Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.16 no.4 Pretoria Dez. 2022
http://dx.doi.org/10.7196/SAJCH.2022.v16i4.1910
RESEARCH
Food provision in early childhood development centres in Harare, Zimbabwe
A LewisI; Y SmitI; M MaraisI; D G NelII
IMNutr; Division of Human Nutrition, Faculty of Medicine and Health Sciences, University of Stellenbosch, Cape Town, South Africa
IIDSc; Division of Human Nutrition, Faculty of Medicine and Health Sciences, University of Stellenbosch, Cape Town, South Africa
ABSTRACT
BACKGROUND. Poor nutrition practices result in malnutrition, a public health concern that affects a third of children globally. In Zimbabwe, ~27.6% of children under-5 years old are stunted. Some of these children spend long hours in early childhood development centres (ECDCs). Children can receive half to two-thirds of their daily food intake while in care, making ECDCs an ideal entry point to influence child nutrition positively. There are no specific nutrition guidelines for ECDCs in Zimbabwe.
OBJECTIVE. The study aimed to investigate food provision at ECDCs of the Northern-Central District of Harare.
METHODS. A descriptive, cross-sectional study with an analytical component was conducted in 15 ECDCs. Fifteen ECD managers (ECDMs) and 14 food handlers (FHs) were included in the study. An observational checklist allowed recording of food preparation and hygiene practices. The Dietary Diversity Score (DDS) of the menu was calculated using the Food and Agriculture Organisation (FAO) 9-group DDS sheet.
RESULTS. Inadequate food storage facilities and food handling practices were observed. Staff had minimal nutrition-related training. Staff displayed a positive attitude towards their role in providing healthy meals. Barriers to serving healthy meals were inadequate funds, children's food preferences, unrealistic parental expectations, and external factors. The mean DDS score for menus was 2.8. Meals consisted mainly of starchy items, legumes and meat, and lacked fruit and dairy items.
CONCLUSION. National guidelines can improve children's dietary intake while in day care. In alignment with Sustainable Development Goals 2 and 3, food provision at ECDCs should be a priority.
Optimal nutritional status is achieved when there is access to affordable, diverse and nutritious food, appropriate care practices, and good hygiene.[1] Poor dietary intake leads to malnutrition, a health problem that severely affects vulnerable groups such as infants and children. Globally, nearly half of all deaths in children under-5 are attributable to malnutrition.[2] Africa is the second-most-affected country after Asia, and malnutrition statistics in sub-Saharan Africa showed a pooled prevalence of 39% stunting, 27% wasting and 25% overweight.[3] Factors contributing to malnutrition in Zimbabwe include insufficient dietary knowledge among mothers and ECD caregivers; incoherent nutrition interventions; and limited execution of appropriate hygiene and sanitation practices.[4] The high micronutrient needs of young children necessitate dietary diversity and high nutrient density of meals to meet individual requirements,[5-yet dietary diversity assessment shows that Zimbabwean households consume an average of five out of 12 foods groups, with a highest average of seven; and the most common consumed foods are cereals, while meat, dairy, pulses and eggs are the least consumed.[6]
Zimbabwe has experienced an increase in the number of privately owned early childhood development centres (ECDCs) over the past several years.[7] These are often home-based businesses operated by individuals who convert part of their home to learning facilities, and are preferred by parents for their close proximity and more affordable fees.[7] Some facilities are unsuitable for ECDCs[8] and fail to meet operational licensing requirements owing to poor infrastructure or insufficient funds to obtain a licence, forcing them to operate unlicensed.[7]
In addition to structural and operational requirements, ECD regulations (Statutory Instrument (SI) 106 of 2005) instruct ECDCs to provide one meal and a snack to children in full-day care.[9] Details about the quality and quantity of the food provided are, however, lacking. Additionally, the country does not have national Food-Based Dietary Guidelines (FBDGs) to guide meals provided for the children. As the country battles malnutrition and more children are cared for in ECDCs, it is important to examine nutrition and hygiene practices in these centres. Of equal importance is identifying barriers to optimal nutrition in ECDCs through understanding the nutrition-related challenges faced by ECD caregivers, and perceptions of their role in providing adequate nutrition for children.
There is a paucity of data on the nutritional issues and challenges faced by caregivers in ECDCs in Zimbabwe, as only one study was identified that focused on nutrition in privately owned ECDCs.[8] Similarly, food and nutrition requirements in early childhood are largely overlooked, and in practice they are only considered in cases where the child has cultural or medical reasons for variations in diet.[10] Results from the present study can inform evidence-based planning for nutrition interventions such as the design of comprehensive nutrition guidelines for ECDCs and as baseline information to inform further research in ECD nutrition interventions.
The objectives of this study were to observe food-handling practices; determine the Dietary Diversity Score (DDS) of food served in ECDCs; investigate perceptions of caregivers regarding their role of food provision within ECDCs; and to identify barriers encountered in providing food to children.
Ethics approval was obtained from the Health Research Ethics Committee of the University and the Medical Research Council of Zimbabwe (ref. no. MRCZ/B71512). The Ministry of Primary and Secondary Education (MoPSE) gave authorisation to conduct the research in ECDCs.
Methods
The descriptive, cross-sectional study was conducted at full-day care ECDCs preparing and serving food to a minimum of six children. Census sampling was done in all licensed and unlicensed ECDCs (N=52) listed in the Northern-Central District. Fifteen ECDCs consented to take part in the study. The ECD manager (ECDM) and one food handler (FH) per centre were conveniently sampled.
Data were gathered by the researcher during a 1-day visit of 5 to 7 hours in each ECDC. Quantitative data were obtained through two interviewer-administered questionnaires: one for ECDMs and the other for FHs. As Zimbabwe lacks detailed nutrition guidelines and FBDGs, no relevant official document in Zimbabwe known to the researcher was identified for assessment of nutrition and food handling practices in ECDCs; therefore questionnaires were based on the South African Operational Manual for the Provision of Food in Care Facilities for Young Children[8] that include various aspects specific to FHs in ECDCs and which aligned with the study objectives, as well as other literature for questions relating to barriers to nutrition provision and perceptions of ECDC caregivers.[11-13] Both questionnaires consisted of open- and closed-ended questions and collected data relating to demographics, training and perceptions towards serving healthy meals. Questions on a safe working environment and fire safety were excluded as these were beyond the scope of the research. Additionally, the ECDM questionnaire included open-ended and multiple-choice questions investigating barriers experienced in providing healthy meals within the ECDC. The FH questionnaire included an observational section that captured information about practices of FHs relating to the storage and handling of food as well as preparing meals and serving of meals.
The menu of the ECD was obtained on the day of the visit. The nine-group dietary diversity score (DDS) sheet compiled by the Food and Agriculture Organisation (FAO)[14] was used to determine the DDS of the menu, by calculating the total food groups represented on the menu. In addition, the actual menu prepared on the day of the visit was recorded by the researcher. Only food that amounted to a portion size of one tablespoon or more was recorded on the DDS sheet.[15] The nine-group DDS was used as it puts more emphasis on micronutrient content of food eaten.
A pilot study was conducted at one ECDC to evaluate the process of data collection and assess the face validity of the open-ended questions. Feedback obtained during the pilot study was incorporated in the final data-collection process and tools. Minor changes were made to improve understanding of two vague questions relating to nutrition perceptions. Data collection was conducted by one researcher.
Content validity was not conducted as the questionnaires were designed from a standard tool used in SA ECDCs, and all questions were relevant to Zimbabwean practices. The DDS is a validated tool widely used in research studies to measure nutritional adequacy.[1]
Data analysis
STATISTICA Version 13.1 (Dell Inc., 2017) was used for data analyses. Contingency tables and likelihood ratio chi-square tests were used to analyse the relationship between nominal variables. A p-value <0.05 represented statistically significant differences.
Participants' responses to open-ended questions were thematically analysed by the researcher. Comments and responses were read several times and coded to determine main themes that were used for interpretation of data.
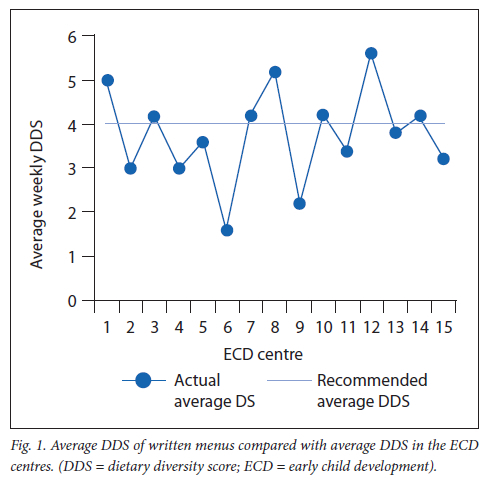
The DDS for each ECDC was calculated and interpreted using DDS=4 as the cut-off value and best indicator for micronutrient adequacy. A DDS <3 indicated low dietary diversity, indicating likelihood of stunting.[15]
Results
Demographic information
The study population comprised 15 ECDMs and 14 FHs who were selected from 15 ECDCs. In one centre, the ECDM fulfilled a dual role as ECM and FH, resulting in 29 participants (15 ECDMs, 14 FHs).
Table 1 provides a summary of the demographics of the study participants. The ECDM questionnaire investigated ECDMs' awareness of SI 106 of 2005, which instructs ECDCs to provide food for children in full-day care and provides structural and hygiene requirements for ECDCs. Results showed that 53.33% (n=8) of the ECDMs (3 licensed ECDCs, 20%; 5 unlicensed ECDCs, 33.3%) were aware of these regulations. Furthermore, less than half (n=6, 40%) of ECDMs reported having policies in place to guide food and nutrition issues within their centres, although these could not be verified as no written documents were presented during the one-day visit. Many ECDMs described their menu instead of the ECD policy when asked about the latter.
Food-handling practices
One ECDC withheld permission to observe food preparation and cleaning in the kitchen facility; therefore, only some observations of practices were recorded at 14 centres. Table 2 provides a summary of the food-handling practices of FHs. Kitchen facilities were generally clean and pests were observed in only two ECDCs (14.3%). Most FHs (n=12, 80%) practised handwashing with soap prior to handling food, and food was served immediately after being dished up. No statistically significant difference was observed between food-handling practices in licensed and unlicensed centres (p<0.05).
A third (n=5, 35.7%) of FHs were observed to wash and rinse utensils between handling of different food items, and 21.4% (n=3) between raw and cooked food. Washing and rinsing was done using water at room temperature, and none of the FHs sanitised their utensils. The majority of FHs used dishcloths, and less than half of the FHs (n=6, 42.9%) practised air drying of utensils. Compliance with regard to wearing of suitable clothing such as aprons, hair restraints and closed shoes was uncommon among FHs. Many FHs had aprons, but infrequent use of hair restraints and closed shoes was observed. Few ECDCs had functional cold storage facilities and relied on daily purchasing of perishables.
Menu plans and DDS
Almost all ECDCs (n=14, 93.3%) displayed their menus. Low compliance with planned menus was observed, and 73.3% (n=11) of the ECDCs partially adhered to their menus; accordingly, their meals were either omitted or substituted with a food on the menu.
DDS was calculated for the written (displayed menus) and the actual menu served. The average DDS for actual meals served was 2.8, ranging between DDS 2 to DDS 5 (SD 0.86). The DDS was significantly lower (p=0.045) in unlicensed (DDS=2.4) than licensed ECD centres (DDS=3.3). The most served foods were starchy foods (n=15, 100%), followed by meat and meat products (n=8, 53.3%) and legumes and nuts (n=6, 40%), respectively.
More than half (n=8, 53.3%) of the ECDCs failed to achieve the minimum DDS of four, based on their written menus. Organ meat and eggs were not included in planned menus; however, eggs were substituted for meat in one ECDC on the day it was visited. Dairy and fruits were lacking in planned ECD menus and consequently in children's meals. The serving of vegetables was observed in only nine ECDCs and, if served, the portion did not meet the required serving of at least a tablespoon to be accounted for in the DDS. Fig. 1 depicts the average DDS of 4 for written menus in the ECDCs.
Perceptions on food provision in ECDCs
ECDC caregivers expressed positive perceptions of the importance of their role in ensuring nutritionally adequate food in ECDCs and the mutually important role of parents in ensuring children receive adequate food. The majority of participants (n=23, 79.3%) also agreed, and strongly agreed with their need for further nutrition training. While many participants either agreed or strongly agreed that educating children in food and nutrition was important (n=26, 90%), many ECDC caregivers disagreed with the need to involve children in meal planning for the centres (n=14, 48%). Table 3 provides a summary of the responses related to perceptions.
ECDMs were asked to narrate some of the challenges they faced in providing healthy food for children in ECDCs. Responses to open-ended questions revealed four main themes: finances, children's acceptance of food, parents' expectations, and external factors. Limited finances resulting from the hyperinflationary economic environment and erratic fees payment by parents affected food procurement in most ECDCs. Many ECDMs raised concerns of introducing varied foods for fear of resentment of unfamiliar tastes as well as potential incompatible religious beliefs which limit food acceptance. Of equal importance was ECDMs' need to ensure they displayed and served more familiar and flamboyant menus which appeal to parents seeking to enrol their children in the ECDC. Lastly, external factors such as cost and availability of healthier food, availability of electricity and fuel for cooking, and foodborne disease outbreaks, affected food procurement in ECDCs. Table 4 provides a summary of the themes and quotations as illustrations.
ECDMs were provided with a list of potential barriers and asked to list them in order of importance. The most important barrier was child food acceptance (n=10, 66.7%), followed by the cost of ingredients (n=9, 60%). These are presented in Fig. 2.
Discussion
The purpose of the study was to investigate dietary diversity of food provided in ECDCs and the challenges in providing food for children. Nearly a third of children in Harare are stunted[16] and some spend long hours in ECDCs where they are fed at least two-thirds of their daily food intake.[17] The ECD policy of Zimbabwe (SI 106 of 2005) provides regulations for establishing and managing ECDCs.[9] Although it covers infrastructure and teacher requirements in detail, the nutrition component is vague, stipulating only the provision of one meal and a snack for children, without an integral strategy outlining its implementation.[18] Key steps towards reducing malnutrition in Zimbabwe could include providing specific food and nutrition mandates, and guidelines stemming from the recommendation to provide food in ECDCs.[19]
Multiple interlinked factors contribute to malnutrition in Zimbabwe. One underlying cause is insufficient knowledge of ECD caregivers and ill-practices regarding children's diets.'41 Nutrition education among ECDC caregivers in the present study was lacking, while the sources of education varied from professional qualifications to brief workshops and past experiences. According to the ECDC regulations, there is no clear requirement on staff qualifications, yet the teacher training course offered by colleges is standard for recruiting teachers and includes food and nutrition courses. However, because this is not for FHs, and targets teachers or ECDMs, there is a need for training specific to FHs; their role requires knowledge of appropriate cooking methods and food hygiene, but they reported less nutrition-specific and food-hygiene training compared with ECDMs. Poor nutrition knowledge was also exhibited by the majority of ECDMs who described their menus instead of nutrition policies. This aspect raises concerns of potential disregard of other factors affecting food provision, such as nutritional adequacy; the eating environment and role of ECDC caregivers; special dietary considerations; and regulation of food brought from home.[19,20] Nutrition is a vital component of early childhood development that equally requires an overarching policy and consideration to support full cognitive and social development.[21] Therefore, the government, through the Ministry of Primary and Secondary Education (MoPSE), should stipulate minimum qualifications for ECDC caregivers and facilitate pre-service and in-service tailor-made training targeting ECDMs and FHs to improve nutrition care in ECD centres. Revision of the current ECD teacher training curricula to include greater emphasis on nutrition, hygiene and sanitation may help to cultivate a nutrition-sensitive environment for children in ECDCs.[8]
Low DDS observed in menu plans and actual meals alike, also reflects poor nutrition knowledge among ECDC caregivers. Observation of meals was limited to a single day of the present study; however, using the actual food served proved to be more accurate for calculating the actual DDS than using the displayed menus, and resulted in low average DDSs of 3.3 and 2.4 for licensed and unlicensed centres, respectively. DDS was affected by insufficient portion sizes of less than one tablespoon and inconsistency between menu plans and actual food served as a result of substitution or omission of dishes. These results are consistent with similar studies that have conducted observations ranging from a single day to several months, which found that matching foods and beverages to written menus varied from only 50% - 87%,[22,23] or even less in the ECD centres. Failure to adhere to displayed menus usually resulted in lower dietary diversity, as FHs who already reported low nutrition education were less likely to use nutritionally adequate alternative dishes, while omitted foods were mostly vegetables and fruits. Furthermore, this inconsistency in planned and prepared food potentially deceives parents trying to complement household meals with ECDC meals, based on the displayed menus. Guidelines for affordable and nutritionally appropriate substitution of ingredients as well as standard menus, recipes and portion sizes are essential to support FHs.
Research studies in ECDCs have reported children's dietary intake to consist of more starchy foods and fewer fruits and vegetables, thus negatively affecting dietary variety. Furthermore, a nutrition survey in Zimbabwe reported that household diets consist of more starch and vegetables, and inadequate weekly consumption of other foods such as dairy, meat and fruits.[6]Therefore, it is also unlikely that a DDS below 4 at the ECDCs will improve with added home meals, as many households lack the food groups, namely dairy, and a variety of vegetables and fruits that comprise important sources of micronutrients.[6]
A healthy environment and good hygiene are also important in child development. In this study, food-handling practices observed by the lack of cold storage facilities and inconsistency in wearing protective gear by FHs indicated potential for foodborne disease. Similarly, failure by FHs to sanitise utensils potentially could cause cross-contamination and spread of disease. Therefore, providing and enforcing food safety recommendations in kitchen facilities is crucial.[17,20]
ECDMs and FHs expressed satisfaction with the food served within their centres; however, four main barriers that hinder adequate food provision were identified by ECDMs. Finances and child acceptance of food ranked high on the list, and this was consistent with other studies.[24-26] Financial challenges resulted in food and nutrition receiving lower priority among the numerous competing needs in ECDCs, yet being a key factor in child development. Some studies have found that establishing vegatable gardens is beneficial in reducing food expenses in ECDCs. Additionally, vegetable gardens have helped increase the intake of fruits and vegetables that children would otherwise scorn, as they form a vital component of food and nutrition education.[20] Child acceptance of food was another challenge that prohibited ECDMs from introducing alternative food that could prove to be more affordable yet nutritious. Food and nutrition education for FHs in methods to improve acceptance of nutritious food by children, such as social influence affecting food intake, attractive presentation, and repeated exposure to less popular albeit healthy options, may yield positive results. The ECD curricula include nutrition topics; however, engagement of ECDC caregivers during mealtimes and including children in more practical nutrition activities could improve their food intake. The provision of government subsidies and social grants for ECDC children from low-income households has been shown to improve dietary diversity.[25,26]
Study limitations
Owing to the small sample size, the results of the study cannot be generalised to other populations and should be interpreted with caution. Observations were only made on one specific day and might not be a true reflection of meals served. Portion sizes, food wastage, nutrient adequacy and children's food preferences were not investigated in this study. Future research studies can investigate nutritional adequacy of the diet by doing nutritional analysis and costing of menus. Lastly, engaging parents or policymakers such as the MoPSE is also recommended to gain better understanding of policies and practices.
Conclusion
Results of the study reflect the need for government to enact a policy that enforces mandatory and comprehensive ECDC caregiver training in food hygiene and food preparation. Through interministerial and multi-stakeholder co-ordination and collaboration, Zimbabwean context-specific national ECDC policy supported by clear institutional mandates and responsibilities in ECDC meals has the potential to promote favourable nutrition outcomes by ensuring that children's nutritional requirements are met. These should provide guidelines on foods to be provided; permissible and/or impermissible food or drink; procurement methods; and also elaborating on average energy and nutrient requirements per child. Promoting local food and onsite vegetable gardens as well as providing alternative menus to suit different ECDC incomes is important in ensuring sustainability of ECDC nutrition. The MoPSE should promote impartial dissemination of policy and guidelines to all ECDCs irrespective of registration status, as this would promote equality of healthy nutrition and hygiene practices across all children in ECDCs. Additionally, the MoPSE ECDC registration requirements should be revised to accommodate ECDCs in low-income neighbourhoods which have limited resources such as space and income, by adopting requirements that encourage optimal care for children and are feasible in such environments. Having more registered ECDCs will allow equitable rollout of interventions to support children from low-income households by government or non-government subsidies in Zimbabwe. Subsidies have been identified to improve nutrition provision in ECDCs and encourage ECDC registration.
Further research including children's diets outside ECDC centres will provide a better understanding of their overall diet and help to identify areas needing improvement to lower malnutrition rates in Zimbabwe. Including MoPSE staff and parents will also add depth to the challenges and opportunities to improve child nutrition at policy and household levels.
Having a policy and guidelines alone is insufficient; therefore, providing mandatory and comprehensive ECDC caregiver training is necessary to ensure meaningful contributions towards reducing malnutrition in Zimbabwe.
Declaration. Except where stated otherwise by reference or acknowledgement, the work presented is entirely that of the authors.
Acknowledgements. The United States Agency for International Development (USAID) funded the Nutrition Assessment, Counseling, and Support Capacity Building Project (NACSCAP) under the Capable Partners Program from 2012 to 2018 to strengthen the South African government's capacity to deliver a comprehensive set of nutrition interventions and integrate nutrition assessment, counseling and support (NACS) as a standard-of-care approach into government systems (national, provincial, district, NGOs). The programme was made possible with the generous support of the American people. The program was managed by FHI 360. The Early Childhood Development (ECD) audit tool was developed by FHI 360 technical staff with the provincial government of the Western Cape to audit food provisions at ECD centres. FHI 360 extends permission for portions of the audit tool to be used in pursuit of research. Thanks are given to Dr Hilary Goeiman, Director - Nutrition, Western Cape Province, for her collaboration in the development of this tool during NACSCAP implementation. The contents are the responsibility of FHI 360 and do not necessarily reflect the views of the USAID or the United States Government.
Author contributions. YS: conceptualisation of research idea, design, interpretation and manuscript input. MM: contributed to research design and manuscript revision. AL: contributed to research design, conducted data collection, contributed to data analysis , interpretation and manuscript writing. DN: statistical analysis.
Funding. None.
Conflicts of interest. None.
References
1. Kennedy GL. Evaluation of dietary diversity scores for assessment of micronutrient intake and food security in developing countries (doctoral thesis). Wageningnen: University of Wageningen; 2009. https://library.wur.nl/WebQuery/wurpubs/fulltext/14551#page=43 (accessed 27 November 2018). [ Links ]
2. UNICEF (United Nations Children's Emergency Fund). Malnutrition. New York, NY: UNICEF; 2018. http://data.unicef.org/topic/nutrition/malnutrition/# (accessed 28 June 2018). [ Links ]
3. UNICEF (United Nations Children's Emergency Fund), WHO (World Health Organization), World Bank. Levels and Trends in Child Malnutrition; 2018. http://www.who.int/nutgrowthdb/2018-jme-brochure.pdf?ua=1 (accessed 26 October 2018). [ Links ]
4. Ministry of Health and Child Care Zimbabwe, Food and Nutrition Council. Zimbabwe National Nutrition Strategy 2014-2018; 2014. https://extranet.who.int/nutrition/gina/sites/default/filesstore/ZWE%202014%20National%20 Nutrition%20Strategy.pdf (accessed 27 June 2018). [ Links ]
5. Fanzo J. The Nutrition Challenge in Sub-Saharan Africa. United Nations Development Programme. Working Paper 2012-012; 2012. https://www.undp.org/content/dam/rba/docs/Working Papers/Nutrition Challenge.pdf (accessed 18 May 2021). [ Links ]
6. Food and Nutrition Council. Zimbabwe national nutrition survey 2018. https://www.unicef.org/zimbabwe/media/1056/file/Zimbabwe2018NationalNutritionSurveyReport.pdf (accessed 14 November 2018). [ Links ]
7. Mujuru L. Zimbabwe mandates preschool, but untrained teachers and unlicensed schools abound. Glob Press J. 18 May 2018. https://globalpressjournal.com/africa/zimbabwe/zimbabwe-mandates-preschool-untrained-teachers-unlicensed-schools-abound/ (accessed 18 May 2021). [ Links ]
8. Mangwaya E, Blignaut S, Pillay SK. The readiness of schools in Zimbabwe for the implementation of early childhood education. S Afr J Educ 2016;36(1): 8. https://doi.org/10.15700/saje.v36n1a792 [ Links ]
9. Government of Zimbabwe. Ministry of Education, Sport, Arts and Culture. Statutory Instrument 106 of 2005. Harare: Government Printers; 2005. [ Links ]
10. Robson SM, Khoury JC, Kalkwarf HJ, Copeland K. Dietary intake of children attending full-time child care: What are they eating away from the child-care center? J Acad Nutr Diet 2015;115(9):1472-1478. https://doi.org/10.1016/j.jand.2015.02.029 [ Links ]
11. McSweeney LA, Rapley T, Summerbell CD, Haighton CA, Adamson AJ. Perceptions of nursery staff and parent views of healthy eating promotion in preschool settings: An exploratory qualitative study. BMC Public Health 2016: 841. https://doi.org/10.1186%2Fs12889-016-3507-x [ Links ]
12. Seward K, Finch M, Yoong SL, et al. Factors that influence the implementation of dietary guidelines regarding food provision in centre based childcare services: A systematic review. Prev Med 2017;105:197-205. https://doi.org/10.1016/j.ypmed.2017.09.024 [ Links ]
13. Grady A, Seward K, Finch M, et al. Barriers and enablers to implementation of dietary guidelines in early childhood education centers in Australia: Application of the theoretical domains framework. J Nutr Educ Behav 2018;50(3):229-237. https://doi.org/10.1016/j.jneb.2017.09.023 [ Links ]
14. Kennedy G, Ballard T, Dop M. Guidelines for measuring household and individual dietary diversity. 2013. http://www.fao.org/fileadmin/user_upload/wa_workshop/docs/FAO-guidelines-dietary-diversity2011.pdf1 (accessed 2 August 2018). [ Links ]
15. Steyn NP, Nel J, Labadarios D, Maunder EMW, Kruger HS. Which dietary diversity indicator is best to assess micronutrient adequacy in children 1 to 9 y? Nutrition 2014;30(1):55-60. https://doi.org/10.1016/j.nut.2013.06.002 [ Links ]
16. Maradzika J, Makwara IP, Chipunza S. Factors associated with stunting among children aged 0 to 59 months in Harare City, Zimbabwe. Int J Child Health Nutr 2016;5(1):31-44. [ Links ]
17. Benjamin-Neelon SE. Position of the Academyof Nutrition and Dietetics: Benchmarks for nutrition in child care. J Acad Nutr Diet 2018;118(7):1291-1300. https://doi.org/10.1016/j.jand.2018.05.001 [ Links ]
18. Ecker O, Nene M. Nutrition policies in developing countries: Challenges and highlights. Policy Note, October 2012. Washington, DC: International Food Policy Research Institute; 2012. [ Links ]
19. Dent C, Matwiejczy L, Fenton J, Kennett L, Mastersson N, McWhinnie JA. Guidelines for Food and Nutrition Policy in Child Care Centres. Adelaide: SA Child Care Nutrition Partnership; 2005. http://qappd.com/wp-content/uploads/2021/01/food_nutrition_policy_guidelines.pdf (accessed 5 September 2018). [ Links ]
20. Regional Overview of National School Food and Nutrition Programmes in Africa. Accra: Food and Agriculture Organization (FAO); 2018. [ Links ]
21. United Nations Children's Emergency Fund (UNICEF). Early Childhood Development. https://docplayer.net/15966001-Early-childhood-development-the-key-to-a-full-and-productive-life.html (accessed 26 April, 2018). [ Links ]
22. United Nations System Standing Committee on Nutrition. Schools as a System to Improve Nutrition: A New Statement for School-Based Food and Nutrition Interventions. Discussion Paper, September 2017. Geneva: UNSCN; 2021. https://www.unscn.org/uploads/web/news/document/School-Paper-EN-WEB.pdf (accessed 18 May 2021). [ Links ]
23. Breck A, Dixon LB, Khan LK. Comparison of planned menus and centre characteristics with foods and beverages served in New York City child-care centres. Public Health Nutr 2016;19(15):2752-2759. https://doi.org/10.1017/S1368980016000720 [ Links ]
24. Benjamin Neelon SE, Copeland KA, Ball SC, Bradley L, Ward DS. Comparison of menus to actual foods and beverages served in North Carolina child-care centers. J Am Diet Assoc 2010;110(12):1890-1895. https://doi.org/10.1016/j.jada.2010.09.012 [ Links ]
25. Dev DA, Garcia AS, Dzewaltowski DA, et al. Provider reported implementation of nutrition-related practices in childcare centers and family childcare homes in rural and urban Nebraska. Prev Med Reports 2019;17:101021.https://doi.org/10.1016/j.pmedr.2019.101021 [ Links ]
26. Zaltz DA, Pate RR, O'Neill JR, Neelon B, Benjamin-Neelon SE. Barriers and facilitators to compliance with a state healthy eating policy in early care and education centers. Child Obes 2018;14(6):349-357 https://doi.org/10.1089/chi.2018.0077 [ Links ]
27. Thorogood CR. Food provision challenges facing early childhood development centres in two Cape Town townships. (Master's thesis.) University of the Western Cape; 2020. http://hdl.handle.net/11394/8238 (accessed 27 July 2021). [ Links ]
 Correspondence:
Correspondence:
A Lewis
agnesmlewis@gmail.com
Accepted 5 October 2021














