Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.17 no.2 Pretoria Jun. 2023
http://dx.doi.org/10.7196/SAJCH.2023.v17i2.1932
ARTICLE
Characteristics of infants requiring mechanical reventilation in those previously ventilated during the neonatal period
W V NogayaI; P JeenaII
IMB ChB, DCH (SA), FC Paeds (SA); Department of Paediatrics, Faculty of Health Sciences, University of KwaZulu-Natal, Durban, South Africa
IIMB ChB, FCP (Paeds), Cert Paeds Pulm, PhD Department of Paediatrics and Child Health, Inkosi Albert Luthuli Central Hospital, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND. Factors predisposing ventilated neonates to the risk for reventilation during infancy are largely unknown.
OBJECTIVE. To identify factors that predispose previously mechanically ventilated neonates to reventilation.
METHODS. Mechanically ventilated infants at the Inkosi Albert Luthuli Central Hospital paedicatric intensive care unit (PICU), South Africa, who were also ventilated during the neonatal period were compared with age-, gender-, timing-, and site-matched controls who were not reventilated during infancy. Neonatal and postnatal records of the two cohorts and data on their clinical presentation and outcomes of the ICU admission were collected and analysed using descriptive and comparative statistics.
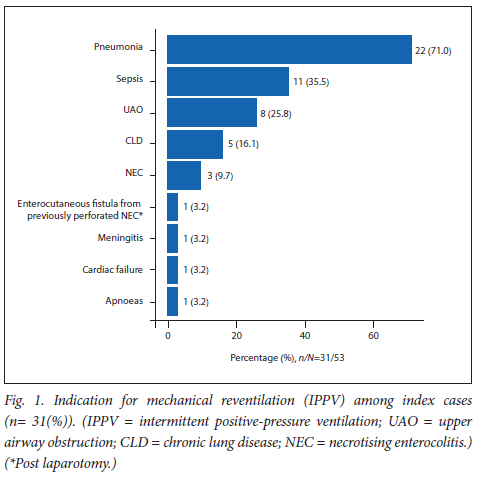
RESULTS. Thirty-one reventilated index cases were identified at the PICU over a 15-month period and were matched with 31 non-reventilated controls. Ex-preterm babies (n=26; 84%), males (n=19; 61.3%), chronic lung disease (CLD) of infancy (n=5; 16.7%) and prolonged neonatal length of stay (LOS) were common neonatal factors in reventilated neonates. Pneumonia (n=22; 71%), sepsis (n=11; 35.5%) and upper airway obstruction (UAO) (n=8; 25.8%) were common reasons for reventilation in neonates. There were no HIV-positive cases. Of the 31 reventilated cases, 5 (16.1%) demised and 15 (57.6%) survivors had morbidities, commonly seizures (n=8; 30.8%) and short bowel syndrome (n=3; 11.5%).
CONCLUSION. Pre-term birth, male, CLD of infancy and prolonged LOS were associated with an increased risk for mechanical reventilation in infancy. Pneumonia, sepsis, CLD of infancy and UAO were common indications for reventilation post neonatal ICU discharge.
Keywords:neonates; infants; risk factors; reventilation; outcomes; prevention.
With the advancement of medical technology and knowledge, an increasing number of sick and low-birthweight newborns requiring mechanical ventilation (MV) are now surviving. Unfortunately, some of these survivors require readmission to the paediatric intensive care unit (PICU) for critical illness during infancy and some demise. There is a need to identify and manage postneonatal discharge risk factors to prevent readmission in these cases. The American Academy of Paediatrics Committee on Fetus and Newborn[1] indicated that high-risk neonates require careful neonatal intensive care, preparation for discharge and good follow-up after discharge to reduce the higher risk of hospital readmission and death during the first year of life. In South Africa (SA), there are no data on these risk factors, including HIV status, persistent respiratory infections, poor growth, neurological deficits and/or surgical conditions. Strategies to optimise nutrition, use of passive and active immunisation, prevention of aspiration syndrome and timely elective surgical interventions during the recovery period post neonatal MV may reduce the need for emergency PICU admission, thereby improving outcomes.
In 2002, Elder et al.[2] identified chronic lung disease (CLD) of infancy in the post-mechanically ventilated neonate as a significant risk factor for hospital readmission. This was later confirmed in a retrospective review by Underwood et al.,[3] where recurrent RSV-associated infection in infants with CLD was associated with increased ICU admission and prolonged ICU stay.[4] In a 2014 study in the USA, Mourani et al.[5] followed up on 512 post-neonatal intensive care unit (NICU) discharges and found that 296 (57.8%) subjects were readmitted to the hospital. Approximately 1 in 5 cases (n=96) were readmitted to the PICU and 1 in 10 cases (n=61) required MV for an average of 11.6 days. Factors associated with the need for reventilation included low birthweight, male sex, prolonged neonatal MV, intracranial haemorrhage and prolonged NICU stay.[5] In 2017, Doctor et al.[6] found 9 out of 76 NICU admissions (11.9%) in Melbourne, Australia, required PICU readmission, of whom 3 (30%) required MV. Risk factors for repeated admissions included neonatal meningitis (with its sequelae) and prolonged neonatal ventilation.
There is a paucity of data on the follow-up of infants from low-and middle-income countries, especially regarding the need for reventilation with a history of MV during the neonatal period. This study aimed to describe the clinical characteristics, risk factors and outcomes of mechanical reventilation in infants who were previously ventilated in the neonatal period.
Methods
We conducted a mixed-method study involving index reventilated cases and non-reventilated controls. Index cases were identified prospectively on admission to the paediatric intensive care unit (PICU) at Inkosi Albert Luthuli Central Hospital (IALCH) in Durban, SA, over a 15-month period from 1 May 2019 to 31 July 2020. The unit serves a catchment population of 3 million children. Inclusion criteria for enrolled index cases included being mechanically ventilated infants and receiving neonatal ventilation in Area 1 government regional hospitals in KwaZulu-Natal Province (KZN), where Area 1 was defined as the coastal region between Port Shepstone and Ilembe. This geographical restriction facilitated the process of finding suitably matched controls - the researchers visited the hospitals where index cases were initially ventilated and selected matched (ventilated) neonates from the same institution. As the PICU at IALCH accepts children from all regions of KZN, as well as the neighbouring Eastern Cape Province, we restricted index cases to those who were referred from institutions situated in Area 1, thereby enabling the researchers to match control cases based on social setting too. Control cases were therefore selected based on the requirement for neonatal ventilation at the same NICU and within 3 months of the neonatal ventilation event of the index case. They were also age- and gender-matched and did not require reventilation during the follow-up period. Cases who were older than 12 months of age or where neonatal ventilation occurred outside Area 1, were excluded. Index cases were followed up using chart audits until death at the PICU or the end of the study period. Even though data on neonatal admission were captured from PICU records, the neonatal records of these cases were tracked and reviewed. Admission data and follow-up records were analysed. Electronic medical chart review of the admission or outpatient notes or telephonic interview within 12 months post NICU discharge were analysed. Neonatal controls for whom follow-up data could not be retrieved were excluded from the study.
The records of both index and control cases were reviewed to identify risk factors for readmission. Data collected included gender, birthweight, gestational age (GA), presence of neurological diseases and their sequelae, presence of surgical lesions (including congenital heart defects), presence of CLD, airway obstruction and HIV status. Risk factors for reventilation, clinical presentation, as well as outcomes (including length of intermittent positive-pressure ventilation (IPPV), length of ICU stay and survival) were analysed on the index reventilated cases. Data on their neonatal ventilator episo des were captured by retrieving their neonatal admission records. Selection of our index cases was done prospectively at a central hospital with electronic record-keeping facilities and hence data accuracy was ensured.
Ethics
This study was approved by the KZN Department of Health (ref. no. KZ-201905-007) and the Biomedical Research Ethics Board Committee (ref. no. BE 108/19).
Statistical methods
Data were captured in a Microsoft Excel (Microsoft, USA) spreadsheet and analyses were performed using SPSS software version 25 (IBM Corp., USA). A p-value <0.05 was considered significant. Categorical variables such as HIV status, age group and gender were summarised as proportions and compared using Fisher's exact test as appropriate.
Results
Two separate cohorts were enrolled in the present study. The first group were 31 prospectively enrolled index reventilated cases. A second group of 31 controls were matched for age, gender, and timing of ventilation - they were selected from the same institution as the index cases but were not reventilated during the 12-month follow-up period after initial ventilation. The controls were identified at Prince Mshiyeni Memorial Hospital, Mahatma Gandhi Memorial Hospital, King Edward VIII Hospital, RK Khan Hospital, Addington Hospital and Stanger Hospital.
Comparison of antenatal and perinatal characteristics of reventilated and non-ventilated cases during the neonatal period
A comparison between reventilated and non-reventilated characteristics during the neonatal period revealed that there were more males than females (61.3% v. 38.7%) in both groups (Table 1). Based on the GA of reventilated and non-reventilated infants, respectively, there were more early premature (GA <34 weeks; (64.5% v. 58.1%) than late preterm (GA >34 weeks; 16.1% v. 25.8%) and term (GA >37 weeks; 19.4% v. 16.1%) neonates in each group but they were almost similar in both groups (Table 1). Furthermore, there was no significant difference between reventilated and non-reventilated infants, respectively, based on birthweight (by group): extremely low birthweight (ELBW), 6.4% v. 13.3%; very low birthweight (VLBW), 25.8% v. 36.7%; low birthweight (LBW), 51.6% v. 40.0%; and term, 16.1% v. 10.0% (Table 1).
Antenatal complications, indications for neonatal ventilation and post-neonatal discharge complications were similar between the groups. There were no statistically significant differences (p=0.23) between ventilated and non-reventilated infants in terms of the median (range) duration of IPPV (4 (1 - 29) v. 3 (1 -15) days), the increased incidence of bronchopulmonary dysplasia (BPD) in the reventilated group (7.4% v. 0%) or the median duration of neonatal admission (32 v. 28 days), respectively (Table 1).
Hyaline membrane disease (HMD) (73.3% v. 64.5%), sepsis (36.6% v. 29.0%) and pneumonia (20% v. 32%) were common neonatal indications for neonatal ventilation for both reventilated and non-reventilated infants, respectively.
Post-neonatal complications including CNS diseases (41.9% (n= 13) v. 33.3% (n=10)) and retinopathy of prematurity (16.7% (n=5) v. 12.9% (n=4)) were similar in both groups. HIV exposure and non-exposure had no impact on the requirement for reventilation.
Descriptive analysis of reventilated infants in PICU
Of the 31 reventilated cases, 19 (61.3%; p=0.209) were male and 26 (83.9%; p<0.001) were ex-preterm (Table 1). Twenty-five (80.6 %) reventilated infants were younger than 6 months old with an overall male-to-female ratio of 2.1:1; the remaining 6 (19.4%) infants had a male-to-female ratio of 1:2. Although more males required admission as well as longer duration of IPPV and ICU stay, these findings were not statistically significant (p=0.209). Based on the mode of ventilation, all 31 infants received conventional (MV), while 5 (16%) required escalation to high-frequency oscillatory ventilation. There were 20 (64%) HIV-unexposed infants, 11 (36%) HIV-exposed uninfected cases and no HIV infected cases in the cohort (Table 2). Although we noted a longer duration of IPPV and ICU stay among HIV-exposed and uninfected compared with HIV-unexposed children, there was no difference in the survival rate.
Indications for mechanical reventilation included the following: multiple diagnoses in 19 (61%) infants; commonly, pneumonia with airway obstruction in 5 (26.3%); and CLD with pneumonia and disseminated sepsis in 3 (15.8%) (Fig. 1). Overall, 22 children had pneumonia (71%), 11 had sepsis (35.5%) and 8 (25.8%) had upper airway obstruction (UAO). Subglottic stenosis was the most common cause of UAO, accounting for 75% (n=6) of these patients. Aetiologies of pneumonia were identified on admission cultures. There were 22 cases of pneumonia on admission and pathogens were identified in 11 cases. There were 5 cases with a single virus identified (adenovirus, n=2; human parainfluenza (HPIV), n=1; cytomegalovirus, n=1; and influenza HINI, n=1), 3 cases with multiple viral aetiologies (adenovirus/respiratory syncytial virus (RSV), n=1; RSV/HPIV/cytomegalovirus, n=1; and cytomegalovirus/ HPIV, n=1), and one case each with mixed viral and fungal infection (Pneumocystis jirovecii pneumonia (PJP)/cytomegalovirus), PJP and pulmonary TB.
Of the 5 cases that demised (16.1%), 3 were female and 2 were male. The median IPPV duration in those who demised was 9 days - the median duration was 7 days and 11 days for females and males, respectively (p=0.170) (Table 2). Fifteen cases (48.4%) who survived had morbidities, including seizures (n=8; 30.8%) and short bowel syndrome (n=3; 11.5%).
Regarding antenatal risk factors for reventilation, 8 of the 31 (26.7%) infants had unexplained pre-term labour, 5 (16.1%) were multiple pregnancies and 4 (13.3%) had infections.
Discussion
Worldwide, there are limited data on risk factors for reventilation among infants who were mechanically ventilated during the neonatal period. In the present study HMD was the most common indication for neonatal MV, therefore more pre-term than term infants required reventilation during infancy. This finding was in agreement with those of earlier studies by Mannan et al.[7] and Kiruthika et al.[8] To the best of our knowledge, the present study was the first African study to identify the following risk factors for reventilation: ex-preterm; of male gender; having CLD of infancy; and prolonged neonatal admission of >6 weeks as possible risk factors for reventilation. These findings were similar to those of other studies where male sex, low GA and extremely low birthweight, neonatal meningitis, intraventricular hemorrhages, prolonged IPPV and length of stay, as well as BPD were identified as risk factors for hospital readmission. [5,6] Most of these studies have focused on the follow-up hospital readmission of pre-terms or very low-birthweight hospital admission follow-ups.[2,5,9] Our study was slightly different in that it included both ex-preterm and ex-term infants, assessed the presentation and outcome of readmitted PICU mechanically reventilated cases and compared risk factors between reventilated and non-reventilated infants during their first year of life.
Common indications for infants requiring PICU readmission were pneumonia, sepsis, CLD of infancy and UAO. Subglottic stenosis was the most common cause of UAO. Possible causes for this include airway trauma during intubation, size of endotracheal tubes inserted and airway care during prolonged ventilation. This suggests the need for careful skills training on the intubation technique to prevent airway trauma and measures to avoid prolonged ventilation. Regarding pneumonia, Doctor et al.[6] found that more than two-thirds of their PICU readmissions requiring MV had respiratory illness, i.e. commonly, bronchiolitis. The diagnosis of CLD of infancy was not seen in the matched control cases who were not reventilated. While it is tempting to comment that children with CLD of infancy are likely to need mechanical reventilation, we cannot make this assumption as we did not study all children with CLD of infancy. However, most studies have indicated that CLD of infancy is a common reason for infant re-hospitalisation post NICU discharge.[10-12] In a study by Rasler et al.,[9] CLD of infancy and male sex were meaningful risk predictors for hospital readmission in the first 4 years of life and later morbidity, reflecting the role of gender difference in early childhood. In the present study, more male than female infants were reventilated in the PICU post NICU discharge (p=0.209) and more of them required prolonged IPPV
We cannot comment on the role of HIV in the need for reventilation, as our sample size was small and none of the 31 reventilated cases were HIV-positive. HIV exposure, compared with HIV unexposed infants were associated with a non-statistically significant prolongation of MV (13 v. 7 days) and PICU stay (15 v. 10 days). There are currently no data on the impact of HIV status on the need for reventilation in previously ventilated neonates.
There was no significant gender difference in the reventilated cases who demised (n=5 16.1%) and all of them had a shorter IPPV duration and length of PICU stay compared with survivors. Seizures and surgical complications (short bowel syndrome, cytomegalovirus enteritis and necrotising enterocolitis strictures) were common morbidities in survivors.
Study strengths and limitations
The strength of the study was the mixed study design of reviewing reventilated cases with non-reventilated cases and selection of cases from similar populations.
Unfortunately, neonatal records of the index cases, matched controls and retrospectively retrieved follow-up data from the regional hospitals were paper-based. Consequently, missing, and incomplete records were a concern. Every effort was made to source all available retrospective data. Electronically saved discharge summaries from regional hospitals were retrieved and telephonic reviews of the mothers of enrolled patients were conducted to obtain follow-up data to the end of study period. Another concern was the small sample size which was a major limitation. The study was impacted by the COVID-19 pandemic as the PICU at IALCH was designated as a COVID-19 ICU. The increased number of COVID admissions, challenging practice of infection control measures with personal protective equipment, as well as a lack of bed capacity, contributed to premature termination of the present study after 15 months.
Conclusion
Prematurity and male sex were common predisposing factors observed in infants requiring reventilation who were previously ventilated in the neonatal period. No significant factors were identified predicting increased risk of reventilation. Pneumonia, sepsis and subglottic stenosis were the most common indications for reventilation. Most reventilated infants survived with good outcomes. Larger studies investigating risk factors for mechanical reventilation in infants are needed in SA, with further studies investigating interventions such as immunisations, nutritional support and education on measures to limit aspiration of feeds, as well as effective lung rehabilitation.
Declaration. None.
Acknowledgements. Staff and patients of IALCH and all the hospitals from which reventilated patients and controls were sourced.
Author contributions. Equal contributions.
Funding. None.
Conflicts of interest. None.
References
1. American Academy of Pediatrics Committee on Fetus and Newborn. Hospital discharge of the high-risk neonate. Am Acad Paediatr 2008;122(5):1119-1126. https://doi.org/10.1542/peds.2008-2174 [ Links ]
2. Elder DE, Hagan R, Evans SF, et al. Hospital admissions in the first year of life in very preterm infants. J Paediatr Child Health 1999;35(2):145-150. https://doi.org/10.1046/j.1440-1754.1999.00308.x [ Links ]
3. Greenough A, Cox S, Alexander J, et al. Health care utilisation of infants with chronic lung disease related to hospitalisation for RSV infection. Arch Dis Childhood 2001;85(6):463-468 https://doi.org/10.1136/adc85.6.463 [ Links ]
4. Underwood M, Danielsen B, Gilbert WM. Cost, causes and rates of rehospitalisation of preterm infants. J Perinatol 2007;27(10):614-619 https://10.1038/sj.jp.7211801 [ Links ]
5. Mourani PM, Kinsella JP, Clermont G, et al. Intensive care unit readmission during childhood after preterm birth with respiratory failure. J Pediatr 2014;164(4):749-755.e3. https://doi.org/10.1016/j.jpeds.2013.11.062 [ Links ]
6. Doctor TN, Harnaen E, Seith B, Tan K, Craig S. Risk factors for hospital readmission and follow-up after NICU discharge of infants born at extremely low gestational age in metropolitan Melbourne. Int J Pediatr Res 2017;3:028. https://doi.org/10.23937/2469-5769/1510028 [ Links ]
7. Mannan A, Jahan N, Iqbal S, et al. Short-term outcome of preterm neonates required mechanical ventilation. Chattagram Maa-O-Shishu Hosp Med Coll J 2016;15(2):9-13. https://doi.org/10.3329/cmoshmcj.v15i2.31796 [ Links ]
8. Kiruthika D, Ramesh P, Bhuvaneshwari CY, et al. Profile and outcome of neonates requiring mechanical ventilation. Medica Innov 2017;6(2):46-49. [ Links ]
9. Ralser E, Griesmaier E, Neubauer V, Gnigler M, Höck M, Kiechl-Kohlendorfer U. Readmission of preterm infants less than 32 weeks gestation into early childhood: Does gender difference still play a role? Glob Paediatr Health 2014;1(11):1-6. https://doi.org/10.1177/2333794X14549621 [ Links ]
10. Jahan N, Nasrin M, Haque ZSM, et al. Indication, and short-term outcome of mechanical ventilation in neonates in a tertiary care hospital. Bangladesh J Med Sci 2017;16(1):24-28. https://doi.org/10.3329/bjms.v16i1.31128 [ Links ]
11. Smith CV, Zupancic JA, McCormick MC, et al. Rehospitalisation in the first year of life among infants with bronchopulmonary dysplasia. J Pediatr 2004; 144(6):799-780. https://doi.org/10.1016/j.jpeds.2004.03.026 [ Links ]
12. Lamarchevadel A, Blondel B, Truffert P, et al. Re-hospitalisation in infants younger than 29 weeks' gestation in the EPIPAGE cohort. Acta Paediatr 2004; 93(10):1340-1345. https://doi.org/10.1080/08035250410032926 [ Links ]
 Correspondence:
Correspondence:
W VNogaya
vtshonaphi@yahoo.com














