Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.16 no.2 Pretoria jun. 2022
http://dx.doi.org/10.7196/sajch.2022.v16i2.1791
RESEARCH
Training, confidence and knowledge of healthcare workers with regard to HIV and infant feeding in eThekwini, South Africa
K A FiddlerI; K PillayII
IMSc (Dietetics); Department of Dietetics and Human Nutrition, College of Agriculture, Engineering and Science, University of KwaZulu-Natal, Pietermaritzburg, South Africa
IIPhD; Department of Dietetics and Human Nutrition, College of Agriculture, Engineering and Science, University of KwaZulu-Natal, Pietermaritzburg, South Africa
ABSTRACT
BACKGROUND: Healthcare workers play an important role in educating mothers living with HIV regarding appropriate infant and young child feeding (IYCF) practices. However, it is not known if healthcare workers in eThekwini, KwaZulu-Natal (KZN), have been adequately trained regarding IYCF in the context of HIV and how knowledgeable and confident they are
OBJECTIVES: To assess the training, confidence and knowledge of healthcare workers regarding IYCF in the context of HIV
METHODS: This was a descriptive cross-sectional study, which used a self-administered questionnaire developed for this survey. Healthcare workers (n=188), primarily doctors and nurses in antiretroviral, antenatal and paediatric departments at three regional hospitals (Addington Hospital, Prince Mshiyeni Memorial Hospital and RK Khan Hospital) in eThekwini, KZN, participated
RESULTS: Only 47.3% (n=89) of the participants had attended formal training on IYCF in the context of HIV. Most participants (n=171; 91.4%) felt they required more training. The mean overall confidence score of the group was 4.54 (standard deviation (SD) 1.28)%. The mean knowledge score of participants regarding IYCF in the context of HIV was 51.7%. The attendance of training did not equate to improved knowledge scores
CONCLUSIONS: Although the healthcare workers were confident with counselling on IYCF in the context of HIV, their knowledge levels were lower than expected. This could be attributed to a lack of training or outdated or inefficient training. There is a need to improve the coverage and quality of IYCF and HIV training. Training courses should address behaviour change and test for understanding
Breastfeeding is recognised globally as the single most effective survival strategy for children <5 years of age.[1] Breastfeeding has protective effects against pneumonia, diarrhoeal disease and malnutrition.[2] The current infant and young child feeding (IYCF) policy in South Africa (SA) strongly recommends exclusive breastfeeding for the first 6 months of an infant's life, followed by the introduction of appropriate complementary foods with continued breastfeeding until >2 years of age.[3,4] This recommendation not only applies to infants and young children in the general population, but also to those of mothers living with HIV.[4] Furthermore, it is in alignment with the 2016 World Health Organization (WHO) guideline on HIV and infant feeding.[2] There is a low risk of HIV transmission from mother to child through breastmilk, with a risk of 0.19% per month in the case of diligent antiretroviral therapy (ART) use.[5] It is clear that the benefits of breastfeeding outweigh the risk of HIV transmission.[2]
However, breastfeeding was not always encouraged for mothers living with HIV. Many changes have been made to the SA prevention of mother-to-child transmission (PMTCT) of HIV programme over the years, including changes to the IYCF recommendations.[4,6,7] Some of these changes include whether mothers living with HIV should breastfeed or not; the duration of breastfeeding; whether mothers should abruptly or gradually stop breastfeeding; and which ART drugs mothers living with HIV should receive.[4,6,7] Ongoing changes to guidelines have the potential to confuse healthcare workers.[8,9] Several African studies found that healthcare workers have poor knowledge regarding IYCF guidelines in the context of HIV.[9-12] This is of concern, as mothers living with HIV require clear, up-to-date and consistent IYCF messages and support.[13] However, it is not known if healthcare workers in eThekwini, KwaZulu-Natal (KZN), have been adequately trained in IYCF in the context of HIV and how knowledgeable and confident they are. Therefore, the aim of this study was to assess the training, knowledge and confidence of healthcare workers, primarily doctors and nurses, employed at eThekwini, KZN regional state hospitals' antiretroviral (ARV), paediatric and antenatal departments, regarding IYCF in the context of HIV.
Methods
Study design and setting
This descriptive cross-sectional study was conducted between July and December 2018 at three eThekwini regional hospitals (Addington Hospital, Prince Mshiyeni Memorial Hospital and RK Khan Hospital). Data were collected intermittently over this period and the days chosen for data collection varied between the different hospitals and departments, depending on the availability of healthcare workers.
Study population and sample selection
Only permanently employed medical officers, medical registrars, medical consultants, enrolled nurses, professional nurses and other healthcare workers at the three hospitals' ARV, paediatric and antenatal departments were considered for inclusion in the study. A convenience sample was used, as only those healthcare workers who met the inclusion criteria and were on duty on the days of data collection were invited to participate in the study.
Self-administered questionnaire
A self-administered questionnaire with primarily closed-ended questions was developed for the study. The questionnaire was based on recommendations included in the National Department of Health (NDoH) 2013 Infant and Young Child Feeding Policy,[3] the 2017 Amendment of the 2013 Infant and Young Child Feeding Policy[4] and the 2015 National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults.[6]
A panel of experts reviewed the questionnaire to ensure content validity. The questionnaire consisted of 8 sections: (i) demographic information; (ii) training on HIV and IYCF; (iii) counselling on HIV and IYCF; (iv) confidence to counsel mothers living with HIV on different aspects of IYCF; (v) knowledge of IYCF; (vi) knowledge of risk of HIV transmission; (vii) understanding of key terms, determining ART compliance and recommendations; and (viii) opinions on guidelines, compliance and practices. However, responses to sections (iii) and (viii) are not reported in this article.
The confidence section involved participants' ranking of how confident they felt counselling mothers living with HIV on IYCF principles in 14 different scenarios. This was assessed using a 6-point Likert scale, where 1 = not at all confident and 6 = very confident. An overall knowledge score was given to the participants by combining the scores from the knowledge questions. The first knowledge section included 17 true/false questions, which tested knowledge of different IYCF principles. The second knowledge section included 4 multiple-choice questions regarding the risk of HIV transmission through breastfeeding in different scenarios. The final knowledge section included open-ended questions.
The first open-ended question asked participants what they understood by the term 'exclusive breastfeeding. The WHO defines exclusive breastfeeding as 'providing breast milk without any liquids or solids, not even water, except for oral rehydration solution or drops or syrups of vitamins, minerals or medicines'. This definition was divided into 3 components for scoring the answers: (i) an infant receives only breastmilk; (ii) no other liquids or solids; and (iii) with the exception of drops or syrups consisting of vitamins, mineral supplements or medicines. If an answer included all 3 components of the definition, this was scored as 'excellent' knowledge and given a score of 100%. If an answer included the first and either of the other components, this was scored as 'good' knowledge and given a score of 66.7%. If only the first component was mentioned, the answer was scored as 'average' knowledge and given a score of 33.3%. If the respondent's answer was completely inappropriate, their knowledge was scored as 'poor' and they were scored 0%.
The second open-ended question asked participants what they understood by the term 'treatment failure'. Treatment failure is defined by the National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults[6] as 'a persistently detectable viral load <1 000 copies/mL, i.e. 2 consecutive viral load measurements within a 2-month interval, with adherence support between measurements, after at least 6 months of using ART drugs'.[6] Participants' answers were scored out of 3. If their answer included having multiple (>2) persistently high viral load readings after using ART for at least 6 months with good adherence, their answer was scored as 'excellent' and a 100% score was awarded. If their answer included having multiple (>2) persistently high viral load readings after using ART for at least 6 months, but adherence was not mentioned, their answer was scored as 'good' and they were given 66.7%. If their answer only mentioned the patient being on ART, but still having a high viral load, their answer was scored as 'average' and they were awarded 33.3%. Incorrect answers, those that did not mention the use of ART or those that mentioned poor adherence as a cause of treatment failure were scored as 'poor' and given 0%.
The third open-ended question asked participants to briefly describe how they would determine ART compliance in pregnant/ lactating women living with HIV. Strategies to assess ART compliance mentioned in the National Antiretroviral Treatment Guidelines, 2004, include: (i) blood tests; (ii) ARV pill-returns count; (iii) routine adherence discussions (self-reports); and (iv) attendance of follow-up visits.[14] Answers that included any of these methods or any other acceptable methods for determining ART compliance (such as clinical assessments) were scored as 'correct' and given 100%. Incorrect answers were given 0%.
The last open-ended question asked when participants would recommend that a mother living with HIV stops breastfeeding. The IYCF policy in SA recommends that mothers living with HIV should continue breastfeeding for 24 months.[3,6] Therefore, it is recommended that these mothers should discontinue breastfeeding at 24 months. However, the guideline also recommends that pregnant and breastfeeding mothers, who have confirmed treatment failure, should not breastfeed their infants owing to the increased risk of mother-to-child transmission, with poor viral suppression. Other medical contraindications for breastfeeding are also listed in the IYCF policy.[3] Answers that included any of the abovementioned scenarios as an appropriate time to recommend a mother to stop breastfeeding were accepted as correct, and the respondent was scored 100% for their answer. Answers that included incorrect and correct information were considered partially correct and scored 50%. Incorrect answers were given 0%.
Data analysis
Responses to the knowledge questions were scored using the recommendations included in the NDoH 2013 IYCF policy,[3] the 2017 amendment of the IYCF policy[4] and the 2015 consolidated guidelines for PMTCT and the management of HIV in children, adolescents and adults.[6] Unanswered questions that investigated knowledge were scored as incorrect. Data were entered into Microsoft Excel (Microsoft Inc., USA) by the researcher and cross-checked by a research assistant to ensure accuracy in data capture. Data were analysed using SPSS, version 22 (IBM Corp., USA). Descriptive statistics, i.e. frequencies and percentages for categorical data and medians and percentiles for continuous data, were calculated. Relationships between variables were calculated and described using 95% confidence intervals (CIs) for differences in medians or percentages. A p-value of <0.05 was considered significant.
Ethical approval
Ethical approval was obtained from the Biomedical Research Ethics Committee of the University of KZN (ref. no. HSS/0296/018M), as well as from the Research Committee, KZN Department of Health (ref. no. HRKM129/18). All participants gave written consent prior to answering the questionnaire. The researcher informed the participants that their participation was voluntary and anonymous, that there were no risks associated with participation and that there would be no remuneration for participation.
Results
Eligible doctors and nurses on duty on data collection days were used to calculate the response rate for the study. The total response rate was 82.2% (n=175). Thirteen other eligible healthcare workers from other departments or professions also participated in the study.
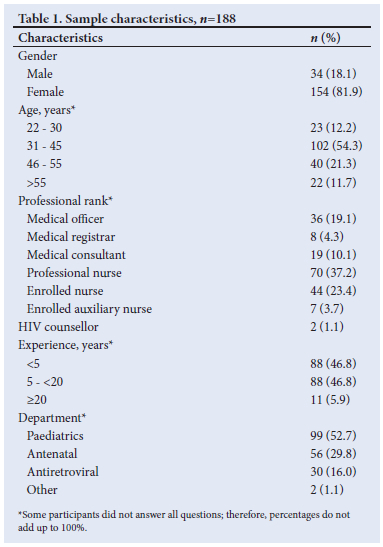
However, they were not included in the response rate calculation, as it was not known how many of them were on duty on the data collection days. This resulted in a total number of participants of 188, some of whom did not answer all questions; the missing data are reported. Table 1 presents the sample characteristics. Just over 81% of the sample (n=154) were female, with 18.1% (n=34) male. The largest group of participants was between 31 and 45 years old (54.3%; n=102). Seventy (37.2%) professional nurses participated in the study, followed by 44 (23.4%) enrolled nurses and 36 (19.1%) medical officers. Equal numbers of participants (46.8%; n=88) had <5 years' experience and between 5 and <20 years of experience, respectively. The majority of participants worked in the paediatrics department (52.7%; n=99), followed by the antenatal department (29.8%; n=56).
Training
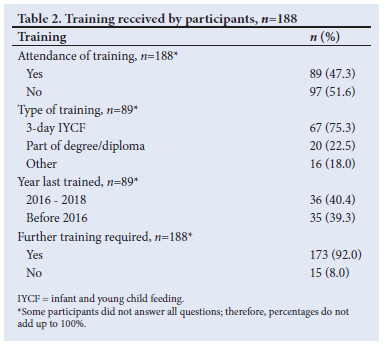
More than half of the participants (n=97; 51.6%) indicated that they had not been formally trained on IYCF in the context of HIV (Table 2). Of the 89 who indicated that they had attended training, 67 (75.3%) had attended the NDoH 3-day ICYF training (an adaptation of the Baby-friendly Hospital Initiative (BFHI) training course developed by the WHO and United Nations Children's Fund (UNICEF)).[15] Twenty participants (22.5%) indicated that they had been trained as part of their formal degree or diploma and 16 (18.0%) that they had received 'other' training. Only 36 (40.4%) of the 89 who had attended IYCF training specified that they had received training during the previous 2 years. One hundred and seventy-three participants (n=92.0%) indicated a need for further training on HIV and IYCF guidelines.
Confidence
Participants were asked to rank how confident they were with counselling mothers living with HIV regarding IYCF principles in different scenarios (Table 3). The majority of participants were found to be confident in all counselling scenarios and the mean overall confidence score for the group was 4.54 (standard deviation (SD)1.28)%.
Knowledge
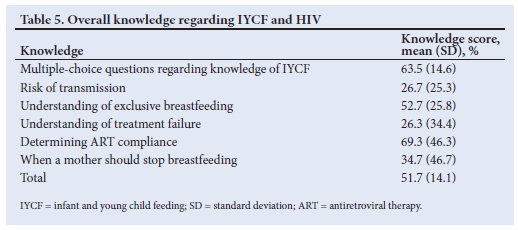
The participants scored a mean of 63.5 (14.6)% for the true/false questions. For the section pertaining to the risk of transmission, the participants had a mean score of 26.7 (25.3)% (Table 4). For the open-ended questions, the participants scored a mean of 52.7 (25.8)% for the definition of exclusive breastfeeding; a mean of 26.3 (34.4)% for the understanding of treatment failure; a mean of 69.3 (46.3)% for determining ART compliance in pregnant/lactating women living with HIV; and a mean of 34.7 (46.7)% for when a mother living with HIV should stop breastfeeding.
The mean knowledge score of the participants was 51.7 (14.1)% (Table 5). No significant relationship was found between the attendance of training and mean knowledge scores (p=0.217).
Discussion
According to the WHO, a clear and well-supported policy, coupled with appropriate training of healthcare workers, is of upmost importance for the successful implementation of an IYCF policy.[16] Despite SA having a comprehensive IYCF policy that states clear guidelines regarding HIV, this study shows that the majority of healthcare workers were insufficiently trained in the HIV component of this policy. This result was unexpected, as all three facilities were Mother-Baby-Friendly Initiative accredited (an adaptation of the BFHI) at the time of the study. This accreditation requires that a minimum of 80% of clinical staff who are in contact with mothers and/or infants must have attended the 3-day IYCF training course offered by the NDoH.[17] The lack of IYCF and HIV training has proven to be a recurrent issue in other African studies.[18-21] This is of concern, as it is essential for healthcare workers to be equipped with the necessary knowledge needed to successfully implement IYCF policies and provide appropriate counselling to mothers.[18] An additional concern is that, in the current study, the healthcare workers who had undergone training were not significantly more knowledgeable than those who had not been trained. Of the participants who received training in this field, three-quarters received training through the 3-day training course offered by the NDoH. This begs us to question the efficacy of this initiative. Moreover, it may be relevant that of the participants who attended the NDoH 3-day IYCF training course, just >40% had done so within the previous 2 years, which may have possibly contributed to the poor knowledge demonstrated. It is likely that these participants may have forgotten a significant amount of what they had learnt or that the training content was outdated.
Healthcare workers in ARV, paediatric and antenatal departments are responsible for the counselling of mothers living with HIV regarding IYCF.[17] A study by Horwood et al.[22] found that SA mothers living with HIV diligently followed the IYCF advice given by healthcare workers, and perceived healthcare workers to be knowledgeable professionals who provide accurate advice. If healthcare workers are not knowledgeable about IYCF, it is likely that they will share incorrect messages with mothers, which in turn could lead to poor IYCF practices.[22] The healthcare workers in the current study were not considered to be adequately knowledgeable about IYCF in the context of HIV, with a mean knowledge score of only 51.7%.
Many participants grossly overestimated the risk of HIV transmission through breastfeeding. This may be due to early PMTCT guidelines, which encouraged mothers to formula feed their infants if they were able to.[2] Many of the participants incorrectly associated mixed feeding with the use of ART, with a much higher risk of HIV transmission. The belief that breastfeeding carries a relatively high risk of HIV transmission may cause healthcare workers to be less supportive of breastfeeding. More than half of the total number of participants estimated the risk of transmission to be > 20%, much higher than the actual risk of 1.13%.[5] Although not relevant at the time of data collection, in 2019 SA adopted the WHO 2016 guiding practice statement, 'Mothers living with HIV and healthcare workers can be reassured that ART reduces the risk of postnatal HIV transmission in the context of mixed feeding. Although exclusive breastfeeding is recommended, practising mixed feeding with formula milk is not a reason to stop breastfeeding in the presence of ARV drugs.'[23] Increased awareness is likely needed regarding the effectiveness of ART in reducing the risk of HIV transmission through breastfeeding, including in cases of mixed feeding, before healthcare workers adopt this recommendation.
The participants had a poor understanding of the term 'exclusive breastfeeding', with a mean score of 52.7%, and only 8.5% of participants showed an excellent understanding of the term and 48.9% a good understanding. This is of concern, as these healthcare workers should be encouraging mothers living with HIV to exclusively breastfeed their infants for the first 6 months of life, as per the country's IYCF policy.[3] Without a proper understanding of the term, it is possible that inadequate or inaccurate information is shared with mothers. A similar study by Van Rensburg et al.'9] found that 70.0% of healthcare workers knew that exclusive breastfeeding meant that only breastmilk should be given, but only 6.7% of healthcare workers could comprehensively explain the term. However, they used a different definition for the term to that in the current study.[9]
In SA, confirmed treatment failure is a contraindication for breastfeeding due to the increased risk of mother-to-child transmission with poor viral suppression.[6] The participants in the current study had a very poor understanding of the term 'treatment failure'. Treatment failure can only be diagnosed in patients who are compliant with their ART. Yet, 35.5% of participants incorrectly described treatment failure as the occurrence of a high viral load because of poor adherence. With poor adherence, it would be expected that the viral load would not be adequately suppressed owing to insufficient ART rather than ineffective ART. If treatment failure is misdiagnosed, a healthcare worker may discourage a mother from breastfeeding her infant. The poor understanding of treatment failure is not only of concern with regard to IYCF, but for overall HIV management.
The participants scored poorly (34.7%) when asked when they would recommend a mother living with HIV to stop breastfeeding. It is a serious concern that many healthcare workers would encourage mothers to discontinue breastfeeding in cases where it is not contraindicated. Incorrect answers frequently given included 'at 6 months' and 'at 1 year. These answers may have been given as a result ofprevious guidelines, which recommended these periods (6 months of breastfeeding was recommended in the 2008 PMTCT guideline, and prior to its 2017 amendment, the 2013 IYCF policy recommended breastfeeding until 1 year of age).[3,4,24] This illustrates a lack of awareness of or a lack of support for the current recommendations.
Overall, the healthcare workers in the study were found to be confident with counselling mothers living with HIV regarding IYCF practices. The more confident a healthcare worker is, the more effective they are at influencing a mother's feeding choice.[25] While it is reassuring to know that healthcare workers are confident with the counselling of mothers living with HIV regarding IYCF, it is a concern that they lack the accompanying knowledge. With high levels of confidence and poor IYCF knowledge, it is possible that these healthcare workers may be contributing to poor feeding practices of mothers living with HIV.
There is a need to improve the coverage of IYCF and HIV training in the three facilities, as well as the quality of training. Training courses should address behaviour change and test for understanding. Facilities need to ensure that guidelines, policies and updates are effectively disseminated to their healthcare workers and that these workers are accountable for the correct implementation of the relevant guidelines and policies. Further research is needed to determine which IYCF and HIV training strategies effectively improve knowledge levels.
Study limitations
The study was limited, as only three regional hospitals in eThekwini participated. These findings are not representative of all the healthcare workers in eThekwini and generalised conclusions cannot be drawn. In addition, many study participants were not supervised when completing their questionnaires owing to logistical limitations. It is possible that some participants could have discussed the questions with each other or looked up the answers. Another limitation was that, although efforts were made to avoid leading questions in the questionnaire, the use of predetermined questions might have introduced bias.
Conclusions
This study identified a lack of training regarding IYCF in the context of HIV among the healthcare workers who participated. Of particular concern is that the attendance of training was not associated with significantly higher knowledge scores. This study highlights a need for improved training on IYCF in the context of HIV at the three hospitals involved in the study. Although the healthcare workers in this study were found to be confident regarding HIV and IYCF counselling, their knowledge level was lower than expected, which could be attributed to a lack of training, outdated training or inefficient training. The coverage and quality of IYCF and HIV training need to be improved. Furthermore, training courses should address the application of knowledge and should test for understanding. Future research should investigate the effectiveness of the different IYCF and HIV training strategies in improving knowledge levels. The impact of IYCF counselling of mothers living with HIV with regard to infant feeding decisions, should also be further investigated.
Declaration. The research for this study was done in partial fulfilment of the requirements for KAF's MSc (Dietetics) degree at the University of KwaZulu-Natal.
Acknowledgements. The authors thank the study participants for their involvement in the study, and Gill Henry for the statistical analysis of the data.
Author contributions. KAF and KP designed the study and developed the methodology. KAF collected the data. KAF prepared the manuscript with input from KP. The study was supervised by KP.
Funding. None.
Conflicts of interest. None.
References
1. Victora CG, Bahl R, Barros AJD, et al. Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet 2016;387(10017):475-490. https://doi.org/10.1016/S0140-6736(15)01024-7 [ Links ]
2. World Health Organization. Guideline: Updates on HIV and Infant Feeding: The Duration of Breastfeeding, and Support from Health Services to Improve Feeding Practices among Mothers Living with HIV. Geneva: WHO, 2016. [ Links ]
3. National Department of Health. Infant and Young Child Feeding Policy. Pretoria: NDoH, 2013. [ Links ]
4. National Department of Health. Amendment of the 2013 Infant and Young Child Feeding (IYCF) Policy. Pretoria: NDoH, 2017. [ Links ]
5. World Health Organization. Revisiting Optimal Breast Feeding Durations: Modelling the Impact of Maternal ARV Use and Infant Mortality. Geneva: WHO, 2015. [ Links ]
6. National Department of Health. National Consolidated Guidelines for the Prevention of Mother-to-Child Transmission of HIV (PMTCT) and the Management of HIV in Children, Adolescents and Adults. Pretoria: NDoH, 2015. [ Links ]
7. Burton R, Giddy J, Stinson K. Prevention of mother-to-child transmission in South Africa: An ever-changing landscape. Obstet Med 2015;8(1):5-12. https://doi.org/10.1177/1753495X15570994 [ Links ]
8. Shayo EH, Vaga BB, Moland KM, Kamuzora P, Blystad A. Challenges of disseminating clinical practice guidelines in a weak health system: The case of HIV and infant feeding recommendations in Tanzania. Int Breastfeed J 2014;9(188):1-13. https://doi.org/10.1186/s13006-014-0024-3 [ Links ]
9. Van Rensburg LJ, Nel R, Walsh CM. Knowledge, opinions and practices of healthcare workers related to infant feeding in the context of HIV. Health SA Gesondheid 2016;21(a943):129-136. https://doi.org/10.4102/hsag.v21i0.943 [ Links ]
10. Adetokunboh OO, Oluwasanu M. Eliminating mother-to-child transmission of the human immunodeficiency virus in sub-Saharan Africa: The journey so far and what remains to be done. J Infect Public Health 2016;9(4):396-407. https://doi.org/10.1016/j.jiph.2015.06.010 [ Links ]
11. Murila F, Obimbo MM, Musoke R, Tsikhutsu I, Migiro S, Ogengo J. Breastfeeding and human immunodeficiency virus infection: Assessment of knowledge among clinicians in Kenya. Int J Nurs Pract 2015;21(1):27-42. https://doi.org/10.1111/ijn.12218 [ Links ]
12. Sint TT, Lovich R, Hammond W, et al. Challenges in infant and young child nutrition in the context of HIV. AIDS 2013;27(Suppl 2):S169-S177. https://doi.org/10.1097/qad.0000000000000089 [ Links ]
13. West NS, Schwartz SR, Yende N, et al. Infant feeding by South African mothers living with HIV: Implications for future training of health care workers and the need for consistent counselling. Int Breastfeed J 2019;14(11):1-7. https://doi.org/10.1186/s13006-019-0205-1 [ Links ]
14. National Department of Health. National Antiretroviral Treatment Guidelines. Pretoria: NDoH, 2004. [ Links ]
15. National Department of Health. A Breastfeeding Course for Health Care Providers: Toolkit. Pretoria: NDoH, 2014. [ Links ]
16. World Health Organization. Global Strategy for Infant and Young Child Feeding. Geneva: WHO, 2003. [ Links ]
17. KwaZulu-Natal Department of Health. Guidelines for the Implementation of the Mother Baby Friendly Initiative in KwaZulu-Natal Healthcare Facilities. Pietermaritzburg: KZN DoH, 2017. [ Links ]
18. Mphasha MH, Skaal L. Infant and young child feeding policy: Do primary health care nurses adhere to the HIV breastfeeding recommendations in Limpopo province? S Afr J Clin Nutr 2019;4(1):1-6. https://doi.org/10.1080/16070658.2018.1457863 [ Links ]
19. Rujumba J, Tumwine JK, Tylleskar T, Neema S, Heggenhougen HK. Listening to health workers: Lessons from Eastern Uganda for strengthening the programme for the prevention of mother-to-child transmission of HIV. BMC Health Serv Res 2012;12(3):1-12. https://doi.org/10.1186/1472-6963-12-3 [ Links ]
20. Leshabari SC, Blystad A, de Paoli M, Moland KM. HIV and infant feeding counselling: Challenges faced by nurse-counsellors in northern Tanzania. Hum Resour Health 2007;5(18):11. https://doi.org/10.1186/1478-4491-5-18 [ Links ]
21. Piwoz EG, Ferguson YO, Bentley ME, et al. Differences between international recommendations on breastfeeding in the presence of HIV and the attitudes and counseling messages of health workers in Lilongwe, Malawi. Int Breastfeed J 2006;1(2):1-8. https://doi.org/10.1186/1746-4358-1-2 [ Links ]
22. Horwood C, Jama NA, Haskins L, Coutsoudis A, Spies L. A qualitative study exploring infant feeding decision-making between birth and 6 months among HIV-positive mothers. Matern Child Nutr 2019;15(2):1-13. https://doi.org/10.1111/mcn.12726 [ Links ]
23. National Department of Health. Guideline for the Prevention of Mother to Child Transmission of Communicable Infections (HIV, Hepatitis, Listeriosis, Malaria, Syphilis and TB). Pretoria: NDoH, 2019. [ Links ]
24. National Department of Health. Policy and Guidelines for the Implementation of the PMTCT Programme. Pretoria: NDoH, 2008. [ Links ]
25. Schmied V, Beake S, Sheehan A, McCourt C, Dykes F. Women's perceptions and experiences of breastfeeding support: A metasynthesis. Birth 2011;38(1):49-60. https://doi.org/10.1111/j.1523-536x.2010.00446.x [ Links ]
 Correspondence:
Correspondence:
K A Fiddler
katenuns@gmail.com
Accepted 7 May 2021














