Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.16 no.2 Pretoria Jun. 2022
http://dx.doi.org/10.7196/sajch.2022.v16i2.1783
RESEARCH
Male partners' experiences of early pregnancy ultrasound scans in Soweto, South Africa: The Healthy Pregnancy, Healthy Baby randomised trial
R E DrysdaleI; W StemmingII; T MakushaI, III, IV; L M RichterI
IPhD; DSI-NRF Centre of Excellence in Human Development, University of the Witwatersrand, Johannesburg, South Africa
IIPhD; Division of Community Paediatrics, Department of Paediatrics and Child Health, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
IIIPhD; Human Sciences Research Council, Pretoria, South Africa
IVPhD; MRC/Wits Developmental Pathways for Health Research Unit (DPHRU), Johannesburg, South Africa
ABSTRACT
BACKGROUND: Despite international evidence highlighting the benefits of male partners attending antenatal visits, including pregnancy ultrasound scans, it is unusual for South African (SA) men to attend such visits, and little is known about their experiences if they do
OBJECTIVES: To explore the experiences and antenatal attachment among male partners who attend early pregnancy ultrasound examinations in Soweto, SA
METHODS: Pregnant women attending ultrasound examinations were invited to bring their partners with them. Both completed individual questionnaires, including the antenatal attachment scale. The results are based on a descriptive analysis of 102 mother-partner pairs
RESULTS: The mean age of partners was 35 years. Only 32% of men were living with their pregnant partner. Before the ultrasound scan, 64% of men reported feeling very anxious, while 54% also felt anxious after the procedure. The ultrasound examination had a positive effect on men and their thoughts regarding their developing baby, with 30% stating that they were ready or excited to be a father. Twenty-eight percent believed their relationship with the mother was stronger as a result of participating in antenatal care
CONCLUSIONS: We found that prenatal ultrasound scans had a positive effect on male partners and their thoughts about the pregnancy, their forthcoming child and their relationship with and support for their partner. Health services in SA should accommodate partners/ fathers and encourage them to attend antenatal care, including pregnancy ultrasound scans. Interventions are needed to encourage more men to be involved - from conception - potentially addressing individual, familial, societal and structural barriers to involvement of the father in long-term maternal and child care
Research and interventions for pregnancy, antenatal care, maternal and child health and education focus mainly on mothers and children. Although the literature on male involvement during pregnancy and their experiences of antenatal services such as ultrasound scans is increasing, these factors remain limited in low-and middle-income countries (LMICs).[1] Fathers or male partners can play an important role by providing practical, emotional and financial support to their expectant partners. They can promote maternal health and wellbeing by encouraging positive behaviours such as healthier eating and increased exercising that indirectly impact fetal development, pregnancy term and birthweight.[2] Male partners can also discourage harmful behaviours, such as smoking and drinking alcohol, and encourage women to attend antenatal healthcare early.[3] Evidence suggests that the inclusion of fathers or male partners in both pre- and perinatal programmes positively impacts a child's attachment security, their emotional regulation and cognitive development. At the same time, such interventions can also positively impact male wellbeing and their relationship with the mother and child.[4]
Attendance at antenatal health visits, e.g. ultrasound appointments, has been shown to have a wide range of benefits. Harpel and Barras,[5] who studied the effects of maternal ultrasound scans on others, including men, found that men struggled more than mothers to cope with a complication or loss of pregnancy after attending an ultrasound examination.[5] It is hypothesised that the visual image of their forthcoming child establishes the reality of the pregnancy, which can strengthen the bond between expectant father and unborn child.[6-8] Male attendance at ultrasound scans has also been associated with improved child outcomes at birth. One study, for example, found that male ultrasound attendance was associated with a 7 percentage point reduction in premature infant births.[9] When male partners are involved, including attending ultrasound scans with their expectant partners, they are more likely to provide extra care and support, while regulating the stress levels of their partners, which can avert premature delivery.[10]
Many pregnant women want their male partners to be involved throughout the pregnancy, labour, delivery and development of their child,[11] and health professionals encourage men to attend antenatal appointments, including ultrasound scans.[12,13] Despite this, and evidence showing the positive impact of father involvement, men face a range of barriers in low- and middle-income settings,[4,11,14] and the timing of health visits that conflict with work schedules,[15] coupled with inflexible clinic hours or under-resourced health services.[16] In addition, families, communities and health workers have been known to disregard or discourage men during pregnancy.[11,16] In South Africa (SA), male partner involvement during and after pregnancy is exacerbated by the diversity in family arrangements and household structures that are intensified by racially differentiated levels of poverty and unemployment.[17] For example, poor African children are the least likely to live with their biological father, mainly as a result of men's lack of economic resources and social capital, as well as cultural norms.[17] Despite being the majority population group, poverty and unemployment are highest in the African population, while mean annual expenditure is lowest.[18] Not only can these financial difficulties lead to economic migration and family separation, but the inability to provide for one's family can result in poor mental health and negative health outcomes for men, which have a ripple effect on women and children.[19]
High levels of inequality also apply to healthcare utilisation, with only 17% of the African population accessing private healthcare at first sign of illness[18] and 10% having private medical insurance.[20] Unlike the private health system, public clinics and hospitals generally cannot accommodate men in the delivery room. Therefore, the majority of men cannot accompany and support their partner during birth. Cultural beliefs and practices can also influence father involvement, particularly in a multicultural country such as SA, where there are a number of different socioreligious orientations, e.g. the Zulu traditional religion, the Xhosa traditional religion, Hinduism, Islam and Christianity. In many southern African cultures, men are not recognised as the legitimate father of a child until financial requirements are met, which can lead to father-child non-residency, restricted visitation and involvement.[21] In the Islamic culture, premarital intercourse is forbidden and couples must be married before reproduction can take place.[22] This is likely to be a contributing factor to why the Indian population has the highest rate of co-residency.[17] Additional barriers to father involvement include incarceration, unusually low national marriage rates, high rates of informal kinship care and high levels of domestic violence.[3] These barriers not only limit men and the support they can provide to the mother, but have a negative impact on them as fathers.[23] Although many of these barriers require long-term political, social and economic solutions, in the short term, men should be provided with tailor-made messages, particularly acknowledging the importance of their involvement for child development and growth, maternal health and their own mental and emotional health.
Following guidelines from the World Health Organization (WHO), the South African National Department of Health (NDoH) adopted the practice of eight antenatal care visits during a pregnancy.[12] Included in these eight visits is the recommendation of an ultrasound scan at <24 weeks' gestation in a district hospital.[24] These routine health checks provide important opportunities to involve male partners and raise awareness of the importance of their involvement in their child's development. This article aims to describe and explore men's experiences of attending an early pregnancy ultrasound scan in SA.
Methods
Study design
This study is embedded in a randomised control trial (RCT) that compares the effects of an enhanced ultrasound experience on early childhood development with standard practice of care. Recruited women were blindly randomised through computer-generated randomisation to the intervention or control arm by the study research assistants, and both groups received an ultrasound examination as part of routine antenatal care. The control group received standard practice of care while the intervention group received the enhanced ultrasound with messages to promote early child development, an educational baby book and a printed and electronic image of their ultrasound scan. Mothers in both the intervention and control groups were encouraged to bring the father of the baby with them. Full details of the trial methods and recruitment procedures can be found in Richter et al.'s[25] article.
Setting
The study was performed in Soweto, home to 43% of the city of Johannesburg's population.[26] The trial was done in a research unit at Chris Hani Baragwanath Academic Hospital (CHBH), a tertiary hospital that attends to >22 000 births annually.
Participants
Women were recruited through the Fetal Medicine Unit (FMU) at CHBH, and were eligible for participation if they lived in Soweto, were >18 years of age and presented with a singleton pregnancy of <25 weeks' gestation. Women among whom major fetal abnormalities or severe maternal morbidities were detected were excluded from the study, but remained in clinical care at CHBH.
The participants in this study were men attending the ultrasound examinations with their partners. All men who attended were eligible, providing they were >18 years old.
Procedures
All participants completed individual questionnaires on information of their relationship status, experiences of the ultrasound scans and their level of anxiety before and after the procedure. All participants also completed the antenatal attachment scale.[27-29] The scale, designed to measure feelings, attitudes and behaviours specifically towards the fetus, has been validated for use among men and women. The male version is a 16-item questionnaire, while the female version is a 19-item questionnaire. A number of the ultrasound examinations where a partner attended were filmed to record the reactions, emotions and experiences of the participants in more detail. Data were collected between March and September 2019.
Data analysis
Data were analysed using Stata, version 14 (StataCorp., USA). Descriptive data are presented as frequencies and proportions. Open-ended questions were coded based on recurring themes and transformed into categorical variables. Responses to open-ended questions are presented qualitatively to report on the men's experiences.
Ethical approval
The study was approved by the Human Research Ethics Committee (Medical) of the University of the Witwatersrand, Johannesburg, SA (ref. no. M181915). An amendment was approved by the University of the Witwatersrand to film some of the ultrasound appointments. Permission was obtained from CHBH to conduct the study. The trial is registered through the Pan African Clinical Trials Registry (ref. no. PACTR201808107241133). Participants provided written consent and were given a unique study identifier to maintain confidentiality. The participants who had their ultrasound appointments recorded provided additional written consent, allowing the procedure to be filmed. The study adheres to CONSORT guidelines.
Results
Sociodemographic characteristics
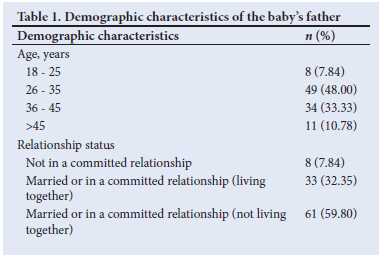
The sociodemographic characteristics of the partners are shown in Table 1. Of 249 mothers who attended the ultrasound examinations, 102 men accompanied their partner. The mean age of the men was 35 years, with the oldest being 56 years and the youngest 20 years. Only 32% of the men were reported to be living with the mothers, while a further 60% were married or in a committed relationship, but not living together. The remaining men were not in a relationship with the pregnant women (8%).
Antenatal attachment
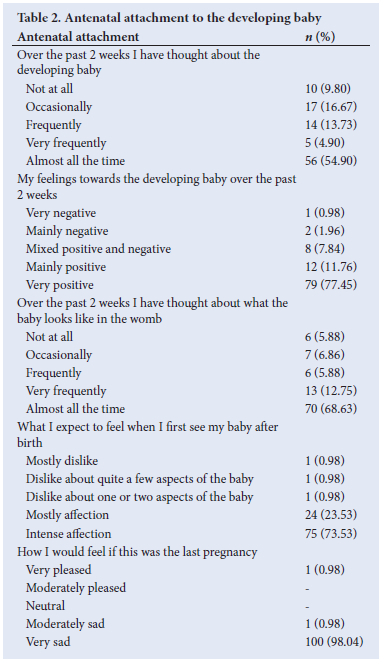
Prior to the ultrasound scan being conducted, the men were asked a range of questions regarding their attachment to the developing baby (Table 2). Ten percent of the men stated that they had not thought about the developing baby at all in the previous 2 weeks, compared with 55% who had thought about the baby almost all the time. Nearly all the men (89%) had positive feelings towards the developing baby, but a small number (3%) reported having negative feelings. Similarly, 97% of the men believed they would feel love and affection towards the baby after the birth, with 3% of the men expecting to feel some form of dislike towards the baby. One participant stated that he would be pleased if the pregnancy was lost.
Ultrasound experiences
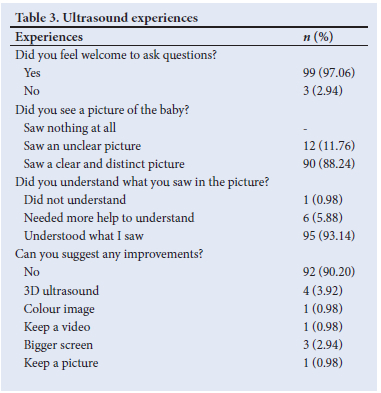
The results of the ultrasound experience questionnaire are shown in Table 3. All the men reported seeing a picture of the baby during the ultrasound scan, although 12% stated that the picture was unclear. Ninety-seven percent of the men felt comfortable asking questions during the scan and the majority (93%) understood what they saw in the picture, but 6% needed help to understand. There were not many suggestions for improvement of the scan, but included a bigger screen, a 3D image or a colour image.
In terms of how attending the ultrasound examination affected their feelings towards the baby, 95% of the men reported a positive effect, with only 5% reporting that there was no impact. Positive comments from the men included feeling happy, excited and more love towards the baby. One of the men, aged 28 years, stated:
'... it made me feel happy because I saw the baby is developing well.
The best part is when I heard the baby's heartbeat.'
When asked how attending the ultrasound scan affected their relationship with their partner, 21% stated that there was no change, while 28% and 19% of the men, respectively, reported having a stronger bond and a goal to be more supportive towards the mother. Feedback from a 28-year-old man included:
'I feel like it stirred up a feeling of oneness and a positive bond.
There was a change in atmosphere between us.'
Another man, aged 34 years, stated:
'It made me closer to her. I didn't care [before], now I have changed and I will help and support her in every way.'
Finally, the men were asked about how the ultrasound scan had affected their expectations of becoming a father. Thirty percent reported that they were excited or ready to be a father, while 13% stated that it made them want to support their child. Additional feedback included that they wanted to be more responsible. A participant, aged 25 years, stated:
'I must be responsible and give time to my child and I have to participate in school. I will also save for my child. The growth of my child is very crucial. I must give him time and love, determination and raise the child with enthusiasm and energy.'
Partner anxiety
The men were asked about the anxiety they were feeling before and after the ultrasound scan.
Before the scan, 64% of the men reported feeling very anxious. After the scan, 54% still reported high levels of anxiety and 2% reported an increase in anxiety. The proportion reporting no anxiety increased from 26% before to 41% after. None of the men who experienced no anxiety before the ultrasound scan reported a rise in anxiety after the procedure.
Discussion
Attendance by men at antenatal ultrasound examinations in the public health sector in SA is low, as highlighted in this study, where <50% of the mothers were accompanied by their partner, even with encouragement and despite the service being offered on a weekend to remove conflicts with work schedules often cited as a reason for non-attendance.[15] Additional reasons why male attendance was low could be the number of non-cohabiting couples and cultural practices. For the couples who did attend together, only 32% reported living together, while 17% of married couples were not living together. With only 36% of children in SA reported as living with their biological father,[30] it is common for men not to live with their wives or children. Reasons include living away for work, divorce or repartnering, cultural practices and incarceration.[3] Within the African community, cultural practices in particular can act as a major barrier to male involvement both during pregnancy and throughout a child's life. Some ethnic groups prescribe only women to be present in the delivery room[31] and it has been reported that men are turned away or forbidden to attend by hospital staff.[32] A study in Tshwane, SA, found that only 18% of participants were allowed to bring their partner into the delivery room while giving birth and 59% chose to give birth alone because of cultural customs.[33] Before birth, women and men are sometimes separated[34] and families may deny unmarried fathers access to their child or partner until payment of inhlawulo (damages) or marriage takes place.[21] Such practices during pregnancy and birth may deter men from being involved to support their partners and add to some of the barriers already faced. There is a need to fully understand the reasons and barriers limiting men from attending antenatal health visits, be it culture, social or economic, to address these issues and improve male involvement during pregnancy, birth and throughout the child's life.
Attending the ultrasound examination had a positive impact on the majority of men in this study, affecting their relationship with the mother and baby. In line with previous studies, positive changes towards their partner included a stronger bond and feelings of love and togetherness.[6-8,23] A number of men also mentioned wanting to ensure increased support of the mother and child as a result of the ultrasound scan, a similar finding to that of Harpel and Barras,[5] who stated that partner attendance at an ultrasound examination is a means to enhance the support system of a pregnant woman. However, not all of the men reported positive changes as a result of attending the scan. This finding could be linked to their level of antenatal attachment. Although many of the men reported having positive thoughts and expected to feel affection towards their child, a few did not and one stated that he would be pleased should the pregnancy be lost. It would be beneficial to explore why these men feel as they do and to assess whether low antenatal attachment hinders male involvement and negatively affects the child. However, the scan was a positive experience for the majority of the men and there is a need for health services in SA to support male attendance and ensure that health facilities are male friendly. Additional interventions such as Healthy Pregnancy, Healthy Baby are needed to encourage more men who utilise the public health system to be involved from conception.
The research regarding paternal mental health has been limited, even though it has been acknowledged as an important factor to consider and is beginning to gain more interest.[35,36] In this study, we examined the anxiety levels of the men before and after the ultrasound procedure. Although levels of anxiety decreased for a number of men after the procedure, for 2% it increased and for 52% it remained high. The antenatal period can be a vulnerable time for men,[37] as they may have fewer support systems and choose not to share their emotions or problems.[38,39] For first-time fathers, navigating the transition to fatherhood may be a difficult time and for many of the men, anxiety may arise owing to concern about supporting their child financially.[35] This may be particularly relevant in SA, where there are high levels of unemployment, poverty and inequality. Anxiety in expectant fathers has also been found to be associated with their experience of depression[37,40] and can affect their parenting skills and social relationships.[40] With limited information on paternal mental health in SA, there is a need to not only determine the rates of paternal depression, but investigate whether depression, anxiety and antenatal attachment are associated. It is also important to explore how men's mental health problems influence father involvement and impact child development.
Study strengths and limitations
To our knowledge, this study is the first to actively include men during pregnancy ultrasound scans in the SA public healthcare system and it provides useful and encouraging evidence to further promote male attendance at antenatal health visits. However, some limitations were apparent. The first was the small sample size of the male partners who attended the study ultrasound scans. Although we provided personal invitation cards and offered the service on a weekend to overcome work or distance barriers, attendance remained low. This indicated additional barriers to male involvement and it would be useful to explore these further. Furthermore, the men who did attend may not be representative of the whole population who utilise the public health service, as they may be more likely already to be supportive of their partners, leading to potential bias towards positive experiences and responses.
Conclusions
The results of this study highlight that male attendance at prenatal ultrasound examinations has a positive effect, not only on the male partner and their thoughts towards the pregnancy, but also towards their forthcoming child and their relationship with and support of their partner. Antenatal attachment among men was high and there was decreased anxiety among some men after the ultrasound scan. Health services in SA should accommodate fathers or male partners and encourage them to attend antenatal healthcare, including pregnancy ultrasound scans. Interventions such as Healthy Pregnancy, Healthy Baby can support the SA healthcare system and address individual, familial, societal and structural barriers to father involvement in long-term maternal and child care. Additional research is needed to determine the prevalence of ante- and postnatal depression in fathers, and how it affects child development and father involvement.
Declaration. None.
Acknowledgements. The authors would like to thank CHBH and the MRC/Wits Developmental Pathways for Health Research Unit (DPHRU) for facilitating the study. RED was supported by the DSI-NRF Centre of Excellence in Human Development.
Author contributions. RED analysed the data and wrote the manuscript. WS, TM and LMR provided substantial contributions and approved the final version for publication. All authors read and approved the manuscript.
Funding. This project was funded by Saving Brains, a partner of Grand Challenges Canada, the Aga Khan Foundation Canada, the Bernard van Leer Foundation, the Bill and Melinda Gates Foundation, the ELMA Foundation, Grand Challenges Ethiopia, the Maria Cecilia Souto Vidigal Foundation, the Palix Foundation, the UBS Optimus Foundation and World Vision Canada (ref. no. SB-POC-1810-19664). The funders did not play a role in the study design, collection, analysis or interpretation of the data, or the writing of the manuscript.
Conflicts of interest. None.
References
1. Xue WL, Shorey S, Wang W, He HG. Fathers' involvement during pregnancy and childbirth: An integrative literature review. Midwifery 2018;62:135-145. https://doi.org/10.1016/j.midw.2018.04.013 [ Links ]
2. Plantin L, Olukoya AA, Ny P. Positive health outcomes of fathers' involvement in pregnancy and childbirth paternal support: A scope study literature review. Fathering 2011;9(1):87-102. https://doi.org/10.3149/fth.0901.87 [ Links ]
3. Makusha T, Richter LM. Father involvement in the first 1 000 days. In: Van den Berg W, Makusha T, eds. State of South Africa's Fathers. Cape Town: Sonke Gender Justice and Human Sciences Research Council, 2018:49-62. [ Links ]
4. McKee CL, Stapleton PB, Pidgeon AM. History of pre- and perinatal (PPN) parenting education: A literature review. J Prenat Perinat Psychol Health 2018;32(3):191-219. [ Links ]
5. Harpel TS, Barras KG. The impact of ultrasound on prenatal attachment among disembodied and embodied knowers. J Fam Issues 2018;39(6):1523-1544. https://doi.org/10.1177/0192513X17710774 [ Links ]
6. Widarsson M, Engstrom G, Tyden T, Lundberg P, Hammar LM. 'Paddling upstream': Fathers' involvement during pregnancy as described by expectant fathers and mothers. J Clin Nurs 2015;24(7-8):1059-1068. https://doi.org/10.1111/jocn.12784 [ Links ]
7. Asenhend L, Kilstam J, Alehagen S, Baggens C. Becoming a father is an emotional rollercoaster - an analysis of first-time fathers' blogs. J Clin Nurs 2013;23(9-10):1309-1317. https://doi.org/10.1111/jocn.12355 [ Links ]
8. Draper J. 'It was a real good show': The ultrasound scan, fathers and the power of visual knowledge. Sociol Health Illn 2002;24(6):771-795. https://doi.org/10.1111/1467-9566.00318 [ Links ]
9. Lee SH, Lazebnik R, Kuper-Sasse M, Lazebnik N. Is the presence of the father of the baby during first prenatal ultrasound study visit associated with improved pregnancy outcomes in adolescents and young adults? Int J Pediatr 2016;2016:4632628. https://doi.org/10.1155/2016/4632628 [ Links ]
10. Redshaw M, Henderson J. Fathers' engagement in pregnancy and childbirth: Evidence from a national survey. BMC Pregnancy Childbirth 2013;13:70. https://doi.org/10.1186/1471-2393-13-70 [ Links ]
11. Adeniran AS, Aboyeji AP, Fawole AA, Balogun OR, Adesina KT, Adeniran PI. Male partner's role during pregnancy, labour and delivery: Expectations of pregnant women in Nigeria. Int J Health Sci (Qassim) 2015;9(3):305-313. https://doi.org/10.12816/0024697 [ Links ]
12. National Department of Health. Improving Antenatal Care in South Africa. Pretoria: NDoH, 2017. [ Links ]
13. World Health Organization. Recommendations on Antenatal Care for a Positive Pregnancy Experience. Geneva: WHO, 2016. [ Links ]
14. Kwambai TK, Dellicour S, Desai M, et al. Perspectives of men on antenatal and delivery care service utilisation in rural western Kenya: A qualitative study. BMC Pregnancy Childbirth 2013;13:134. https://doi.org/10.1186/1471-2393-13-134 [ Links ]
15. Humphries H, Nolan M. Evaluation of a brief intervention to assist health visitors and community practitioners to engage with fathers as part of the healthy child initiative. Prim Health Care Res Dev 2015;16(4):367-376. https://doi.org/10.1017/S1463423615000031 [ Links ]
16. Davis J, Vyankandondera J, Luchters S, Simon D, Holmes W. Male involvement in reproductive, maternal and child health: A qualitative study of policymaker and practitioner perspectives in the Pacific. Reprod Health 2016;13(1):81. https://doi.org/10.1186/s12978-016-0184-2. [ Links ]
17. Ratele K, Nduna M. An overview of fatherhood in South Africa. In: Van den Berg W, Makusha T, eds. State of South Africa's Fathers. Cape Town: Sonke Gender Justice and Human Sciences Research Council, 2018:29-46. [ Links ]
18. Statistics South Africa. Inequality Trends in South Africa: A Multidimensional Diagnostic of Inequality. Pretoria: Stats SA, 2019. [ Links ]
19. Springer KW Economic dependence in marriage and husbands midlife health: Testing three possible mechanisms. Gender Society 2010;24(3):378-401. https://doi.org/10.1177%2F0891243210371621. [ Links ]
20. Statistics South Africa. General Household Survey 2018. Pretoria: Stats SA, 2019. [ Links ]
21. Makusha T, Richter LM. Gatekeeping and its impact on father involvement among Black South Africans in rural KwaZulu-Natal. Cult Health Sex 2016;18(3):308-320. https://doi.org/10.1080/13691058.2015.1083122 [ Links ]
22. Francis Z. Premarital first-time fatherhood among young Muslim men in Cape Town. Honours degree (Psychology). Cape Town: University of Cape Town, 2018. [ Links ]
23. Backstrom C, Thorstensson S, Martensson LB, Grimming R, Nyblin Y, Golsater M. 'To be able to support her, I must feel calm and safe': Pregnant women's partners perceptions of professional support during pregnancy. BMC Pregnancy Childbirth 2017;17(1):234. https://doi.org/10.1186/s12884-017-1411-8 [ Links ]
24. National Department of Health. Guidelines for Maternity Care in South Africa: A Manual for Clinics, Community Health Centres and District Hospitals. 4th ed. Pretoria: NDoH, 2015. [ Links ]
25. Richter L, Slemming W, Norris SA, Stein A, Poston L, Pasupathy D. Health Pregnancy, Healthy Baby: Testing the added benefits of pregnancy ultrasound scan for child development in a randomised control trial. Trials 2020;21:25. https://doi.org/10.1186/s13063-019-3924-0 [ Links ]
26. Statistics South Africa. Census 2011. Pretoria: Stats SA, 2011. [ Links ]
27. Condon JT. Maternal antenatal attachment scale. 2015. https://dspace.flinders.edu.au/xmlui/bitstream/handle/2328/35292/Maternal_Antenatal_Attachment_Scale.pdf?sequence=5&isAllowed=y (accessed 23 March 2020). [ Links ]
28. Condon JT, Boyce P, Corkindale CJ. The first-time fathers study: A prospective study of the mental health and wellbeing of men during the transition to parenthood. Aust N Z J Psychiatry 2004;38(1-2):56-64. https://doi.org/10.1177/000486740403800102 [ Links ]
29. Condon JT. The assessment of antenatal emotional attachment: Development of a questionnaire instrument. Br J Med Psychol 1993;66(2):167-183. https://doi.org/10.1111/j.2044-8341.1993.tb01739.x [ Links ]
30. Statistics South Africa. General Household Survey 2017. Pretoria: Stats SA, 2017. [ Links ]
31. Mullick S, Kunene B, Wanjiru M. Involving men in maternity care: Health service delivery issues. Agenda Special Focus 2005;6:124-135. [ Links ]
32. Hastings-Tolsma M, Nolte AGW, Temane A. Birth stories from South Africa: Voices unheard. Women Birth 2018;31(1):e42-e50. https://doi.org/10.1016/j.wombi.2017.06.015 [ Links ]
33. Oosthuizen SJ, Bergh A, Pattinson RC, Grimbeek J. It does matter where you come from: Mothers' experiences of childbirth in midwife obstetric units, Tshwane, South Africa. Reprod Health 2017;14(1):151. https://doi.org/10.1186/s12978-017-0411-5 [ Links ]
34. Ngomane S, Mulaudzi FM. Indigenous beliefs and practices that influence the delayed attendance of antenatal clinics by women in the Bohlabelo district in Limpopo, South Africa. Midwifery 2012;28(1):30-38. https://doi:10.1016/j.midw.2010.11.002 [ Links ]
35. Darwin Z, Galdas P, Hinchliff S, et al. Fathers' views and experiences of their own mental health during pregnancy and the first postnatal year: A qualitative interview study of men participating in the UK Born and Bred in Yorkshire (BaBY) cohort. BMC Pregnancy Childbirth 2017;17:45. https://doi.org/10.1186/s12884-017-1229-4 [ Links ]
36. Fisher SD. Paternal mental health: Why is it relevant? Am J Lifestyle Med 2017;11(3):200-211. https://doi.org/10.1177/1559827616629895 [ Links ]
37. Beesley A, Karwatzki E, Sullivan K. Anxiety and depression symptoms in fathers during their partner's pregnancy: How does this impact fetal attachment? J Prenat Perinat Psychol Health 2019;33(3):221-240. [ Links ]
38. McKenzie SK, Collings S, Jenkin G, River J. Masculinity, social connectedness, and mental health: Men's diverse patterns of practice. Am J Men's Health 2018;12(5):1247-1261. https://doi.org/10.1177/1557988318772732 [ Links ]
39. Zelkowitz P, Milet TH. Stress and support as related to postpartum paternal mental health and perceptions of the infant. Infant Ment Health J 1997;18(4):424-435. https://doi.org/10.1002/(sici)1097-0355(199724)18:4<424::aid-imhj8>3.0.co;2-k [ Links ]
40. Philpott LF, Savage E, FitzGerald S, Leahy-Warren P. Anxiety in fathers in the perinatal period: A systematic review. Midwifery 2019;76:54-101. https://doi.org/10.1016/j.midw.2019.05.013 [ Links ]
 Correspondence:
Correspondence:
R E Drysdale
rdrysdale@wrhi.ac.za














