Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.17 no.1 Pretoria 2023
http://dx.doi.org/10.7196/SAJCH.2023.v17i1.1929
RESEARCH
Breastfeeding intentions and behaviours of doctor mothers in Bloemfontein, South Africa
C C Van der BijlI; W J SteinbergII; T E KellermanIII; J BotesIV; C van RooyenV
IMMed (Fam Med); Department of Family Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIDip Obstet (SA), MFamMed, FCFP (SA); Department of Family Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIMFamMed; Department of Family Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IVBA, MHPE; Department of Family Medicine, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
VMComm; Department of Biostatistics, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Doctor mothers are a high-risk group for early cessation of breastfeeding. Improving breastfeeding among doctor mothers would not only improve the wellbeing of their babies, but the experience might also enhance their advocacy for breastfeeding to patients
OBJECTIVE: To describe the infant feeding intentions and behaviours of doctor mothers in Bloemfontein, South Africa, focusing on breastfeeding and factors that impact the decision on feeding method
METHODS: This was a descriptive study. The target population included female medical doctors with a biological child under the age of 5 years, recruited via snowball sampling. Respondents completed an electronic questionnaire, answering questions regarding infant feeding intentions and behaviours
RESULTS: There were 104 respondents who provided information on 132 children. The median intended duration of exclusive breastfeeding for the first-born child was 6 months and 6.5 months for the second-born, but the actual median duration for both children was 3 months shorter. The intention to express breastmilk at work was 67.7% for Child 1 and 57.7% for Child 2; however, the actual outcome was less than half of the intention (32.0%). Most respondents (71.0%) indicated there was no dedicated area for expressing breastmilk at their place of work
CONCLUSION: The intention to exclusively breastfeed was high (6 months), but the actual duration was 3 months shorter. The percentage of doctor mothers who eventually expressed breastmilk at work was less than half of those who intended to do so. Breastfeeding female doctors need more support in the postpartum period, especially when returning to work after maternity leave
Keywords: Breastfeeding; employment; expressing; medical doctor; mother.
The World Health Organization (WHO) advises mothers to exclusively breastfeed their infants for the first 6 months of life to achieve optimal growth, infant development and health. Furthermore, the WHO employs breastfeeding as a strategy to improve child survival worldwide.[1] South Africa (SA) also supports this endeavour, as shown by the Tshwane Declaration for the Promotion of Breastfeeding in South Africa (2011) for the support of breastfeeding.[2] UNICEF calculated the global exclusive breastfeeding rate at 6 months at about 40%,[3] while the 2016 South Africa Demographic and Health Survey reported a rate of 31.6%.[4]
The WHO recommends complementary food to be introduced at 6 months, but in 2014 the SA National Health and Nutrition Examination Survey[5] found that the local average age for solid food introduction was 4.5 months. These feeding practices carry a high risk to the infant for malnutrition, diarrhoea and infections.[5,6]
Positive and motivating factors enabling mothers to breastfeed exclusively for 6 months include a family history of breastfeeding, the mother's determination, as well as the partner's support.[8-10] On the other hand, factors that play negative roles in breastfeeding include prenatal intention, mother's lack of knowledge, perceived difficulty to breastfeed, inappropriate advice from healthcare workers, caesarean procedures, early addition of other fluids or food and maternal employment.[8,9-13]
Maternal employment is negatively associated with exclusive breastfeeding.[12,14] In an SA study, returning to work was found to be a barrier to exclusive breastfeeding - mothers would supplement with formula milk during the day and only breastfeed at night or express at work.[8] A shorter maternity leave, lack of appropriate breastfeeding/ expressing facilities, and no daycare/childminding facilities at work, are all contributing factors.[12] A study in the UK[15] found that extended maternity leave is associated with longer breastfeeding duration. In SA, the Basic Employment Act makes provision for 4 consecutive months' maternity leave.[16] In Cape Town, a study on the factors influencing high-socioeconomic class mothers' decision regarding formula feeding found that part-time employed mothers who did not qualify for maternity leave reduced their breastfeeding duration.[7]
Mothers who intend to maintain a milk supply while away from their infants need to express breastmilk regularly. For this purpose, they require adequate time and space.[15,17,18] The Code of Good Practice on the Protection of Basic Conditions of Employment and Pregnancy in SA (1998)[19] attempted to overcome this potential barrier by insisting on two 30-minute breaks each day for expressing, which should continue for the child's first 6 months.
Anyanwu et al.[20] studied the breastfeeding behaviour ofhealthcare workers at a teaching hospital in Nigeria. They reported that doctor mothers stopped breastfeeding earlier than other healthcare workers in the same hospital and the reasons for early cessation of breastfeeding included a busy work schedule and that breastfeeding was too stressful. Healthcare workers who had negative breastfeeding experiences also displayed lower breastfeeding knowledge scores.[21] Compared with other employed females, doctor mothers are most likely to be dissatisfied with their work v. family balance, citing lack of family and private life as one of the contributing factors.[22] This demand has been deemed the 'second shift' and is a significant contributor to burnout. They feel guilty about not being able to spend adequate time with their children. Doctor mothers in academia reported less overall institutional support and reportedly had lower career satisfaction than females who were not mothers.[23]
Positive personal breastfeeding experiences among doctor mothers is a significant predictor of increased breastfeeding initiation and breastfeeding duration among their patients. Doctor mothers were more likely to promote breastfeeding actively and assist women with breastfeeding difficulties.[24,25] Rural general practitioner registrars in Australia felt that they learned more through personal experience than during their studies to become doctors.[26] In a study on breastfeeding education, treatment and referrals by female doctors in the USA, the participating doctors with personal breastfeeding experience were more comfortable in diagnosing and treating breastfeeding-related problems such as sore nipples, mastitis, infected nipples, low milk supply and latching problems.[27]
In the USA, doctor mothers' intentions to breastfeed are usually high (80 - 97%) owing to ideals of infant health, bonding, ease of feeding, cost, support system, such as family and partners, and being a role model to patients.[25,28] In contrast, the mean duration of exclusive breastfeeding among these doctor mothers was low, and 6-month continuation rates were between 15 and 21%.[25] Many doctor mothers stated that early breastfeeding cessation was due to demands at work. Other work-related reasons included returning to work after maternity leave, insufficient time and space to express breastmilk and diminishing milk supply.[24,25] Studies on breastfeeding in SA focus largely on mothers in the general population, mothers who are HIV positive and mothers from poor socioeconomic background. No current SA literature could be found on the personal breastfeeding experiences of healthcare professionals, such as doctors.
Objectives
The present study aimed to describe infant feeding intentions and behaviours of doctor mothers in Bloemfontein, SA, especially regarding breastfeeding. Additionally, the researchers attempted to identify factors playing a role in doctor mothers' infant feeding decisions.
Methods
Setting, study design, population and sampling strategy
This was an observational descriptive study conducted in Bloemfontein, SA. Bloemfontein has three private hospitals, private specialist and general practitioner (GP) practices, three public hospitals and primary healthcare clinics. The target population included doctor mothers with a minimum of a medical or equivalent degree including MB ChB, MB BCh, MBBS or any internationally recognised medical degree, working full or part-time in the government or private sector, with a biological child/children under the age of 5 completed years. The cut-off age of 5 years was selected to reduce recall bias.
According to the iRegister facility (http://isystems.hpcsa.co.za/iregister/), an estimated 900 female doctors were working in Bloemfontein at the time of this study. The sample size was determined from the probability of 100 doctor mothers with children under the age of 5 years.
To find potential respondents, the first author identified known doctor mothers with children under the age of 5 years and then used a snowball sampling via word of mouth to procure more respondents. All respondents were asked to provide an e-mail address. An email explaining the study as well as inclusion criteria was sent to all potential respondents. The email also contained a hyperlink to access the questionnaire.
Data collection
Data collection took place from May 2018 to June 2018. An electronic questionnaire, available in English only, was formulated using SurveyMonkey (Momentive Inc., USA) (https://www.surveymonkey.com/). The questionnaire consisted of six sections: (i) inclusion criteria (A); (ii) demographic data about the respondent (B); (iii) information about child/children (C); (iv) infant feeding intentions (D); (v) outcomes of the infant feeding journey (E); and (vi) open-ended questions on their opinion on breastfeeding-related matters (F). The respondents completed parts C to E of the questionnaire for each child under the age of 5 years.
Pilot study
A pilot study was done on three qualifying respondents working at a district hospital in Bloemfontein. No changes were made to the questionnaire and the data were included in the main study.
Data analysis
The closed-ended questions were automatically coded by SurveyMonkey into a Microsoft Excel spreadsheet. Open-ended questions were categorised and coded by the researcher and biostatistician. Data were analysed by the Department of Biostatistics, Faculty of Health Sciences, University of the Free State, using SAS Version 9.3 (SAS Institute Inc., USA). Results were summarised by frequencies and percentages.
Ethics
The protocol was approved by the Health Sciences Research Ethics Committee, Faculty of Health Sciences, University of the Free State (ref. no. UFS-HSD2018/0226). Implied consent was given when the respondents completed the online questionnaire. The respondents were made aware of the implied consent by the following statement at the beginning of the online questionnaire 'By completing this questionnaire, informed consent is granted for participation in this study.' No identifiable information was included in the questionnaire. All data were handled confidentially.
Results
In total, 112 doctor mothers were identified through snowball sampling and received an email as they qualified for the study. Of these, 104 completed the questionnaire (92.9% response rate). The mean age of the mothers was 34 years. The majority (84.6%) of mothers stated that they were trained on infant feeding during their undergraduate studies.
Upon return from maternity leave, 71.6% returned to the government sector and 24.5% to the private sector. The highest percentage of doctor mothers listed their professional position after maternity leave as medical officer/general practitioner (42.2%), followed by consultant/specialist (25.5%), registrar (21.6%), intern (5.9%) and community service provider (2.9%).
The 104 mothers had 132 children in total: 77 had one child; 26 had two children; and one respondent had three children. Because there was only one child reported on as the third child, data were excluded from the analysis for that child. Of the 131 children, 51.1% were female and 48.9% were male. Two-thirds (67.2%) of the children were delivered via caesarean section and 32.8% were born vaginally. Seventy-three percent of the children were breastfed within the first hour after birth, and 65.1% received skin-to-skin contact from their mother or father within the first hour after birth. Ninety-six percent of the breastfeeding mothers of Child 1 reported spousal support of breastfeeding and 100% for Child 2. Ninety-eight percent reported support from family and friends for Child 1 and 100% for Child 2.
Infant feeding intentions and eventual behaviours
Intended feeding method
For Child 1, 89.3% of mothers intended to exclusively breastfeed their children, 5.8% wanted to exclusively formula feed and 4.9% wanted to mix feed. For Child 2, 84.6% of mothers intended to exclusively breastfeed their children, 11.5% wanted to exclusively formula feed and 3.9% wanted to employ mixed feeding.
Reasons for wanting to exclusively formula feed included: convenience; having twins; previous bad experience with breastfeeding an older child; time constraints; returning to work; medical reasons, including breast cancer; or/and that the child was cared for by a caregiver in another town.
Duration of breastfeeding
Almost 45% of mothers wanted to breastfeed until their child self-weaned (44.1%). The remaining 55.9% of mothers intended to exclusively breastfeed Child 1 for a median (range) period of 6 (1 - 30) months but eventually breastfed for a median period of 3 months. For Child 2, the mothers intended to breastfeed for a median (range) period of 6.5 (4 - 18) months with an eventual outcome of a median period of 3.5 months.
The 6-month exclusive breastfeeding continuation rate was 16.7% and 18.2% for Child 1 and Child 2, respectively. Of those who were still exclusively breastfeeding at 6 months, the 12-month breastfeeding rate was 18.3% and 40.0% for Child 1 and Child 2, respectively.
Only four mothers for Child 1 and two mothers for Child 2 were still mixed feeding at the time of the study. Those who ceased breastfeeding showed a median (range) duration of 6 months (4 days - 25 months) of total breastfeeding for Child 1 and 6.5 months (range 0 - 18) months for Child 2. Half (51.5%) of the mothers initiated weaning from breastfeeding for Child 1 while 36.4% self-weaned. The remaining mothers were either still breastfeeding or did not attempt breastfeeding. For Child 2, 52.0% of the mothers initiated weaning and 28.0% self-weaned.
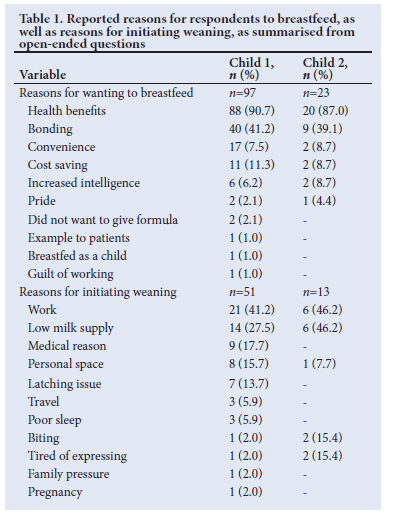
Table 1 depicts reasons given by mothers why they wanted to breastfeed as well as reasons for initiating weaning.
Formula feeding and introduction of solids
The median (range) age intended to introduce solid foods was 6 (2 - 12) months with the eventual behaviour showing a median (range) age of 5 (2 - 12) months. Only one mother for Child 1 and Child 2, respectively, had not introduced solid foods to their child yet, aged 3 months and 4 months, respectively.
For Child 1, 6.7% of mothers had never given their child a formula feed, in contrast to 11.5% for Child 2. The median age for the introduction of a formula feed was 90 days (range 0 - 420 days) for Child 1 and 25 days (range 0 - 390 days) for Child 2.
For Child 1, 25.7% of the mothers felt that they were pressured by their spouses or families to start solid foods earlier. This decreased to 8.3% for Child 2. Table 2 summarises the reasons given for the introduction of the first formula feed as well as the influencers of the mothers' decision to start solid foods.

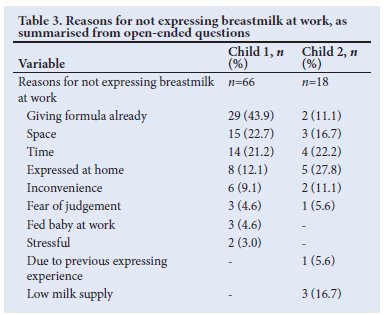
Expressing at work
Of the mothers who wanted to express breastmilk at work, 67.7% intended to express for Child 1, but only 32.0% eventually did. Of the 57.7% of mothers who intended to express breastmilk for Child 2, 28.0% did. Reasons for not expressing breastmilk at work are shown in Table 3.
The median (range) duration for expressing breastmilk for Child 1 was 5 months (range 1 week - 16 months) and for Child 2 it was 3 (1 - 9) months.
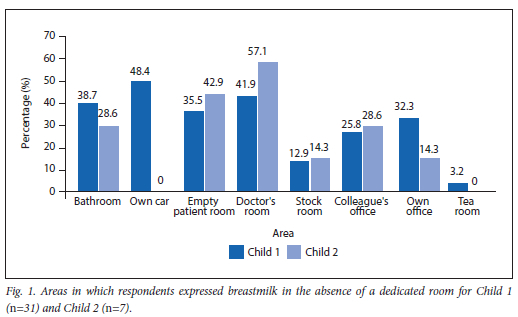
Most mothers (71%) indicated that they did not have a dedicated room at work for expressing breastmilk. Those who did not have a dedicated room, expressed in the places as shown in Fig. 1. More than a third (39.5%) of the mothers indicated that while expressing breastmilk at work, someone walked in on them.
The level of support from spouses, colleagues and employers for expressing at work is included in Table 4.
Advocacy for breastfeeding
Most mothers (73.0%) felt that their infant feeding journey had made them advocates for breastfeeding, citing reasons such as convenience, cost saving and increased bonding between mother and child, while 27% were unsuccessful in their breastfeeding journey and felt that there was too much pressure on mothers to breastfeed and that the process was emotionally and physically draining.
Factors that influence breastfeeding duration
More than half (55.0%) of the mothers felt that being a doctor influenced their breastfeeding duration, both positively, as they understood the benefits of breastfeeding, and negatively, in that there was not enough time, they were seldom at home owing to overtime, poor facilities for expressing breastmilk at work and increased anxiety and stress experienced in the profession. Those who felt it had not influenced their breastfeeding duration said that they stopped when they were comfortable, for cultural reasons, or that all working mothers have a shorter breastfeeding duration, not necessarily just doctors.
For Child 1, 93.2% of mothers took maternity leave compared with 84.0% for Child 2. For Child 1, 77.0% of mothers took maternity leave for 4 months v. 42.8% for Child 2. Only 17.7% of mothers took <4 months' maternity leave for Child 1 v. 19.0% for Child 2, while 22.9% of mothers took >4 months' maternity leave for Child 1 v. 38.0% for Child 2. Regarding more extended maternity leave, 73.0% of the mothers felt that doctor mothers needed longer maternity leave than the time their working sector allowed. They believed bonding would be better and they would be able to breastfeed for longer. They also felt that they were frequently absent owing to long working hours and that the risk for postpartum depression was higher with shorter maternity leave. Those who felt otherwise stated reasons including that doctor mothers should not get preferential treatment, they would be bored at home, and that in private practice it would not be financially viable.
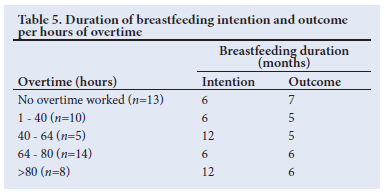
For Child 1, 25.5% of mothers did not work any overtime after returning from maternity leave; 14.2% worked >80 hours' overtime and 60.2% worked <80 hours' overtime. For Child 2, all of the mothers worked overtime after returning from maternity leave; 12.5% worked more than 80 hours' overtime and 87.5% less than 80 hours' overtime.
The intention and eventual outcome of breastfeeding duration for the different categories of overtime worked is shown in Table 5.
Most mothers (71.0%) felt that concessions regarding overtime were necessary for doctor mothers and that they would appreciate flexibility in this regard. They had difficulty expressing breastmilk at work and felt that they could not be primary caregivers if they were absent most of the time, fatigued and under increased stress. In comparison, 29.0% felt that it would be discriminatory towards men if they were allowed concessions and that it would make them better doctors if they continued with overtime.
Discussion
Doctor mothers' infant feeding behaviours have not been extensively researched in SA. Globally, however, doctor mothers have been identified as a high-risk population group with regards to early cessation of breastfeeding.[25]
The results found that a high number of respondents were trained on infant feeding during their undergraduate studies, which is commendable for SA medical schools. The number compares to a cross-sectional study done in the UK, where 85% of institutions provided compulsory breastfeeding education.[30] The intention to exclusively breastfeed among the respondents was relatively high, with a slight decrease from Child 1 (89.3%) to Child 2 (84.6%).
Reasons given by the small group of respondents who preferred exclusive formula feeding included previous formaula feeding experience or the convenience experienced with using formula previously.
Even though the caesarean section rate was quite high in the present study (67.2% v. 10 - 15% recommended by WHO), many babies were breastfed within the first 'golden' hour, and many had skin-to-skin contact soon after birth. Caesarean births are associated with poorer exclusive breastfeeding outcomes.[13] Owing to the surgical procedure, medications used during surgery, postoperative care and/or pain, breastfeeding may be initiated later.
Regarding the intention of breastfeeding duration, many respondents (44.1%) planned to breastfeed exclusively until their child self-weaned. Some mothers specified a duration (6 months for Child 1 and 6.5 months for Child 2). The increased duration for Child 2 could be attributed to breastfeeding experience with a previous child.
Respondents provided reasons for why they wanted to breastfeed exclusively, which included health benefits, convenience and cost saving. Emotional reasons, such as increased bonding, the guilt of working, pride and being an example to their patients were also listed. These reasons are consistent with studies done in SA on the general public.[8]
Unfortunately, the eventual median duration for exclusive breastfeeding was much lower (3 months for Child 1 and 3.5 months for Child 2) than intended. The 6-month exclusive breastfeeding continuation rates were lower (16.7% for Child 1 and 18.2% for Child 2) but showed similarity to results in the USA.[25]
For the mixed-fed infants, the median duration of breastfeeding of 6 months for Child 1 and 6.5 months for Child 2 -this was not very reassuring as the WHO recommends continued breastfeeding until 2 years and beyond.[1] The 12-month nonexclusive breastfeeding continuation rate reported by Sattari et al.[28] was 41%, while we found it was 18.3% and 40.0% for Child 1 and Child 2, respectively.
It is concerning that our results show some children are not even reaching the halfway goal of the WHO recommendations of breastmilk for at least 2 years.[1] The disparity in breastfeeding duration for Child 1 and Child 2 could be attributed to the mother's previous breastfeeding experience. Another possible factor could be career advancement, leading to more responsibilities and work-related stress.
Eventual behaviour (median of 5 months) of our respondents regarding the introduction of solid foods may also have played a role in the reduced time of exclusively breastfeeding. This may have lowered the exclusive 6-month breastfeeding rate in this study. More than a quarter of respondents for Child 1 felt their spouses and families pressured them to start solid foods earlier, which further decreased the 6-month exclusive breastfeeding rate.
Successful expression of breastmilk at work plays a significant role in breastfeeding duration,[12] especially for doctor mothers returning to work after maternity leave with immediate resumption of overtime shifts. This study measured a great disparity regarding intention (67.7% for Child 1 and 57.7% for Child 2) to express breastmilk and the eventual outcome (32.0% for Child 1 and 28.0% for Child 2) - the disparity may be attributed to previous negative experiences during attempts to express at work.
The early introduction of formula observed in the present study meant that most respondents' children were already on formula at the time of returning to work and it is possible that these mothers did not feel the need to express breastmilk at work. Furthermore, time and space at work were key issues among respondents. Unfortunately, not expressing during working hours could lead to decreased milk production, which invariably reduces the duration of breastfeeding.[12]
Of those who expressed at work, it is worrying to know that 71.0% of respondents did not have a dedicated room at work where they could express breastmilk and that most of them had to use other areas such as their cars, bathrooms and offices. These areas are unhygienic and offer no privacy, as evidenced by more than a third of respondents who experienced someone walking in on them while expressing. As a result of this study, the institution where the author is employed has opened up a dedicated room for mothers returning from maternity leave.
Study strengths and limitations
The method of snowball sampling was quite effective in procuring respondents for the present study. As the medical community in Bloemfontein is relatively small and many doctors know each other, saturation was reached quite rapidly, with a good response rate. The method of using an electronic questionnaire that could be completed in the respondent's own time also contributed to the high response rate.
Owing to the small sample size, clear statistically significant associations could not be made from collected data. As there is no official register of all doctor mothers in Bloemfontein, snowball sampling may have missed potential respondents, which may introduce an element of selection bias. Another limitation was geographical bias, which reduced generalisability, as only respondents currently working in Bloemfontein could participate in the study.
Owing to respondents being questioned about feeding intentions up to 5 years prior to answering the questionnaire, some recall bias may have occurred. Although most doctor mothers with children under 5 years of age were recruited, some mothers who were not successful in breastfeeding might have been less motivated to complete the questionnaire, increasing selection bias.
Conclusion
Doctor mothers in Bloemfontein are at high risk for early cessation of exclusive breastfeeding. Before birth, the intention to exclusively breastfeed was quite high, but after birth, the mean duration was 3 months shorter than planned. Less than half of those who initially intended to express breastmilk at work followed through with expressing. Doctor mothers struggle to complete the recommended breastfeeding term while also concentrating on their careers. This could be detrimental when the doctor is expected to act as an advocate for breastfeeding.
Recommendations
The present study adds to the discussion of working breastfeeding mothers, with specific reference to breastfeeding doctor mothers, who need more support in the postpartum period, and especially when returning to work after maternity leave. Below are some recommendations that would provide and improve this support to breastfeeding doctors on their return to work after maternity leave:
• Continuous breastfeeding education to doctor mothers before and after graduating, to inform them about breastfeeding issues they (or their patients) may experience.
• Improving facilities at workplaces to encourage mothers to safely express breastmilk while at work, including a dedicated private room with adequate facilities, time allocated for expressing, and supportive employers.
• Employers should be open for discussion to negotiate a working schedule ideal for the child, mother and facility.
• Limit the number of overtime hours upon returning to work after maternity leave, or at least provide the option to reduce overtime hours.
Declaration. This paper was submitted in partial fulfilment of the requirements for CVDB's MMed (Fam Med) at the University of the Free State, Bloemfontein, SA.
Acknowledgements. The authors thank all the female doctors who participated in the study, everyone who assisted with procurement of respondents, consultants in the Department of Family Medicine at the University of the Free State (UFS) for their support and assistance during the research project and Ms T Mulder (medical editor) of the Faculty of Health Sciences (UFS) for technical and editorial preparation of the manuscript.
Author contributions. CVDB conceived the study idea, developed the project protocol, conducted the research process, and prepared the manuscript for publication. WJS and TEK were study leaders, and were involved with concept development, protocol preparation, and assistance with the report and final manuscript. CVR provided advice regarding achievability of the objectives, protocol development, data analysis and final interpretation. JB assisted with the literature review, protocol and questionnaire development, report preparation and manuscript write-up. All authors read and approved the final article.
Funding. None.
Conflicts of interest. None.
References
1. World Health Assembly. Global strategy for infant and young child feeding: The optimal duration of exclusive breastfeeding. Geneva: WHA, 2001. https://apps.who.int/iris/handle/10665/78801 (accessed 15 February 2019). [ Links ]
2. Office E. The Tshwane declaration of support for breastfeeding in South Africa. S Afr J Clin Nutr 2011;24(4):214. [ Links ]
3. World Health Organization, UNICEF. Global Breastfeeding Scorecard 2018. Enabling women to breastfeed through better policies and call to action priorities. Geneva: WHO, 2018. https://www.who.int/nutrition/publications/infantfeeding/global-bf-scorecard-2018.pdf?ua=1 (accessed 15 February 2019). [ Links ]
4. National Department of Health (NDoH), Statistics South Africa (Stats SA), South African Medical Research Council (SAMRC), and Inner City Fund (ICF). South African Demographic and Health Survey 2016. Pretoria and Rockville: NDoH, Stats SA, SAMRC, and ICF. https://dhsprogram.com/pubs/pdf/FR337/FR337.pdf (accessed 12 May 2020). [ Links ]
5. Shisana O, Labadarios D, Rehle T, et al. South African National Health and Nutrition Examination Survey, 2012 (SANHANES-1). Cape Town: HSRC Press, 2014. [ Links ]
6. Victora CG, Bahl R, Barros AJ, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016;387(10017):475-490. https://doi.org/10.1016/S0140-6736(15)01024-7 [ Links ]
7. Bester M. Factors influencing high socio-economic class mothers' decision regarding formula feeding practices in the Cape Metropole. MNutr Thesis. Stellenbosch: Stellenbosch University, 2006. http://scholar.sun.ac.za/handle/10019.1/2136 (accessed 15 February 2019). [ Links ]
8. Jama NA, Wilford A, Masango Z, et al. Enablers and barriers to success among mothers planning to exclusively breastfeed for six months: A qualitative prospective cohort study in KwaZulu-Natal, South Africa. Int Breastfeed J 2017;12:43. https://doi.org/10.1186/s13006-017-0135-8 [ Links ]
9. Hector D, King L, Webb K, et al. Factors affecting breastfeeding practices: Applying a conceptual framework. NSW Public Health Bull 2005;16(3-4):52-55. https://doi.org/10.1071/nb05013 [ Links ]
10. Al-Akour NA, Okour A, Aldebes RT. Factors associated with exclusive breastfeeding practices among mothers in Syria: A cross-sectional study. Br J Med Med Res 2014;4(14):2713-2724. https://doi.org/10.9734/BJMMR/2014/8395 [ Links ]
11. Doherty T, Sanders D, Jackson D, et al. Early cessation of breastfeeding amongst women in South Africa: An area needing urgent attention to improve child health. BMC Pediatr 2012;12:105. https://doi.org/10.1186/1471-2431-12-105 [ Links ]
12. Alzaheb RA. Factors influencing exclusive breastfeeding in Tabuk, Saudi Arabia. Clin Med Insights Pediatr 2017;11:1-8. http://10.0.4.153/1179556517698136 [ Links ]
13. Prior E, Santhakumaran S, Gale C, et al. Breastfeeding after cesarean delivery: A systematic review and meta-analysis of world literature. Am J Clin Nutr 2012;95(5):1113-1135. https://doi.org/10.3945/ajcn.111.030254 [ Links ]
14. Leslie J, Powell D, Jackson J, Searle K. The relationship between maternal work patterns and infant feeding practices in Jamaican female headed households. Ecol Food Nutr 2001;40(3):215-252. https://doi.org/10.1080/03670244.200L9991651 [ Links ]
15. Hawkins SS, Griffiths LJ, Dezateux C, Law C; Millennium Cohort Study Child Health Group. The impact of maternal employment on breast-feeding duration in the UK Millennium Cohort Study. Public Health Nutr 2007;10(9):891-896. https://doi.org/10.1017/S1368980007226096 [ Links ]
16. Department of Labour, South Africa. Basic Conditions of Employment Act, 1997 (Act No. 75 of 1997). Government Gazette No. 42124, 1998. [ Links ]
17. Hirani SA, Karmaliani R. Evidence-based workplace interventions to promote breastfeeding practices among Pakistani working mothers. Women Birth 2013;26(1):10-16. https://doi.org/10.1016/j.wombi.2011.12.005 [ Links ]
18. Dabritz HA, Hinton BG, Babb J. Evaluation of lactation support in the workplace or school environment on 6-month breastfeeding outcomes in Yolo County, California. J Hum Lact 2009;25(2):182-193. https://doi.org/10.1177/0890334408328222 [ Links ]
19. Department of Labour. Basic Conditions of Employment Act, 75 of 1997. Code of good practice on the protection of employees during pregnancy after the birth of a child. Pretoria: DOL, 1998. http://www.saflii.org/za/legis/consol_reg/copotpoedpaatboac770/ (accessed 12 May 2020). [ Links ]
20. Anyanwu OU, Ezeonu TC, Ezeanosike OB, Okike CO. The practice of breastfeeding by healthcare workers in the Federal Teaching Hospital, Abakaliki, south-eastern Nigeria. S Afr J Child Health 2014;8(2):55-58. https://doi.org/10.0.28.28/SAJCH.668 [ Links ]
21. Lowe T. Breastfeeding: attitudes and knowledge of health professionals. Aust Fam Physician 1990;19(3):392-398. [ Links ]
22. Treister-Goltzman Y, Peleg R. Female physicians and the work-family conflict. Isr Med Assoc J 2016;18(5):261-266. [ Links ]
23. Bernard R. Marriage, children burnout contributors: For women physicians, having a family may mean greater stress. Contemporary OB/GYN 2017;62(5):16-18. [ Links ]
24. Sattari M, Levine D, Neal D, Serwint JR. Personal breastfeeding behavior of physician mothers is associated with their clinical breastfeeding advocacy. Breastfeed Med 2013;8(1):31-37. https://doi.org/10.1089/bfm.2011.0148 [ Links ]
25. Sattari M, Levine D, Serwint JR. Physician mothers: An unlikely high-risk group - call for action. Breastfeed Med 2010;5(1):35-39. https://doi.org/10.1089/bfm.2008.0132 [ Links ]
26. Brodribb WE, Jackson C, Fallon AB, Hegney D. Gender and personal breastfeeding experience of rural GP registrars in Australia - a qualitative study of their effect on breastfeeding attitudes and knowledge. Rural Remote Health 2007;7(3):737. [ Links ]
27. Arthur CR, Saenz R, Replogle WH. Breastfeeding education, treatment, and referrals by female physicians. J Hum Lact 2003;19(3):303-309. https://doi.org/10.1177/0890334403255643 [ Links ]
28. Sattari M, Levine D, Bertram A, Serwint JR. Breastfeeding intentions of female physicians. Breastfeed Med 2010;5(6):297-302. https://doi.org/10.1089/bfm.2009.0090 [ Links ]
29. Sattari M, Serwint JR, Neal D, Chen S, Levine DM. Work-place predictors of duration of breastfeeding among female physicians. J Pediatr 2013;163(6):1612-1617. https://doi.org/10.1016/j.jpeds.2013.07.026 [ Links ]
30. Biggs KV, Fidler KJ, Shenker NS, Brown H. Are the doctors of the future ready to support breastfeeding? A cross-sectional study in the UK. Int Breastfeed J 2020;15(1):46. https://doi.org/10.1186/s13006-020-00290-z [ Links ]
 Correspondence:
Correspondence:
C C van der Bijl
chantelle@vanderbijl.mobi
Accepted 10 December 2021














