Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.15 no.4 Pretoria Dez. 2021
http://dx.doi.org/10.7196/SAJCH.2021.v15i4.1792
REVIEW
A scoping review to identify the type and effect of hand hygiene interventions on the reduction of infectious diseases (including COVID-19) in pre-school children
S LangeI; TG BarnardII; N NaickerIII, IV
IM Tech; Water and Health Research Centre, Faculty of Health Sciences, University of Johannesburg, Johannesburg, South Africa
IIPhD; Water and Health Research Centre, Faculty of Health Sciences, University of Johannesburg, Johannesburg, South Africa
IIIPhD The Epidemiology and Surveillance Section, National Institute for Occupational Health, National Health Laboratory Services, Braamfontein, South Africa
IVPhD Environmental Health Department, Faculty of Health Sciences, University of Johannesburg, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Proper handwashing can reduce the burden of diseases related to hand hygiene (HH) and so contribute reducing under-5 mortality. Preschoolers can benefit from HH interventions by the burden of disease and absenteeism being reduced.
OBJECTIVE. To perform a scoping review of literature to assess the types and effectiveness of HH interventions at preschools, with a view to providing a guideline for appropriate interventions for South African facilities.
METHODS. A literature search was conducted through the PubMed database to identify relevant studies. An iterative screening process to focus the review allowed for information on the type and effectiveness of interventions to be collated. An updated PubMed search was conducted to determine whether any interventions related to COVID-19 at preschools could be included.
RESULTS. No additional studies relating to COVID-19 were found. Of the 305 studies identified during the initial search, only 12 fitted the specific search criteria. Of these, 10 studies showed improvements in HH-related indicators following the interventions. Only two studies used health education as an intervention, whereas the others included the supply of HH products (to varying extents) as part of the intervention.
CONCLUSION. HH interventions appear successful in reducing diseases spread by poor HH, improving general HH practices and reducing absenteeism among preschoolers. Studies using innovative, entertaining methods of educating children have shown to be successful in improving handwashing techniques and decreasing microbial growth on children's hands. HH interventions are suggested as an effective measure to improve HH during the COVID-19 pandemic.
Diseases associated with insufficient hand hygiene (HH), such as diarrhoea and respiratory diseases (including COVID-19), remain a leading cause of death worldwide in children under the age of 5 years. The United Nations reports that 12% of deaths related to pneumonia and 8% of diarrhoeal deaths occur in this age group.[1] Diarrhoea is estimated to cause between 7.7% and 20% of deaths among under-5s in South Africa (SA).[2-5]
COVID-19 was declared a pandemic by the World Health Organization (WHO) on 11 March 2020. Although most paediatric cases of COVID-19 acquire their infection from adults, children may also transmit SARS-CoV-2 to adults.[6] As handwashing has been shown to reduce the risk of infection with SARS-CoV-2 and MERS dramatically,[7] the directive to adhere to strict HH practices in the context of COVID-19 has been emphasised as a measure to help curb the spread of the disease.
The value of proper HH in health has been recognised for more than 150 years. In 1854, Dr John Snow identified the incorrect placement of a water pump as the cause of a cholera outbreak.[8] Similarly, Dr Ignaz Semmelweis was able to reduce mortality rates in hospitals through a handwashing intervention in the mid nineteenth century.[9] Today, water, sanitation and hygiene (WASH) interventions are accepted measures to considerably reduce HH-related diseases.[10]
WASH interventions are implemented either as single interventions, such as through the provision of water, sanitary facilities or hygiene programmes, or as a combination of these elements.[11] These interventions can range from the supply of infrastructure (e.g. in the form of entire water purification and reticulation systems[12]) to teaching target groups to wash their hands correctly.[13,14] Education efforts can be aimed at entire communities or focus on smaller groups such as households, caregivers, parents or children.[15-18]
Hand washing with soap and water at key times is considered the most effective method to ensure proper HH; however, only 19% of people adhere to correct HH practice.[19] A study from Wuhan, China, showed that only 42% of children exhibited good HH practices.[20] When it is considered that over 2 million children attend day care in SA, practical, cost-effective interventions to improve HH can help to reduce related diseases among preschoolers, particularly in the time of the COVID-19 pandemic.
This study presents a scoping literature review to identify HH intervention methods and tools that would be suited for implementation in SA preschools, as well as to assess their effectiveness in preventing HH-related diseases.
Methods
The scoping review was guided by the Arksey and O'Malley framework stages as recommended by Calqohoun et al.[21]The framework consists of six stages, namely: identifying the research question; identifying the relevant studies; study selection; charting the data; collating, summarising and reporting results; and, ideally, a final stage of consultation. The PRISMA statement[22] was used to guide article selection (Fig. 1).
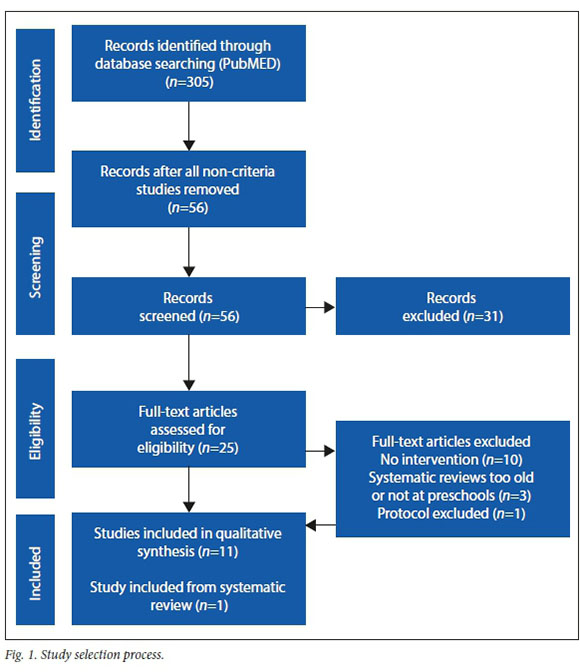
A PubMed search of literature published between 2010 and 2020 was conducted using the key words 'hand hygiene, 'preschool' and 'intervention'. This search was updated on 24 June 2020 to include any literature specific to HH in preschools during the COVID-19 pandemic; however, no literature was found to meet the search criteria in the updated search. The original search yielded 305 results. Of the initial set, 98 articles that were clearly based in a healthcare setting (e.g. a hospital) or dealt with medical procedures were discarded. Of the remaining 207 titles, 95 were discarded as they did not include terms such as 'intervention', 'practice', 'hand hygiene promotion', 'hand hygiene improvement' or other terms that suggested a type of intervention activity. A further 56 titles were removed as they did not include any reference to schools or preschools.
This resulted in a set of 56 studies of which the abstracts were read to determine whether the intervention was implemented at preschools and included a hygiene component. If a hygiene component was not included, the study was disregarded, as the aim of the scoping review was specifically to identify hygiene interventions implemented in preschool settings.
This yielded a set of 25 studies to be read in full. Of these, 10 studies did not specifically address hygiene interventions, one was a protocol, which was discarded, and three were reviews that did not meet the specific focus criteria or were too old. One of the reviews[23] included a study from 2012 that complied with the scoping criteria[24] and was therefore included in the scoping set. The described screening process yielded a final set of 12 studies for analysis.[11,16,18,24-32]. Extracted information was collated in table format (see Table 1).
Seven of the articles in the scoping set were randomised controlled trials. The quality of these studies was scrutinised using the 5-point JADAD scoring system.[33] The average score was 2.4, with all studies having randomised sample groups and five including a description of the randomisation process. In five of the studies, drop-outs or withdrawals could be accounted for. However, none of these seven randomised controlled trials were conducted blind, which is seen as a general weakness in HH intervention studies.[12,34]
Of the 12 studies eligible for analysis, all were examined for publication bias based on the following criteria: positive results in line with accepted norms; funding for the study; and reporting of statistically significant results.[35] Eight of the articles reported positive results in line with the expected results for a particular indicator, two were sponsored by pharmaceutical companies, which could have resulted in bias had the results not shown positive improvement, and nine showed statistically significant results. These three factors can influence publication bias. It should also be noted that it is possible that unpublished studies may exist that contradict the outcomes of the studies included in this review.
Regression models were used in seven of the final set of 12 studies reviewed, providing evidence of homogeneity. The use of t-tests was mentioned in three articles to determine significant differences. Two studies did not describe the data analysis process comprehensively.
Results
A total of 12 studies were included in the scoping review. Only one of the studies was conducted in Africa,[11] five were set in European countries,[16,25,30-32] three in Asia,[26,28,29] two in the Middle East[18,27] and one in South America.[24]
To determine the success of an intervention a measurable variable needs to be defined. Four of the studies used the decrease in diarrhoea or respiratory infections[11,16,24,31] as primary outcome. This was measured through varying degrees of record-keeping based on a type of incident register, where parents, caregivers or medical personnel noted the incidence of disease cases prior to and after the intervention. Definitions of a positive disease case were provided (most commonly for diarrhoea, defined by the WHO as passing three loose stools within a 24-hour period). Absenteeism was also recorded, either by the parent or the caregiver at the preschool, although in one study it also included the use of the temporary parental benefit provided by that country's government and claimed by parents when taking time off to care for sick children.[32]
One study measured the success of an intervention according to the improvement in children's handwashing skills. Wall-mounted tablet devices (running an Android operating system) at hand wash basins automatically recorded children's handwashing motions, rating their adherence with stars after they had completed the process.[28] Handwashing compliance was also assessed through observation of caregivers' compliance with HH practices,[31] and another study assessed the improvement of the HH environment through hygiene inspections at baseline and end line.[18] Determining bacterial colony density on children's hands was used as the main indicator of HH compliance between intervention and control groups in one study.[27]
The sample population of these studies included parents, caregivers and preschool children aged 5 years or younger, either singly or in combination. Sample sizes ranged from 40 preschool facilities[18] to 3 523 children,[11] depending on the study design. The methodology of the studies was mostly based on a pretest-post test design, as data were collected at baseline and at the end of the intervention (sometimes also during the course of the intervention).
Questionnaires were used as the data collection tool in five of the studies.[11,16,25-27] Of these, two articles mentioned administering a simple questionnaire to the children participating in the study,[26,27] two administered questionnaires to parents[11,25] and in one the questionnaire was administered to both parents and caregivers.[16] The registers used to track whether children were ill or absent were kept variously by parents, the school or both. In one study, government records were accessed to determine whether parents had used their temporary parental benefits to care for children at home[32] and in some cases medical professionals were used to scrutinise registers to determine whether recorded disease incidents complied with the defined descriptions of the disease.
Interventions in nine of the studies included education to caregivers. This was in the form of lectures, workshops, pamphlets or training sessions. One study provided health education to siblings of children under the age of five at school, to determine whether the intervention provided at school would transfer to younger children at home. The type of health promotion given to the school-going children was not described.
The provision of hygiene products such as soap, paper towels, alcohol-based rub and, in one study, separate drinking cups,[18] for the duration of the intervention, the study or a period of 6 months was identified in nine of the studies.
Two of the studies provided only HH training as an intervention, with one being directed at children (a clown character demonstrating handwashing)[27] and the other being directed at caregivers (a 2-hour lecture).[32] Three of the studies used incidents of diarrhoea or respiratory infections to assess the effectiveness of the intervention and in two others absenteeism was used as the indicator. The results of the interventions were tabulated according to the indicator used for each study.
HH interventions resulted in no improvement in only two studies, both of which used a combination of diarrhoeal and respiratory infections as indicator of effectiveness. The authors of one of the studies propose that the most likely explanation for this outcome is that the standard of hygiene at baseline was too high to support any significant effect of the intervention.[16] They were able to show compliance with hygiene protocols by caregivers, as measured by the use of the hygiene products during the study. In the other study showing no effect,[31] the authors explained that the HH compliance of the caregivers possibly did not increase enough to result in fewer infections. In addition, children attended school on average only 2.7 days per week and so may have been ill elsewhere.
In one of the studies using a decrease in absenteeism as indicator of the intervention's effectiveness, no decrease in absenteeism was observed. This may have been a result of strict guidelines regarding absenteeism being implemented to prevent the spread of communicable diseases prior to the start of the study.[32] However, as a secondary result, there was a significant decrease in absenteeism in preschool groups smaller than 15 children. The authors speculated that this may have been because caregivers were able to direct more time and attention to hygiene protocols in smaller groups.
The 10 other studies all showed positive effects ofthe interventions, although authors also listed possible reasons for this in addition to the actual intervention. In the study by Dreibelbis et al.,[11] which assessed the effect of an intervention delivered at school on diarrhoea incidents among under-5 siblings at home, it was noted that the most effective intervention was a combination of water provision, sanitation, health promotion and water treatment.[11] In a study that showed a significant reduction in diarrhoeal and respiratory infections after intervention, the authors attributed the outcome to intensive follow-up and the guaranteed supply of alcohol-based hand sanitisers.[24] Interestingly, of the 12 studies reviewed, nine included the provision of various HH-related products as part of the intervention. However, there is little evidence that availability of these products can be sustained in the relevant study populations after completion of the study.
A study assessing absenteeism as a result of respiratory infections also showed a decrease in both absenteeism and infections in the test group, who were provided with hand sanitiser.[25] Another study using this indicator showed a 25% reduction in absenteeism due to respiratory infections, following four training sessions in which a fluorescent staining gel and ultraviolet light were used to improve children's handwashing technique.[26] Another study focused on handwashing showed a 52.1% improvement in children's technique, which the authors attributed to the use of tablet devices fitted at wash basins, showing the proper handwashing technique and recording their actions.[28] However, the authors note that human observations are preferable, as they would be able to identify strengths and weaknesses in the technique.
Caregivers' compliance with HH practices was found to increase in a study where information was disseminated to this target group, although the authors noted the possibility of the Hawthorne effect due to direct observation and also possible bias by observers as potential concerns.[31] The environment where HH is practised has been shown to influence the effectiveness of hygiene interventions, as seen in increased use of HH products supplied as part of a study where the environment was positively enabled. This study also showed that there was no difference between secular and religious environments, but that HH practices could generally be improved at all preschools, with the researchers commenting that 'it is not possible to wash one's hands with soap if soap is not available'[18]
Finally, in a study using microbial growth as an indicator of the effectiveness of the intervention, a 31% reduction in microbial growth was seen on the hands of children in the intervention group, despite no marked increase in handwashing frequency in either group. The intervention included a character (clown) to teach children about pathogens ('germs') and proper handwashing, and the authors concluded that health messages to children could be more effective if entertaining methods are used.[27]
Discussion
The aim of this scoping review was to synthesise information on the effectiveness of HH interventions in preschools or among children of preschool age. The analysis shows that interventions led to decreases in diarrhoeal diseases, respiratory infections, absenteeism and microbial growth on hands, although there was no definitive 'one-size-fits-all' intervention. This review did not assess the quality of the studies included, but rather used the analysis to determine a way forward when looking at formulating a proposed intervention for preschools in SA to improve the health of under-5s and decrease the burden of HH-related diseases in this population.
Many of the studies showed improvements in child health, absenteeism or HH, but in a number of studies the outcome relied on the provision of HH products as part of the intervention. As the studies do not comment on the long-term sustainability of these interventions, it was not clear whether preschools continued to procure these products themselves after the conclusion of the study. In a country such as SA, where there are large socioeconomic divides, an intervention would need to be sustainable in a way that does not place additional financial burdens on the school or parents.
Two of the 12 studies included in this scoping review did not include the provision of HH supplies as part of the study, but relied on health promotion and education activities as an intervention. Using a fluorescent gel and ultraviolet light in teaching children to wash their hands resulted in a decrease in absenteeism due to influenza and the authors regarded the intervention as successful; the education campaign continued for four weeks to improve the children's attention to the handwashing process. This is consistent with findings showing that automaticity of an action increases steadily over time when the action is repeated in a constant setting.[36]
Another study that used health promotion as an intervention, not only offered HH education to the caregivers but also used a character (clown) to teach children about HH in an entertaining manner. Although there was no change in handwashing frequency or increase in the use of HH materials, bacterial colonisation was reduced by 31% in the experiment group and the growth rate of bacterial coliforms was reduced as a result of using the correct handwashing technique, as was demonstrated during the intervention.[27] The authors subsequently recommended that children should be taught in an entertaining way to achieve positive results. This is reiterated in a recent letter to the editor of the Journal of Hospital Infection,[37]which suggested a song to be used to teach children the correct handwashing procedures, which in the COVID-19 pandemic have become an important preventive measure. Experimentally, music has been shown to facilitate verbal and motor learning, which facilitates correction of a missed step or action through repetition and rehearsal.[37]
Using hygiene inspections and a two-hour lecture to caregivers on HH had no effect on children's absenteeism. This may have been as a result of stricter contagious disease control guidelines that had been implemented at baseline; however, other studies have shown interventions to be effective if they are directed at children and caregivers and, where practical, parents. Electronic communication with parents or sending health messages via email, short message services or other digital platforms can be effective, as has been shown with other health interventions for disease prevention.[38]
Study limitations
The scoping of literature in this review is limited to studies found through the PubMed database, which could have introduced bias. However, many of the articles are also available on other platforms. PubMed was chosen as search platform as it provides data in both text and comma-separated value (csv) format, which allowed for easy sorting.
The search was limited to studies published between 2010 and 2020 and therefore may have excluded articles on other interventions published earlier. Studies published after the COVID-19 pandemic may provide additional insights into effective and sustainable HH interventions in future.
Conclusion
The analysis presented here suggests that the interventions described by the reviewed studies can successfully improve HH, and possibly reduce disease incidents or absenteeism related to HH. Interventions where the necessary HH products were supplied would be expected to result in better outcomes, although the sustainability of this approach is unknown and warrants further study. However, using an innovative, entertaining approach to teach children about HH, repeating these lessons and including caregivers and, if possible, parents, could be a cost-effective, sustainable intervention to successfully improve HH practices among preschool children in SA. Given that HH is considered a crucial element of infection control and its effectiveness in reducing viral transmission,[20] the analysis presented here may help to implement effective interventions to combat the spread of HH-related diseases, such as COVID-19, in preschools and communities at large.
Declaration. None.
Acknowledgements. None.
Author contributions. SL was the main author and data collector. TGB provided additional information and contributed to manuscript development. NN was involved in checking the dataset and manuscript development. All authors read and approved the final manuscript. The datasets used in this analysis are available from the corresponding author on reasonable request.
Funding. None.
Conflicts of interest. None.
References
1. United Nations Children's Fund. Under-five mortality. https://data.unicef.org/topic/child-survival/under-five-mortality (accessed 24 May 2020). [ Links ]
2. Statistics South Africa. Mortality and causes of death in South Africa, 2016: Findings from death notification. Pretoria: StatsSA, 2016:1-127. [ Links ]
3. United Nations Children's Fund. Levels and trends in child mortality Report 2019. New York: Unicef, 2019. [ Links ]
4. Bamford LJ, McKerrow NH, Barron P, Aung Y. Child mortality in South Africa: Fewer deaths, but better data are needed. S Afr Med J 2018;108(3):25-32. https://doi.org/10.7196/SAMJ.2018.v108i3.12779. [ Links ]
5. Statistics South Africa. Millennium Development Goals: Reduce child mortality 2015. Pretoria: StatsSA, 2015:1-33. [ Links ]
6. Dong Y, Mo X, Hu Y, et al. Epidemiology of COVID-19 among children in China. Pediatrics 2020;145(6):e20200702. https://doi.org/10.1542/peds.2020-0702 [ Links ]
7. Yang C. Does hand hygiene reduce SARS-CoV-2 transmission? Graefes Arch Clin Exp Ophthalmol 2020;258(5):1133-1134. https://doi.org/10.1007/s00417-020-04652-5. [ Links ]
8. Cairncross S, Hunt C, Boisson S, et al. Water, sanitation and hygiene for the prevention of diarrhoea. Int J Epidemiol 2010;39(Suppl 1):i193-205. https://doi.org/10.1093/ije/dyq035. [ Links ]
9. Greenland K, Cairncross S, Cumming O, Curtis V. Can we afford to overlook hand hygiene again? Trop Med Int Health 2013;18(3):246-249. https://doi.org/10.1111/tmi.12055. [ Links ]
10. World Health Organization. Water, sanitation and hygiene in health care facilities: status in low and middle income countries and way forward. Geneva: WHO, 2015. [ Links ]
11. Dreibelbis R, Freeman MC, Greene LE, Saboori S, Rheingans R. The impact of school water, sanitation, and hygiene interventions on the health of younger siblings of pupils: A cluster-randomised trial in Kenya. Am J Public Health 2014;104(1):e91-97. https://doi.org/10.2105/AJPH.2013.301412. [ Links ]
12. Prüss-Ustün A, Bartram J, Clasen T, et al. Burden of disease from inadequate water, sanitation and hygiene in low- and middle-income settings: A retrospective analysis of data from 145 countries. Trop Med Int Health 2014;19(8):894-905. https://doi.org/10.1111/tmi.12329. [ Links ]
13. Croghan E. Preventing sickness absence from early years education. Br J School Nurs 2008;3(5):230-233. [ Links ]
14. Shrestha A, Angolkar M. Improving hand washing among school children: An educational intervention in South India. Al Ameen J Med Sci 2015;8:81-85. [ Links ]
15. Biran A, Schmidt WP, Varadharajan KS, et al. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): A cluster-randomised trial. Lancet Glob Health 2014;2(3):e145-154. https://doi.org/10.1016/S2214-109X(13)70160-8. [ Links ]
16. Gudnason T, Hrafnkelsson B, Laxdal B, Kristinsson KG. Does hygiene intervention at day care centres reduce infectious illnesses in children? An intervention cohort study. Scand J Infect Dis 2013;45(5):397-403. https://doi.org/10.3109/00365548.2012.749424. [ Links ]
17. Pandejpong D, Danchaivijitr S, Vanprapa N, Pandejpong T, Cook EF. Appropriate time-interval application of alcohol hand gel on reducing influenza-like illness among preschool children: A randomized, controlled trial. Am J Infect Control 2012;40(6):507-511. https://doi.org/10.1016/j.ajic.2011.08.020 [ Links ]
18. Rosen L, Zucker D, Brody D, Engelhard D, Meir M, Manor O. Enabling hygienic behavior among preschoolers: Improving environmental conditions through a multifaceted intervention. Am J Health Promot 2011;25(4):248-256. [ Links ]
19. Freeman MC, Stocks ME, Cumming O, et al. Hygiene and health: Systematic review of handwashing practices worldwide and update of health effects. Trop Med Int Health 2014;19(8):906-916. https://doi.org/10.1111/tmi.12339. [ Links ]
20. Chen X, Ran L, Liu Q, Hu Q, Du X, Tan X. Hand hygiene, mask-wearing behaviors and its associated factors during the COVID-19 epidemic: A cross-sectional study among primary school students in Wuhan, China. Int J Environ Res Public Health 2020;17(8):2893. https://doi.org/10.3390/ijerph17082893. [ Links ]
21. Colquhoun HL, Levac D, O'Brien KK, et al. Scoping reviews: Time for clarity in definition, methods, and reporting. J Clin Epidemiol 2014;67(12):1291-1294. https://doi.org/10.1016/j.jclinepi.2014.03.013 [ Links ]
22. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med 2009;151(4):264-269, W64. https://doi.org/10.7326/0003-4819-151-4-200908180. [ Links ]
23. Serra ME. Prevention of respiratory infections at day care centers: Recommendations and systematic review of the evidence. Arch Argent Pediatr 2014;112(4):323-331. https://doi.org/10.5546/aap.2014.323. [ Links ]
24. Correa JC, Pinto D, Salas LA, Camacho JC, Rondón M, Quintero J. A cluster-randomized controlled trial of handrubs for prevention of infectious diseases among children in Colombia. Rev Panam Salud Publica 2012;31(6):476-484. https://doi.org/10.1590/s1020-49892012000600005. [ Links ]
25. Azor-Martinez E, Yui-Hifume R, Munoz-Vico FJ, et al. Effectiveness of a hand hygiene program at child care centers: A cluster randomized trial. Pediatrics 2018;142(5):e20181245. https://doi.org/10.1542/peds.2018-1245. [ Links ]
26. Or PPL, Ching PTY, Chung JWY. A program to improve the hand hygiene compliance of Hong Kong preschoolers with an insight into their absenteeism. Am J Infect Control 2019;47(5):498-503. https://doi.org/10.1016/j.ajic.2018.11.014 [ Links ]
27. Arikan D, Gürarslan Ba§ N, Kurudirek F, Ba§topcu A, Uslu H. The effect of therapeutic clowning on handwashing technique and microbial colonisation in preschool children. J Nurs Scholarsh 2018;50(4):441-450. https://doi.org/10.1111/jnu.12392. [ Links ]
28. Mohd Rani MD, Mohamed NA, Tengku Jamaluddin TZM, et al. Effectiveness of comprehensive hand hygiene module on preschool children in Klang Valley, Malaysia. Clin Exp Pediatr 2020;63(3):115-116. https://doi.org/10.3345/cep.2019.01277. [ Links ]
29. Mohamed NA, Mohd Rani MD, Tengku Jamaluddin TZM, et al. Effect of hand hygiene intervention on the absenteeism of pre-school children in Klang Valley, Malaysia: A quasi-experimental study. World J Pediatr 2020;16(4):416-421. https://doi.org/10.1007/s12519-019-00283-x [ Links ]
30. Zomer TP, Erasmus V, Looman CW, et al. A hand hygiene intervention to reduce infections in child daycare: A randomized controlled trial. Epidemiol Infect 2015;143(12):2494-2502. https://doi.org/10.1017/S095026881400329X. [ Links ]
31. Zomer TP, Erasmus V, Looman CW, et al. Improving hand hygiene compliance in child daycare centres: a randomized controlled trial. Epidemiol Infect 2016;144(12):2552-2560. https://doi.org/10.1017/S0950268816000911. [ Links ]
32. Hall C, Lindahl E. Illness-related absence among preschool children: Insights from a health intervention in Swedish preschools. J Health Econ 2017;56:191-200. https://doi.org/10.1016/j.jhealeco.2017.10.004. [ Links ]
33. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials 1996;17(1):1-12. https://doi.org/10.1016/0197-2456(95)00134-4. [ Links ]
34. Brown J, Cairncross S, Ensink JHJ. Water, sanitation, hygiene and enteric infections in children. Arch Dis Child 2013;98(8):629-634. https://doi.org/10.1136/archdischild-2011-301528. [ Links ]
35. Song F, Hooper L, Loke Y. Publication bias: What is it? How do we measure it? How do we avoid it? Open Access J Clin Trials 2013;2013(5):71-81. [ Links ]
36. Lally P, Van Jaarsveld CH, Potts HW, Wardle J. How are habits formed: Modelling habit formation in the real world. Eur J Soc Psychol 2010;40(6):998-1009. https://doi.org/10.1002/ejsp.674. [ Links ]
37. Thampi N, Longtin Y, Peters A, Pittet D, Overy K. It's in our hands: A rapid, international initiative to translate a hand hygiene song during the COVID-19 pandemic. J Hosp Infect 2020;105(3):574-576. https://doi.org/10.1016/j.jhin.2020.05.003. [ Links ]
38. Déglise C, Suggs LS, Odermatt P. Short message service (SMS) applications for disease prevention in developing countries. J Med Internet Res 2012;14(1):e3. https://doi.org/10.2196/jmir.1823. [ Links ]
 Correspondence:
Correspondence:
S Lange
samlange18@gmail.com
Accepted 2 February 2021














