Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.16 no.3 Pretoria Set. 2022
http://dx.doi.org/10.7196/SAJCH.2022.v16i3.1890
RESEARCH ARTICLE
HIV exposure and its association with paediatric ICU outcomes in children admitted with severe pneumonia at Chris Hani Baragwanath Academic Hospital, South Africa
K H KeelingI, II; J PriceIII, IV; K D NaidooV, VI
ICert Crit Care (SA) Paed; Nelson Mandela Children's Hospital, Johannesburg, South Africa
IICert Crit Care (SA) Paed; Division of Critical Care, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIMB ChB, DPhil (Oxon), Division of Critical Care, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IVMB ChB, DPhil (Oxon), MRC/Wits Rural Public Health and Health Transitions Research Unit, School of Public Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VCert Crit Care (SA) Paed Division of Critical Care, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
VICert Crit Care (SA) Paed; Division of Critical Care, Chris Hani Baragwanath Academic Hospital, Soweto, South Africa
ABSTRACT
BACKGROUND. Pneumonia is one of the leading causes of under-5 death in South Africa and accounts for a substantial burden of paediatric intensive care unit (PICU) admissions. However, little is known about PICU outcomes in HIV-exposed uninfected (HIV-EU) children with pneumonia, despite the growing size of this vulnerable population.
OBJECTIVES. To determine whether HIV exposure without infection is an independent risk factor for mortality and morbidity in children admitted to PICU with pneumonia.
METHODS. This retrospective review included all patients with pneumonia admitted to the PICU at Chris Hani Baragwanath Academic Hospital between 1 January 2013 and 31 December 2014. Patients were classified as HIV-unexposed (HIV-U), HIV-EU and HIV-infected. Medical records were reviewed to determine survival to PICU discharge, duration of PICU admission and duration of mechanical ventilation. Survival analysis was used to determine the association between HIV infection/exposure with mortality, and linear regression was used to examine the association with length of stay and duration of mechanical ventilation. This study included 107 patients: 54 were HIV-U; 28 were HIV-EU; 23 HIV-positive; and 2 had an unknown HIV status.
RESULTS. Overall, 84% (n=90) survived to PICU discharge, with no difference in survival based on HIV infection or exposure. Both HIV-EU and HIV-U children had significantly shorter PICU admissions and fewer days of mechanical ventilation compared with HIV-infected children (p=0.011 and p=0.004, respectively).
CONCLUSION. HIV-EU children behaved similarly to HIV-U children in terms of mortality, duration of PICU admission and length of mechanical ventilation. HIV infection was associated with prolonged length of mechanical ventilation and ICU stay but not increased mortality.
Pneumonia accounts for 16% of all deaths in children under 5 years of age annually.[1-4] However, the mortality rate from pneumonia in low- and middle-income countries (LMICs) is substantially greater than in high-income countries,[5] with sub-Saharan Africa accounting for almost 50% of global pneumonia deaths.[2,5] Given the high burden of HIV in sub-Saharan Africa, it is conceivable that HIV is a significant contributor to the morbidity and mortality of pneumonia, which increases the demands on scarce paediatric intensive care unit (PICU) services in the region.[2,6,7]
The introduction of antiretroviral drugs (ARVs) in South Africa (SA) has significantly decreased the mortality rate from HIV.[6,8] Furthermore, prevention of mother-to-child transmission programmes with lifelong maternal ARVs and infant prophylaxis, improved obstetric management, and changes in infant feeding practices have reduced vertical transmission rates to between 1% and 3% nationally.[9-13] As a result, HIV-exposed uninfected (HIV-EU) babies now account for as many as 30% of all births in
parts of southern Africa.[9,14,15] However, the effect of HIV exposure on pneumonia morbidity and mortality risk is less well known. They are nevertheless considered a vulnerable population and appear to have an increased morbidity and mortality rate from infections when compared with their HIV-unexposed (HIV-U) counterparts.[16]
This study describes the population of children admitted to the PICU at Chris Hani Baragwanath Academic Hospital (CHBAH) with a primary diagnosis of pneumonia and aims to determine whether HIV exposure without infection is an independent risk factor for mortality and morbidity in children with pneumonia.
Methods
Study design, site and participants
This retrospective review was conducted in the PICU at CHBAH between 1 January 2013 and 31 December 2014. CHBAH is a tertiary level hospital located in Soweto, Johannesburg. As a tertiary hospital, it accepts patients from primary and secondary referral centres, as well as providing sub-specialist care. With respect to paediatrics, there are ~450 combined paediatric in-patient beds at CHBAH. Given the relatively scarce economic resources of state hospitals in SA, the PICU at CHBAH has only 9 dedicated beds which accommodate ~350 admissions per year. Despite the ratio of PICU beds to paediatric beds being far less than internationally recommended norms, the PICU accepts patients from CHBAH itself, as well as surrounding referral hospitals, in a catchment area which stretches as far as the North West Province (~185 km away).
The study population included all patients admitted to the PICU with the World Health Organization (WHO) clinical definition of pneumonia.[1] Admission age in the PICU is from 1 month to 16 years of age.
Data collection and analysis
Data sheets were completed using medical records to obtain demographic data (age, sex, weight and HIV status), as well as the PICU outcomes, arterial blood gas on admission and ventilator parameters to obtain the oxygenation index (OI) on admission.
The primary outcome was survival to PICU discharge or death in ICU. Secondary outcomes included duration of mechanical ventilation and length of PICU stay. The prevalence of HIV infection and exposure and malnutrition in this population was specifically sought, given the high burden of HIV among the patients of CHBAH and the opportunity to provide empirical epidemiological data that are not currently available.
Continuous variables were checked using the Shapiro-Wilk test and found to be skewed; they are therefore described using median and interquartile ranges (IQRs). The study population was divided into 3 groups based HIV status (HIV-EU, HIV-U and HIV-infected)
and into 2 groups based on outcome, i.e. alive at discharge or died in PICU. The Mann-Whitney (7-test was used for comparison of two groups and the Kruskal-Wallis test was used to compare three or more groups. The categorical variables were described using percentages and frequencies. Comparisons of proportions were done using the chi-square test or Fisher's exact test where appropriate. A p-value of <0.05 was considered significant.
Survival analysis (Cox regression) was used to determine the independent and interactive effects of age, sex, weight, HIV status and OI as risk factors for mortality, while linear regression was used to determine their association with duration of PICU stay and mechanical ventilation. OI data were collected as a possible predictive factor based on the Paediatric Acute Lung Injury Consensus Conference (PALICC) recommendation for the use of OI to characterise the severity of lung disease in children.[17] OI is defined as (fraction of inspired oxygen (FiO2) χ mean airway pressure (P) χ 100/partial pressure of oxygen in arterial blood (PaO2), where an OI >16 indicates severe paediatric acute respiratory distress syndrome (PARDS).[17]
All statistical analyses were performed using Stata 13 (StataCorp., USA). Anthropometry was analysed using WHO STAT growth charts.
Ethics
Ethical approval was obtained from the Human Research Ethics Committee (HREC (Medical)) at the University of the Witwatersrand (ref. no. M150861).
Results
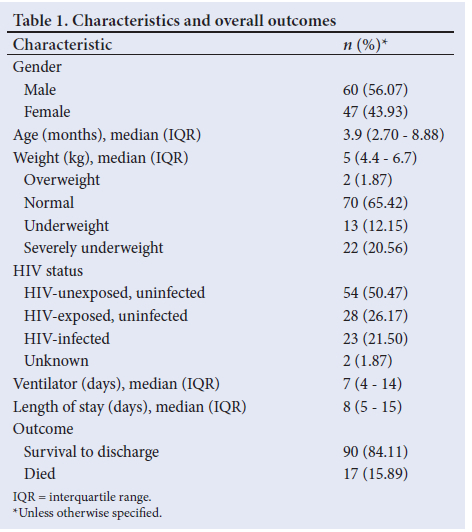
A total of 117 patients were eligible for inclusion in the study; 10 files could not be found in the records room and therefore were excluded from further analysis. Of the remaining 107 patients, 90 (84.11%) were discharged from the PICU and 17 (15.89%) died. There were 60 males (56.07%) and 47 females (43.93%). The median (IQR) age was 3.91 (2.70 - 8.88) months, with ages ranging from 29 days to 9 years 7 months, noting that 78.50% of patients were <1 year of age. The median (IQR) weight was 5.00 (4.40 -6.70) kg. Only 2 children (1.87%) were overweight, 13 (12.15%) were underweight (z-score -2; -3 weight-for-age) and 22 (20.56%) were severely underweight for age (z-score <3 weight-for-age) (Table 1).
HIV status
Eighty-two patients (76.64%) were HIV-negative, 23 (21.50%) patients were HIV-positive, and 2 (1.87%) patients had unknown HIV statuses. Among the HIV-negative patients, 54 (65.85%) were born to HIV-negative mothers and 28 (34.15%) were born to HIV-infected mothers (HIV-EU) (Table 1). The three groups were compared with regard to their baseline characteristics and PICU outcomes (Table 2). There were no significant differences found with respect to sex (p=0.627), age (p=0.972) or weight (p=0.333). The HIV-infected group required significantly more days of mechanical ventilation (p=0.004) and had longer PICU stays (p=0.011). A comparison of HIV-EU with HIV-U patients revealed no significant differences in either their baseline characteristics or PICU outcomes, despite the difference in HIV exposure.
Survival to discharge
The admission OI was independently associated with survival to discharge, with an OI >16 increasing the hazards of death four-fold (adjusted hazard ratio (HR) 4.01; 95% confidence interval (CI) 1.16 - 13.88; p=0.028). Neither HIV exposure (p=0.575) nor infection (p=0.602) was significantly associated with increased mortality among children with pneumonia requiring PICU admission. Lastly, despite age having a statistically significant association with survival to discharge, it has no clinical significance as the adjusted HR was ~1.00 (Table 3).
Duration of mechanical ventilation and length of stay
The median (IQR) length of mechanical ventilation for all patients was 7 (4 - 14) days. Duration of ventilation increased significantly in HIV-infected children compared with HIV-U and HIV-EU children (coefficient = 4.38 (95% CI 0.93 - 7.84); p=0.013 and 5.43 (95% CI 1.53 - 9.33); p=0.007, respectively).
The length of stay in PICU for all patients (survivors and non-survivors) ranged from 1 to 39 days with a median (IQR) stay of 8 (5 -15) days. The median (IQR) length of PICU stay for patients who were discharged (survivors) was 8 (5 - 15) days and 11 (7 - 17) days for non-survivors (p=0.366). The length of PICU stay increased significantly in HIV-infected children compared with HIV-U and HIV-EU children (coefficient = 4.39 (95% CI 0.93 - 7.84) (p=0.013) and 5.43 (95% CI 1.53 - 9.33) (p=0.007), respectively). No other variables were found to be significantly associated with duration of PICU stay.
Oxygenation index
The median (IQR) OI was 10.30 (6.94 - 16.30) with a range of 3 - 51. The median (IQR) OI of surviving patients was 8.80 (5.96 - 14.16) and 23.88 (IQR 14.89 - 36.14) for those patients who died (p=0.005). Patients were grouped using the PALICC definition of severe PARDS, using an OI <16 and an OI >16. An OI >16 was significantly associated with both lower survival to ICU discharge (64.71 v. 93.15%; /<0.001) and longer length of mechanical ventilation (9 v. 7 days; p=0.037). However, the association with longer length of mechanical ventilation was not significant after adjusting for HIV status (adjusted coefficient = 0.11 (95% CI -0.03 - 0.24); p=0.126).
Discussion
This study included 107 participants; 76% (n=82) were HIV-uninfected, of whom two-thirds were HIV-U. The overall survival to discharge was 84%, with chances of survival significantly higher in children with an admission OI <16. Neither HIV exposure nor HIV infection was significantly associated with increased mortality. However, both HIV-EU and HIV-U children had significantly shorter PICU stays and required fewer days of ventilation compared with HIV-infected children.
The overall mortality was in keeping with recent studies which have shown an improvement in survival from 32% to 35% in the early 1990s to 82% to 90% in 2009 - 2011.[15·18-20] However, although it was still slightly higher than that found in high-income countries where overall PICU mortality averages 6%, it is in keeping with their mortality rates for serious bacterial infections and pneumonia (~17.5% in children).[19-21] The median PICU length of stay was 8 days. This finding was similar to those of other PICUs in tertiary institutions in LMICs, ranging from 5 to 8 days.[22]
The prevalence of HIV infection among patients in this study was 22%, nearly twice that reported among general paediatric in-patients at CHBAH in 2012.[21] This was most likely due to selection bias, given the specific subpopulation of pneumonia patients within the study, rather than a reflection of the general incidence of HIV. Thus, this study has established the prevalence of HIV infection among children with pneumonia admitted to an SA public sector PICU.
HIV infection was not associated with increased hazard of death, nor was HIV exposure without infection, which supports current policy that neither HIV infection nor exposure should be a contraindication to the provision of intensive care. However, the HIV-infected group had both significantly longer ICU stays and required a longer duration of mechanical ventilation when compared with either the HIV-EU or HIV-U groups, which is in keeping with the literature.[18,10]
Previous studies have shown that HIV-EU children had similar outcomes to HIV-infected children,[19-11,16,23,24] and therefore warrants consideration as a potentially vulnerable population. However, in this study HIV-EU children had similar outcomes to the HIV-U children, with no statistical differences noted when comparing mortality, length of stay or duration of mechanical ventilation. The lack of any differences in PICU outcomes was somewhat surprising given the emerging reports of increased morbidity and mortality among HIV-EU children.
There is very little published work on OI and outcome in an SA setting. The evidence in this study confirms the prognostic value of an OI >16, given the independent association with lower survival rates.
Study strengths
This study contributes to a growing body of literature to provide locally relevant data on HIV and PICU outcomes, which can serve as reference standards for hospitals with similar disease burdens and patient populations. It also provides valuable insights into the PICU outcomes of HIV-EU children which is critical given the growing size of this population.
Study limitations
Firstly, the retrospective nature of this study meant that we could only analyse data already routinely collected as part of PICU admissions and were forced to exclude participants whose files could not be found. Secondly, weight was the only anthropometrical data recorded in the files so detailed description of the nutritional status of HIV-EU children was not possible, thus limiting the ability to explore the impact of nutritional status on PICU outcomes. We would recommend further research in this area.
Conclusion
HIV infection and exposure were not associated with differences in mortality in this study, suggesting that HIV infection should not be an exclusion criterion for PICU admission. However, HIV-infected children had a significantly longer stay in PICU and longer duration of mechanical ventilation which have resource utilisation implications. HIV EU children do well in PICU and behaved in a similar manner to HIV U children with regard to length of stay, duration of ventilation and survival. OI may be a useful predictor of overall mortality. Further research is recommended to validate its use in PICU decision-making in SA settings.
Declaration. This paper was submitted in partial fulfilment of the requirements for KHK's MMed (Paeds) degree at the University of the Witwatersrand.
Acknowledgements. None.
Author contributions. KHK and KDN contributed to the design of the study; KHK completed data collection; KHK and JP contributed to data analysis; KHK, JP and KDN contributed to final manuscript preparation.
Funding. None.
Conflicts of interest. None.
References
1. World Health Organization. Pneumonia. Geneva: WHO, 2021. https://www.who.int/news-room/fact-sheets/detail/pneumonia (accessed 2 July 2021). [ Links ]
2. Walker CLF, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet 2013;381(9875):1405-1416. https://doi.org/10.1016/s0140-6736(13)60222-6 [ Links ]
3. Delport SD, Brisley T. Aetiology and outcome of severe community-acquired pneumonia in children admitted to a paediatric intensive care unit. S Afr Med J 2002;92(11):907-911. [ Links ]
4. Langley JM, Bradley JS. Defining pneumonia in critically ill infants and children. Pediatr Crit Care Med 2005;6(3 Suppl):S9-S13. https://doi.org/10.1097/01.pcc.0000161932.73262.d7 [ Links ]
5. Rudan I, Boschi-Pinto C, Biloglav Z, Mulholland K, Campbell H. Epidemiology and etiology of childhood pneumonia. Bull World Health Organ 2008;86(5):408-416. https://doi.org/10.2471/blt.07.048769 [ Links ]
6. Jeena PM, McNally LM, Stobie M, Coovadia HM, Adhikari MA, Petros AJ. Challenges in the provision of ICU services to HIV infected children in resource poor settings: A South African case study. J Med Ethics 2005;31(4):226-230. https://doi.org/10.1136/jme.2003.004010 [ Links ]
7. Zar HJ, Apolles P, Argent A, et al. The etiology and outcome of pneumonia in human immunodeficiency virus-infected children admitted to intensive care in a developing country. Pediatr Crit Care Med J Soc Crit Care Med 2001;2(2):108-112. https://doi.org/10.1097/00130478-200104000-00003 [ Links ]
8. Argent AC. Managing HIV in the PICU - the experience at the Red Cross War Memorial Children's Hospital in Cape Town. Indian J Pediatr 2008;75(6):615-620. https://doi.org/10.1007/s12098-008-0118-2 [ Links ]
9. Afran L, Garcia Knight M, Nduati E, Urban BC, Heyderman RS, Rowland-Jones SL. HIV-exposed uninfected children: A growing population with a vulnerable immune system? Clin Exp Immunol 2014;176(1):11-22. https://doi.org/10.1111/cei.12251 [ Links ]
10. Kelly MS, Wirth KE, Steenhoff AP, et al. Treatment failures and excess mortality among HIV-exposed, uninfected children with pneumonia. J Pediatr Infect Dis Soc 2015;4(4):e117-e126. https://doi.org/10.1093/jpids/piu092 [ Links ]
11. Nicholson L, Chisenga M, Siame J, Kasonka L, Filteau S. Growth and health outcomes at school age in HIV-exposed, uninfected Zambian children: Follow-up of two cohorts studied in infancy. BMC Pediatr 2015;15(1):66. https://doi.org/10.1186/s12887-015-0386-8 [ Links ]
12. Goga A, Chirinda W, Ngandu NK, et al. Closing the gaps to eliminate mother-to-child transmission of HIV (MTCT) in South Africa: Understanding MTCT case rates, factors that hinder the monitoring and attainment of targets, and potential game changers. S Afr Med J 2018;108(3a):S17-S24. https://doi.org/10.7196%2FSAMJ.2017.v108i3b.12817 [ Links ]
13. Wessels J, Sherman G, Bamford L, et al. The updated South African National Guideline for the Prevention of Mother-to-Child Transmission of Communicable Infections (2019). South Afr J HIV Med 2020;21(1):8. https://doi.org/10.4102%2Fsajhivmed.v21i1.1079 [ Links ]
14. Moraleda C, de Deus N, Serna-Bolea C, et al. Impact of HIV exposure on health outcomes in HIV-negative infants born to HIV-positive mothers in Sub-Saharan Africa. J Acquir Immune Defic Syndr 2014;65(2):182-189. https://doi.org/10.1097/qai.0000000000000019 [ Links ]
15. Cloete J, Becker P, Masekela R, et al. Severe pneumonia in HIV-infected and exposed infants in a paediatric ICU. S Afr J Child Health 2015;9(3):76-80. https://doi.org/10.7196%2FSAJCH.7941 [ Links ]
16. Von Mollendorf C, von Gottberg A, Tempia S, et al. Increased risk for and mortality from invasive pneumococcal disease in HIV-exposed but uninfected infants aged <1 year in South Africa, 2009 - 2013. Clin Infect Dis 2015;60(9):1346-1356. https://doi.org/10.1093/cid/civ059 [ Links ]
17. The Pediatric Acute. Lung Injury Consensus Conference Group. Pediatric Acute Respiratory Distress Syndrome: Consensus Recommendations From the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med 2015;16(5):428-439. https://doi.org/10.1097%2FPCC.0000000000000350 [ Links ]
18. Jeena PM, Githinji L, Green R. Outcomes of HIV-1-positive children with pneumonia admitted to the paediatric intensive care unit: A retrospective review. Afr J Thorac Crit Care Med 2017;23(3):49-54. https://doi.org/10.7196/SARJ.2017.v23i3.166 [ Links ]
19. Jeena PM, Wesley AG, Coovadia HM. Admission patterns and outcomes in a paediatric intensive care unit in South Africa over a 25-year period (1971 - 1995). Intensive Care Med 1999;25(1):88-94. https://doi.org/10.1007/s001340050792 [ Links ]
20. Riera-Fanego J, Wells M, Lipman J, Luyt D, Dance M, Mathivha L. Demographic and outcome evaluation of a paediatric intensive care unit - Baragwanath Hospital ICU - 6 years' experience, 1989 - 1994. S Afr Med J 1997;87:1586-1590. [ Links ]
21. Mathot F, Duke T, Daley AJ, Butcher T. Bacteremia and pneumonia in a tertiary PICU: An 11-year study. Pediatr Crit Care Med 2015;16(2):104-113. https://doi.org/10.1097/pcc.0000000000000300 [ Links ]
22. Ahmed N. Admission pattern and outcome in a paediatric intensive care unit of a tertiary care paediatric hospital in Bangladesh - a two-year analysis. https://www.academia.edu/7861789/Admission_pattern_and_outcome_in_a_paediatric_intensive_care_ unit_of_a_tertiary_care_paediatric_hospital_in_ Bangladesh_A_two-year_analysis (accessed 2 July 2021). [ Links ]
23. Cotton MF, Slogrove A, Rabie H. Infections in HIV-exposed uninfected children with focus on sub-Saharan Africa. Pediatr Infect Dis J 2014;33(10):1085-1086. https://doi.org/10.1097/inf.0000000000000489 [ Links ]
24. Divala O, Michelo C, Ngwira B. Morbidity and mortality in HIV-exposed under-five children in a rural Malawi setting: A cohort study. J Int AIDS Soc 2014;17(4 Suppl 3):19696. https://doi.org/10.7448/ias.17.4.196960 [ Links ]
 Correspondence:
Correspondence:
K H Keeling
kathkeeling@gmail.com
Accepted 21 July 2021














