Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.16 no.2 Pretoria Jun. 2022
http://dx.doi.org/10.7196/sajch.2022.v16i2.1943
CASE REPORT
Neonatal medium-sized vessel vasculitis: A rare case report
M FallahiI; F AbdollahimajdII, III; S TajalliIV; A RakhshanV; S ShahnavazI; S TabatabaeeVI; F PalizbanI
IMD; Neonatal Health Research Center, Research Institute for Children's Health, Shahid Beheshti University of Medical Sciences, Tehran, Iran
IIMD; Skin Research Center, Shahid Beheshti University of Medical Sciences, Tehran, Iran
IIIMD; Clinical Research Development Unit, Shohada-e-Tajrish Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
IVPhD; Nursing Care Research Center, School of Nursing and Midwifery, Iran University of Medical Sciences, Tehran, Iran
VMD; Department of Pathology, Shohada-e-Tajrish Educational Hospital, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
VIMD; Imam Hossein Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
ABSTRACT
Vasculitis is a rare disorder during the neonatal period. We present a term male neonate of consanguineous parents and birthweight of 4 030 g who presented at 11 days of life with an evolving skin rash. There was no history of drug exposure in the neonate except for routine care. On day 7 of life, multiple erythematous plaques with necrotic or pustular centres appeared. There were no signs of mucosal involvement or sepsis and laboratory findings were normal. Skin biopsy revealed small and intermediate vessel vasculitis. At follow-up 2 weeks after discharge from the hospital, the skin lesions persisted, and at age 2 months, the patient presented with features of severe pneumonia and subsequently died. Vasculitis was reported as the cause of death on postmortem biopsy.
Keywords: neonate; vasculitis; cellulitis; acute oedema of infancy.
Inflammation of the skin and soft tissues is uncommon in healthy neonates, but when it occurs it should primarily be considered as being due to infective or inflammatory processes, most commonly cellulitis. Organisms commonly implicated in neonatal cellulitis include group B Streptococcus (GBS), Staphylococcus aureus, Gram-negative bacteria, anaerobic microorganisms and fungi. In primary neonatal cellulitis, the infection is acquired from the mother during the intrauterine period or during the passage from the vaginal canal, or postnatally from environmental sources. In secondary skin infections, haematogenous spread of microorganisms to the skin occurs during systemic infection, i.e. neonatal sepsis.[1,2] Clinical symptoms of infection such as fever, poor feeding, lethargy, irritability, respiratory distress, vomiting and gastrointestinal problems, along with skin manifestations, support infection as a potential cause of disease. Drug reactions, although uncommon, may cause skin eruptions in the neonatal period.[3,4]
Skin eruptions may be a symptom of systemic disorders other than infections, and may be prominent in patients with vasculitis disorders.
Vasculitis is defined as inflammation of the wall of blood vessels.[5] Its aetiology is not fully understood but during pregnancy the immune system undergoes many changes to accommodate the fetus. Known causes of vasculitis include the following: infections (hepatitis B and Streptococcus spp.); other autoimmune diseases (lupus and scleroderma); and malignancies (leukaemia and lymphoma).[5] The treatment ofvasculitis in infants is not defined and recommendations are based on generalisations from large observational cohort studies in adults. The overall goal of treatment is control of vessel inflammation and prevention of irreversible vascular and organ damage. Corticosteroids are the first-line therapy; however, half of affected children need an additional immunosuppressant. Additionally, intravenous immunoglobulin (IVIG; 2 g/kg) and aspirin should be administered within 10 days of fever onset.[8-11]
The classification and severity of disease are determined based on the size and site of involved vessels, underlying pathophysiology and the extent of vascular injury.[6] Takayasu's arteritis is an example of a large-vessel vasculitis in childhood, whereas Kawasaki disease and polyarteritis nodosa are examples of medium-vessel vasculitis disorders. Henoch-Schonlein purpura is a vasculitic process involving small vessels. The neonatal period is an uncommon time for the presentation of vasculitis and primary neonatal vasculitis is a particularly rare entity.[7]
We report a rare case of neonatal vasculitis presenting with skin manifestations similar to infection-based cellulitis.
Case report
An 11-day-old term male neonate with a birthweight of 4 030 g was delivered by caesarean section from a healthy mother after a normal pregnancy (gravida 1, para 1 miscarriages 0). From the third trimester, the mother received levothyroxine (50 μg daily) to treat primary hypothyroidism. There was parental consanguinity, with no specific family history of vasculitis. There was no history of significant medical problems or drug exposure in the parents. There was no history of drug exposure in the neonate except vaccination with oral poliovirus vaccine, bacille Calmette-Guerin (BCG) and hepatitis B vaccine, and oral vitamin D drops for the first 5 days of life in accordance with routine care in Iran. He was circumcised on the fifth day of life with lidocaine as a local anaesthetic. The patient was breastfed. There were no concurrent symptoms of sepsis such as fever, irritability, poor feeding, lethargy, vomiting, diarrhoea, respiratory distress, or other problems in neonates.
After the appearance of skin lesions, the patient was admitted to a paediatric hospital in his hometown (Qom, Iran) for sepsis work-up and antibiotic treatment. Owing to the lack of improvement, he was referred to our hospital.
From day 7 of life, a disseminated skin rash manifesting as large, targetoid erythematous patches was noted. There were purpuric plaques on the face, trunk, limbs and digits. The proximal, middle and distal phalanges of the middle fingers of both hands were involved. Fig. 1 illustrates the skin lesions. There were no concurrent symptoms of sepsis and no sign of mucosal involvement. The vital signs of the neonate were normal as follows: axillary temperature, 37.2°C; pulse rate, 110 bpm, respiratory rate, 38 bpm; oxygen saturation on room air, 95%. On further examination, he had a mild hydrocele.

He commenced intravenous antibiotic therapy with vancomycin and gentamycin to cover common skin infections, i.e. infection with Staphylococcus spp., group B Streptococcus spp. and Gram-negative bacteria. Antibiotics were administered after culture results were obtained. The white blood cell count (WBC) was 9.7 x 109/L, with 34% polymorphonuclear cells and 56% lymphocytes. The neonate's haemoglobin level was 14 g/dL, and platelets were 301 000/ μL. C-reactive protein (CRP), blood urea nitrogen (BUN) and creatinine levels were normal, and blood, skin lesion, cerebrospinal fluid (CSF) and urine cultures were negative for bacteria.
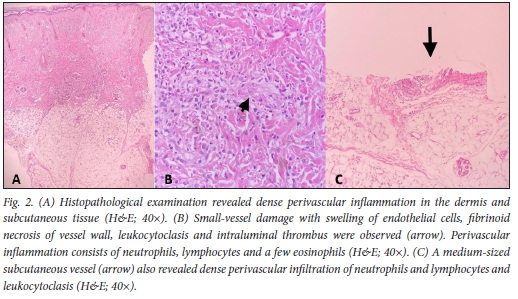
Owing to the lack of improvement of the skin lesions despite antibiotic administration, and after consultation with a dermatologist, a differential diagnosis of acute haemorrhagic oedema of infancy or erythema multiforme was considered, and a skin biopsy was done. Histology confirmed the presence of small and medium-sized vessel vasculitis (Fig. 2). The histological findings were notable in terms of the dense perivascular inflammation in the dermis and subcutaneous tissue, small vessel damage with swelling of endothelial cells, fibrinoid necrosis of the vessel wall, leukocytoclasis and intramural thrombus (arrows in Fig. 2). The perivascular inflammatory infiltrate consisted of neutrophils, lymphocytes and a few eosinophils.
Based on transition course of disease, the consulting dermatologist recommended ongoing immunodeficiency evaluations, as well as conservative supportive care. As the overall condition of the neonate was normal, his parents decided to discharge against medical advice for the provision of continuous evaluations and management of the patient. The patient was discharged in a stable condition with the written consent of the parents and an outpatient work-up for inherited immunological or rheumatological conditions was planned. The autoimmune disease work-up and vasculitis evaluations of both parents were also requested after discharge.
At subsequent follow-up, the skin lesions persisted. In the autumn of 2019, early in the influenza season, the patient died with fulminant respiratory disease (rapidly progressing over 4 - 5 hours) that was non-responsive to medical intervention. He was 2 months old at the time of death. No aetiological agent was identified in the terminal disease episode. A postmortem examination revealed vasculitis as the cause of death.
Discussion
This case was notable for the early onset of idiopathic histologically confirmed vasculitis involving small- and medium-sized blood vessels, and a rapidly fatal course. Vasculitis is an unusual disorder in the neonatal period. Transplacental passage of maternal protein may lead to a transient vasculitis in infants born to mothers with underlying disorders such as Behcet disease, Sjogren's syndrome, systemic lupus erythematosus, undifferentiated connective tissue disease, or microscopic polyarteritis.[12-15]
Although Kawasaki disease is a relatively common form of vasculitis in children, it is rarely reported in neonates.[16] Infantile Henoch-Schonlein purpura, or acute haemorrhagic oedema of infancy (AHEI), is a self-limiting cutaneous vasculitis of small vessels without any systemic involvement that occasionally presents at birth.[12]
AHEI manifests with fever, oedema and large palpable purpuric skin lesions that resemble those seen in Henoch-Schonlein purpura. Conservative management is the most commonly adopted approach in treating AHEI. The skin manifestations of our patient were similar to those observed in AHEI; however, fever and oedema were not significant. The persistence of the skin manifestations and outcome of our patient do not support a diagnosis of AHEI.
In a report by Roy et al.,[16] an 8-month-old male infant presented with skin eruptions which developed following a mild respiratory illness for which amoxicillin-clavulanate and paracetamol were prescribed. The rash consisted of multiple plaques and oval-to-round ecchymotic patches varying in diameter from 2 to 5 cm, involving the arms, hands, face, gluteal area, feet and legs. No histological assessment was done in the diagnostic work-up of the case. Topical application of calamine lotion resulted in resolution of the skin rash.
Allergic reactions to drug administration often involve the skin.[17] In view of the low prevalence of allergy in the neonatal period,[18] and the negative history of drug exposure in our patient, this diagnosis would have been highly unlikely. Malignancies, including lymphoma and other lymphoproliferative syndromes, may result in secondary vasculitis and in cases of persistent vasculitis,[19] malignancy should be considered. Altammar and Lang[20] reported a case of Kawasaki disease in a 15-day-old male who presented with irritability, a rash and poor feeding. Fever (39.6°C), tachypnoea, tachycardia, extreme irritability and a generalised maculopapular rash were noted on physical examination. Bilateral non-purulent conjunctivitis, bilateral non-pitting oedema, palmar erythema, erythema of the feet and arthritis were present on day 6 of hospitalisation. The complete blood count, CRP, and erythrocyte sedimentation rate (ESR) were normal at baseline, but thrombocytosis was detected on day 9 of hospitalisation. Symptoms of the disease resolved subsequent to intravenous immunoglobulin administration. Coronary artery aneurysms were not detected in the echocardiography.[20]
Krapf et al.[21] reported a neonate with fatal myocardial infarction owing to vasculitis of the coronary arteries. Pathological involvement of the coronary arteries is indistinguishable from mucocutaneous lymph node syndrome and/or infantile periarteritis nodosa. The epidemiology and etiology of these rare conditions remain to be clarified.[21]
In a case report by Simonetti et al.,[22] a term neonate with aesophageal atresia requiring surgery on day 2 of life developed respiratory distress, empyema, thrombocytopenia, severe proteinuria, and haematuria with red cell casts on urinalysis, a rise in creatinine level, and a generalized maculopapular rash. Leukocytoclastic vasculitis with marked eosinophilia was detected in the skin biopsy. A 7-day course of intravenous methylprednisolone cured the patient's renal involvement and at long-term follow-up (12 months old) the patient was well.[22]
Primary or secondary vasculitis in the neonatal period can be life-threatening and requires timely diagnosis and treatment. The death of our patient during the early period of seasonal influenza led us to consider that a fulminant viral infection may have contributed to his death. As he died prior to widespread circulation of SARS-CoV-2, his death was not considered to be COVID-19 related. It is a pity that specific viral diagnostic tests were not done in our patient during his terminal admission episode.
Conclusion
Neonatal vasculitis should be considered in infants under 28 days of life who present with the following: widespread skin involvement resembling cellulitis; no concurrent signs and symptoms of sepsis; and no resolution despite antibiotic administration. Timely work-up and laboratory assessment must be done for the initiation of appropriate treatment, and to prevent death in early infancy.
Also, we conclude that the parents need to be investigated for an autoimmune disease.
Declaration. Written informed consent was obtained from the parents of the patient to publish this information and the images of the neonate.
Acknowledgements. The authors would like to thank the staff of the neonatal ward of Mofid Children's Hospital for their sincere co-operation.
Author contributions. MF and FA: study design; MF, FA, and SS: manuscript preparation; ST and ST: critical review.
Funding. None.
Conflicts of interest. None.
References
1. Martic J, Mijac V, Jankovic B, Kandolf Sekulovic L, Vasiljevic Z, Vuksanovic J. Neonatal cellulitis and sepsis caused by group A Streptococcus. Pediatr Dermatol 2010;27(5):528-530. https://doi.org/10.1111/j.1525-1470.2010.01262.x [ Links ]
2. Breinig S, Roques-Gineste M, Marcoux M, Bloom M. Neonatal cellulitis caused by group B Streptococcus. Archives de Pediatrie: Organe Officiel de la Societe Francaise de Pediatrie 2012;19(10):1079-1081. https://doi.org/10.1016/j.arcped.2012.07.015 [ Links ]
3. Priyadharsini R, Surendiran A, Adithan C, Sreenivasan S, Sahoo FK. A study of adverse drug reactions in pediatric patients. J Pharmacol Pharmacother 2011;2(4):277. https://doi.org/10.4103%2F0976-500X.85957 [ Links ]
4. Smyth RMD, Gargon E, Kirkham J, et al. Adverse drug reactions in children - a systematic review. PLoS ONE 2012;7(3):e24061. https://doi.org/10.1371%2Fjournal.pone.0024061 [ Links ]
5. Weiss PF. Pediatric vasculitis. Pediatr Clin 2012;59(2):407-423. https://doi.org/10.1016%2Fj.pcl.2012.03.013 [ Links ]
6. Schnabel A, Hedrich CM. Childhood vasculitis. Front Pediatr 2019;6:421. https://doi.org/10.3389/fped.2018.00421 [ Links ]
7. Sharma A, Gopalakrishan D, Nada R, et al. Uncommon presentations of primary systemic necrotizing vasculitides: The great masquerades. Int J Rheum Dis 2014;17(5):562-572. https://doi.org/10.1111/1756-185x.12223 [ Links ]
8. Aeschlimann FA, Eng SW, Sheikh S, et al. Childhood Takayasu arteritis: Disease course and response to therapy. Arthritis Res Ther 2017;19(1):1-10. https://doi.org/10.1186%2Fs13075-017-1452-4 [ Links ]
9. Wardle AJ, Connolly GM, Seager MJ, Tulloh RM. Corticosteroids for the treatment of Kawasaki disease in children. Cochrane Database Syst Rev 2017(1):CD011188. https://doi.org/10.1002/14651858.cd011188.pub2 [ Links ]
10. Cannon L, Wu EY. Recent advances in pediatric vasculitis. Rheum Dis Clin 2021;47(4):781-796. https://doi.org/10.1016/j.rdc.2021.07.007 [ Links ]
11. Wong S, Demirkaya E, Berard R. A case report of a severe neonatal systemic vasculitis on the first day of life. Pediatr Rheumatol 2021;19:154. https://doi.org/10.1186/s12969-021-00618-x [ Links ]
12. Cunningham BB, Caro WA, Eramo LR. Neonatal acute hemorrhagic edema of childhood: Case report and review of the English-language literature. Pediatr Dermatol 1996;13(1):39-44. https://doi.org/10.1111/j.1525-1470.1996.tb01186.x [ Links ]
13. Boh EE. Neonatal lupus erythematosus. Clin Dermatol 2004;22(2):125-128. https://doi.org/10.1016/j.clindermatol.2003.12.019 [ Links ]
14. Wiik A. Drug-induced vasculitis. Curr Opin Rheumatol 2008;20(1):35-99. https://doi.org/10.1097/BOR.0b013e3282f1331f [ Links ]
15. Fain O, Mathieu E, Lachassinne E, Buisson P, Bodemer C. Neonatal Behcet's disease. Am J Med 1995;98(3):310-311. https://doi.org/10.1016/s0002-9343(99)80382-9 [ Links ]
16. Roy K, Madke B, Kar S, Yadav N. Acute hemorrhagic edema of infancy. Indian J Dermatol 2015;60(6):624-625. https://doi.org/10.4103/0019-5154.169150 [ Links ]
17. Atanaskovic-Markovic M, Gomes E, Cernadas JR, et al. Diagnosis and management of drug-induced anaphylaxis in children: An EAACI position paper. Pediatr Allergy Immunol 2019;30(3):269-276. https://doi.org/10.1111/pai.13034 [ Links ]
18. Chen J, Liao Y, Zhang H-Z, Zhao H, Chen J, Li H-Q. Prevalence of food allergy in children under 2 years of age in three cities in China. Chinese J Pediatr 2012;50(1):5-9. [ Links ]
19. Kermani TA, Warrington KJ, Amin S. Malignancy risk in vasculitis. Ther Adv Musculoskelet Dis 2011;3(1):55-63. https://doi.org/10.1177%2F1759720X10387460 [ Links ]
20. Altammar F, Lang B. Kawasaki disease in the neonate: Case report and literature review. Pediatr Rheumatol 2018;16(1):43. https://doi.org/10.1186%2Fs12969-018-0263-8 [ Links ]
21. Krapf R, Zimmermann A, Stocker F. Lethal vasculitis of coronary arteries in a neonate and two infants: Possible neonatal variant of the MLNS/IPN complex? Helvetica Paediatrica Acta 1981;36(6):589-598. [ Links ]
22. Simonetti G, Markwalder R, Tönz M, Pfenninger J, Bianchetti M. Severe systemic vasculitis in a neonate. Eur J Pediatr 2007;166(4):381-382. https://doi.org/10.1007/s00431-006-0242-9 [ Links ]
 Correspondence:
Correspondence:
S Tajalli
saleheh.tajalli1990@gmail.com
Accepted 3 January 2022














