Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.17 n.1 Pretoria 2023
http://dx.doi.org/10.7196/sajch.2023.v17i1.1924
RESEARCH
Clinical outcomes of intussusception: The experience in Johannesburg, South Africa
V KumaloI; A WithersII; B JugmohanIII; C Westgarth-TaylorIV; A GrieveI; D HarrisonI; J LovelandIII
IMMed (Surg); Department ofPaediatric Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIMB BCh; Department ofPaediatric Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIFCS (SA); Department ofPaediatric Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVFC Paed Surg (SA); Department ofPaediatric Surgery, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND: A previous study on intussusception from our institution demonstrated a pneumatic reduction (PR) rate of 33%, with a mortality rate of 9.1%. Numerous protocol changes were implemented, and as part of a national prospective observational study, a subsequent cohort of patients was compared with the initial series
OBJECTIVES: To compare our current series of children presenting with intussusception with our previous series. Specifically, we aimed to compare PR rates, resection rates, morbidity and mortality
METHODS: This was a retrospective review of patients aged <3 years who presented with intussusception to Chris Hani Baragwanath Academic Hospital in Johannesburg, South Africa, from 2011 to 2015 (era 2). Clinical outcomes of patients and management modalities were reviewed. These were compared with results reported in the previous article (2007 - 2010, era 1
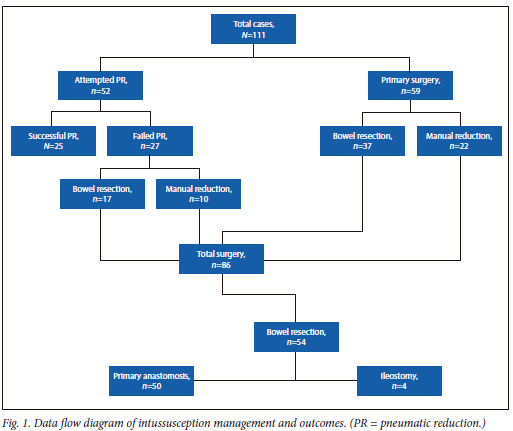
RESULTS: A total of 111 patients were included. PR was attempted in 52 patients (46.8%). It was successful in 25 patients (48.1%) and unsuccessful in 27 (51.9%), with an overall success rate of 22.5%. Eighty-six patients (77.5%) underwent surgical intervention. Bowel resection was performed in 54/86 of the surgically managed patients. No deaths were reported during the era 2 study period
CONCLUSION: Despite improved protocols, we could not demonstrate an improvement in the proportion of attempted PR cases compared with our previous series, and we did not achieve better PR rates. This failure is thought to be due to the delayed presentation of our patients, as well as an aggressive approach to management. However, this aggressive management strategy has decreased our mortality rate to zero
Intussusception is the most common cause of bowel obstruction in the paediatric population. If not promptly identified and appropriately treated, it has the potential to cause significant morbidity and mortality.[1] The worldwide incidence of intussusception is variable, and the true prevalence is difficult to calculate.[2] In 1972, Mayell[3] at Red Cross War Memorial Children's Hospital in Cape Town, South Africa (SA), demonstrated that 63% of cases occurred in infants aged <1 year. Intussusception has a male predilection, with boys affected two to eight times more frequently than girls, the reasons for which are not known.[4] The aetiology of intussusception can be classified as idiopathic or secondary to pathological causes. Idiopathic intussusception is the most common and usually occurs between 3 and 36 months of age, with only 10% of cases in this age group having an identifiable pathological cause.[5] Patients presenting outside of this age group have a higher incidence of a pathological lead point these including Meckel's diverticulum, hyperplastic lymph nodes, lymphoma, benign polyps and duplication cysts.[4]
The clinical presentation of intussusception has classically been described as a triad of intermittent colicky abdominal pain, vomiting and the passage of 'red currant jelly' stools, in which the stool contains blood and mucus.[6] This classic clinical triad is seen in <25% of patients.[7-10] In addition, a palpable right upper quadrant abdominal mass with an empty right lower quadrant may be felt on examination (Dance sign). The sequelae of untreated intussusception can potentially be devastating, putting the patient at risk of complete bowel obstruction, perforation, shock and death.[11] The aim of treatment is to reduce the intussusceptum from the intussuscipiens. This may be achieved by radiologically directed pneumatic or hydrostatic reduction, or by surgical reduction, sometimes including bowel resection.
In an initial prospective observational study performed in the Department of Paediatric Surgery at Chris Hani Baragwanath Academic Hospital (CHBAH), Johannesburg, SA, between 2007 and 2010 (era 1), a cohort of 97 patients was examined. The pneumatic reduction (PR) rate was documented to be 33.0% (n=32/97), 65 patients (68.4%) required operative reduction, and 53 (81.5%) of these patients required intestinal resection. The overall mortality rate was 9.1%. These results are markedly different from the international standard, where PR rates exceeding 90% are regularly reported as the 'standard of care'. Our initial publication postulated that delays in diagnosis and referrals and lack of structured management protocols contributed to the low PR rate.[12] After 2010, the number of paediatric surgery consultants and trainees increased, the Department of Radiology also saw an increase in its staff complement, and there was an active focus on improving the relationships between the two departments. These changes facilitated the development of a formal intussusception management protocol, including PR, with the objective of improving patient outcomes, specifically aiming to decrease mortality and improve PR rates. The objective of the present study was to compare the outcomes of our patients with intussusception in era 2 (2011 -2015) with those from era 1 (2007 - 2010).
Methods
A retrospective study of prospectively collected data on all children aged 0-36 months who presented to CHBAH with idiopathic ileocolic intussusception between January 2011 and December 2015 was performed. Demographic data collected included gender and age at presentation. Medical information included duration of symptoms (DoS), length of stay (LoS), baseline vital signs, pre-reduction imaging modality, results of baseline blood tests including inflammatory markers such as the white cell count (WCC) and C-reactive protein (CRP), and lactate and base excess values at presentation (extracted from arterial blood gas analysis). Data on treatment included whether the patient underwent PR or surgical reduction. The number of attempts made at PR and intraoperative findings for patients who underwent surgical reduction were also assessed. With regard to surgery, we documented whether the patient had manual reduction without resection, or bowel resection, or needed formation of a temporary stoma. The outcomes of surgery, such as bowel resection, anastomosis and stoma rates, were assessed, and morbidity and mortality were documented. The study was approved by the Human Research Ethics Committee of the University of the Witwatersrand (ref. no. M170437).
Data were collected and entered into Excel version 16.71 (Microsoft Corp., USA) and exported to Statistica software version 13.2.0.17 (TIBCO Software Inc., USA). Continuous variables were described using means and standard deviations if normally distributed, and medians and interquartile ranges (IQRs) if not normally distributed. Categorical variables were described using numbers and percentages. Regression analysis was used to quantify the association between determining factors and clinical outcomes. A Mann-Whitney (7-test was performed to measure differences for non-parametric continuous variables, and the X2 test was used for categorical variables. A p-value <0.05 was regarded as statistically significant. The current cohort was identified as era 2, while the previously published cohort collected between 2007 and 2010 was identified as era 1. Finally, era 1 and era 2 were compared, looking specifically at the rate of PR, rate of surgical exploration, rate of intestinal resection, ileostomy rate, and mortality.
Results
A total of 111 patients were registered on the data collection system during the defined time period, and all were included in the study. Of these, 59.5% (n=66) were male and 40.5% (n=45) female. Ninety-six patients (86.5%) were aged <10 months, and the median (IQR) age at presentation was 6 (5 - 9) months. Ultrasonography confirmed a diagnosis of intussusception in 81.1% of the patients (n=90), with only 1 patient documented as having a nondiagnostic ultrasound scan. Imaging in the remaining patients (n=20; 18.0%) was not documented. There were no deaths related to intussusception during this study period (era 2).
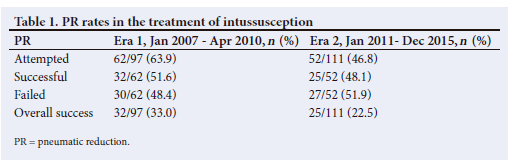
The admission CRP was recorded in 77 patients, with a range from 1 to 394 mg/L and a median (IQR) of 31 (10 - 62) mg/L. PR was attempted in 52/111 (46.8%) of the study participants. It was successful in 25/52 (48.1%) of those patients and unsuccessful in 27 (51.9%), with an overall PR success rate of 22.5% (Table 1). Of the patients who underwent PR, 24.3% (n=27/111) had repeat attempts. Of these, 1 had three unsuccessful attempts and was then taken to theatre. The remaining 26 patients all had two attempts, with successful reduction in 10 but failure in 16, who therefore went to theatre.
Primary surgical management was implemented in 59 patients (68.6%) with contraindications to PR, such as peritonitis, perforation, shock or bowel obstruction, while 27 (31.4%) required surgical exploration after failed PR. A total of 86 patients (77.5%) therefore underwent surgical exploration. The majority of patients who underwent surgery were aged <10 months (n=90/111; 81.1%). Thirty-two patients (37.2%) had manual reduction without resection. Fifty-four patients (62.8%) required bowel resection secondary to necrotic bowel. Of the patients taken primarily for surgical therapy, 62.7% (n=37/59) had bowel resection and 37.3% (n=22/59) had a manual reduction intraoperatively, whereas of the cohort taken for surgery after failed PR, 63.0% (n=17/27) had bowel resection and 37.0% (n=10/27) had manual surgical reduction. Of the total number of patients included in the study, 48.6% (n=54/111) therefore required surgical resection. The majority of the patients (n=50/54; 90.7%) underwent resection with primary anastomosis, and 4 patients (n=4/54; 7.4%) had diverting ileostomies performed; 3 of these 4 were in the primary surgical therapy group and 1 was in the failed PR group. Two of 86 patients (2.3%) required relook laparotomy. Of these patients, 1 had normal findings and the other had an anastomotic leak, which was then converted to an ileostomy.
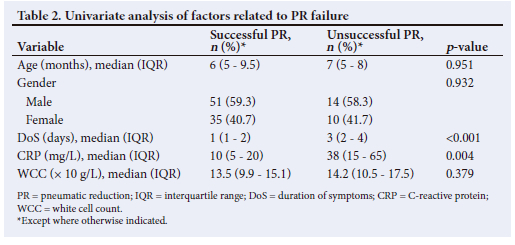
One hundred and five patients (94.6%) had a documented DoS. The DoS ranged from 1 to 14 days, with a median (IQR) of 3 (1 - 4) days. Additional analysis was undertaken to establish risk factors associated with failure of PR in this cohort of patients. Longer DoS and a high initial CRP were associated with high PR failure rates (p<0.001 and p<0.0028, respectively). Patients who had successful PR were more likely to be discharged earlier than those in whom PR failed. Age, gender and number of PR attempts had no effect on the outcome of the study (p=0.951, p=0.932 and XXXXX, respectively). The overall LoS of the study population ranged from 1 to 32 days (IQR 4 - 7). As expected, a longer LoS was noted in the group that required surgery. When PR was successful, the median (IQR) LoS was 3 (2 - 4) days, while for those with failed PR, the median was 6 (5 - 8.5) days.
Univariate analysis showed no significant difference in the outcome of PR according to the age, gender or WCC of the patients. Duration of symptoms and CRP differed significantly between patients who had successful PR and those who did not (p<0.001 and/xO.004, respectively) (Table 2). The median (IQR) DoS of patients with successful PR was 1 (1 - 2) day, while the median DoS was 3(3-4) days for those with unsuccessful PR. The median CRP in patients with successful PR was 10 (5 - 20) mg/L, in patients with unsuccessful PR it was 38 (15 -65) mg/L, and in those who went directly to theatre it was 45.5 (21 - 69) mg/L.
Discussion
Non-operative management of intussusception by means of PR has gained wide acceptance internationally. However, in low- and middle-income countries (LMICs) the spectrum of disease differs, mainly with patients presenting much later after the onset of symptoms.[13] From unpublished experience at our institution, we suspect this to be due to delayed presentation to local clinics, and delays in diagnosis and in transfer. Optimal management of this subset of patients has not been widely published and may focus on a more aggressive surgical approach. In era 1, our results demonstrated that rates of open operative reduction were high and that reductions were associated with significant morbidity, such as sheath dehiscence, anastomotic leak and abdominal compartment syndrome, and high mortality. Among the 97 patients documented, the PR rate was 33.0% (n=32/97), with a rate of open operative reduction of 67.0% (n=65/97) and a resection rate of 81.5% (n=53/65). Of note was a mortality rate of 9.1%. This high mortality rate mandated the introduction of revised management protocols aimed at the resuscitative, investigative and interventional phases of patient management. These guidelines and stricter adherence to protocols were implemented to provide the treating clinician with the ability to choose between PR and surgical exploration based on clinical parameters. In the past, surgical reduction was often performed purely because of unavailability of PR, due to lack of staff, experience or equipment.
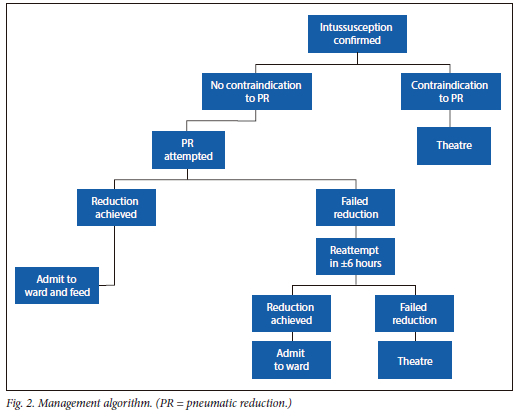
Our management strategy at CHBAH has shifted to focus on adequate resuscitation of these patients prior to any intervention, aiming for normalisation of parameters including base excess and lactate. After the initial resuscitation, the first radiological investigation, a plain abdominal radiograph, is quick and simple to perform. While it is neither specific nor sensitive in diagnosing intussusception, it may assist in the diagnosis of intestinal obstruction or perforation, which would mandate prompt surgical exploration. However, ultrasound is the diagnostic modality of choice, as it is usually easily accessible, is cheap, avoids additional radiation, and, most importantly can confirm the diagnosis in the emergency department. It has high sensitivity and specificity of 97.9% and 97.8%, respectively, and therefore helps in making the decision as to which patients will proceed to PR.[14] Our initial reduction protocol is directed towards PR in suitable candidates. Many of our patients present with established intestinal obstruction, perforation, profound shock or significant metabolic derangements. These are all contraindications to attempting PR, and patients with these clinical or biochemical features are therefore candidates for primary surgical exploration. Our current PR protocol includes a senior paediatric surgical registrar and a radiology consultant, and is performed in the radiology department. A Foley catheter is inserted into the rectum, the balloon is inflated with 20 - 30 mL of water or air, and air is insufflated at escalating pressures using a hand pump, with three cycles of 80, 100 and 120 mmHg, respectively, attempted under fluoroscopy. Each insufflation cycle lasts for 3 minutes, with a 1-minute break between each cycle, with the aim of achieving reduction of the intussusceptum using the lowest insufflation pressure possible. In era 2, these protocols may have led to a slightly reduced PR rate and a lower resection rate, but most importantly resulted in elimination of a previously high mortality rate. The overall rate of successful PR in era 2 was 22.5% (n=25/111), which is still higher than internationally reported rates; this is despite improved patient evaluation and resuscitation, and now the formalised treatment protocols and guidelines, as well as a better staff complement in both the paediatric surgery and radiology departments.
In era 2, patients with a shorter DoS had higher successful PR rates, which could explain the lower PR rates in era 2, as a longer DoS (3 days) was associated with higher PR failure rates.
It should also be noted that the proportion of patients selected for PR was much lower in era 2 compared with era 1 (46.8% v. 63.9%), which probably reflects patients presenting late, but could also reflect a more aggressive approach with a low threshold for surgical exploration over PR in era 2, both of which probably contributed to the low PR rate in era 2. We suspect that the motivation for this more aggressive approach in era 2 was the unacceptably high mortality rate in era 1, but it is important to note that this approach may have contributed to the eradication of mortality in era 2.
The male-to-female ratio of intussusception seen in this study showed a higher proportion of males (59.5% v. 40.5%). The reason for this predilection is unknown,
but it is consistent with previously published data in SA and internationally. Most of our patients were aged <10 months, with a mean age of 6 months, which correlates with a 2013 study done in SA by Venter et al.,[15] where the peak incidence of intussusception was seen in the age group <12 months. Higher admission CRP levels were associated with failed PR and the need for surgical exploration. Two previous studies have found that high CRP levels were significantly associated with worsening disease severity.[13,15] In our era 1, increased CRP levels were found to be predictors of poor clinical outcomes, specifically failure of PR (p=0.043) and the need for relook laparotomy (p=0.025). In 2001, Willetts et al[16] also reported that children with intussusception should be placed into treatment groups based on their CRP levels, as a higher CRP level was significantly associated with worse outcomes in patients treated by PR (p=0.01). Our era 2 results are comparable to the findings from era 1, where a low CRP (median (IQR) 10 (5 -20) mg/L) predicted successful PR, and a higher CRP (median 38 (15 - 65) mg/L) was predictive of unsuccessful PR.
For obvious reasons, if feasible, manual reduction is preferred over bowel resection in patients undergoing surgical exploration. The resection rates in our era 2 were lower compared with those in era 1 (48.6% (n=54/111) v. 54.6% (n=53/97), respectively), which probably reflects our more aggressive decision to proceed with surgery more often, as one perceived strategy to reduce mortality. This finding could also be attributed to better intraoperative decisions made by more experienced surgeons in era 2. It is important to note that in era 2, the resection rates for patients taken for primary surgical exploration and for those taken to surgery after failed PR were approximately equal at 62.7% (n=37/59) v. 63.0% (n=17/27), respectively. This is difficult to explain, as we would expect patients with failed reduction to have higher resection rates.
The overall stoma rate in era 2 was 4.7% (n=4/86), which is lower than in era 1, where the stoma rate was 13.8% (n=9/65). This is again probably the result of better intraoperative decisions by a more experienced surgical team as well as improved preoperative resuscitation, with both contributing to the confidence of the team to complete an anastomosis on a more stable patient. Unsurprisingly of the 4 stomas created in era 2, 3 were performed in patients who had primary surgical exploration, and only 1 was done after a failed PR.
Perhaps most importantly, in era 2 no deaths were recorded, which is in stark contrast to the mortality rate of 9.1% in era 1. This is a significant and notable improvement and is comparable to international standards. The eradication of mortality is attributed to the aggressive approach described above that was undertaken in era 2, which included a shift in focus to prioritising resuscitation before any investigation or intervention, formalisation of PR protocols and a more decisive approach to surgical intervention, which may be a result of involvement of senior paediatric surgical staff.
Conclusion
Internationally, advances in diagnosing and treating intussusception have improved outcomes in this disease. Higher CRP levels on admission have again been demonstrated to be a risk factor for poor outcomes. In the absence of contraindications, PR remains the first-line therapy for paediatric intussusception. Despite the formalised protocols in our department, we could not demonstrate an improvement in the proportion of attempted PR cases compared with our previous series, and we could not achieve better PR rates. This is mainly thought to be due to the delayed presentation of our patients. However our formalised protocols, which include aggressive resuscitation, PR technique and proceeding to surgical reduction in appropriately selected patients, have resulted in the eradication of mortality secondary to intussusception during era 2, which is extremely encouraging. Future protocols will aim to risk-stratify children based on the ranges of CRP levels and potentially manage these children along different algorithms from the onset of presentation. In addition, we need to investigate the incorporation of other biochemical parameters into the standardised treatment algorithms for intussusception in SA and other LMICs. Clinical assessment and use of point-of-care investigations remain vital in the management algorithm.
Declaration. The research for this study was done in partial fulfilment of the requirements for VK's MMed (Surgery) degree at the University of the Witwatersrand.
Acknowledgements. VK thanks all co-authors for their support.
Author contributions. VK: collection of data and writing the article as primary author. IL: initial conception, provision of data, overall supervision. BJ: advisor, proofreading, and helped draft the article. AW: statistical analysis and interpretation. AG, CW-T, DH: helped with advice on the topic, and guidance on writing the article.
Funding. None.
Conflicts of interest. None.
References
1. SklarCM,ChanE,Nasr A. Laparoscopic versus open reduction of intussusception in children: A retrospective review and meta-analysis. J Laparoendosc Adv Surg Tech2014;24(7):518-522. https://doi.org/10.1089/lap.2013.0415 [ Links ]
2. Clark AD, Hasso-Agopsowicz M, Kraus MW, et al. Update on the global epidemiology of intussusception: A systematic review of incidence rates, age distributions and case-fatality ratios among children aged <5years before the introduction of rotavirus vaccination. Int J Epidemiol 2019;4S(4):13161326. https://doi.org/10.1093/ije/dyz028 [ Links ]
3. Mayell MJ. Intussusception in infancy and childhood in Southern Africa: A review of 223 cases. Arch Dis Child 1972;47(251):20-25. https://doi.org/10.1136/adc.47.251.20 [ Links ]
4. Gluckman S, Karpelowsky J, Webster A, McGee R. (2017). Management for intussusception in children. Cochrane Database Syst Rev 2017, Issue 6. Art. No.: CD006476. https://doi.org/10.1002/14651858.CD006476.pub3 [ Links ]
5. Mar sic ove tere P, Ivatury SJ, White B, Holubar SD. Intestinal intussusception: Etiology, diagnosis, and treatment. Clin Colon Rectal Surg 2017;30( 1):30-39. https://doi.org/10.1055/s-0036-1593429 [ Links ]
6. Ntoulia A, Tharakan SJ, Reid JR, Mahboubi S. Failed intussusception reduction in children: Correlation between radiologic, surgical, and pathologic findings. AJR Am J Roentgenol 2016;207(2):424-433. https://doi.org/10.2214/AJR.15.15659 [ Links ]
7. Fallon SC, Kim ES, Naik-Mathuria BJ, Nuchtern JG, Cassady CI, Rodriguez JR. Needle decompression to avoid tension pneumoperitoneum and hemodynamic compromise after pneumatic reduction of pediatric intussusception. Pediatr Radiol 2013;43(6):662-667. https://doi.org/10.1007/s00247-012-2604-y [ Links ]
8. Mandeville K, Chien M, Willyerd F, Mandell G, Hostetler MA, Bulloch B. Intussusception: Clinical presentations and imaging characteristics. Pediatr Emerg Care 2012;28(9):842-844. https://doi.org/10.1097/PEC.0b013e318267a75e [ Links ]
9. Weihmiller SN, Buonomo C, Bachur R. Risk stratification of children being evaluated for intussusception. Pediatrics 2011;127(2):e296-e303. https://doi.org/10.1542/peds.2010-2432 [ Links ]
10. Yap Shiyi E, Ganapathy S. Intussusception in children presenting to the emergency department. Pediatr Emerg Care 2017;33(6):409-413. https://doi.org/10.1097/PEC.0000000000000548 [ Links ]
11. Ko HS, Schenk JP, Troger J, Rohrschneider WK. Current radiological management of intussusception in children. Eur Radiol 2007;17(9):2411-2421. https://doi.org/10.1007/s00330-007-0589-y [ Links ]
12. Carapinha C, Truter M, Bentley A, Welthagen A, Loveland J. Factors determining clinical outcomes in intussusception in the developing world: Experience from Johannesburg, South Africa. S Afr Med J 2016406(2):177-180. https://doi.org/10.7196/SAMJ.2016.vl06i2.9672 [ Links ]
13. Applegate K. Intussusception in children: Evidence-based diagnosis and treatment. Pediatr Radiol 2009;39(Suppl2):S140-S143. https://doi.org/10.1007/S00247-009-1178-9 [ Links ]
14. Edwards EA, Pigg N, Courtier J, Zapala MA, MacKenzie JD, Phelps AS. Intussusception: Past, present and future. Pediatr Radiol 2017^47(9):1101-1108. https://doi.org/10.1007/s00247-017-3878-x [ Links ]
15. Venter J, le Grange SM, Otto SF, Joubert G. An audit of paediatric intussusception radiological reduction at the Bloemfontein Academic Hospital Complex, Free State, South Africa. S Afr J Child Health 2013;7(2):60-64. https://doi.org/10.7196/sajch.531 [ Links ]
16. Willetts IE, Kite P, Barclay GR, et al. Endotoxin, cytokines and lipid peroxides in children with intussusception. Br J Surg 2001;88(6):878-883. https://doi.org/10.1046/J.0007-1323.2001.01799.X [ Links ]
 Correspondence:
Correspondence:
V Kumalo
vusisizwek@yahoo.com
Accepted 18 April 2022














