Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.16 no.2 Pretoria Jun. 2022
http://dx.doi.org/10.7196/sajch.2022.v16i2.1864
RESEARCH
Moderate to severe neonatal encephalopathy with suspected hypoxic-ischaemic encephalopathy in cooled term infants born in Tygerberg Academic Hospital: Characteristics of fetal monitoring and modifiable factors
T AdamsI; D MasonII; G S GebhardtIII
IMMed; Department of Obstetrics and Gynaecology, Faculty of Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
IIMB ChB; Department of Obstetrics and Gynaecology, Faculty of Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
IIIMB ChB, PhD; Department of Obstetrics and Gynaecology, Faculty of Health Sciences, Stellenbosch University and Tygerberg Academic Hospital, Cape Town, South Africa
ABSTRACT
BACKGROUND: In South Africa, in babies >2 500 g, intrapartum asphyxia is the main cause of neonatal death or stillbirth in those who were alive prior to labour. In a developing population, -60% of neonatal encephalopathy (NE) has evidence of intrapartum hypoxic ischaemia. Therapeutic hypothermia for term babies born with NE can improve neonatal prognosis and long-term survival
OBJECTIVES: To identify the healthcare worker- and system-related modifiable factor(s) that were associated with NE in babies of >36 weeks' gestation born at Tygerberg Hospital (a secondary/tertiary referral hospital) between 1 January 2016 and 30 December 2018
METHODS: This was an observational cross-sectional study analysing data from the Tygerberg Hospital Hypoxic Ischaemic Encephalopathy database, the electronic labour ward register, the mortality database and clinical data from patient folders
RESULTS: A total of 118 babies were admitted for head cooling, and therefore included in the study. The hospital in-born rate for serious encephalopathy is 5.5/1 000 in singleton live-born babies (9/1 000 rate for live-born deliveries >36 weeks). A sentinel event was identified in 19 (16%) cases. Delay in accessing theatre was the main system-related modifiable factor (25/58 or 43% of cases delivered by emergency caesarean delivery). The average decision-to-incision time was 1 hour 40 minutes, while the average bed occupancy in the emergency maternity centre was 102%. Failure to recognise or respond to an abnormal cardiotocograph was the dominant avoidable factor related to healthcare workers in 34 cases (36.4%
CONCLUSION: Babies born with severe NE place a burden on parents, healthcare staff and resources. Careful intrapartum care, including utilisation of protocols for the use of oxytocin, are imperative. It is recommended that improved access to emergency theatres and appropriately trained staff for maternity units should be a priority for healthcare planners
Despite modern obstetric practice and a global increase in facility-based births, perinatal morbidity and mortality are still very high in low- to middle-income countries (LMICs). According to the United Nations Children's Fund, there were approximately 2.5 million neonatal deaths (deaths within the first month of life) in 2018, of which almost all occurred in LMICs.[1] In South Africa (SA), birth asphyxia plays a significant role in the perinatal death rate. In the category for term infants (>2 500 g), intrapartum asphyxia is the main cause of stillbirth in babies who were alive before the onset of labour, and the main cause of neonatal deaths.[2]
However, not all babies exposed to intrapartum asphyxia die. It is estimated that in a developing population, 60% of neonatal encephalopathy (NE) has some evidence of intrapartum hypoxic ischaemia.[3] With the increased availability and utility, even in low-resourced settings, of modern neuroprotective methods such as therapeutic hypothermia, there is improved prognosis and long-term survival of these neonates.[4] Children who survive an acquired neonatal brain injury live with a wide spectrum of neurological morbidity ranging from mild affectation to profound cerebral palsy. Even though therapeutic hypothermia may prevent cerebral palsy, emotional, cognitive and motor performance difficulties may become obvious in later childhood.[5] The morbidity that stems from hypoxic-ischaemic encephalopathy (HIE) imposes an immeasurable personal, social and financial cost on the survivor, their family, the healthcare system and society as a whole.[6,7] This forms the basis for justification of the massive medicolegal costs involved with litigation in these cases.
Reasons for these tragic outcomes are often sought in the obstetric sphere. Based on the national Perinatal Problem Identification Programme (PPIP) data of the 2014 - 2016 triennium for SA, there was no decrease in the percentage of babies who died secondary to intrapartum asphyxia.[2] This is despite 76% of women accessing antenatal care and 97% of women being delivered by qualified healthcare providers, therefore suggesting that the contributors to these outcomes are likely multifactorial and deserve scrutiny. Some of these factors extend beyond the control of healthcare workers: for example, no antenatal attendance, delay in transport to hospital, unexpected sentinel events such as cord prolapse or abruptio placentae, intrauterine infection or prematurity. Mothers who deliver at a tertiary/central hospital are referred for specific indications that usually infer underlying maternal risk factors. When delivered at Tygerberg Hospital, at or near term, the expectation is that high-quality care (which includes continuous fetal monitoring and quick access to theatre when indicated) will be available and provided.
Likewise, the baby should have access to a range of post-delivery interventions, including adequate resuscitation, access to high care or neonatal intensive care unit (NICU) and therapeutic hypothermia.
The aim of the present study was to undertake a detailed analysis of a narrowly defined group of babies with NE to determine which obstetric healthcare worker- and/or system-related modifiable factors potentially contributed to adverse neurological outcome.
Methods
This was an observational cross-sectional study using data from the routinely collected Tygerberg HIE database, electronic labour ward register, PPIP mortality database and clinical data from patient folders.
Setting and study population
The study included all infants at a gestation >36 weeks who were delivered at Tygerberg Hospital between 1 January 2016 and 30 December 2018 (a period of 36 months) and were referred to the NICU for therapeutic hypothermia. Babies are considered for this intervention when the following criteria are met: prolonged (>10 minutes) need for resuscitation, and/or a pH <7 or base deficit >16 on cord gas or infant blood within an hour of birth. Additional clinical criteria to be met include moderate to severe encephalopathy seizures or a Thompson HIE score[8] >10.[4]
Babies referred to the Tygerberg NICU from other institutions were excluded, as their prognosis would be influenced by transport availability and the quality of pre-hospital care. The other exclusion criteria were multiple pregnancies, congenital anomalies and congenital viral infection.
Tygerberg Hospital is a large regional and tertiary referral hospital for one-half of the metropolitan area of Cape Town and surrounding rural towns. It serves a predominantly poor socioeconomic population, and has an average of 7 600 deliveries annually. It was classified by the National Department of Health (NDoH) in 2012 as one of 10 central hospitals in SA.
Data analysis
Data were analysed using Excel 365 (Microsoft Corp., USA) and Stata 14 (StataCorp, USA). Demographic characteristics are described with summary statistics such as mean, standard deviation (SD) and range for quantitative variables.
Main outcome measurements
This audit utilised the same broad categories to measure avoidable (or modifiable) factors as are utilised in the SA national PPIP tool: patient-related, healthcare-related and systematic errors that preceded and probably contributed to the event. These are defined as incidents related to the actions of the mother, the healthcare worker or the health system that may have altered the outcome of the specific case had it been managed differently.[9]
Prolonged labour in the first or second stage was defined using the criteria in use at that time in SA (as published in the national Guidelines for Maternity Care in South Africa of 2016).[10] Poor progress in the first (active) phase of labour was defined when there was crossing of the 2-hour action line on the partogram after 4 cm cervical dilatation. Poor progress in the second stage of labour was defined when delivery had not occurred after 30 minutes of pushing (in a multigravida) or 45 minutes of pushing (in a primigrávida).
For intrapartum events, the focus was on fetal monitoring during labour. Cardiotocographic traces were interpreted using the criteria of the National Institute for Health and Care Excellence (NICE)[11] as this is also the system of classification used in daily practice at Tygerberg Hospital. Traces were analysed by three specialist obstetricians, one of whom is a maternal fetal subspecialist. As this was part of the audit, they were not blinded to the outcome.
Definitions and measuring instruments
The bed occupancy rate was calculated as the ratio between the number of occupied beds (based on inpatient admission and discharge data) divided by the number of beds available, with the ratio multiplied by 100 to obtain a percentage.
TBH fetal growth charts were used to correlate gestational age and fetal weight.[12]
Delay in access to emergency theatre was measured as the difference between the time of incision and the time of decision in minutes. The hospital uses the Royal College of Obstetricians and Gynaecologists (RCOG) classification of urgency for caesarean delivery (CD),[13] and a delay of more than 30 minutes for life-threatening cases is regarded as significant at TBH.
Oxytocin for induction or augmentation of labour at TBH is governed by a strict protocol, with a high concentration/low volume dosage regimen starting at 2 milliunits (mU)/min with incremental increase up to a maximum of 20 mU/min. Oxytocin use was regarded as injudicious when there was gross deviation from the protocol, e.g. failure to stop the infusion during severe fetal distress.
The SA NDoH has not published staffing norms for maternity wards in regional or tertiary hospitals in SA, so any modifiable factors relating to staffing norms are mostly subjective. If vital or critical patient information was missed by a midwife, it is difficult to measure whether this was due to inexperience, genuine oversight or too few midwives on duty. For this reason, modifiable factors related to 'insufficient nurses on duty' were not measured, but coded under related items (e.g. fetal distress not detected).
Results
During the audit period there were 20 068 live-born babies in TBH, of whom 13 052 were at >36 weeks' gestation. A total of 118 babies met the criteria for this audit. This equates to a hospital in-born rate of 5.5/1 000 for serious encephalopathy in singleton live-born babies (9/1 000 rate for live-born deliveries >36 weeks' gestation only). As the rate excludes referrals and HIE cases delivered in hospitals outside of Tygerberg, it is not a population-based rate.
Twenty-three babies of > 36 weeks' gestational age died intrapartum owing to severe asphyxia during the time of the audit. As the purpose of the audit was to identify modifiable factors in babies admitted for head cooling, these were not included in the audit, but the results are given here for completeness. Eight of these deaths were due to severe maternal disease (abruptio, severe pre-eclampsia, chorioamnionitis or attempted late abortion), with no healthcare worker-related modifiable factors. In the remaining 15 cases, modifiable factors were identified in 5 (fetal distress not detected in 3 cases and theatre delay in 2).
The mean (SD) age of the birth mothers was 26 (7) years. The median (range) gravidity was 2(1-6) and the median (range) parity 0 (0 - 7). The mean (SD) birthweight of the babies in the study group was 3 086 (576) g.
The bed occupancy rate for the labour ward was 102% during the study period. The hospital CD rate for the study period was 46.4%, and there were 299 vacuum extractions, 312 breech deliveries and 43 forceps deliveries. The corresponding population-based CD rate (for the total hospital referral area) during this time was 25%. The methods of delivery of the study group are given in Fig. 1, showing a significantly higher percentage of instrumental deliveries (16.9% in the study group, v. 1.7% in the total hospital population, p<0.001).
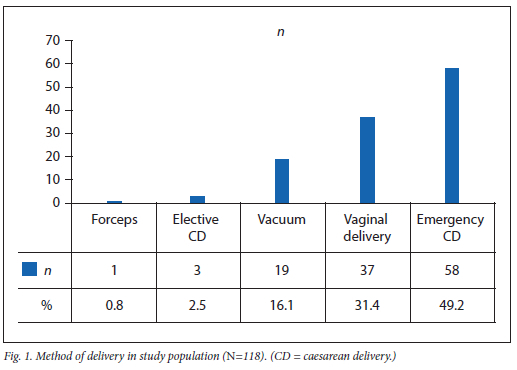
For 8 cases (42%), a vacuum delivery was done for fetal distress as there was no immediate access to theatre. A further 9 vacuum-assisted delivers were done for poor progress in the second stage of labour, and 2 for maternal indications. The other delivery methods had a similar distribution to the general hospital.
All the women in the study were referred for specialist care during the antenatal or intrapartum period, and a number of underlying disorders were identified: hypertensive disease of pregnancy (n=56; 47%); morbid obesity (body mass index (BMI) >40 kg/m2) in 27 women (23%); and overt diabetes (n=9; 7.6%). Some women had more than one underlying condition. Twenty women were HIV-positive (all of them on the standard fixed dose of three antiretroviral drugs).
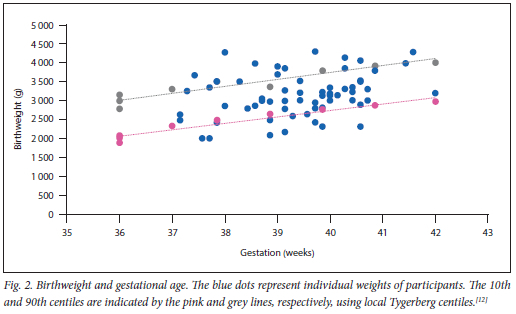
For 73 (62%) of the pregnancies, accurate gestational age was available using early (<24 weeks) ultrasound. Plotting of the birthweight against the growth centiles for these babies reveals that 15% of babies weighed less than the 10th centile and 22% above the 90th centile. This is shown in Fig. 2. Fifty percent (n=7) of the 14 large-for-gestational-age babies were born to mothers with severe obesity (body mass index >40 kg/m2), and a further 4 to mothers with diabetes in pregnancy.
A sentinel event was identified in 19 (16%) cases: 8 shoulder dystocia, 6 abruptio placentae, 3 cord prolapse and 2 cases of uterine rupture.
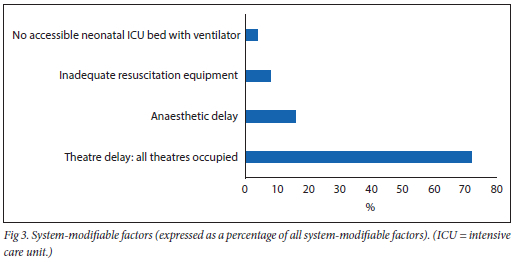
System-related modifiable factors were identified in 18 cases (Fig. 3). The main system-related factor that was deemed avoidable was a delay in getting a patient to theatre once the decision was made for an abdominal delivery (n=25/58 or 43% of cases delivered via emergency CD). The longest waiting time for theatre was 7 hours. This was due to the use of theatre to ventilate another patient until an intensive care unit bed became available. The shortest time interval was 20 minutes. However, on average, the waiting time (decision to incision) was 1 hour and 40 minutes.
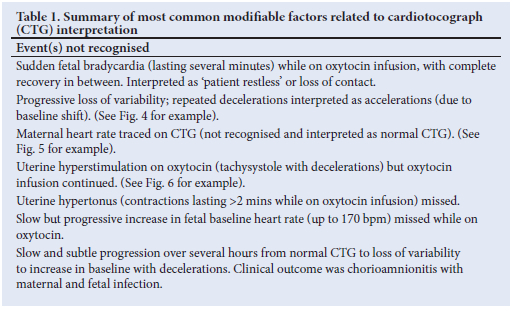
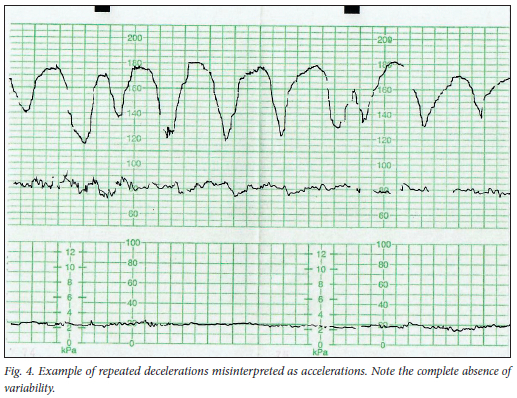
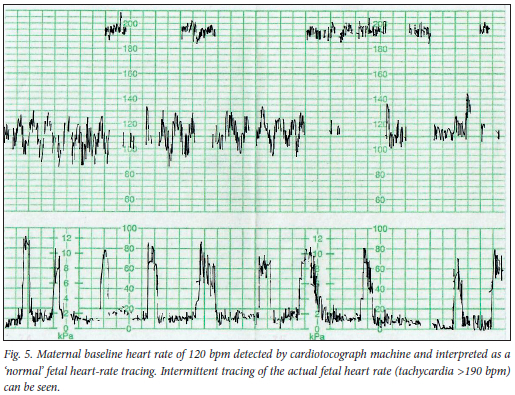
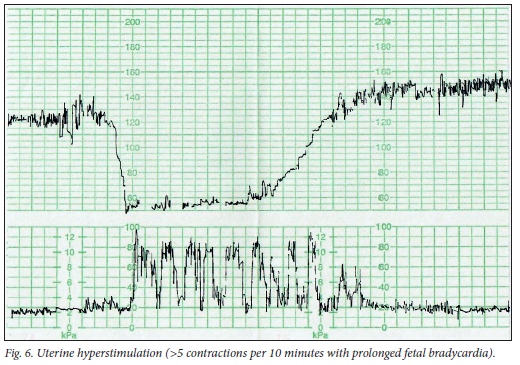
The dominant avoidable factor related to healthcare workers was the failure to recognise or react to abnormal cardiotocograph (CTG) tracings during labour in 34 cases (36.4%). A further 5 cases were not monitored with CTG during labour for various reasons (mostly lack of sufficient monitors). The most common modifiable factors in CTG interpretation are summarised in Table 1, and examples are given in Figs 4-6.
For 22 patients, there was a combination of these two factors: firstly, a lack of recognition of fetal distress, and then a delay getting the patient to theatre once the urgency to deliver was confirmed.
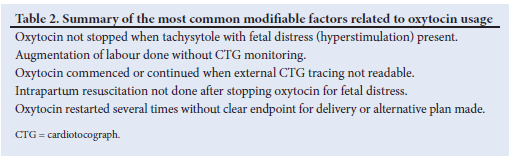
Injudicious use of oxytocin was identified in 16 cases. Many of these were associated with fetal distress, and therefore described above, but a short summary is given in Table 2.
Inadequate clinical assessments, inappropriate management of conditions such as the hypertensive disease spectrum in pregnancy, and inaccurate estimation of fetal size were found in 10 (8.9%) cases.
Prolonged labour was also missed in 10 (8.9%) cases. The partogram was either used incorrectly or, when used, was interpreted incorrectly, in 6 cases (5.4%).
Baby outcome
The long-term neurological findings of the babies will be reported separately, but all infants were tracked for a minimum of 2 years after birth as an indication of outcome. The mean hospital stay for all babies was 13 days, with a range of 3 -103 days. Thirteen babies died during the neonatal period. Of the remaining 105 babies, 11 were lost to follow-up (no evidence of any contact with Western Cape provincial health services anywhere in the province after discharge). The remaining 94 all had follow-up visits at TBH (n=91) or other provincial hospitals (n=3). For the total group, the follow-up visits can be traced for a mean of 80 weeks (3 - 236 weeks). For 25 babies there were continued visits or admissions to TBH >2 years after discharge. The mean number of contacts with healthcare after discharge was 10. The diversity of disciplines visited (including speech therapy, neurology, neurosurgery, cardiology, imaging, respiratory clinics, dietetics, ear, nose and throat and emergency services) is an indication of the impact on health services. The highest number of visits recorded was 111 over 4 years, for 1 of the first babies entered into the audit.
Discussion
This study investigated modifiable obstetric factors in high-risk pregnancies delivering in a large central hospital in SA, where the outcome was moderate to severe NE. Most babies were appropriately grown, but 22% were above the 90th centile for gestation, confirming the high-risk nature of the pregnancies (many women with high BMI or gestational diabetes). The hospital HIE incidence of 5.5/1 000 live births is understandably higher than the 2.3 -4.3/1 000 reported in community settings in SA.[14]
In 19 cases, a sentinel event occurred that was unavoidable. However, for a number of women and babies there was a double insult: a delay in recognising abnormal fetal heart rate tracings and then a further delay (average of 100 minutes) from booking an emergency CD to incision in the skin. This delay was mostly due to another case already occupying theatre (there is only one emergency CD theatre available 24 hours per day). Decision-to-incision time was utilised as a marker for theatre delay in this audit as the alternative measure, incision-to-delivery time, is influenced by factors that will not necessarily be deemed an avoidable factor for HIE, for example BMI, repeat v. primary CD, skill of surgeon and indication for surgery.[15]
Where there is an immediate threat of life to the baby, the ideal decision-to-incision time for an emergency CD is 30 minutes. This is the target used at TBH and therefore for this audit. This target, however, is not often met, even in high-income countries.[13] The NICE guideline on CD urges a category 1 CD (immediate threat to the baby) to be done 'as quickly as possible', and for fetal compromise that is not life-threatening to be done within 75 minutes.[16] Almost half (42%) of the vacuum-assisted deliveries were done for fetal distress where an abdominal delivery was the first choice but no theatre was immediately available.
The central question is why fetal distress was not recognised or managed appropriately in cases where an earlier delivery may potentially have changed the outcome for the baby. TBH has 142 maternity beds in total, of which 34 are in the emergency centre. Since 2012, many quality-improvement measures have been put in place at TBH to decrease morbidity, including a larger consultant presence in the labour ward, reorganisation of working hours and a centralised CTG storing and monitoring system.[17] At night and after hours, when most of the avoidable factors occur, there is one registrar and two medical officers available in the emergency centre (another registrar runs the critical care unit). One doctor continuously runs the theatre, and the remaining two doctors manage all the emergency cases. If one considers ideal circumstances, where a doctor can complete a patient assessment every 15 minutes, the number of patients in the emergency centre would make the next review of that patient only possible ~3 hours later. This situation is not unique to TBH but rather indicative of the critical shortage of doctors in SA, and especially in maternity services.[18] The responsibility for intrapartum care is shared with midwives. Nursing staff who are maternity-trained are in equally short supply in SA.[19]
Similar audits elsewhere in the country have identified the same challenges: ambulance delay (not counted in this audit of in-born babies only), lack of access to theatre and lack of recognition of fetal distress. In an audit of HIE from Mowbray Maternity Hospital in Cape Town, 34% of cases had fetal distress not recognised on CTG.[20]
The second question, central to the high rate of litigation in SA for neurological events following birth trauma,[21] is why babies are still born with hypoxic brain damage despite newer technologies and numerous quality-improvement interventions over the years.[22] Gregerson et al.[23] in 1999 and Buchmann[24] in 2002 alerted the country to the unacceptably high rates of birth asphyxia and NE. For many hospitals, the number of births have increased over the past 20 years without a concomitant increase in infrastructure and staff numbers. Overcrowding in nurseries (in addition to the risk of infectious outbreaks) leads to delay in admission of sick neonates, creating further bottlenecks in an equally overcrowded labour ward.[25]
The injudicious use of oxytocin was a potential important contributor in many of these cases. The SA maternity care guideline follows the RCOG protocol for oxytocin use, starting at a low dose of 2 mU/min, gradually increasing to a high dose of 30 mU/min, which is higher than the maximum (20 mU/ min) allowed at TBH. It is worth pointing out that the physiological dose of oxytocin is equivalent to 4 -6 mU/min, and that doses >16 mU/min do not decrease the CD rate, but can increase the rate of uterine hyperstimulation.[26] Cluver and Odendaal[27] summarise the evidence and dangers of the use of oxytocin in SA.
The strength of this specific audit is that it focuses on inpatient management of complicated pregnancies at the highest level of care available in the state sector in SA. Though not an inherent weakness of the audit, it is noteworthy that many of these women had multiple risk factors, and it would be simplistic to suggest that altering one factor alone would necessarily have resulted in a perfectly normal outcome. High-risk pregnancies preferably need 24-hour specialist-rendered care and one-on-one nursing (the so-called labourist model of obstetric care),[28] an ideal that is difficult to meet even in high-income countries, and certainly unattainable in current SA. The importance of training medical and nursing staff in CTG interpretation, the correct use and interpretation of the partogram and the judicious use of oxytocin in labour cannot be overstated.
Conclusion
Babies born with severe NE represent a catastrophe firstly for the parents, but also have a major impact on medical staff, resources and morale. Careful intrapartum care can potentially reduce some of the risks. Protocols for the use and monitoring of women on oxytocin should be in place in all hospitals in SA. Immediate access to emergency theatres for labour wards, and appropriately trained healthcare workers, should be priorities for healthcare planners.
Declaration. None.
Acknowledgements. The authors thank the management of Tygerberg Hospital for permission to do the audit.
Author contributions. All authors participated equally in writing and revising the manuscript. Each author approved the final version of the manuscript that was submitted for publication.
Funding. None.
Conflicts of interest. None.
References
1. Neonatal mortality. UNICEF DATA, https://data.unicef.org/topic/child-survival/neonatal-mortality/ (accessed 14 August 2020). [ Links ]
2. Gebhardt GS, Rhoda N. Saving Babies 2014 - 2016: Triennial report on perinatal mortality in South Africa. Pretoria: Department of Health, 2018. [ Links ]
3. Kurinczuk JJ, White-Koning M, Badawi N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy Earl Hum Dev 2010;86(6):329-338. https://doi.Org/10.1016/j.earlhumdev.2010.05.010 [ Links ]
4. Kali GTJ, Martinez-Biarge M, Van Zyl J, Smith J, Rutherford M. Therapeutic hypothermia for neonatal hypoxic-ischaemic encephalopathy had favourable outcomes at a referral hospital in a middle-income country ActaPaediatr 2016;105(7):806-815. https://doi.org/10.1111/apa.13392 [ Links ]
5. Lee-Kelland R, JaryS, Tonks J, Cowan FM, ThoresenM,Chakkarapani E. School-age outcomes of children without cerebral palsy cooled for neonatal hypoxic-ischaemic encephalopathy in 2008 - 2010. Arch Dis Child Fetal Neonatal Ed 2020;105(1):8-13. https://doi.org/10.1136/archdischild-2018-316509 [ Links ]
6. Padayachee N, Ballot DE. Outcomes of neonates with perinatal asphyxia at a tertiary academic hospital in Johannesburg, South Africa. S Afr J Child Health 2013;7(3):89. [ Links ]
7. Eunson P The long-term health, social, and financial burden of hypoxic-ischaemic encephalopathy Dev Med Child Neurol 2015;57(S3):48-50. https://doi.org/10.1111/dmcn.12727 [ Links ]
8. Thompson CM, Puterman AS, Linley LL, et al. The value of a scoring system for hypoxic ischaemic encephalopathy in predicting neurodevelopmental outcome. Acta Paediatr 1997;86(7):757-761. https://doi.Org/10.1111/j.1651-2227.1997.tb08581.x [ Links ]
9. Centre for Maternal, Fetal, Newborn and Child healthcare Strategies. Perinatal Problem Identification Program, https://www.up.ac.za/centre-for-maternal-fetal-newborn-and-child-healthcare (accessed 1 April 2021). [ Links ]
10. Guidelines for Maternity Care in South Africa - 2016. Department of Health Knowledge Hub. https://www.knowledgehub.org.za/elibrary/guidelines-maternity-care-south-africa-2016 (accessed 7 April 2021). [ Links ]
11. National Institute for Health and Care Excellence. Intrapartum care for healthy women and babies. London: NICE, 2019. https://www.nice.org.uk/guidance/cgl90 (accessed 7 April 2021). [ Links ]
12. Theron GB, Thompson ML. A centile chart for birth weight for an urban population of the Western Cape. S Afr Med J 1995;85(12):1289-1292. [ Links ]
13. Classification of urgency of caesarean section - a continuum of risk (Good Practice No. 11). Royal College of Obstetricians and Gynaecologists, 2010. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/good-practice-11/ (accessed 13 June 2015). [ Links ]
14. Horn A, Swingler G, Myer L, et al. Defining hypoxic ischemic encephalopathy in newborn infants: Benchmarking in a South African population. J Perinatal Med 2012;41(2). https://doi.org/10.1515/jpm-2012-0107 [ Links ]
15. Rossouw JN, Hall D, Harvey J. Time between skin incision and delivery during cesarean. Int J Gynaecol Obstet 2013;121(l):82-85. https://doi.Org/10.1016/j.ijgo.2012.11.008 [ Links ]
16. Caesarean section. Guidance and guidelines. National Institute for Health and Care Excellence, 2011. http://www.nice.org.uk/guidance/cg132/evidence (accessed 15 June 2015). [ Links ]
17. Gebhardt GS. A critical evaluation of healthcare reform in maternity services in the Western Cape Province of South Africa, 2007 - 2012. PhD thesis. Stellenbosch: Stellenbosch University, 2016. https://scholar.sun.ac.za:443/handle/10019.1/100351 (accessed 26 November 2020). [ Links ]
18. Bateman C. Doctor shortages: Unpacking the 'Cuban solution. S Afr Med J 2013;103(9):603-605. http://doi.org/10.7196/SAMJ.7323 [ Links ]
19. Matlala MS, Lumadi TG. Perceptions of midwives on shortage and retention of staff at a public hospital in Tshwane District. Curationis 2019;42(1):1-10. https://doi.org/10.4102/curationis.v42i1.1952 [ Links ]
20. Dietrich L, Fawcus S, Linley L. A descriptive restrospective audit of the obstetric conditions which occur in mothers of babies with neonatal encephalopathy at Mowbray Maternity hospital in 2016. 39th Conference on Priorities in Perinatal care. 2020. https://www.perinatalpriorities.co.za/proceedings-database/ (accessed 10 November 2020). [ Links ]
21. Pepper MS, Slabbert MN Is South Africa on the verge of a medical malpractice litigation storm? S Afr J Bioethics Law 2011;4(1):29-35. [ Links ]
22. Pattinson R. Does completion of the Essential Steps in the Managing Obstetric Emergencies (ESMOE) training package result in improved knowledge and skills in managing obstetric emergencies? S Afr J Obstet Gynaecol 2009;15(3):94. [ Links ]
23. Gregersen NE, Ballo DE, Guidozzi F, Cooper PA. Birth asphyxia - presenting the case for 'a stitch in time'. S Afr Med J 1999;89(3):329. [ Links ]
24. Buchmann EJ, Pattinson RC, Nyathikazi N. Intrapartum-related birth asphyxia in South Africa: Lessons from the first national perinatal care survey S Afr Med J 2002;92(11):897-901. [ Links ]
25. Dramowski A, Aucamp M, Bekker A, Mehtar S. Infectious disease exposures and outbreaks at a South African neonatal unit with review of neonatal outbreak epidemiology in Africa. Int J Infect Dis 2017;57:79-85. https://doi.org/10.1016/j.ijid.2017.01.026 [ Links ]
26. Hayes EJ, Weinstein L. Improving patient safety and uniformity of care by a standardised regimen for the use of oxytocin. Am J Obstet Gynecol 2008;198(6):622.e1-7. [ Links ]
27. Cluver CA, Odendaal HJ. Oxytocin augmentation: Poison or potion in the multipara? Obstetr Gynaecol For 2010;20(1). https://www.ajol.info/index.php/ogf/article/view/52281 (accessed 12 November 2020). [ Links ]
28. Srinivas SK, Lorch SA. The laborist model of obstetric care: We need more evidence. Am J Obstet Gynecol 2012;207(1):30-35. [ Links ]
 Correspondence:
Correspondence:
G S Gebhardt
gsgeb@sun.ac.za
Accepted 30 April 2021














