Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.16 no.4 Pretoria Dez. 2022
http://dx.doi.org/10.7196/SAJCH.2022.v16.i4.1808
RESEARCH
Sociodemographic factors associated with mixed-feeding practices among a cohort of mothers with infants aged 4 - 14 weeks in Tlokwe subdistrict, North West Province, South Africa
N M SemenekaneI; C B WittenII, III; E SwanepoelIV;H S KrugerII
IMSc (Nutrition); Centre of Excellence for Nutrition, North-West University, Potchefstroom, South Africa
IIPhD (Nutrition); Centre of Excellence for Nutrition, North-West University, Potchefstroom, South Africa
IIIPhD (Nutrition); Division of Health Professions Education, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IVMSc (Dietetics); School of Physiology, Nutrition and Consumer Sciences, North-West University, Potchefstroom, South Africa
ABSTRACT
BACKGROUND. Exclusive breastfeeding for the first 6 months of an infant's life is the recommended gold standard for infant feeding; however, mixed feeding (MF) is common in various settings. In South Africa (SA), especially in the Tlokwe subdistrict of North West Province, there is little information on the association between sociodemographic factors and infant MF practices.
OBJECTIVE. To identify the sociodemographic factors associated with MF practices in a cohort of mothers of infants aged 4 - 14 weeks in the Tlokwe subdistrict of North West.
METHODS. The study setting was 8 health facilities in the Tlokwe subdistrict. Participants comprised postpartum women with infants aged 4 - 14 weeks. Data analysis used SPSS version 25.0. Normal data are presented as means (standard deviation (SD)), skewed data as median values (25th, 75th percentiles) and categorical values as percentages and frequencies. Chi-square tests and logistic regression analysed the association between sociodemographic factors and MF practices at time point 2 (10 - 14 weeks).
RESULTS. The majority of the mothers were aged between 25 and 29 years, and 37% had at least 2 live children. MF increased with infant age. There was no significant association between any of the sociodemographic variables and MF practices. Logistic regression analysis showed a significant association between increased parity and MF. There was also a significant association between changes in infant-feeding practices after receiving the child support grant at 10 - 14 weeks.
CONCLUSION. The high proportion of mothers who mixed-fed indicates that it is still the norm, as in other SA contexts. Therefore, strengthened breastfeeding education regarding appropriate infant-feeding choices in the promotion of infant development and survival for the short and long term should be emphasised.
The evidence documented in the 2016 Lancet series on breastfeeding (BF) has without a doubt proven that it is very beneficial, contributing to a smarter, healthier and more thriving future for the world.[1] BF has short- and long-term benefits, including reduced morbidity caused by infectious and respiratory diseases in childhood, and a diminished risk of childhood obesity[2,3] and diabetes.[4,5] In spite of these well-established advantages, global exclusive BF (EBF) rates remain far below target.[1]
The World Health Organization (WHO) recommends that globally, infants should be exclusively breastfed for the first 6 months of life, continuing with appropriate, adequate and safe complementary foods from age 6 months to 2 years or beyond.[6]
The most recent South Africa Demographic and Health Survey (SADHS) showed that 36.1% of mothers exclusively breastfed during the first 3 months of life, while 31.6% continued to exclusively breastfeed for the first 6 months.[7] It also reported 39.9% and 43.2% of mothers mixed-feeding (MF) at ages 3 and 5 months, respectively.[7] Various interventions exist in SA to address poor infant-feeding practices. The Tshwane Declaration, National Department of Health (NDoH), is specifically committed to increasing BF interventions by providing free antiretroviral drugs to prevent HIV transmission through BF, and to improve the health and survival of HIV-infected mothers.[8] It is also committed to fully implementing national regulations of the International Code of Marketing of Breastmilk Substitutes, Mother-Baby Friendly Initiative (MBFI) and Kangaroo mother care in all public and private health facilities.[8]
Unfortunately, early cessation of BF in favour of commercial breastmilk substitutes, introduction of liquids such as water, juices and tea, needless supplementation and prematurely timed introduction of solid, semi-solid and soft foods, often of poor quality, are far too common.[9] It has been reported that MF practices could reduce the economic dividends and increase healthcare costs, reduce the intelligence quotient (IQ), and lead to poor school attainment and a lower salary in later years.[10] In SA, it has been shown that MF is the norm.[11,12] The aim of this study was to identify the MF practices in a cohort of mothers of infants aged 4 - 14 weeks in the Tlokwe subdistrict of North West Province, SA, and to determine the sociodemographic factors associated with MF practices. Understanding sociodemographic determinants is critical for informing effective evidence-based interventions to improve EBF rates and reduce MF practices, thereby ultimately improving the nutritional status of infants and young children.
Methods
Research design
This is a substudy of a larger prospective cohort study, which was designed to follow up mothers and examine the rate of discontinuation of EBF from the early BF period (day 3 - 14), at4 - 8 weeks, 10 - 14 weeks through to 20 - 24 weeks of age. The study recruited pregnant women in their third trimester or postpartum mothers, with infants aged 3 - 14 days, attending 8 health facilities in the Tlokwe subdistrict of North West. Data collection took place during routine visits by the study participants to the health facility or at their homes. This substudy focused only on sociodemographic factors and MF practices at 2 time points - infants aged 4 - 8 weeks and 10 - 14 weeks.
Study context and technique
The sample size of this study was 159 infants at age 4 - 8 weeks and 109 infants at age 10 - 14 weeks. The study sample power was calculated at 80%, which was «=110 at 10 - 14 weeks, based on the prevalence of EBF of 32% among a cohort of infants <6 months of age. The recruitment process was supported by the Tlokwe subdistrict primary healthcare programme manager and the subdistrict primary healthcare facilities. Sociodemographic data were obtained at 4 - 8 weeks, with selected questions repeated at 10 - 14 weeks; infant-feeding and food-frequency data were gathered at both time points. The researcher administered the questionnaire by asking the mother to provide sociodemographic background information (living arrangements, type of house, relationship status, employment status and source of income). A 7-day infant-feeding and food-frequency questionnaire based on the food categories of the standardised WHO 24-hour recall form was used.
Data analysis
Data were analysed using SPSS version 25.0 (IBM Corp., USA). Normal data are presented as means (standard deviation (SD)), skewed data as median values (25th, 75th percentiles), and categorical values as percentages and frequencies.
Data were analysed for associations using χ2 and logistic regression, adjusting for potential covariates.
Ethical considerations
The Health Research Ethics Committee of North-West University granted ethical approval to conduct the study (ref. no. NWU-00030-17-A1-02).
Results
Table 1 shows the sociodemographic information of the mothers. One-third of mothers were in the age category 25 - 29 years. More than half (57.2%) spoke SeTswana. While the majority of the mothers reported being in stable relationships (89.3%), only 28.9% lived with the father of their infant. The majority (80.5%) of the mothers had some degree of high school education (grade 8 - 12) and 75.5% were unemployed. Most households received an income of <ZAR3 000 (41.5%), with only 48.4% receiving child support grants (CSGs). The majority (93.1%) of mothers self-reported as the primary caregiver. Approximately half (55.3%) reported having received mobile health (mHealth) messages from MomConnect, a National Department of Health (NDoH) program.
The mixed-feeding practices of mothers with infants aged 4 - 8 and 10 - 14 weeks
Fig. 1 presents the infant-feeding practices analysed by infant age at time point 1 (4 - 8 weeks) and time point 2 (10 - 14 weeks), including BF together with formula feeding (BFFF), water (BFwater) or foods (BFfoods). At time point 2, the proportion of infants who were breastfed was 86.2%, with a low EBF rate of 38.5%, while 20% received formula milk and breastmilk. MF increased with infant age. MF rates (61.5%) were: BFwater (36.7%) and BFfoods (15.6%).
The practices of mixed feeding with water
Fig. 2 presents the mothers who were MF with either water, water with formula or foods. Of the mothers (n=159) who were feeding their infants water at 4 - 8 weeks, 8.2% gave them plain water. More than a quarter of mothers (29.3%) gave their infants water with added sugar, 13.8% gave water and formula milk and 4.4% water and food. At time point 2 (10 - 14 weeks), 46% of mothers reported giving plain water. At this time point (n=109), 20.1% of mothers gave plain water and those who gave water with added sugar increased to 28.9%, while those who gave their infants water and formula feeding and water and food increased to 15.1% and 9.4%, respectively.
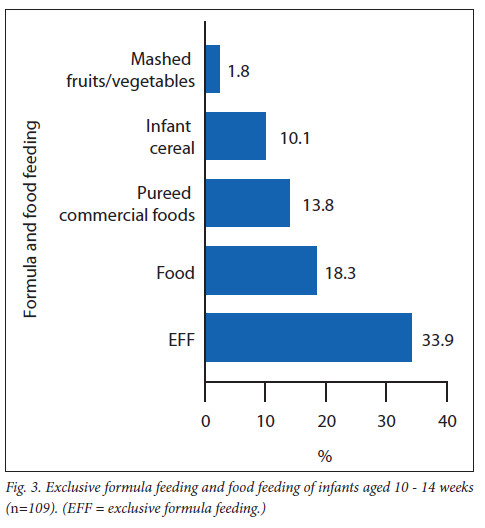
Formula feeding and food feeding
Fig. 3 illustrates the formula feeding and food feeding of infants aged 10 - 14 weeks. The percentage of mothers practising exclusive formula feeding at 10 - 14 weeks was 33.9%. Food feeding at 10 - 14 weeks increased 6-fold from that at 4 - 8 weeks to 18.3%. With regard to food feeding, 13.8% gave pureed commercial food, while 10.1% and 1.8% gave infant cereal and mashed fruits/vegetables, respectively.
Association of sociodemographic factors and mixed-feeding practices
Table 2 illustrates the association between sociodemographic factors and MF practices. There was no significant association between any of the sociodemographic variables and MF practices. A weak association with MF was seen between receiving MomConnect messages and age of the mother, with p=0.103 and p=0.123, respectively. With the application of the goodness-of-fit test (Hosmer-Lemeshow test), an improvement was seen from the full model to the final model (χ2=15.3; p=0.009). The result of this test was a significant association between parity and MF (odds ratio (OR) 0.536; confidence interval (CI) 0.357, 0.805; p=0.003). Therefore, the more children a mother has, the more likely she is to use MF. The mother as a primary caregiver showed an association with being less likely to mix feed, although it was not statistically significant (p=0.109). There were no significant associations between other sociodemographic variables and MF (Table 3).
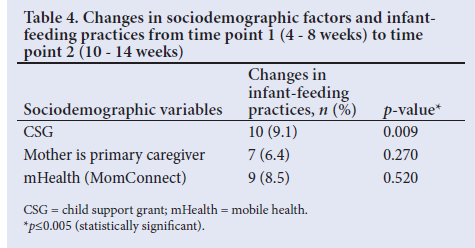
Table 4 illustrates the sociodemographic factors and infant-feeding practices between two time points (4 - 8 weeks and 10 - 14 weeks). There were only three changes. Although there was a significant change for receiving CSGs (p=0.009), no significant change was seen when the mother was the primary caregiver and could access mHealth.
Discussion
The importance of EBF in improving children's health is well established, but poor EBF rates are still prevalent in SA.[7] In this study, the duration of EBF decreased as infants grew older. The findings of low EBF (38.5%) at 10 - 14 weeks are similar to those in a 2016 national survey (36.1%).[7] In addition,
Budree et al.[13] reported low rates of EBF at 3 months in a cohort study conducted in a peri-urban area in Paarl, SA. These rates indicate that in the SA context, low EBF rates seem to be independent of location.
The study showed an increase in water feeding with infant age, from 39.6% at 4 - 8 weeks to 46% at 10 - 14 weeks. This finding is similar to that in a study by Goosen et al.[14] conducted in a low-income area among infants during their first 6 months of life; water was introduced within the first month of life (85%) and nutritive liquids or food within the first 3 months of life. Moreover, both BF and formula-feeding mothers supplemented their milk feeds with water. In another SA study, from Mpumalanga Province, it was recognised that mothers self-reported high EBF practices, as they were not specifically questioned about providing their infants with water.[15] In general, water was boiled with either gripe water or added sugar.[14] Infants receiving water were also more likely to receive food, such as infant cereal or pureed commercial foods. These results concur with those of Goosen et al.[14] Early introduction of water, foods or drinks is a cause for concern, as it marks the end of EBF with its protective and nutritious benefits to the infant.
Studies reported that the reasons to give these other items include fear regarding milk insufficiency, and perceived reduced milk production because the infant is hungry and not receiving optimal nutrition.[14-16] Furthermore, Nor et al.[17] reported that the reason for giving water and traditional medicines was for 'cleansing of the stomach'. Water, foods or drinks may not be hygienically prepared, thus increasing the risk of infections such as respiratory infections or diarrhoea and the risk of HIV transmission from mother to infant.[18 Other liquids and foods given to the baby alongside breastmilk may damage the already delicate and permeable gut wall of the infant and allow the virus to be transmitted more easily.[18]
Of the sociodemographic factors assessed in this study, increased parity of the mother was significantly associated with MF practices. Mothers who had >2 children were more likely to mix-feed their infants at 10 - 14 weeks. Ntuli and Modibedi,[19] in their case study of women in a prevention of mother-to-child transmission programme in Gauteng Province, proposed possible reasons for these results and postulated that mothers may have previously mixed-fed their older child, which did not seem to lead to any observable negative consequences; therefore, MF the second child would be the normative decision. In contrast, in two subdistricts that had facilities with MBFI accreditation (Mbombela and Emalahleni) in Mpumalanga, mothers with at least one older child were more likely to practise either EBF or exclusive replacement feeding.[15]
There was a significant association change regarding MF with CSG receipt at time point 2 (10 - 14 weeks). Zembe-Mkabile et al.[20] reported that the CSG was an important source of financial maintenance for all families, irrespective of geographical context, providing for basic needs such as food, schooling and healthcare. Consequently, mothers buy formula milk with the CSG, which is not enough to maintain a child and provide these basic needs. The results may also explain the significant association with increased parity: the more children a mother has, the more money she receives from multiple CSGs; therefore, she has more to spend on inappropriate infant foods.
The results showed the difference in age among mothers practising MF, with older mothers MF more than younger mothers (<25 years of age). Similarly, Van der Merwe et al.[15] proposed that older mothers have more independent choices than younger inexperienced mothers, who are dependent on antenatal care and support at home.
The data showed no significant association between relationship status (living with a partner or family) and MF. Similarly, Goosen et al.[14] found no association between marital status and MF (partially BF) in a low-income setting; however, a high proportion (84%) of MF occurred among unmarried mothers with infants aged <6 months. A high proportion of mothers in this study were in a relationship, but were not living with the father of the child, which is in line with the findings of Hall et al.[21] in the 2018 South African Child Gauge. Sherriff and Hall[22] suggest that some fathers may benefit from attending antenatal education sessions held in informal or casual settings, such as pubs or sports clubs, as engaging men through conventional health services is often challenging. A study conducted in a high-income country (Tasmania, Australia), showed that fathers generally viewed BF as optimal for their child's nutrition and some described it as healthy, natural, pure and essential.[23] More studies that include fathers in the BF fraternity need to be conducted in low- and middle-income countries.
The current study did not show an association between mothers who did not receive MomConnect messages and MF. In contradiction to our findings, a cluster-randomised controlled trial conducted in Bauchi, Dass and Ganjuwa subdistricts, Nigeria, investigating mobile phone messaging and women's adherence to international BF recommendations, found the odds of EBF to 3 months as elevated in the intervention group (p=0.05) v. the control group.[24] A systematic review and meta-analysis showed that prenatal interventions using text messages/mobile phone v. general routine visits improved EBF rates for 3 months by 52.8%.[25]
This study limitations were the small sample size, exclusion of fathers and teenage mothers, and limited follow-up time.
Conclusion
The high proportion of mothers who mixed-fed indicates that MF is still the norm, as in other SA contexts. MF increased with infant age. Most mothers mixed-fed with water, formula and food. There was also a significant association between parity and MF. Furthermore, there was a trend of an association with infant-feeding practices when the CSG was received at age 4 - 8 weeks or at 10 - 14 weeks. In Tlokwe especially older multiparous mothers receiving the CSG must be encouraged to continue with EBF for longer periods, with special focus on BF support throughout the first 6 months of an infant's life. There should be health education interventions for those women with sociodemographic factors that seem to be associated with lower BF rates and increased MF. To assist with engagement of fathers, a father-mother team and father-baby bond should be encouraged. Mothers and fathers should receive infant-feeding information at antenatal care visits, when it is appropriate to plan and decide on feeding practices, and mothers should be encouraged and supported at postnatal care to continue with BF.
Declaration. The research for this study was done in partial fulfilment of the requirements for NMS's MSc Nutrition degree at North-West University, Potchefstroom campus.
Acknowledgements. The authors acknowledge the support of the Tlokwe subdistrict Department of Health and staff in the 8 health clinics, as well as Mrs Noloyiso Matiwane and Ms Bakang Olifant during data collection.
Author contributions. NMS, CBW, EP and HSK conceptualised the study and designed data collection methods. NMS collected the data. HSK performed statistical analysis of the data. All authors contributed to writing and reviewing the manuscript and approved the final manuscript.
Funding. Funding for this research was received from the Department of Science and Technology (DST)/National Research Foundation (NRF) Centre of Excellence for Food Security Project: 160502.
Conflicts of interest. None.
References
1. Rollins NC, Bhandari N, Hajeebhoy N, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet 2016;387(10017):491-504. https://doi.org/10.1016/S0140-6736(15)01044-2 [ Links ]
2. Sankar MJ, Sinha B, Chowdhury R, et al. Optimal breastfeeding practices and infant and child mortality: A systematic review and meta-analysis. Acta Paediatr 2015;104:3-13. https://doi.org/10.1111/apa.13147 [ Links ]
3. Reynolds D, Hennessy E, Polek E. Is breastfeeding in infancy predictive of child mental well-being and protective against obesity at 9 years of age? Child Care Health Develop 2014;40(6):882-890. https://doi.org/10.1111/cch.12126 [ Links ]
4. Bernardo H, Cesar V, World Health Organization. Long-term effects of breastfeeding: A systematic review. 2013. https://apps.who.int/iris/handle/10665/79198 (accessed 31 October 2022). [ Links ]
5. Victora CG, Bahl R, Barros AJ, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016;387(10017):475-490. https://doi.org/10.1016/so140-6736(15)01024-7 [ Links ]
6. World Health Organization/United Nations Children's Fund. Global strategy for infant and young child feeding. 2003. https://www.who.int/nutrition/publications/infantfeeding/9241562218/en/ (accessed 2 November 2022). [ Links ]
7. National Department of Health - NDoH, Statistics South Africa - Stats SA, South African Medical Research Council - SAMRC, and ICF. South Africa Demographic and Health Survey 2016. Pretoria and Rockville, Maryland: NDoH, Stats SA, SAMRC, and ICF, 2019. https://dhsprogram.com/publications/publication-fr337-dhs-final-reports.cfm (accessed 2 November 2022). [ Links ]
8. National Department of Health. The Tshwane Declaration of support for breastfeeding in South Africa. S Afr J Clin Nutr 2011;24(4):214. [ Links ]
9. Labbok MH, Wardlaw T, Blanc A, Clark D, Terreri N. Trends in exclusive breastfeeding: Findings from the 1990s. J Hum Lactation 2006;22(3):272-276. https://doi.org/10.1177/0890334405279256 [ Links ]
10. United Nations Children's Fund/World Health Organization. Nurturing the health and wealth of nations: The investment case for breastfeeding. 2017. https://www.who.int/publications/m/item/nurturing-the-health-and-wealth-of-nations-the-investment-case-for-breastfeeding/ (accessed 2 November 2022). [ Links ]
11. Ijumba P, Doherty T, Jackson D, Tomlinson M, Sanders D, Persson LÁ. Social circumstances that drive early introduction of formula milk: An exploratory qualitative study in a peri-urban South African community. Matern Child Nutr 2014;10(1):102-111. https://doi.org/10.1111/mcn.12012 [ Links ]
12. Siziba L, Jerling J, Hanekom S, Wentzel-Viljoen E. Low rates of exclusive breastfeeding are still evident in four South African provinces. S Afr J Clin Nutr 2015;28(4):170-179. https://doi.org/10.1080/16070658.2015.11734557 [ Links ]
13. Budree S, Goddard E, Brittain K, Cader S, Myer L, Zar HJ. Infant feeding practices in a South African birth cohort - a longitudinal study. Matern Child Nutr 2017;13(3):e12371. https://doi.org/10.1111/mcn.12371 [ Links ]
14. Goosen C, McLachlan M, Schübl C. Infant feeding practices during the first 6 months of life in a low-income area of the Western Cape Province. S Afr J Child Health 2014;8(2):50-54. https://doi.org/10.7196/SAJCH.675 [ Links ]
15. Van der Merwe S, du Plessis L, Jooste H, Nel D. Comparison of infant-feeding practices in two health subdistricts with different baby-friendly status in Mpumalanga Province. S Afr J Clin Nutr 2015;28(3):121-127. https://doi.org/10.1080/16070658.2015.11734546 [ Links ]
16. Du Plessis L, Peer N, English R, Honikman S. Breastfeeding in South Africa: Are we making progress? S Afr Health Rev 2016;2016(1):109-123. [ Links ]
17. Nor B, Ahlberg BM, Doherty T, et al. Mother's perceptions and experiences of infant feeding within a community-based peer counselling intervention in South Africa. Matern Child Nutr 2012;8(4):448-458. https://doi.org/10.1111/j.1740-8709.2011.00332.x [ Links ]
18. Gribble KD, Hausman BL. Milk sharing and formula feeding: Infant feeding risks in comparative perspective? Austr Med J 2012;5(5):275. https://doi.org/10.4066/amj.2012.1222 [ Links ]
19. Ntuli B, Modibedi K. Decision-making and practice on infant feeding: A case study of women in a prevention of mother to child transmission programme in Gauteng Province, South Africa: Public health intervention for maternal and child health. Afr J Phys Health Educ Recr Dance 2015;21(Suppl 2):12-24. [ Links ]
20. Zembe-Mkabile W, Surender R, Sanders D, Jackson D, Doherty T. The experience of cash transfers in alleviating childhood poverty in South Africa: Mothers' experiences of the child support grant. Glob Public Health 2015;10(7):834-851. https://doi.org/10.1080/17441692.2015.1007471 [ Links ]
21. Hall K, Richter L. Children, families and the state. S Afr Child Gauge 2018. [ Links ]
22. Sherriff N, Hall V. Engaging and supporting fathers to promote breastfeeding: A new role for health visitors? Scand J Caring Sc 2011;25(3):467-475. https://doi.org/10.1111/j.1471-6712.2010.00850.x [ Links ]
23. Hansen E, Tesch L, Ayton J. 'They're born to get breastfed' - how fathers view breastfeeding: A mixed method study. BMC Preg Childbirth 2018;18(1):238. https://doi.org/10.1186/AS12884-018-1827-9 [ Links ]
24. Flax VL, Negerie M, Ibrahim AU, Leatherman S, Daza EJ, Bentley ME. Integrating group counseling, cell phone messaging, and participant-generated songs and dramas into a microcredit program increases Nigerian women's adherence to international breastfeeding recommendations. J Nutr 2014;144(7):1120-1124. https://doi.org/10.3945/jn.113.190124 [ Links ]
25. Lee SH, Nurmatov UB, Nwaru BI, Mukherjee M, Grant L, Pagliari C. Effectiveness of mHealth interventions for maternal, newborn and child health in low- and middle-income countries: Systematic review and meta-analysis. J Glob Health 2016;6(1). https://doi.org/10.7189/jogh.06.010401 [ Links ]
 Correspondence:
Correspondence:
H S Kruger
salome.kruger@nwu.ac.za
Accepted 17 August 2021














