Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.16 n.3 Pretoria Sep. 2022
http://dx.doi.org/10.7196/SAJCH.2022.v16i3.1879
RESEARCH ARTICLE
The knowledge and practices of caregivers regarding the administration of oral liquid medication to children at a healthcare clinic in Bloemfontein, South Africa
W BezuidenhoutI; J CummingsI; L de KlerkI; D FinlayI; C LewisI; L PienaarI; A BouwerII; R CoetzeeIII; G JoubertIII
I3rd-year medical student; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIMPharm; Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIIPharmD; School of Public Health, Faculty of Community and Health Sciences, University of the Western Cape, Cape Town, South Africa
IVBA, MSc Department of Biostatistics, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND. Children are dependent on their caregivers to accurately administer medication to them.
OBJECTIVES. To determine the knowledge and practices of primary caregivers regarding their methods of oral liquid medication administration, preferred measuring utensils, accuracy of preferred measuring utensils and different medication classifications that they collected. The study was conducted at Pelonomi Polyclinic Pharmacy, Bloemfontein, South Africa.
METHODS. A quantitative, cross-sectional descriptive study (with analytical aspects) was conducted, which used consecutive, convenient sampling. The pharmacy staff assisted in recruiting participants, after which a screening form was used to determine their eligibility. Participants were provided with an information document and consent form. The liquid medication was classified according to a drug classification list, and one medication was selected for the focus of the structured interview. The questionnaire was completed using REDCap. Thereafter, researchers used the information on the medication label to determine the accuracy of the caregiver's answers.
RESULTS. The majority of the 89 participants (56.2%) answered all 3 administration-related questions correctly, with 84.3% answering the questions regarding quantity and frequency correctly. The medication measure (43.8%) was the preferred measuring utensil for any liquid medication at home, and the syringe (53.9%) for the selected liquid medication used in the interview, both accurate measuring utensils. Most children (56.2%) were prescribed 'other medication' (e.g. vitamins and mineral supplements), followed by analgesics (47.2%) and antibiotics (42.7%).
CONCLUSION. Primary caregivers at Pelonomi Polyclinic Pharmacy know how to administer oral liquid medication to children accurately. Most caregivers indicated that they use accurate measuring utensils.
Paediatric patients are a unique patient group and because of the complexity of paediatric dosing, they require greater attention and vigilance.[1] Medication administration errors by caregivers or parents may occur and are influenced by various factors, such as lack of counselling, inappropriate measuring equipment and literacy levels. Reports suggest that >40% of caregivers make errors when administering liquid medication to children.[2,3]
Treatment failures in children most likely occur because ofinaccurate administration of medication rather than the incorrect choice of medication.[4] Dosing tools are known contributors to medication dosing errors.[5] Errors occur due to incorrectly used utensils or lack of knowledge, which include using kitchen utensils (teaspoon or tablespoon) or oral syringes incorrectly.[3,6] The lack of knowledge of caregivers could include the misunderstanding of measurement abbreviations or of decimals used in the prescribed dosage.[3,7]
A study conducted in Ghana[7] investigated the accuracy of household spoons available to caregivers. All categories of household spoons used (i.e. teaspoons and non-teaspoons, including tablespoons) did not measure volumes accurately to 5 mL or 10 mL. Small, prescribed dosing amounts lead to more errors in administration and may create confusion when the caregiver needs to measure the dose. The study 'Safe Administration for Rx for Kids' (SAFE Rx for Kids) found that oral syringes should be used rather than dosing cups, and that teaspoon units on prescriptions should be avoided to eliminate confusion.[8,9]
The US Food and Drug Administration recommends that standardised utensils should be included in all over-the-counter products where the measurement of liquid medication is necessary, as caregivers are less likely to make errors when they receive measuring utensils.[10,11] Medication administration errors in children can therefore be reduced by providing dosing utensils more accurately matched to the prescribed dose.[6]
In addition, labels that include the mL unit compared with the mL/ tsp unit may cause less confusion and result in fewer errors. Caregivers also tend to confuse the abbreviation tsp (teaspoon) with tbsp (tablespoon).[8] The US Department of Health and Human Services, in a study of 287 caregivers, found that 41.7% of labels had a mL-only unit and 50.0% a tsp-only unit. The 42.5% of caregivers who used tsp or tbsp units made more errors than the 27.6% who used mL-only units. Furthermore, 16.7% of caregivers used a teaspoon or tablespoon when labels indicated tsp units, rather than using a standard utensil: only 38.0% would use oral syringes, 13.9% a dosing cup, 13.6% a dosing spoon and 1.7% a measuring spoon.[10]
Errors in medication administration can result in overdosing and underdosing of the child. Although less serious than overdosing, the general symptoms of drug underdosing include adverse drug events and poor clinical outcomes, such as drug resistance, prolonged illness and symptoms and unnecessary visits to the doctor.[7,12] Antibiotic resistance can also result from incorrect administration practices by caregivers, which include inaccurate doses, or the discontinuation of the treatment course of medication, such as when the child's health improved.[13,14]
A Malaysian study[13] reported that many caregivers were unaware that the full treatment course of antibiotics must be completed to avoid antibiotic resistance. Antibiotic regimen compliance of caregivers who had sufficient knowledge of this type of therapy was better than that of those who had lesser knowledge of antibiotics.
Medication administration errors in paediatric patients are a common problem; however, the South African (SA) literature regarding this topic is limited. SA studies have focused on the hospital setting[15] or on children receiving a specific type of medication, such as antiretroviral therapy[16] or over-the-counter painkillers.[17]
Aim and objectives
The aim of the study was to gain insight into primary caregivers' administration practices at home of oral liquid medication collected at Pelonomi Polyclinic Pharmacy in Bloemfontein, Free State, SA, in terms of the correct dose, duration and frequency, in children <8 years. The secondary objectives were to determine these caregivers' preferred measuring utensil and report on its accuracy, as well as to determine the different classifications of medication collected by the caregivers from Pelonomi Polyclinic Pharmacy.
Methods
Setting and study design
This cross-sectional, descriptive quantitative study with analytical aspects was conducted at Pelonomi Polyclinic Pharmacy. Pelonomi Regional Hospital is situated in Bloemfontein, Free State, SA, and is the referral centre for patients from neighbouring health districts and regional hospitals.
Population and sampling
The target population consisted of caregivers who collected medication for children <8 years of age. The caregiver should also have been responsible for administering the medication to the child at home. Caregivers were excluded if they were <18 years old, collected only one oral liquid medication that was in drop form, or could not converse in English, Afrikaans or Sesotho.
A convenience consecutive sampling technique was used, based on the caregivers' availability and willingness to participate. The data collection was completed in 20 working days over 4 months (August -November 2019) when the student researchers were available.
Participant recruitment
Pelonomi Polyclinic Pharmacy staff directed eligible participants to the student researchers. A private consultation area was used to conduct interviews with the participants. After screening for eligibility to participate in the study, participants received the information document and consent form in English, Afrikaans or Sesotho. The researchers divided into pairs to discuss the study and conduct the consent process, using consistent lay terms with every participant. Sesotho translations were effected by one of the researchers.
Data collection
The design of the interview questionnaire, as well as collecting and managing of study data, was done using REDCap (Research Electronic Data Capture) tools.[18,19] The REDCap interview questionnaire was completed on cellular devices. One researcher of the pair asked the participant questions while the other researcher entered the data. The medications which the participants collected at that visit were classified in order of priority according to a drug classification list received from Pelonomi Polyclinic Pharmacy, i.e. antibiotics, antivirals, analgesics, anthelminthics, antihistamines and 'other medication. Antibiotics were prioritised because of the possible serious consequences, such as antibiotic resistance due to incorrect administration. One bottle of liquid medication (of the greater priority) was selected per participant. If the participant had more than one liquid medication in the same category, the medication that appeared first alphabetically was selected. The participants could refer to the medication label during the interview.
The interview proceeded based on the selected medication. A series of questions followed to determine the participants' medication administration practices. The selected bottle of medication was placed on the table and participants were able to look at the label on the bottle at their discretion, which was noted on the questionnaire.
Participants were then asked to choose the measuring utensil they would normally use at home, followed by what they would use for the selected medication. A selection of measuring utensils was presented to them: teaspoon, tablespoon, medication measure (plastic dosing spoon), syringe, measuring cup, cap of a medication bottle or drinking from the bottle. The medication measure, syringe and measuring cup were considered accurate measuring utensils and the remainder inaccurate. If the participant did not use any of the abovementioned utensils, 'other' would be indicated on the questionnaire and the alternative measuring utensil noted. The measuring utensils were placed in the abovementioned order for every interview.
After the interview, the unit and dosage used, duration of treatment and frequency of administration indicated on the label of the selected bottle were noted. If the label did not indicate the duration of the treatment course, the dispensing staff were consulted regarding the instructions they had given and these were considered to be correct.
Pilot study
In the pilot study, 10 caregivers were interviewed at Pelonomi Polyclinic Pharmacy. There was no misunderstanding of the questions or any poor feedback from participants regarding the content of the questionnaire. As no changes were made, the results were included in the main study.
Data analysis
The data were analysed using SAS version 9.4. Data were summarised by frequencies and percentages (categorical variables) and medians and ranges (numerical variables due to skew distributions). Subgroup comparisons were done using χ2 or Fisher's exact tests.
Ethical approval
Ethical approval to conduct the study was obtained from the Health Sciences Research Ethics Committee of the University of the Free State (ref. no. UFS-HSD2019/0622/2506). Permission to conduct the study at Pelonomi Polyclinic Pharmacy was granted by the Free State Department of Health. The researchers informed the head of Pelonomi Polyclinic Pharmacy, as well as the head of Pelonomi Hospital, of the study and made arrangements with Pelonomi staff so as to not disrupt their services.
The information document and consent form provided information regarding the research project, the researchers and details regarding participation in the study. This information ensured that the caregivers were able to grant informed consent if they wanted to participate in the study. All data collected remain confidential. The same number appeared on the participant's consent form and information document; therefore, if the participant wished to withdraw from the study, their questionnaire could be traced and removed.
Results
Demographics of the study population
In total, 100 primary caregivers were approached and 89 were eligible to participate (Fig. 1).

The median age of the 89 children was 2 years and 4 months (range 9 days - 8 years and 9 months). A total of 22 (25.0%) children were <10 months old. The gender distribution of the children was 43.8% (n=39) female and 56.2% (n=50) male. Participating caregivers were predominantly female (98.9%) and included mostly the mother of the child (92.1%), as well as 'other family' (6.7%) and legal guardians (1.1%).
Caregivers' medication administration practices at home
The primary objective was to gain insight into the participants' medication administration practices at home regarding the collected medication - in terms of dose, duration and frequency. Table 1 summarises the results of the correctness of the caregivers' responses regarding their medication administration practices.
Most participants (56.2%) answered all 3 administration-related questions correctly, whereas 29 (32.6%) answered 2 questions correctly, 8 (9.0%) answered only 1 question correctly and 2 (2.2%) did not answer any of the questions correctly. Of the 37 participants whose interview related to an antibiotic, 24 (64.9%) answered all 3 administration-related questions correctly, 8 (21.6%) answered 2 questions correctly and 5 (13.5%) answered 1 question correctly.
Measuring utensils
The secondary objective was to determine participants' preferred measuring utensil for administering liquid medication. Fig. 2 indicates the participants' responses regarding the measuring utensil that they would use to administer any liquid medication and the utensil they would use for the selected medication discussed during the interview.
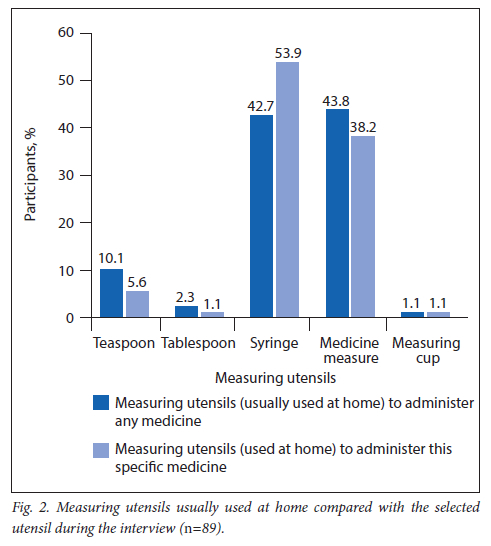
Accurate measuring utensils were provided to 63 (70.8%) of the caregivers on the day that they collected the medication, while 26 (29.2%) did not receive a measuring utensil.
Medication labelling
The results showed that 87 (97.8%) of the bottle labels indicated the dosage in mL, whereas 2 (2.2%) of the bottle labels indicated the dosage in tsp units.
The duration of treatment was not indicated on 38 (42.7%) of the bottle labels. During the interview, most of the participants (n=58; 65.2%) did not refer to the label on the bottle, and 34 (58.6%) of those participants answered the 3 administration-related questions correctly. A total of 16 participants (n=16/31; 51.6%) did refer to the label during the interview and provided the correct answers (p=0.53). In both groups, most of the participants indicated that they refer to the label
at home before administering the medication to the child (p=0.38). These groups included 24 participants (n=24/31; 77.4%) who referred to the label during the interview and 48 participants (n=48/58; 82.8%) who did not look at the label during the interview.
Classification of collected medication
The number of liquid medications collected ranged between 1 and 10 per child, with 50 (56.1%) and 22 (24.7%) children being administered 1 and 2 medications, respectively. Most children (56.1%) received medication classified as 'other medication' (e.g. vitamins and mineral supplements). Antibiotics were received by 38 children (42.7%), and 42 children (47.2%) received an analgesic. Nine (10.1%), 16 (18.0%) and 2 (2.2%) children received antihistamines, anthelminthics and antivirals, respectively.
The selected liquid medication used during the interview was mainly antibiotics (41.5%), followed by analgesics (17.9%), anthelminthics (17.9%) and antihistamines (5.6%), while 15 medications (16.8%) were classified as 'other medication' (e.g. vitamins and mineral supplements).
Discussion
Most of the caregivers interviewed were female and were the mothers of the children - similar to the demographic profile of a study conducted by Ramanayake et al.[20] in Sri Lanka. The median age of the children in the Sri Lanka study was 2 years and 4 months. A study conducted in Tanzania[21] found that medication in the form of liquids was preferred among younger children, as it is easier to swallow.
Dose (quantity), duration and frequency
Most caregivers were accurate regarding the dose (quantity), duration and frequency of administration. In contrast, a similar study found that 43.0% of caregivers would have overdosed their children, and 16% exceeded the dosing frequency.[20]
Measuring utensils
This study findings suggest that participants commonly used syringes, as well as medicine measures, when administering oral liquid medication to children at home. The results are similar to those of Williams et al.,[5] who found that oral syringes (62%) were most commonly used by parents to give medication to children.
Household spoons are considered inaccurate; their use for dosing oral liquid medications is anachronistic and should be discouraged.[7] Therefore, the results from our study are considered satisfactory, as syringes and medication measures are considered accurate measuring utensils and the use of syringes may decrease the chance of administration errors which may lead to overdosing or underdosing, especially when small volumes are measured.[8,22] Errors using measuring cups occur more frequently than errors using syringes.[6,22] Sobhani et al.[23]found that household teaspoons can measure from 1.9 to 9 mL; therefore, the use of household teaspoons increases the risk of administration errors. In their study, 66.7% of participants measured liquid medication accurately with a syringe. Yin et al.[22] showed that 85.0% of participants dosed accurately with appropriate measuring utensils, such as a dropper, medication measure and syringe. A reason for the increased accuracy with measuring utensils, such as syringes, could be the ease of use.[7,23]
Although 42.7% of participants indicated that they use a syringe at home to administer liquid medication, 53.9% proceeded to select a syringe to administer the medication selected for the interview. The reason for this difference could be that most caregivers (70.8%) were supplied with measuring utensils (i.e. syringes) by the pharmacy when collecting the medication. Whether they were provided with a measuring utensil could also explain the change in choice to use syringes when administering the medication selected for the interview. A study conducted in Ghana by Bayor et al.[7]found that most people (95%) used household spoons in dosing oral liquid medications, which could be due to almost half (46%) of oral liquid remedies in the Ghanaian market not having enclosed dosing devices.
Medication labelling
Very few bottles were labelled with tsp units, while 97.8% of bottle labels had mL units. A study conducted by Tanner et al.'81 found that labels that include the mL unit compared with mL/tsp units caused less confusion and resulted in fewer errors. A mL-only measuring system on prescriptions clarifies the administration instructions for caregivers and decreases the use of non-standard utensils.[11,24,25]
In the current study, only 1 participant was not told the duration of the treatment course by the pharmacy, and 42.7% of the labels on the selected bottles of medication did not state the duration of the treatment course. For these cases, the researchers consulted the pharmacy dispensing staff to determine whether the participant answered correctly.
According to the Good Pharmacy Practice Manual and associated South African Pharmacy Council (SAPC) rules (in accordance with the South African Medicines Act), the following information must be included on the label of all prescribed medication: the proprietary name/approved name/names of all active ingredients, patient's name, how the medication must be used, name and address of the dispenser, date and reference number.[26] It is therefore not a legal requirement to include the duration of the treatment course on the label, and pharmacies dispensing to many people every day (such as Pelonomi Polyclinic Pharmacy) may choose to exclude this information and (instead) explain it verbally. Several medications also have variable durations (i.e. when necessary, when stopping breastfeeding), depending on the condition needing treatment. However, labels not stating the duration of the treatment course are potentially detrimental to the treatment of the child, as caregivers may not understand the instructions given to them, or may be forgetful and not have the information on the label to which they can refer when at home.[27]
Most participants indicated that they would look at the bottle's label at home before administering the medication. However, most participants did not look at the label when answering the administration-related questions during the interview, which may be because they remembered the instructions given to them by the pharmacist. Many of the participants answered all 3 administration-related questions correctly. This is a positive result, as most caregivers would, theoretically, administer the medication accurately to the child at home.
Study limitations
A noticeable limitation was the communication barrier with several of the participants. This barrier could have affected the way that caregivers interpreted the instructions given to them by a non-Sesotho-speaking pharmacist. A study conducted by Samuels-Kalow et al.[28] found that Spanish-speaking caregivers were more likely to make administration errors after receiving instructions in English.
The researchers acknowledge that the participants' accuracy with regard to the administration-related questions may be due to the interview being conducted directly after collecting medication from the pharmacy. The pharmacy dispensing staff would have informed the caregivers how to administer the medication correctly. During the interview, the caregivers recalled this information quite easily from their short-term memory, thus giving accurate answers.
A further limitation was that several caregivers were reluctant to participate owing to time constraints, such as transport and work commitments.
Conclusion
The caretakers' results show adequate knowledge with regard to administering an accurate dose of oral liquid medication at the correct frequency and for the correct duration to the children at home. Most participants prefer accurate measuring utensils at home and also administer prescribed medication with an accurate measuring utensil (i.e. syringe or medication measure). Therefore, the handing out of measuring utensils by the pharmacy together with all liquid medication has a positive impact on the medication administration practices of caregivers.
Pharmacy staff play a pivotal role in educating caregivers about medication administration to children at home. Correct administration of medication, i.e. the correct dose, frequency and duration, lowers the risk of adverse effects associated with the overdosing and underdosing in this vulnerable population.
Recommendations
The researchers recommend a larger study sample for future studies to enable the investigation of associations between caregivers' sociodemographic characteristics and knowledge and practice. Translators must be available during the interviews. Interviews should not be conducted immediately after the caregivers have left the pharmacy with their medication (i.e. rather a while after they have heard the instructions given by pharmacy dispensing staff).
Future studies could include the type of measuring utensils that participants receive from the pharmacy. The results of this study and/or future studies may be useful in the implementation of educational pictographic instructions to assist caregivers with a better understanding of medication administration practices. This could include how to use a syringe and measuring cup as dosing utensils, and the inaccuracy of using household utensils (e.g. teaspoons and tablespoons).
The results of this study can support the importance of proper education and counselling of primary caregivers to ensure safe medication use in paediatric patients. Medication errors have been associated with healthcare professionals' knowledge and training, patient characteristics, environmental factors, prescribing errors and lack of communication.[6] To optimise medication safety in paediatric patients, a multidisciplinary, integrated approach is critical.
Declaration. None.
Acknowledgements. The researchers acknowledge the staff of Pelonomi Polyclinic Pharmacy for being a continuous source of encouragement during the duration of the study. Ms T Mulder, medical editor/writer, Faculty of Health Sciences, University of the Free State, is thanked for technical and editorial preparation of the manuscript.
Author contributions. WB, JC, LdK, DF, CL and LP wrote the protocol, performed the data collection, interpreted the results and did the initial write-up of this study. AB was the supervisor, suggested the concept, and assisted with the protocol development, interpretation of data and write-up. RC was the co-supervisor, and assisted with the protocol development, interpretation of data and write-up. GJ assisted with the planning, performed data analysis and assisted with the interpretation and write-up.
Funding. None.
Conflicts of interest. None.
References
1. Cunningham KJ. Analysis of clinical interventions and the impact of pediatric pharmacists on medication error prevention in a teaching hospital. J Pediatr Pharmacol Ther 2012;17(4):365-373. https://doi.org/10.5863/1551-6776-17A365 [ Links ]
2. Yin HS, Dreyer BP, Moreira HA, et al. Liquid medication dosing errors in children: Role of provider counseling strategies. Acad Pediatr 2014;14(3):262-270. https://doi.org/10.1016/j.acap.2014.01.003 [ Links ]
3. Honey BL, Condren M, Phillips C, Votruba A. Evaluation of oral medication delivery devices provided by community pharmacies. Clin Pediatr (Phila) 2013;52(5):418-422. https://doi.org/10.1177/0009922813479160 [ Links ]
4. Buddhadev MD, Patel KS, Patel VJ, Bhatt SP, Deshpande SS. Perceptions about oral liquid medication dosing devices and dosing errors by caregivers of hospitalised children. J Pharm Res 2016;10(12):810-813. [ Links ]
5. Williams TA, Wolf MS, Parker RM, et al. Parent dosing tool use, beliefs, and access: A health literacy perspective. J Pediatr 2019;215:244-251.e1. https://doi.org/10.1016/j.jpeds.2019.08.017 [ Links ]
6. Yin HS, Parker RM, Sanders LM, et al. Pictograms, units and dosing tools, and parent medication errors: A randomised study. Pediatrics 2017;140(1):e20163237. https://doi.org/10.1542/peds.2016-3237 [ Links ]
7. Bayor MT, Kipo SL, Ofori-Kwakye K. The accuracy and quality of household spoons and enclosed dosing devices used in the administration of oral liquid medication in Ghana. Int J Pharm Pharm Sci 2010;2(Suppl 1):150-153. [ Links ]
8. Tanner S, Wells M, Scarbecz M, McCann BW Sr. Parents' understanding of and accuracy in using measuring devices to administer liquid oral pain medication. J Am Dent Assoc 2014;145(2):141-149. https://doi.org/10.14219/jada.2013.20 [ Links ]
9. Yin HS, Parker RM, Sanders LM, et al. Liquid medication errors and dosing tools: A randomised controlled experiment. Pediatrics 2016;138(4):e20160357. https://doi.org/10.1542/peds.2016-0357 [ Links ]
10. US Department of Health and Human Services: Center for Drug Evaluation and Research (CDER). Guidance for Industry: Dosage Delivery Devices for Orally Ingested OTC Liquid Drug Products. Silver Spring, MD: US Food and Drug Administration, 2011. [ Links ]
11. Yin HS, Mendelsohn AL, Wolf MS, et al. Parents' medication administration errors: Role of dosing instruments and health literacy. Arch Pediatr Adolesc Med 2010;164(2):181-186. https://doi.org/10.1001/archpediatrics.2009.269 [ Links ]
12. Dahmash DT, Shariff ZB, Kirby DJ, Terry D, Huynh C. Literature review of medication administration problems in paediatrics by parent/caregiver and the role of health literacy. BMJ Paediatr Open 2020;4(1):e000841. https://doi.org/10.1136/bmjpo-2020-000841 [ Links ]
13. Ling Oh A, Hassali MA, Al-Haddad MS, Syed Sulaiman SA, Shafie AA, Awaisu A. Public knowledge and attitudes towards antibiotic usage: A cross-sectional study among the general public in the state of Penang, Malaysia. J Infect Dev Ctries 2011;5(5):338-347. https://doi.org/110.3855/jidc.1502 [ Links ]
14. Kotwani A, Wattal C, Katewa S, Joshi PC, Holloway K. Factors influencing primary care physicians to prescribe antibiotics in Delhi India. Fam Pract 2010;27(6):684-690. https://doi.org/10.1093/fampra/cmq059 [ Links ]
15. Truter A, Schellack N, Meyer JC. Identifying medication errors in the neonatal intensive care unit and paediatric wards using a medication error checklist at a tertiary academic hospital in Gauteng, South Africa. S Afr J Child Health 2017;11(1):5-10. https://doi.org/10.7196/SAJCH.2017.v11i1.1101 [ Links ]
16. Coetzee B, Kagee A, Bland R. Video observations of treatment administration to children on antiretroviral therapy in rural KwaZulu-Natal. AIDS Care 2016;28(Suppl 2):34-41. https://doi.org/10.1080/09540121.2016.1176674 [ Links ]
17. Bennin F, Rother HA. 'But it's just paracetamol': Caregivers' ability to administer over-the-counter painkillers to children with the information provided. Patient Educ Couns 2015;98(3):331-337. https://doi.org/10.1016/j.pec.2014.11.025 [ Links ]
18. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap) - a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42(2):377-381. https://doi.org/10.1016/j.jbi.2008.08.010 [ Links ]
19. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208 [ Links ]
20. Ramanayake RP, Jayasinghe LR, de Silva AH, Wijesinghe WA, Kanaganayagam N. Knowledge and practices of paracetamol administration among caregivers of pediatric age group patients. J Fam Med Prim Care 2012;1(1):30-33. https://doi.org/10.4103/2249-4863.94448 [ Links ]
21. Adams LV, Craig SR, Mmbaga EJ, et al. Children's medicines in Tanzania: A national survey of administration practices and preferences. PLoS ONE 2013;8(3):e58303. https://doi.org/10.1371/journal.pone.0058303 [ Links ]
22. Yin HS, Dreyer BP, Ugboaja DC, et al. Unit of measurement used and parent medication dosing errors. Pediatrics 2014;134(2):e354-e361. https://doi.org/10.1542/peds.2014-0395 [ Links ]
23. Sobhani P, Christopherson J, Ambrose PJ, Corelli RL. Accuracy of oral liquid measuring devices: Comparison of dosing cup and oral dosing syringe. Ann Pharmacother 2008;42(1):46-52. https://doi.org/10.1345/aph.1K420 [ Links ]
24. Yin HS, Parker RM, Sanders LM, et al. Effect of medication label units of measure on parent choice of dosing tool: A randomised experiment. Acad Pediatr 2016;16(8):734-741. https://doi.org/10.1016/j.acap.2016.04.012 [ Links ]
25. Lovegrove MC, Sapiano MRP, Paul IM, Yin HS, Wilkins TL, Budnitz DS. Primary care provider perceptions and practices regarding dosing units for oral liquid medications. Acad Pediatr 2018;18(4):405-408. https://doi.org/10.1016/j.acap.2017.12.002 [ Links ]
26. The South African Pharmacy Council. Good Pharmacy Practice in South Africa. Pretoria: SAPC, 2018. [ Links ]
27. Lokker N, Sanders L, Perrin EM, et al. Parental misinterpretations of over-the-counter pediatric cough and cold medication labels. Pediatrics 2009;123(6):1464-1471. https://doi.org/10.1542/peds.2008-0854 [ Links ]
28. Samuels-Kalow ME, Stack AM, Porter SC. Parental language and dosing errors after discharge from the pediatric emergency department. Pediatr Emerg Care 2013;29(9):982-987. https://doi.org/10.1097/PEC.0b013e3182a269ec [ Links ]
 Correspondence:
Correspondence:
A Bouwer
annatjie.bouwer@gmail.com
Accepted 16 August 2021














