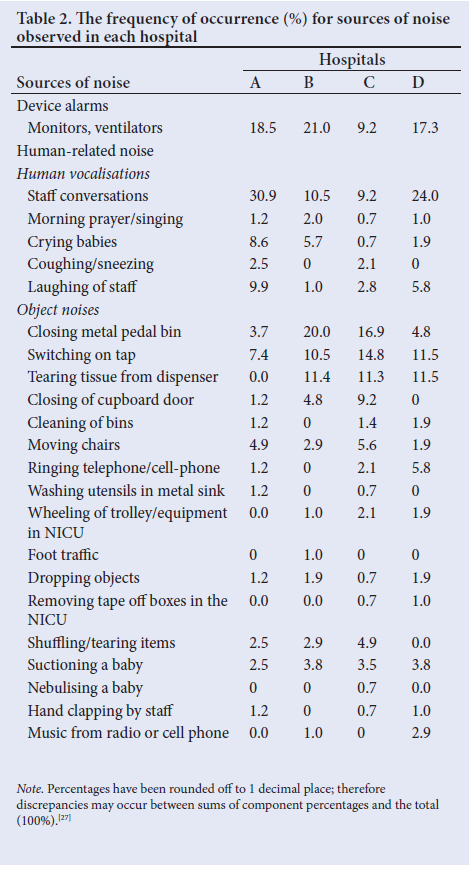
RESULTS: This study included one tertiary hospital and three regional hospitals in the eThekwini District. Mean noise levels exceeded international recommendations of an A-weighted equivalent continuous sound level (LAeq) of 45 A-weighted decibel (dBA) and an A-weighted maximum sound level (LAmax) of 65 dBA in all four hospitals. The most frequently occurring sources of noise were staff conversations (30.9%, Hospital A), device alarms (21.0%, Hospital B) and closing metal pedal bins (20.0%, Hospital B). Mean LAeqs >45 BA were found in the mid and high frequencies (250 Hz - 6 300 Hz) in all hospitals, particularly during the afternoon.
CONCLUSION: The findings emphasise the need for continuous noise monitoring, awareness and education among healthcare professionals in the NICU. Future research should expand on existing findings and focus on interventions for noise control in NICUs.
Noise is a known environmental stressor in the neonatal intensive care unit (NICU), as it may result in adverse effects on preterm neonates because of the unique vulnerability and physiological immaturity of their central nervous systems.[1-7] The neonate's auditory system is developed and functional from 20 - 25 weeks of gestational age; therefore, in the absence of a congenital abnormality, most preterm neonates can hear when admitted to the NICU.[8] An intense noise may startle the neonate and result in adverse physiological effects, such as increased blood pressure, heart rate or respiratory rate, decreased oxygen saturation and sleep disorders.[3,5,8-10] Overexposure to constant high levels of noise, particularly at high frequencies, can adversely affect neurodevelopmental outcomes and auditory development, resulting in delayed speech and learning acquisition, which is often seen in the preterm population.[8,10] In addition to noise, neonates in the NICU are exposed to other risk factors for hearing loss, such as prematurity, very low birth weight, intensive care treatment with mechanical ventilation, hypoxia, hyperbilirubinaemia and exposure to HIV and ototoxic medication, with a higher occurrence in developing countries.[6] The well-documented effects of noise that are seen in preterm neonates emphasise the need for investigating and reducing noise in the NICU.[1-3]
A sound level meter (SLM) with an A-weighted filter is commonly used when investigating noise in the NICU. This filter setting approximates the frequency sensitivity of human hearing and is reported in A-weighted decibels (dBA).[11] A-weighted equivalent continuous sound levels (LAeqs) are used to measure the overall level of noise exposure over a period of time.'[12] Z-weighted peak sound levels (LZpeaks) are used to identify the highest noise levels that occur instantaneously.'121 A-weighted maximum sound levels (LAmax) differ from LZpeaks, as they measure maximum noise levels over a period of time.[12] LAeqs are associated with identifying continuous noise sources (babies crying, conversations), and LZpeaks are associated with identifying transient noise sources (closing metal pedal bins, dropping an object).[13] Prolonged exposure to continuous noise, especially at higher frequencies, may result in permanent auditory damage and hearing loss, whereas the high intensity from a transient noise can also cause acoustic trauma.[11,14]
Several studies have found that noise in the NICU exceeds the American Academy of Pediatrics (AAP) recommendation, which stipulates that continuous sound should not exceed an LAeq of 45 dBA and a transient sound or LAmax of 65 dBA.[1-3,5,9] The risk for auditory damage depends on the level (loudness), duration (time period) and frequency of exposure to noise, which should be continuously measured over 24 hours representing a full day and night. However, previous studies have short measurement periods and limited data on the frequency content of noise in the NICU.'[2,14-16] The majority of studies have found that human-generated sounds and device alarms are the main sources of noise in the NICU.[9,13,17-20] Two local studies conducted in Gauteng and the Western Cape provinces suggest that noise levels may be related to staff activities and room acoustics; however, lack of data in the South African (SA) context limits generalisations to other hospitals.[17,18] Consequently, the present study aimed to investigate noise levels, sources and the frequency content in public sector hospitals in the eThekwini District, KwaZulu-Natal Province.
Method
This study adopted an analytical observational study design at four public sector hospitals, including one tertiary, and three regional hospitals, in the eThekwini District. Ethics approval was obtained from the University of KwaZulu-Natal (UKZN) Humanities and Social Sciences Research Ethics Committee (HSSREC) (ref. no. HSS/1903/017M). An SLM (Cel-450 C; Keison, UK) with an A-weighted frequency weighting and a time-weighting of slow response was used, according to the South African National Standards (SANS 10083:2013).[12] Noise measurements were expressed in LAeq, minimum A-weighted sound level (LAmin), LAmax, and LZpeak.[12] The frequency analysis was conducted using a one-third octave band filter setting to determine intensities in low, mid and high frequencies, which were measured in Hertz (Hz).[11]
A pilot study was conducted at a tertiary public sector hospital in eThekwini that was not included in the main study. The pilot study was conducted to assess the functioning of the SLM in the NICU, as well as the feasibility of the methods used, including the duration of the measurements and observation of the sources of noise. The main study occurred at four public hospitals where the researcher conducted site surveys (Table 1) and developed floor plans for each NICU. The SLM and microphone were calibrated according to the manufacturer's specifications on each day. The SLM was positioned using the central site procedure and SANS 10083:2013 to determine the overall noise that neonates were exposed to in each NICU.[12,17,19-21] Noise measurements were conducted continuously for 48 hours on 2 consecutive days of the week. A Sunday and Monday were purposively selected to represent a weekend and a weekday, as research has identified significant differences in noise levels between them.[16,22,23] Noise measurements were recorded on a noise measurement form, categorised as morning (7h00 - 13h00), afternoon (13h00 - 19h00) and night (19h00 - 7h00) periods. A sample of the sources of noise and their frequency of occurrence were observed during the morning and recorded in a field diary and a sources-of-noise checklist (Table 2). The checklist was categorised according to device alarms and human-related sources, adapted from other studies.[13,18]
After the data collection period, the results were entered into an Excel worksheet (Microsoft Corp., USA), with descriptive and inferential statistics being used to calculate frequency counts and percentages for each source of noise, which were represented in tables. Noise measurements and one-third octave band analysis results were transferred from the SLM to a portable computer using the dB23 software and displayed on Excel worksheets for data analysis. With the assistance of a statistician (Dr Wilbert Sibanda) the statistical analysis was performed using computer-based software, the Statistical Package for Social Sciences - version 25 (SPSS-V25; IBM Corp, USA). For the interpretation of inferential statistics, a p-value of <0.05 was considered significant.
Results
The highest mean LAeqs were observed during the afternoon in all NICUs, and the lowest during the night (Table 3). There were no significant differences between mean LAeqs during the morning, afternoon and night except in hospital D, with a marginal difference being recorded (p=0.05). There were no significant differences between the LAeqs on Sunday and Monday, except in hospital C, where Sunday had significantly lower mean LAeq levels than Monday (p=0.028).
The most frequently occurring sources of noise were staff conversations (30.9%, Hospital A), monitors and ventilators (21.0%, Hospital B) and closing metal pedal bins (20.0%, Hospital B) (Table 2). Further analysis of the results found that activities which increased the LAeq were the morning prayer (72.7 dBA), the presence of multiple high-frequency alarms (74.6 dBA), closing metal pedal bins (63.6 dBA), doctors' rounds (59.7 dBA) and dropping a metal stool (64.1 dBA). The sources of noise which increased the LZpeak were the presence of multiple high-frequency alarms (109.7 dBA), closing a metal pedal bin (110.1 dBA), doctors' rounds (103.6 dBA), and dropping objects (116.0 dBA, 110.8 dBA).
One-third octave band analysis from 20 Hz to 20 000 Hz found that the highest LAeqs were seen in the mid to high frequencies (200 Hz to 8 000 Hz). Further analysis found that mean LAeqs >45 dBA were seen specifically between 250 Hz and 6 300 Hz on Sunday and Monday. On Sunday, the afternoon had the highest LAeq levels in the mid frequencies (mean (SD) 50.0 (3.7)) and the high frequencies (mean (SD) 41.3, (11.8)), compared with the morning and night shifts. A similar result was seen on Monday, as the afternoon had higher LAeq levels in the mid frequencies (mean (SD) 51.7 (3.8)), compared with the morning and night shifts, except that the morning had a higher LAeq in the high frequencies (mean (SD) 40.8 (11.3)), compared with the afternoon and night shifts.
Discussion
Consistent with other studies, the noise levels exceeded AAP recommendations, which may result in negative outcomes for the health and recovery of preterm neonates.[9,17,18] High noise levels that are constant throughout the day and night may result in overstimulation and alter the functioning of the auditory system, as the hair cells in the cochlea have no time to rest. In an occupational setting, the time that an individual spends in a noisy environment is reduced should the noise level exceed the recommended level, but this is not the reality in most NICUs.[11,12] This study found that noise levels were the highest during the afternoon; this is similar to other studies that related high noise levels to shift changes, visiting hours, treatment activities and more device alarms being activated.[13,20,23] This study found a significant difference between LAeqs on Sunday and Monday in hospital C, which may be due to Sundays having fewer staff members and associated activities compared with Mondays, although this was not seen in other hospitals. Implementation of proper noise control guidelines in all NICUs is needed, which should include posting visual reminders to be quiet, dimming the light, closing doors to external noise sources and lowering of voices to create a calm acoustic environment, especially during the night.[8,24] The present study found that staff conversations and device alarms occurred the most, this being consistent with previous studies[9,17,18,22,24] Staff conversations were most frequent in hospital A (30.9%) (Table 2), which was surprising, as it had the least number of staff members (four nurses) (Table 1). A plausible reason may be that hospital A was a tertiary facility that was involved in many activities, such as student training, multiple ward rounds and frequent visits from specialists, which may have increased the number of conversations. Device alarms occurred the most in hospital B (21.0%), as it had the highest number of babies (10) at that time, while hospital A (18.5%) had 4 babies yet the number of alarms activated was similar to hospital B. The number of alarms may not only be related to the number of babies but also to their critical state, as critically ill babies require more machines and monitoring, which may have resulted in frequent alarms having been activated.[19,23] This study found that the presence of multiple high-frequency alarms increased the LAeq to 74.6 dBA and the LZpeak to 109.7 dBA, which is of concern for preterm babies. The findings have implications for educating both medical staff and students, and limiting the number of people entering the ward at the same time.
The most frequently occurring object noise was the closing of metal pedal bins, specifically in hospitals B (20.0%) and C (16.9%) (Table 2), which had the most metal pedal bins (hospital B (9) and C (15)) (Table 1). However, further analysis found that the frequent use of metal pedal bins may not be a concern if closed quietly. When they are closed loudly, the LZpeak increased to 110.1 dBA, which subsequently increased the LAeq to 63.6 dBA. The findings are of concern, as there are multiple metal pedal bins situated next to the babies' beds and various other metal objects in the NICU. Intervention may include a reduction of metal pedal bins in the room, use of alternative bins and stools, such as plastic ones, use of protector pads on bin lids, and most importantly, educating staff on careful handling of noisy objects to alleviate potential noise hazards.
Additionally, a possible contributor to the overall noise level was singing during the morning prayer (72.7 dBA), which has not been identified in other international and local studies. Research suggests that singing is the most common and simplest form of spiritual nursing care in SA public hospitals, particularly found in KwaZulu-Natal.[25] Further research is needed to investigate its relationship to the noise levels in hospitals. The findings have implications for creating awareness among healthcare professionals of the various sources of noise in the NICU. Nurses are the most consistent healthcare professionals in the NICU and should be key role players in the development of noise control protocols. The inclusion of multiple role players may also alleviate any negative attitudes towards noise monitoring in this environment.
Research has found that common sources of noise in the NICU (staff conversations, device alarms) produce frequencies in the mid to high range, consistent with the findings in the present study, which is of concern for preterm babies.[2,14-16] The portion of the cochlea sensitive to high frequencies is the most vulnerable to outer hair cell damage because of the tonotopically organised cochlea.[11] Therefore, preterm babies are susceptible to developing a high-frequency hearing loss as a result of the overexposure of noise for long periods of time in the NICU (greater than 48 hours) in combination with pre-existing risk factors.[26] The potential risk of high-frequency noise is further increased by the fact that the frequency content of noise is rarely monitored and researched, leaving the problem of excessive exposure to mid- and high-frequency noise in the NICU largely overlooked.[14,15] The findings in this study have implications for the role of audiologists to ensure that regular hearing-screening protocols and noise assessment and monitoring programmes, together with targeted education and training for healthcare professionals in the NICU, are provided.[18]
Recommendations
Further research is required to investigate existing standards, and the healthcare professionals' knowledge, attitude and practices towards noise control in the NICU. Such information may assist researchers in understanding gaps in education and training that require immediate attention. The findings from this study may be used to implement noise control programmes and education and training in NICUs. These findings also suggest that noise-control protocols and policies should be established and implemented in all local hospitals.
Study strengths and limitations
This study obtained a realistic representation of the noise exposure, including intensity, duration, frequency content and contextually relevant sources of noise in the NICU. These findings may be generalised to other public hospitals. To ensure reliability and validity of the measurements, this study utilised one SLM in a central location, as differing measuring equipment may introduce variability. Although noise measurements were conducted for 48 hours, possible sources of noise were only observed during the morning. Therefore, reasons for the high noise levels during the afternoon could not be explained further. The researcher's presence during the morning may also have altered the staff behaviour. Future research should consider conducting random observations, using multiple observers or concealing the SLM.
Conclusion
The present study findings emphasise the need for continuous noise monitoring, awareness and education among all healthcare professionals to reduce the high noise levels in the NICU. Further research and intervention are needed to establish evidence-based protocols and policies for noise control in that environment. The findings of this study have implications for promoting a change in the way that noise in the NICU should be controlled and managed. This may provide better health outcomes for vulnerable preterm neonates, and possibly improve their developmental outcomes later in life.
Declaration. This article is based on a thesis submitted in partial fulfilment of the requirements for the Master of Audiology degree at the University of KwaZulu-Natal.
Acknowledgments. The authors acknowledge the KwaZulu-Natal Department of Health District Office and management of the hospitals for granting us permission to conduct this study. We extend our appreciation to Carrin Martin for proofreading and editing the manuscript.
Author contributions. SI and SP were responsible for conceptualisation and preparation of the research and manuscript. SI was responsible for data collection and analysis. SI and SP reviewed and approved the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. White RD, Smith JA, Shepley MM. Recommended standards for newborn ICU design. J Perinatol 2013;33(1):S2-S16. https://doi.org/10.1038/jp.2013.10 [ Links ]
2. Lejeune F, Parra J, Berne-Audéoud F, et al. Sound interferes with the early tactile manual abilities of preterm infants. Sci Rep 2016;6(1):1-8. https://doi.org/10.1038/srep23329 [ Links ]
3. Thakur N, Batra P, Gupta P. Noise as a health hazard for children: Time to make a noise about it. Indian Pediatr 2016;53(2):111-114. https://doi.org/10.1007/s13312-016-0802-7 [ Links ]
4. Gallo LF, Olivera JM. Noise pollution control system in the hospital environment. J Physics Conference Series 2016;705(1):012042. https://doi.org/10.1088/1742-6596/705/1/012042 [ Links ]
5. DeArmond AC, Yello JR, Bubshait KS, Krueger CA. Revisiting sound in the NICU: Implications for the developmental timing, amount and type of sound. Pediatr Neonatal Nurs 2016:2470-0983. https://doi.org/10.16966/2470-0983.116 [ Links ]
6. Zimmerman E, Lahav A. Ototoxicity in preterm infants: Effects of genetics, aminoglycosides, and loud environmental noise. J Perinatol 2013;33(1):3-8. https://doi.org/10.1038/jp.2012.105 [ Links ]
7. Smith SW, Ortmann AJ, Clark WW. Noise in the neonatal intensive care unit: A new approach to examining acoustic events. Noise Health 2018;20(95):121. https://doi.org/10.4103/nah.NAH_53_17 [ Links ]
8. McMahon E, Wintermark P, Lahav A. Auditory brain development in premature infants: The importance of early experience. Ann New York Acad Sci 2012;1252(1):17-24. https://doi.org/10.1111/j.1749-6632.2012.06445.x [ Links ]
9. Joshi G, Tada N. Analysis of noise level in neonatal intensive care unit and postnatal ward of a tertiary care hospital in an urban city. Int J Contemp Pediatrics 2016;3(4):1358-1361. https://doi.org/10.18203/2349-3291.ijcp20163677 [ Links ]
10. Venkataraman R, Kamaluddeen M, Amin H, Lodha A. Is less noise, light and parental/caregiver stress in the neonatal intensive care unit better for babies? Indian Pediatr 2018;55(1):17-21. https://doi.org/10.1007/s13312-018-1220-9 [ Links ]
11. Gelfand SA. Pure tone audiometry. In: Essentials of Audiology. 3rd ed. New York: Thieme 2009:127-157 [ Links ]
12. South African National Standards. The Measurement and Assessment of Occupational Noise for Health Conservation Purposes. Pretoria: South African National Standards, 2013: Volume 10083. [ Links ]
13. Laroche C, Fournier P. Study of noise levels in a neonatal intensive care unit. Can Acoust 1999;27(1):11-19. https://jcaa.caa-aca.ca/index.php/jcaa/article/view/1185 (accessed 10 April 2022) [ Links ]
14. Lahav A, Skoe E. An acoustic gap between the NICU and womb: A potential risk for compromised neuroplasticity of the auditory system in preterm infants. Front Neurosci 2014;8:381. https://doi.org/10.3389/fnins.2014.00381 [ Links ]
15. Livera MD, Priya B, Ramesh A, et al. Spectral analysis of noise in the neonatal intensive care unit. Indian J Pediatr 2008;75(3):217-222. https://doi.org/10.1007/s12098-008-0048-z [ Links ]
16. Konkani A, Oakley B. Noise in hospital intensive care units: A critical review of a critical topic. J Crit Care 2012;27(5):522-e1. https://doi.org/10.1016/j.jcrc.2011.09.003 [ Links ]
17. Nathan LM, Tuomi SK, Müller AM. Noise levels in a neonatal intensive care unit in the Cape metropole. S Afr J Child Health 2008;2(2):50-54. [ Links ]
18. Neille J, George K, Khoza-Shangase K. A study investigating sound sources an noise levels in neonatal intensive care units. S Afr J Child Health 2014;8(1):6-10. https://doi.org/10.7196/sajch.676 [ Links ]
19. Valizadeh S, Hosseini MB, Alavi N, Asadollahi M, Kashefimehr S. Assessment of sound levels in a neonatal intensive care unit in Tabriz, Iran. J Caring Sci 2013;2(1):19. https://doi.org/10.5681/jcs.2013.003 [ Links ]
20. Fortes-Garrido JC, Velez-Pereira AM, Gázquez M, Hidalgo-Hidalgo M, Bolívar JP. The characterisation of noise levels in a neonatal intensive care unit and the implications for noise management. J Environ Health Sci Engine 2014;12(1):1-8. https://doi.org/10.1186/2052-336X-12-104 [ Links ]
21. Van Reenen CA. Staff and patient perceptions of noise in SA hospitals: A pilot study. Occup Health South Afr 2016;22(1):18-20. https://doi.org/10520/EJC184668 [ Links ]
22. Alberto Alves Carvalhais C, Vieira Da Silva M, Xavier A, Santos J. Newborns safety at neonatal intensive care units: Are they exposed to excessive noise during routine health care procedures? Global Environment, Health and Safety 2017;1:1-3. http://hdl.handle.net/10400.22/10256 [ Links ]
23. Matook S, Sullivan M, Salisbury A, Miller R, Lester B. Variations of NICU sound by location and time of day. Neonatal Network 2010;29(2):87-95. https://doi.org/10.1891/0730-0832.29.2.87 [ Links ]
24. Ahamed MF, Campbell D, Horan S, Rosen O. Noise reduction in the neonatal intensive care unit: A quality improvement initiative. Am J Med Qual 2018;33(2):177-184. https://doi.org/10.1177/1062860617711563 [ Links ]
25. Chandramohan S, Bhagwan R. Utilisation of spirituality and spiritual care in nursing practice in public hospitals in KwaZulu-Natal, South Africa. Religions 2016;7(3):23. https://doi.org/10.3390/rel7030023 [ Links ]
26. Kanji A, Khoza-Shangase K. The occurrence of high-risk factors for hearing loss in very- low-birth-weight neonates: A retrospective exploratory study of targeted hearing screening. S Afr J Commun Disord 2012;59(1):3-7. https://doi.org/10.4102/sajcd.v59i1.16 [ Links ]
27. United Nations Department of Economic and Social Affairs 2014. Policy on Rounding of Numbers, Statistics New Zealand. https://unstats.un.org/unsd/dnss/docViewer.aspx?docID=134#start (accessed 10 April 2022). [ Links ]
 Correspondence:
Correspondence:
S Ismail
ismail.sabah12@gmail.com
Accepted 23 August 2022














