Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.17 no.3 Pretoria sep. 2023
http://dx.doi.org/10.7196/sajch.2023.v17i3.1967
RESEARCH
Hypothermia in preterm very-low-birthweight infants in a neonatal care unit of a tertiary hospital in Limpopo Province, South Africa
T S NtuliI; M P A MashegoII; M H K HameseIII
IPhD; Department of Public Health, University of Limpopo (Turfloop Campus), Sovenga, South Africa; Department of Statistics and Operations Research, Sefako Makgatho Health Sciences University, Pretoria, South Africa
IIMMed (Paed), FCPaed (SA); Department of Paediatrics, University of Limpopo, Sovenga, South Africa
IIIFCPaed (SA); Department of Paediatrics, University of Limpopo, Sovenga, South Africa
ABSTRACT
BACKGROUND: Despite numerous interventions to prevent neonatal heat loss, preventing hypothermia after delivery continues to be a concern in developing countries
OBJECTIVE: To determine the prevalence of hypothermia and its risk factors among preterm very-low-birthweight infants admitted to the neonatal care unit (NCU) of a tertiary hospital in Limpopo Province, South Africa
METHOD: A retrospective study (January - July 2015) was undertaken to analyse data from the medical records of infants admitted to the NCU of Mankweng Hospital. Hypothermia at admission was the major outcome and was defined as an axillary body temperature <36.5°C. Maternal data collected were age, parity, use of antenatal corticosteroids, and mode of delivery, while neonatal data included sex, birthweight, gestational age, Apgar score, resuscitation at delivery, admission and discharge dates, length of stay, morbidity, interventions and infant outcomes
RESULTS: A total of 252 neonate-and-mother pairs were included in the study, with hypothermia on admission being present in 35% of infants. Factors associated with hypothermia on admission include being born in the winter season, resuscitation at delivery, use of synchronised inspiratory positive airway pressure (SiPAP), respiratory distress syndrome and mortality
CONCLUSION: In our study, hypothermia on admission occurs relatively frequently, and is associated with resuscitation in the delivery room, respiratory distress syndrome, use of SiPAP, winter season and neonatal mortality. Therefore maintaining infant temperature in the desired range of 36.5°C to 37.5°C after delivery, during transport and on NCU admission might improve neonatal outcomes
Hypothermia immediately after birth remains a concern and is associated with increased morbidity and mortality worldwide, particularly in developing countries.[1,2] The World Health Organization (WHO) defines hypothermia in newborns as axillary temperature <36.5°C, and classifies it as mild (36.0 - 36.4°C), moderate (32.0 - 35.9°C) and severe (<32.0°C).[3] The WHO also recommends that neonatal body temperature be maintained at 36.5°C to 37.5°C. However, evidence has shown that there are global differences in the case definition of hypothermia and methods used to measure neonatal temperature.[1] Earlier studies have shown that an increase in heat loss among neonates is mainly due to poor thermoregulation and a large surface area to body mass ratio.[4-6] The prevalence of hypothermia among hospital-born neonates ranges from 30% to 85%,[7-10] while in those born outside of hospital it is between 10% and 90%.[1,11] The risk factors of hypothermia vary markedly within different settings, with preterm birth, very low birthweight (VLBW), transportation (within or between facilities) and seasonality (being born during the winter season) being important factors associated with neonatal hypothermia. [7,12-14]
There are numerous interventions to prevent heat loss, such as early drying and wrapping, covering the head of the newborn with a cap, skin-to-skin contact, breastfeeding, delayed bathing and weighing, appropriate clothing and bedding, and warm transportation.[1,11,15-19] Despite all these, preventing hypothermia in neonates continues to be a major challenge, particularly in developing countries.[8-10,12] In the rural tertiary hospitals of South Africa (SA), particularly in Limpopo Province (LP), there is a paucity of published research on the prevalence and risk factors associated with hypothermia among neonates admitted to neonatal care units (NCUs). Therefore, this study aimed to determine the prevalence and risk factors of hypothermia on admission among preterm VLBW neonates.
Method
Study design and setting
A retrospective descriptive study based on the review of medical records of VLBW premature neonates admitted to the NCU was undertaken at Mankweng Hospital, the only rural tertiary referral hospital in LP. The data for this study were collected for a period of 7 months from January to July 2015. There is one NCU, which is a 60-bed unit with 18 intensive care and high-care beds, a nursery with 30 beds and 12 kangaroo mother care beds. The unit has a total admission of approximately 2 000 patients per annum. A consecutive sample (n=252) of all preterm VLBW infants paired with their mothers was selected for the study.
Data collection
Data were collected using a data collection form designed for the study. The NCU register was used to identify infants admitted during the study period. Then the relevant medical records were retrieved. Using the register and patient files, the following maternal data were collected: age, parity, use of antenatal corticosteroids, HIV status, mode of delivery and maternal morbidity. Infant data included sex, birthweight, gestational age, Apgar score, resuscitation on delivery, admission date and discharge date, length of stay, morbidity and mechanical ventilation, synchronised inspiratory positive airway pressure (SiPAP), nasal continuous positive airway pressure (nCPAP), the administration of surfactant and infant outcome. In the present study, hypothermia was defined as an axillary body temperature of <36.5°C on NCU admission, while hypoglycaemia was defined as a blood glucose level of <2.6 mmol/L.
Data analysis
Statistical analyses were performed using the statistical programme Stata version 10.0 (StataCorp, USA). Characteristics of the study population were presented as mean and standard deviation (SD) for continuous variables and frequency and percentage for categorical variables. Comparisons between hypothermic and normothermic groups were performed using Student i-tests and x2/Fisher exact tests for continuous and categorical data, respectively. A p-value <0.05 was considered statistically significant.
Ethics considerations
Ethics approval to conduct the study was obtained from the University of Limpopo Ethics Committee (ref. no. TREC/84/2016: PG), and permission to conduct the study was also granted by the Limpopo Department of Health. Anonymity and confidentiality of patient personal information were protected.
Results
Demographic characteristics
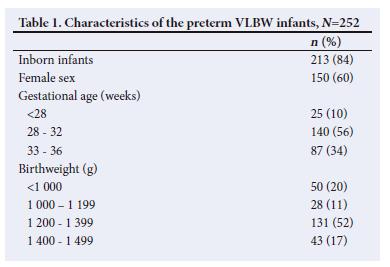
Two hundred and fifty-two preterm VLBW infants were admitted to the NCU during the study period. Of these, 84% were inborn and 16% were outborn infants. Three-quarters (76%) of outborn babies were from district hospitals, 15% born on arrival and 9% from regional and primary healthcare centres. The mean (SD) gestational age was 31.1(2.5) weeks, while the mean birthweight was 1 180.5 (206.7) g. The mean (SD) age of the mother was 26.4 (6.6) years. Table 1 shows a detailed description of the demographic profile of the study participants.
Prevalence and factors of hypothermia on admission
Hypothermia on admission was present in 89 (35; 95% confidence interval 29.2 - 41.3) of the infants admitted to the NCU. As shown in Table 2, resuscitation in the delivery rooms was performed in 13% (n=32/252) of the newborns and was more common among the hypothermic than normothermic group (21% v. 8%, p<0.05). The use of SiPAP was significantly higher in the hypothermic group as compared with the normothermic group (29% v. 18%, p<0.05). The hypothermic group was significantly more likely to have respiratory distress syndrome (46% v. 28%, p<0.05), be born in the winter season (38% v. 25%, p<0.05) and had higher neonatal mortality (33% v. 17%, p<0.05) than the normothermic group.
Infant factors such as being referred (from another healthcare facility or ward), male sex, gestational age, birthweight, 1-min Apgar score <6, season (i.e. summer and fall), length of stay in NCU, sepsis, hypoglycaemia, and intraventricular haemorrhage were not significantly associated with hypothermia on admission (p>0.05). We also observed that maternal factors, which include age, parity, caesarean section, and antenatal steroids, were not associated with hypothermia on admission.
Discussion
This study reports on the prevalence and factors associated with hypothermia on admission to the NCU among preterm VLBW neonates. Overall, 35% of the neonates arrived in the NCU with a body temperature <36.5°C. This rate is lower than the 64.8% in Malaysian NICUs,[8] 51% in Brazil,[9] 56.2% in the USA,[12] 76.8% in Taiwan,[10] and 46.1% in SA.[27] A systematic review in developing countries found that the hypothermia prevalence rate in hospital-based studies ranges from 32% to 85%, with the exception of 8% in Guinea Bissau, while in the community-based studies the rates are between 10% and 90%.[1] The wide range in the rates might be attributable to the case definition and also the differences in the method used to measure temperature.
Additionally, it could be related to the quality of care delivered by the centres.
Consistent with previous studies, our study found that hypothermia may increase mortality in preterm VLBW neonates[9,10,12,20,21] In addition, similarly to previous studies,[1,11] our findings revealed that a significantly greater proportion of hypothermia on admission occurred in the winter season. A warm delivery room, early drying and wrapping, skin-to-skin contact, breastfeeding, postponing bathing and weighing, appropriate clothing and bedding, and warm transportation could reduce the high prevalence of hypothermia.[1,11,5-19]
The WHO has recommended that delivery or resuscitation room temperatures should be kept in the range of 25°C to 28°C to prevent heat loss.[31 Although the temperature of the room to which each infant was exposed at birth was not recorded in this study, our findings showed that a higher proportion of hypothermic neonates were delivered by caesarean section and resuscitated after birth compared with their normothermic counterparts. The implementation of the standard practices based on the Neonatal Resuscitation Program guidelines on temperature control[22] has been shown to reduce the number of neonates with a low temperature at birth.[23]
Hypothermia is known to be more prevalent in preterm and low birthweight infants,[24,25] and the incidence is higher in infants with birthweight <1 500 g and at <28 weeks' gestation.[7,10] However, in our study, preterm and VLBW did not significantly affect admission hypothermia. A possible reason may be the small sample size. The transfer of neonates between different health facilities,[26] or between wards within hospitals, increases the risk of cold exposure and adverse events.[11] In our study, referred neonates were more likely to have a low admission temperature than inborn neonates; however, the results were not statistically significant.
Limitations of the study
Causality could not be established as this is a retrospective study. Moreover, as with retrospective studies, missing data from patient files affected the reliability of the data. Another limitation is that the study is based on the results from one referral centre, conducted over a short period, with a small sample size, and it is therefore not possible to generalise the results. Lastly, it was not possible to assess the severity of hypothermia, as the results on the infants' medical records were classified as categorical data (i.e. above or below 36.5°C).
Conclusion
Based on the results of this study, more than one-third (35%) of the infants were hypothermic on NCU admission, which indicates a need to closely monitor the NCU admission temperatures of preterm infants. We also observed that hypothermia on admission was associated with resuscitation in the delivery room, use of SiPAP, respiratory distress syndrome, winter season and neonatal mortality. As a result, maintaining infant temperature in the desired range of 36.5°C to 37.5°C after delivery, during transport and on NCU admission might improve neonatal outcomes, because hypothermic neonates were found to have high mortality. Further population-based investigations are also needed to look into infant transport systems, processes, and clinical care. In addition, organising helping babies breathe (HBB) workshops may assist in improving neonatal resuscitation skills, as well as training healthcare workers on measures to prevent hypothermia.
Declaration. This manuscript was submitted in partial fulfilment of the requirements for the degree of Master of Medicine.
Acknowledgments. We thank the records clerks and information officers of Mankweng Hospital for their assistance during the fieldwork.
Author contributions. TSN analysed and interpreted data and prepared the manuscript. MPA and MHK prepared the data collection instrument, collected data, interpreted data, and reviewed the manuscript. All authors read and approved the final manuscript.
Funding. None.
Conflicts of interest. None.
References
1. Lunze K, Bloom DE, Jamison DT, Hamer DH. The global burden of neonatal hypothermia: A systematic review of a major challenge for newborn survival. BMC Med 2013;11:24. https://doi.org/10.1186/1741-7015-11-24. [ Links ]
2. Onalo R. Neonatal hypothermia in sub-Saharan Africa: A review. Niger J Clin Pract 2013;16(2):129-138. https://doi.org/10.4103/1119-3077.110120. [ Links ]
3. World Health Organization. Thermal protection of the newborn: A practical guide. Geneva: World Health Organization, 1997. [ Links ]
4. Hammarlund K, Sedin G. Water evaporation and heat exchange with the environment in newborn infants. Acta Paediatr Scand Suppl 1983;305:32-35. https://doi.org/10.1111/j.1651-2227.1983.tb09856.x [ Links ]
5. Hammarlund K, Strömberg B, Sedin G. Heat loss from the skin of preterm and full-term newborn infants during the first weeks after birth. Biol Neonate 1986;50(1):1-10. https://doi.org/10.1159/000242554 [ Links ]
6. Bissinger RL, Annibale DJ. Thermoregulation in very-low-birth-weight infants during the golden hour: Results and implications. Adv Neonatal Care 2010;10(5):230-238. https://doi.org/10.1097/ANC.0b013e3181f0ae63. [ Links ]
7. Mullany LC, Katz J, Khatry SK, et al. Neonatal hypothermia and associated risk factors among newborns of southern Nepal. BMC Med 2010;8:43. https://doi.org/10.1186/1741-7015-8-43 [ Links ]
8. Boo NY, Guat-Sim Cheah I, Malaysian National Neonatal Registry. Admission hypothermia among VLBW infants in Malaysian NICUs. J Trop Pediatr 2013;59(6):447-552. https://doi.org/10.1093/tropej/fmt051. [ Links ]
9. De Almeida MF, Guinsburg R, Sancho GA, et al. Hypothermia and early neonatal mortality in preterm infants. J Pediatr 2014;164(2):271-275.e1. https://doi.org/10.1016/j.jpeds.2013.09.049. [ Links ]
10. Chang HY, Sung YH, Wang SM, et al. Short- and long-term outcomes in very low birth weight infants with admission hypothermia. PLoS ONE 2015; 10(7):e0131976. https://doi.org/10.1371/journal.pone.0131976 [ Links ]
11. Kumar V, Shearer JC, Kumar A, Darmstadt GL. Neonatal hypothermia in low resource settings: A review. J Perinatol 2009;29(6):401-412. https://doi.org/10.1038/jp.2008.233 [ Links ]
12. Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: Distribution, risk factors and outcomes. J Perinatol 2011;31(Suppl 1):S49-56. https://doi.org/10.1038/jp.2010.177. [ Links ]
13. Delavar MA, Akbarianrad Z, Mansouri MM, Yahyapour M. Neonatal hypothermia and associated risk factors at baby friendly hospital in Babol, Iran. Ann Med Health Sci Res 2014;4(Suppl 2):S99-S103. https://doi.org/10.4103/2141-9248.138022 [ Links ]
14. Salmani F, Abadi A, Taheri M, Alavi Majd H, Nayeri F. The effects of risk factors on the improvement of neonatal hypothermia using fuzzy transition. Soc Determinants Health 2016;2(1):15-20. https://doi.org/10.22037/sdh.v2i1.13710 [ Links ]
15. McCall EM, Alderdice FA, Halliday HL, Jenkins JG, Vohra S. Interventions to prevent hypothermia at birth in preterm and/or low birth weight infants. Cochrane Database Syst Rev 2008;1:CD004210. https://doi.org/10.1002/14651858.CD004210.pub3. [ Links ]
16. Lyon AJ, Freer Y. Goals and options in keeping preterm babies warm. Arch Dis Child Fetal Neonatal Ed 2011;96(1):F71-4. https://doi.org/10.1136/adc.2009.161158. [ Links ]
17. Lunze K, Hamer DH. Thermal protection of the newborn in resource-limited environments. J Perinatol 2012;32(5):317-324. https://doi.org/10.1038/jp.2012.11. [ Links ]
18. Pinheiro JM, Furdon SA, Boynton S, Dugan R, Reu-Donlon C, Jensen S. Decreasing hypothermia during delivery room stabilisation of preterm neonates. Pediatrics 2014;133:e218-226. https://doi.org/10.1542/peds.2013-1293 [ Links ]
19. Russo A, McCready M, Torres L, et al. Reducing hypothermia in preterm infants following delivery. Pediatrics 2014;133:e1055-1062. https://doi.org/10.1542/peds.2013-2544 [ Links ]
20. Jensen CF, Ebbesen F, Petersen JP, Sellmer A, Bach CC, Henriksen TB. Hypothermia at neonatal intensive care unit admission was not associated with respiratory disease or death in very preterm infants. Acta Paediatr 2017;106(12):1934-1939. https://doi.org10.1111/apa.13998. [ Links ]
21. Wilson E, Maier RF, Norman M, et al. Admission hypothermia in very preterm infants and neonatal mortality and morbidity. J Pediatr 2016;175:61-67.e4. https://doi.org/10.1016/j.jpeds.2016.04.016. [ Links ]
22. Kattwinkel J, Perlman JM, Aziz K, et al; American Heart Association. Neonatal resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 2010;126(5):e1400-e1413. [ Links ]
23. Lyu Y, Shah P, Ye XY, et al. Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks gestation. JAMA Pediatr 2015;169(4):e150277. https://doi.org/10.1001/jamapediatrics.2015.0277. [ Links ]
24. Day RL, Caliguiri L, Kamenski C, Ehrlich F. Body temperature and survival of premature infants. Pediatrics 1964;34:171-181. [ Links ]
25. Senthilkumar R, Corpuz N, Ratnavel N, et al. Adverse events during an emergency transfer of neonates performed by regionalised dedicated transfer service. Arch Dis Child 2011;96:A91. [ Links ]
26. Ashokcoomar P, Naidoo R. An analysis of inter-healthcare facility transfers of neonates within the eThekwini Health District of KwaZulu-Natal, South Africa. S Afr Med J 2016;106(5):514-518. https://doi.org/10.7196/SAMJ.2016.v106i5.8554. [ Links ]
27. Ngeny JC, Velaphi S. Hypothermia among neonates admitted to the neonatal unit at a tertiary hospital in South Africa. J Perinatol 2020;40(3):433-438. https://doi.org/10.1038/s41372-019-0539-y. [ Links ]
 Correspondence:
Correspondence:
T S Ntuli
tsntuli@hotmail.com
Accepted 8 May 2023














