Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.17 no.1 Pretoria 2023
http://dx.doi.org/10.7196/SAJCH.2023.v17i1.1885
RESEARCH
Crescentic glomerulonephritis in children: A retrospective review of data from Chris Hani Baragwanath Academic Hospital
S MansoorI, II; K L PetersenIII, IV; U K KalaIII, IV; P MosianeV, VI
IFCPaed (SA); Department of Paediatrics, University of the Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa
IIFCPaed (SA); Thelle Mogoerane Regional Hospital, Johannesburg, South Africa
IIICert Paed Nephrol; Department of Paediatrics, University of the Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa
IVCert Paed Nephrol; Department of Paediatrics, Chris Hani Baragwanath Academic Hospital, Soweto, South Africa
VFCPath (SA) Anat; Department of Paediatrics, University of the Witwatersrand, Faculty of Health Sciences, Johannesburg, South Africa
VIFCPath (SA) Anat; National Health Laboratory Service, Johannesburg, South Africa
ABSTRACT
BACKGROUND: Crescentic glomerulonephritis (CGN) as a cause of progressive renal failure is rare. Crescent formation on kidney biopsy represents a response to injury of the glomerular capillary walls. There are limited published reports on paediatric CGN in Africa
OBJECTIVES: To describe the clinical presentation and outcome of children with CGN in Soweto, South Africa, over a 22-year period
METHODS: A retrospective study was conducted at the Paediatric Renal Unit at Chris Hani Baragwanath Academic Hospital. Children younger than 14 years with crescent formation in more than 50% of glomeruli on renal biopsy were included in the study. Kidney biopsy specimens were examined by light microscopy, immunofluorescence and electron microscopy. Demographic and clinical data were extracted from the patient files
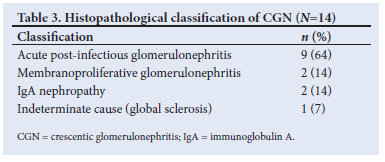
RESULTS: During the study period, 961 kidney biopsies were performed. Fourteen patients (1.5%) met inclusion criteria of crescents in >50% of glomeruli. Common clinical findings were oedema (n=13; 93%), microscopic haematuria (n=12; 86%), hypertension (n=11; 79%) and proteinuria (n=10; 71%). The median estimated glomerular filtration rate (eGFR) at presentation was 23.9 mL/min/1.73m2. Thirteen patients (93%) had immune-complex-mediated glomerulonephritis. The underlying cause was acute post-infectious glomerulonephritis in 9 patients (64%), membranoproliferative glomerulonephritis and IgA nephropathy in 2 patients each (14%) and global sclerosis in 1 patient (7%). Prolonged duration of symptoms resulted in a lower eGFR at follow-up. Treatment included peritoneal dialysis, methylprednisolone and cyclophosphamide. Seven (54%) patients had a normal eGFR at a median (range) follow-up of 36.7 (4.5 - 61.5) months. Six (46%) patients had progressed to chronic kidney disease stages 2 - 5. One patient was followed up for less than 3 months, and therefore was not included in the follow-up results
CONCLUSION: Poor outcomes were observed in patients who presented late. The clinical findings of haematuria, hypertension and acute kidney injury warrant early referral and kidney biopsy to determine management
Crescentic glomerulonephritis (CGN) is a rare condition in childhood.[1-5] Histologically, it is characterised by the presence of crescents on kidney biopsy specimens, and clinically by a sudden and progressive decline in kidney function.[3-4] This clinical entity is referred to as rapidly progressive glomerulonephritis (RPGN).[4]
Crescent formation accompanies primary glomerulonephritis or systemic disease.[3-4] It is initiated by multiple pathogenic mechanisms.[6] Crescents represent a response to injury of the glomerular capillary walls.[7] Breaks in the glomerular capillary walls cause plasma products to move into Bowman's space,[7] which causes fibrin formation, an influx of macrophages and T-cells, and the release of pro-inflammatory cytokines, such as interleukin-1 (IL-1) and tumour necrosis factor-a (TNF-a).[7]
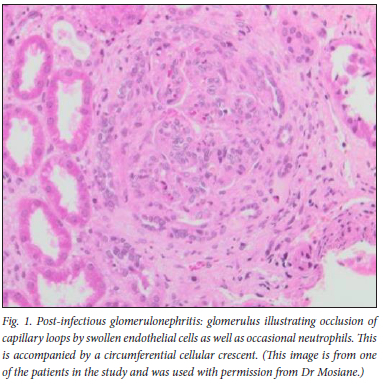
Crescents are classified as cellular, fibrocellular or fibrous according to the World Health Organization classification of glomerular disease.[3,4,8,9] Cellular crescents show a prominent proliferation of epithelial cells with a combination of macrophages and neutrophils filling Bowman's space and compressing the glomerular tuft.[4,7] Fibrocellular crescents occur when collagen fibres are present among the cells forming the crescent.[4,8] Fibrous crescents describe a lesion within Bowman's space composed predominantly of fibrous tissue.[8] Development of fibrocellular and fibrous crescents represents a disease stage that is unlikely to respond to immunosuppressive therapy.[7] The aetiologies that lead to RPGN are grouped into three main categories[6,9] based on the pattern of immunoglobulin (Ig) deposition on immune-histological examination.[6,10,11] These are: immune-complex-mediated, which include post-infectious glomerulonephritis (Fig. 1), membranoproliferative glomerulonephritis, lupus nephritis and IgA nephropathy; pauci-immune crescentic glomerulonephritis (PICGN), which is commonly attributed to anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis; and anti-glomerular basement membrane (anti-GBM) disease.[10,11]
The exact incidence of CGN is unknown; however, in various studies it has been reported to account for about 5% of renal biopsies.[5] Regarding CGN in paediatric patients, a few African studies are noted. A recent South African (SA) study found 24 cases of CGN among 430 renal biopsies (5.1%) over a 10-year period. The most common underlying pathology was immune-complex mediated disease.[12] An earlier study from SA by Parag et al.[13] reviewed adult and paediatric patients over a period of 6 years. CGN accounted for 5.9% of kidney biopsy specimens. There were 4 patients of paediatric age from 12 to 14 years old and immune-complex-mediated disease accounted for the aetiology in all patients.
In paediatric studies, similar findings were found in a study from India.[13] The study was conducted over 5 years and 22 (5.1%) of all kidney biopsy specimens were CGN. The most common aetiology was immune-complex-mediated disease. A study from Turkey[5] reviewed 45 patients with CGN over 11 years, comprising 8.5% of kidney biopsies. Immune-complex-mediated disease was the most common aetiology. A study in Germany[14] found CGN in 7.5% of kidney biopsies performed over a period of 16 years.
PICGN is emerging as a cause among children.[1] Anti-GBM disease is very rare in children. A study over 25 years showed 4 cases of anti-GBM disease.[15]
Follow-up studies indicate that renal functional impairment is a common consequence in children with CGN, with only between 13.6% and 46.2% having a normal eGFR.[1,3,4-5,12,16]
The present study serves to describe the clinical presentation, patient outcomes and responses to therapy in children with CGN in SA.
Methods
A retrospective, observational study was conducted at a tertiary hospital, situated in Soweto, Johannesburg, SA. This is the largest hospital in the southern hemisphere, serving a population of 1.27 million people.[17]
The study period was between 1 January 1990 and 30 June 2012 in children up to 14 years of age. Patients were included in the study if the results of their kidney biopsy showed crescents involving >50% of their glomeruli.[2-5,8,12] Kidney biopsies were done if a patient had haematuria, hypertension and elevated serum creatinine levels. Histopathological examination was done by light microscopy, immunofluorescence and electron microscopy. CGN was identified from an in-house registry of kidney biopsies done at our hospital.
Clinical data were extracted from patient record files. Kidney biopsy results were reported by pathologists from the National Health Laboratory Service (NHLS). The kidney biopsy results are reviewed at monthly histopathology meetings. Follow-up is defined as the last documented follow-up visit to the hospital as of 30 June 2012. Blood tests were performed based on the clinical suspicion of underlying kidney pathology causing CGN. The results are reported using the STROBE guidelines.[18]
Continuous variables were represented by a median, range and interquartile range (IQR). Analysis of outcome was performed by linear regression models. One patient whose follow-up was only for 3 months was excluded from the outcome analyses. Statistical analysis was performed using the statistical software STATA version 14.2 (SPSS Inc., USA). A p-value <0.05 was considered as statistically significant.
Ethics
Ethical approval was obtained from the Human Research Ethics Committee at the University of the Witwatersrand (ref.no. M190289).
Results
A total of 961 renal biopsies were performed during the study period. Although 78 (8.1%) of these biopsies had some crescent formation, only 14 (1.5%) had crescents in >50% of glomeruli and were included in the study. All patient files could be retrieved; however, records were incomplete in 6 files. The median (range; IQR) age at presentation was 123 (49 - 164, 81.5 - 144.5) months. Table 1 summarises the demographics, presenting features and clinical findings of the 14 patients with CGN included in the study. Six (67%) patients with acute post-infectious glomerulonephritis (APIGN) had decreased complement (C3) levels and 5 (56%) patients had elevated antistreptolysin O (ASO) titres. No patients had anti-nuclear antibodies (ANA). Anti-GBM antibodies were not tested for.
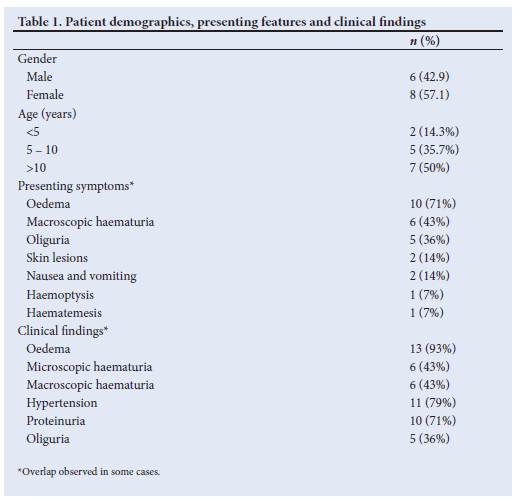
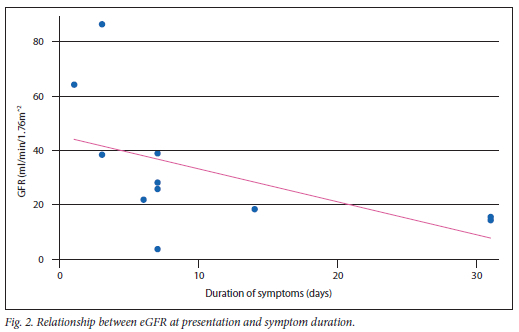
The duration of symptoms was unknown for 2 patients (14%). The median (range; IQR) duration of symptoms was 6 (1 - 7; 3 - 7) days for the patients with normal renal function at their last follow-up visit, compared with 22 (7 - 30; 10.5 - 30.0) days for patients with chronic kidney disease (CKD) at their last hospital visit. The mean (standard deviation (SD)) number of days of symptoms was significantly higher (p=0.0067) in patients with CKD (20.25 (11.62)) days compared with those with normal renal function (4.86 (2.47)).
A regression model was created to ascertain if there was a relationship between eGFR at presentation and the duration of symptoms. There was a non-significant inverse relationship between the two variables (B = -0.53; p=0.093) (Fig. 2).
Thirteen patients presented with acute kidney injury (AKI), which was defined as an increase in serum creatinine by >26.5 μmol/L within 48 hours or an increase in serum creatinine > 1.5 times baseline, which was known or presumed to have occurred within the past 7 days.[19] One patient was referred after 3 months of symptoms and was classified as having CKD. This patient was excluded from the outcome analysis.
The median (range; IQR) eGFRs at presentation and the last hospital visit were 23.9 (3.3 - 86.4; 9.2 - 49.1) and 89.7 (3.8 - 175; 12.7 - 140.4) mL/min/1.73m2, respectively. The median (range; IQR) duration of hospital stay was 38.5 (20 - 121; 22.5 - 53) days.
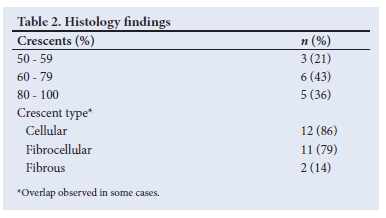
Kidney biopsies were performed after a median (range; IQR) of 12 (2 - 34; 7 - 19) days following hospital admission. Thirteen (93%) specimens had data on the number of glomeruli seen on light microscopy of kidney biopsies. The median (range; IQR) number of glomeruli was 26 (5 - 100; 19.0 - 46.5). Biopsies were performed prior to commencing treatment in 11 (79%) patients. Kidney biopsy findings are summarised in Table 2. Appendix 1 (https://www.samedical.org/file/1955) summarises the demographics, pathology findings, treatment and outcomes of patients with CGN. Patients with fibrocellular and cellular crescents had an eGFR recovery >50mL/min/1.73m2, while patients with fibrous crescents had improvements of at least 30 mL/min/1.73m2.
Treatment
The median (range; IQR) duration from the onset of symptoms to the commencement of specific therapy was 19.5 (8 - 42; 10.5 - 33.5) days. The median (range; IQR) duration from the time of presentation to treatment was 10 (0 - 35; 2.0 - 17.5) days. One patient was treated with methylprednisolone, 2 patients (14%) were treated with cyclophosphamide, and 9 patients were treated with both agents. Three doses of methylprednisolone were given at 10 - 30 mg/kg/dose. Oral prednisone followed the doses of methylprednisolone and were given at 2 mg/kg/dose for 4 weeks, after which the dose was tapered off. Cyclophosphamide was given at 500 mg/m2 intravenously monthly for 3 to 6 months. The treatment for 1 (7%) patient was unknown.
Six patients required renal replacement therapy with continuous ambulatory peritoneal dialysis (CAPD). The median (range; IQR) duration of dialysis was 28 (8 - 116; 11.5 - 77.5) days. Of these 6 patients, 1 (17%) patient died, 1 patient was well, and the remaining 4 patients did not return for scheduled follow-up visitations. Peritoneal dialysis was stopped in all but one patient who later demised.
Outcomes
The median (range; IQR) duration of follow-up was 12.2 (1.1 - 72.3; 4.7 - 54.7) months. The median (range; IQR) age at follow-up was 128 (54 - 208; 105.5 - 178.0) months. One patient had a follow-up of less than 3 months and was excluded from the analysis.
At the last follow-up visit, 7 (54%) patients had normal kidney function. These patients were followed-up for a median (range; IQR) period of 36 (4 - 61; 10 - 55) months. Six (46%) patients had progressed to CKD: 1 (8%) patient had CKD stage 2; 1 (8%) had CKD stage 4; and 4 (31%) patients had CKD stage 5.
The median (range; IQR) eGFR was 89.7 (3.8 - 175; 12.7 - 140.4) mL/min/1.73m2. A total of 9 patients were hypertensive at their last follow-up visit and were on anti-hypertensive treatment.
Two patients died. The first patient was a female (aged 13 years 6 months) with an eGFR at presentation of 3.7 mL/min/1.73m2. She died 7 months after her first presentation, with her kidney biopsy showing global sclerosis. The second patient presented at age 4 years 10 months. Her eGFR at presentation was 15.6 mL/min/1.73m2. She died 6 years after diagnosis while on CAPD. Her kidney biopsy showed post-infectious glomerulonephritis.
Eight (62%) patients did not return for scheduled follow-up visits. Of these patients, 4 patients had normal renal function, 1 patient had CKD stage 1, 1 patient had CKD stage 4, and 2 patients had CKD stage 5. These patients had follow-up visits for a median duration of 11.2 months.
Discussion
CGN is uncommon in children, and accounts for 5% of renal biopsies.[5] The present study spanned 22 years and demonstrated that only 1.5% of all paediatric kidney biopsies had crescent formation involving >50% of glomeruli. This difference may be due to the inclusion criteria in this study which included patients younger than 14 years of age, while other studies included patients younger than 18 years of age.[1,3-5,13,21] CGN may not have been recognised or patients with symptoms may not have been referred owing to a paucity of paediatric nephrologists in SA.[20] The percentage of crescent formation used to diagnose CGN differs between studies, therefore the incidence of CGN varies with the location and local policies on the indications for kidney biopsy.[21]
The median age at presentation was 123 months. This was similar to other reports.[1,4,5,8,12] There were 2 (14.3%) patients under the age of 5 years. CGN in patients under the age of 4 years is unusual.[7] This may be attributed to immature immune responses in young children.
The most common clinical findings were haematuria and hypertension, which was similar to findings in other studies.[4,7,16] These signs ought to be specifically sought at the bedside. Serum creatinine levels should be monitored in a patient with haematuria and hypertension. In patients with AKI, rapidly progressing glomerulonephritis needs to be diagnosed. A kidney biopsy should be performed to confirm CGN.
Oliguria was not a common feature in patients in the present study. Oliguria for >24 hours should be considered stage 3 in AKI[19] and distinguishes RPGN from acute glomerulonephritis.[16] Five (36%) patients presented with this complaint, compared with between 50% and 86% in other studies.[1,3] This could be attributed to the study being retrospective with poor documentation of symptoms, or patients presenting early.
Histological confirmation by kidney biopsy should be performed as soon as possible. Where kidney biopsy is not possible owing to patient or resource factors, treatment should not be delayed secondary to a delay in histological confirmation. The progression of cellular to fibrous crescents takes 2 weeks.[6] Thus there is a short window of opportunity to prevent permanent damage.
Cellular crescents indicate that the lesions are in the early stages of formation and that patients presented early. Fibrous crescents are associated with a poor outcome[4,8] and give an indication of the chronicity of the disease.
We have documented that cellular and fibrocellular crescents occur most commonly in patients seen at this centre and these crescent types have a better outcome in terms of GFR recovery.[3,5,7]
Ninety-three percent of patients in this study had an immune-mediated cause for CGN, and most of the literature had similar results.'3-5,8,12,161 The most common cause of CGN in the present study was APIGN (64%). In India, Dewan et al.[3] reported 86% of cases had immune-complex-mediated CGN and, of these, 50% of cases also had post-infectious glomerulonephritis. In China
and Macedonia, the high prevalence of CGN was attributed to the prevalence of infection with nephritogenic strains of group A Streptococcus.[2] In contrast, in Saudi Arabia, lupus nephritis was found in 54.1% of cases,[22] which is attributed to a high prevalence of lupus nephritis among Saudi Arabian patients with SLE. PICGN was a common cause of CGN in 52.8% of patients in another paediatric study,[1] where the authors postulated that this could be a result of a changing aetiological profile, or more severe cases being referred, resulting in a higher proportion of patients with PICGN.[1] Primary diseases that develop into CGN show regional variation.[21] PICGN has been reported in higher-income countries,[1] lupus nephritis has been reported in Saudi Arabia[22] and post-infectious CGN in middle- and lower-income countries.[3,5,12]
The finding of normal eGFRs in 54% of patients after a 36-month follow-up period in the present study should be interpreted with caution. Long-term studies may show different results, since patients with AKI are at risk of CKD.[23] This compares with other reports of normal eGFR in 13.3% to 46.7%[1,3-5,12] of patients with a follow-up between 8.1 and 34.0 months.[1,3-4,12]
A higher initial eGFR correlating well with a higher final eGFR may be attributed to early diagnosis and initiation of treatment. A few days' delay in diagnosis and treatment may have a negative impact on outcome owing to the rapidly progressive loss of kidney function.[6]
The good recovery in eGFR reported here could be attributed to most of our patients presenting within a week of symptom onset, and most crescents still being in the early phase of development.
Study limitations
As this was a retrospective study, patient records were not complete. The study population was very small, and a larger data set would allow for more robust statistical analyses. This may be difficult as CGN is an uncommon disease. Multicentre collaboration is needed. In addition, long-term outcomes are hampered by non-adherence of patients to scheduled appointments related to socioeconomic factors of a mobile population and lack of funds for transport to healthcare facilities.[24] Children with normal kidney function who are not on chronic medication may feel well and show no symptoms, thus parents may not appreciate the need for continued follow-up.
Despite the limitations, the results of the present study document APIGN as the most common cause of CGN and report a favourable short-term outcome in those who are treated early, as evidenced by cellular crescents on kidney biopsy.
A national database would assist in the recognition and management of this disease. After reporting their results of a national survey on RPGN in Japan, Koyama et al.[25] found that recognition of the disease improved in general practice.
Conclusion
In the present study, symptoms patients presented with were indicative of glomerulonephritis and the associated renal failure raised suspicion for CGN. Indicators of a better outcome are cellular and fibrocellular crescents. Earlier presentation was associated with a higher eGFR at follow-up.
A national database would assist in the recognition and management of this disease. Raising awareness for early diagnosis improves outcomes in patients with CGN as this is a disease in which renal function deteriorates rapidly. Simple bedside tests such as blood pressure monitoring and urine dipstick tests can alert the clinician to the need for serum creatinine measurement. Referral to a renal centre is recommended when RPGN is diagnosed.
Declaration. This manuscript was completed in partial fulfilment of SM's MMed (Paediatrics) at the University of the Witwatersrand.
Acknowledgements. Morelearnings Sibanda for help with the statistics.
Author contributions. SM: conception of research question, data collection and analysis, manuscript preparation and revision; KLP and UKK: conception of research question, manuscript revision and approval of final manuscript; PM: data collection, manuscript revision.
Funding. None.
Conflicts of interest. None.
References
1. Sinha A, Puri K, Hari P, Dinda A, Bagga A. Etiology and outcome of crescentic glomerulonephritis. Indian Pediatrics 2013;50(3):283-288. https://doi.org/10.1007/s13312-013-0095-z [ Links ]
2. Gupta R, Singh L, Sharma A, Bagga A, Agarwal SK, Dinda AK. Crescentic glomerulonephritis: A clinical and histomorphological analysis of 46 cases. Indian J Pathol Microbiol 2011;54(3):497-500. https://doi.org/10.4103/0377-4929.85081 [ Links ]
3. Dewan D, Gulati S, Sharma RK, et al. Clinical spectrum and outcome of crescentic glomerulonephritis in children in developing countries. Pediatr Nephrol 2008;23(3):389-394. https://doi.org/10.1007/s00467-007-0647-3 [ Links ]
4. Jardim HMPF, Leake J, Risdon RA, Barratt TM, Dillon MJ. Crescentic glomerulonephritis in children. Pediatr Nephrol 1992;6(3):231-235. https://doi.org/10.1007/bf00878354 [ Links ]
5. Özlü SG, Çaltik A, Aydog Ö, et al. Crescentic glomerulonephritis in children: A single-centre experience. World J Pediatr 2016;12(2):225-230. https://doi.org/10.1007/s12519-015-0036-0 [ Links ]
6. Jennette JC. Rapidly progressive crescentic glomerulonephritis. Kidney Int 2003;63(3):1164-1177. https://doi.org/10.1046/j.1523-1755.2003.00843.x [ Links ]
7. Mahmoud MA, Hassan AA. A clinicopathologic study of proliferative glomerulonephritis with crescents in children: A review of 21 cases. Kidney Forum 2000;2(1):37-42 [ Links ]
8. Southwest Pediatric Nephrology Study Group. A clinic-pathologic study of crescentic glomerulonephritis in 50 children. Kidney Int 1985;27(2):450-458. https://doi.org/10.1038/ki.1985.30 [ Links ]
9. World Health Organization. Renal disease: Classification and Atlas of Glomerular Disease. Tokyo: Igaku-Shoin Medical Publishers, 1981:3-9. https://doi.org/10.7326/0003-4819-97-5-801_2 [ Links ]
10. Greenhall HB, Salama AD. What is new in the management of rapidly progressive glomerulonephritis? Clin Kidney J 2015;8(2):143-150. https://doi.org/10.1093/ckj/sfv008 [ Links ]
11. Mejia-Vilet JM, Parikh SV. Overview of the current approach to glomerular disease classification. Glomerulonephritis 2017, 1-28. https://doi.org/10.1007/978-3-319-27334-1_5-1 [ Links ]
12. Mwaba C, Nourse P, Pillay K, Gajjar P. Aetiology and outcomes of crescentic glomerulonephritis in South African children: A ten-year folder review. Afr J Paed Nephrol 2020;7(1):15-21. [ Links ]
13. Mayer U, Schmitz J, Brásen JH, et al. Crescentic glomerulonephritis in children. Pediatr Nephrol 202;35(5):829-842. https://doi.org/10.1007/s00467-019-04436-y [ Links ]
14. Parag KB, Naran AD, Seedat YK, Nathoo BC, Naiker IP, Naicker S. Profile of crescentic glomerulonephritis in Natal - a clinical-pathological assessment. Quart J Med 1988;68(2):629-636. https://doi.org/10.1093/oxfordjournals.qjmed.a068230 [ Links ]
15. Williamson SR, Phillips CL, Andreoli SP, Nailescu C. A 25-year experience with pediatric anti-glomerular basement membrane disease. Pediatr Nephrol 2011;26(1):85-91. https://doi.org/10.1007/s00467-010-1663-2 [ Links ]
16. Cunningham RJ, Gilfoil M, Cavallo T, et al. Rapidly progressive glomerulonephritis in children: A report of thirteen cases and a review of the literature. Pediatr Res 1980;14(2):128-132. https://doi.org/10.1203/00006450-198002000-00012 [ Links ]
17. Statistics South Africa. Census 2011. Pretoria: StatsSA, 2011. http://www.statssa.gov.za/?page_id=4286&id=11317 (accessed 14 January 2019). [ Links ]
18. Von Elm E, Altman DG, Egger M, Pocock SJ, G0tzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Epidemiology 2007;18(6):800-804. https://doi.org/10.1097/ede.0b013e3181577654 [ Links ]
19. KDIGO guideline. https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2012-AKI-Guideline-English.pdf (accessed 14 January 2019). [ Links ]
20. Kumashie DD, Tiwari R, Hassen M, Chikte UME, Davids MR. Trends in the nephrologist workforce in South Africa (2002 - 2017) and forecasting for 2030. PLoS ONE 2021;16(8):e0255903.00 https://doi.org/10.1371/journal.pone.0255903 [ Links ]
21. Choudhury TA, Singh RG, Usha, et al. Clinicopathologic spectrum of crescentic glomerulonephritis: A hospital-based study. Saudi J Kidney Dis Transpl 2014;25(3):689-696. https://doi.org/10.4103/1319-2442.132241 [ Links ]
22. Alsaad K, Oudah N, Al Ameer A, Fakeeh K, Al Jomaih A, Al Sayyari A. Glomerulonephritis with crescents in children: Etiology and predictors of renal outcome. ISRN Pediatr 2011;3:507298. https://doi.org/10.5402/2011/507298 [ Links ]
23. Kamath N, Iyengar A, George N, Luyckx V. Risk factors and rate of progression of CKD in children. Kidney Int Rep 2019;4(10):1472-1477. https://doi.org/10.1016/j.ekir.2019.06.004 [ Links ]
24. Kala U. Pediatric Nephrology in South Africa: International Pediatric Nephrology Association IPNA Currents (2020). https://theipna.org/wp-content/uploads/2023/01/IPNA-Current-_PN-in-South-Africa.pdf (accessed 9 January 2023). [ Links ]
25. Koyama A, Yamagata K, Makino H, et al. A nationwide survey of rapidly progressive glomerulonephritis in Japan: Etiology, prognosis and treatment diversity. Clin Exp Nephrol 2009;13(6):633-650. https://doi.org/10.1007/s10157-009-0201-7 [ Links ]
 Correspondence:
Correspondence:
S Mansoor
sajeda.m@gmail.com
Accepted 15 November 2021














