Services on Demand
Article
Indicators
Related links
-
 Cited by Google
Cited by Google -
 Similars in Google
Similars in Google
Share
South African Journal of Child Health
On-line version ISSN 1999-7671
Print version ISSN 1994-3032
S. Afr. j. child health vol.15 n.3 Pretoria Sep. 2021
http://dx.doi.org/10.7196/SAJCH.2021.v15.i3.1798
RESEARCH
Health facility obstacles result in missed vaccination opportunities in Tshwane Region 5, Gauteng Province
D N MontwediI; J C MeyerII, III; V V NkwinikaIV, V; R J BurnettVI, VII
IMPharm Division of Public Health Pharmacy and Management, School of Pharmacy, Sefako Makgatho Health Sciences University, Pretoria, South Africa
IIPhD; Division of Public Health Pharmacy and Management, School of Pharmacy, Sefako Makgatho Health Sciences University, Pretoria, South Africa
IIIPhD; South African Vaccination and Immunisation Centre, Sefako Makgatho Health Sciences University, Pretoria, South Africa
IVMSc (Medical Virology) South African Vaccination and Immunisation Centre, Sefako Makgatho Health Sciences University, Pretoria, South Africa
VMSc (Medical Virology) Department of Virology, Sefako Makgatho Health Sciences University, Pretoria, South Africa
VIPhD; South African Vaccination and Immunisation Centre, Sefako Makgatho Health Sciences University, Pretoria, South Africa
VIIPhD; Department of Virology, Sefako Makgatho Health Sciences University, Pretoria, South Africa
ABSTRACT
BACKGROUND. South Africa (SA) experiences vaccine-preventable disease outbreaks despite officially reporting high administrative fully immunised under-1-year-old coverage (FIC) figures.
OBJECTIVE. To investigate immunisation coverage and reasons for missed vaccinations in Tshwane Region 5 in Gauteng province, SA, in 2017.
METHODS. A household survey, based on a World Health Organization protocol, was conducted among consenting caregivers of children aged 12 - 23 months who had Road to Health cards (RtHC). RtH cards were checked and photographed, and reasons were recorded for missed vaccinations. Epi Info 7 was used for descriptive statistical analysis.
RESULTS. Eligible children resided in 327 of 8 060 houses visited, with 84.4% (n=276/327) of caregivers consenting to participate. Vaccination coverage ranged from 99.6% (n=275/276) for the oral polio vaccine at birth to 87.3% (n=241/276) for the third dose of the pneumococcal conjugate vaccine (PCV3). Of the children who received PCV3, 24 had missed earlier vaccinations, resulting in a FIC rate of 78.6% (n=217/276). Overall, 123 vaccinations were missed by 59 children, with reasons related to health facility obstacles (34.1%; n=42/123) and lack of information (26.8%; n=33/123) being the largest contributors.
CONCLUSION. The FIC rate of 78.6% can realistically be improved, as most missed vaccinations are due to modifiable healthcare facility obstacles, including poor communication. Suggested solutions include providing accredited programmes for empowering vaccinators to effectively communicate with their clients and manage vaccination logistics, and extending clinic hours to early evenings and weekends.
Immunisation is one of the most cost-effective public health interventions for preventing and controlling vaccine-preventable diseases (VPDs).[1] However, vaccines provide long-term protection only when all required doses are received, and evidence is mounting that this is not the case with vaccinations delivered through the South African Expanded Programme on Immunisation (EPI-SA).[2] This was highlighted by the most recent (2016) South African (SA) Demographic and Health Survey, with only 53% of children between 12 and 23 months and 42% of children between 24 and 35 months being fully immunised.[3] The data added to a growing list of concerns regarding the effectiveness of the EPI-SA programme, including that: full immunisation coverage (FIC) of children under 1 year old was unlikely to have reached the 90% target for 2020 set by the World Health Organization (WHO); SA regularly experiences VPD outbreaks; estimates of national immunisation coverage reported by WHO and the United Nations Children's Fund have been substantially lower than the figures reflected by the SA district health information system (DHIS) for more than a decade; and that household surveys have reported suboptimal FIC in some SA districts.[2,4-7]
Historically, one of the districts with suboptimal FIC was the former Metsweding district, which now forms the greater part of Tshwane Region 5 after being incorporated into this Tshwane district, Gauteng, in 2011 (http://www.tshwane.gov.za/sites/regions/Pages/Region-5.aspx). FIC in Metsweding reached 54% in 2004/05 and 66% in 2005/06.[8,9] Following changes to the under-1-year-old population estimates in 2005/06,[10] Metsweding, remarkably, failed to reach the 80% FIC district target in 2009/10 only in the period between 2006/07 and 2010/11.[11] However, there are no household survey data validating the FIC figures in Metsweding prior to 2011, nor in Tshwane Region 5 after Metsweding's incorporation into the Tshwane district.
This study subsequently investigated immunisation coverage and reasons for missed vaccinations in children aged 12 - 23 months from Tshwane Region 5 in 2017.
Methods
This descriptive household survey was adapted from the WHO protocol for vaccination coverage cluster surveys,[12] as previously described.[2] The study population was caregivers of children aged 12 - 23 months who had spent the night prior to the survey in Tshwane Region 5 and were in possession of the child's Road to Health card (RtHC). Not having a RtHC card was an exclusion criterion in order to limit recall bias.
According to the WHO protocol,[12] 26 participants were to be sampled per cluster. This assumed FIC at 50%, a desired precision of ~5%, a confidence level of 95% and a design effect of 2. The target sample was therefore 780 participants across 30 clusters. A map showing all households in Tshwane Region 5, as obtained from the City of Tshwane municipal records, was divided into 30 clusters (~400 - 520 houses/cluster) based on the number of households per residential area.[13] Adjacent areas with fewer households were combined to form one cluster. The 30 identified clusters were made up of either existing extensions or blocks bordered by roads (Supplementary Table 1; http://www.sajch.org.za/public/files/1798.pdf).
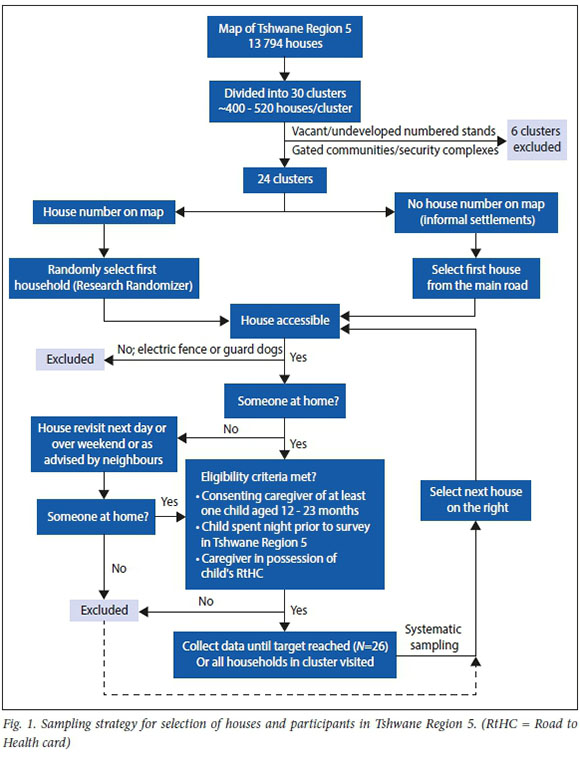
Sampling was conducted as previously described,[2] using Research Randomizer (https://www.randomizer.org) to select starting points in clusters with numbered houses. For clusters containing informal settlements, sampling started from the first household encountered from the entrance to the settlement. Systematic sampling ensued until the sample size was reached or all houses had been visited. Unoccupied houses were revisited on the following day or weekends, or as advised by neighbours.[2] A detailed daily record was kept of the houses visited, follow-up visits and the outcome of each visit.[12] The sampling strategy is illustrated in Fig. 1.
Two data collection teams, each consisting of a master's-level student assisted by two field workers, were trained according to the WHO protocol.[12] The data collectors were all fluent in English and Setswana and explained the aim and objectives ofthe study to the participants prior to data collection. Data collection, using two researcher-administered questionnaires adapted from the WHO protocol,[12] commenced after verbal consent to participation was given. Participants were free to withdraw from the study at any time.
Demographic data, immunisation status and immunisation dates (obtained from the RtHC) were recorded using the first questionnaire. A photograph of the participant's RtHC was taken using a cellphone camera and immediately emailed to one of the study supervisors to allow for real-time supervision. As the time, date and geographic co-ordinates were captured in the properties of the photograph, the supervisor was able to track the data collection team as they moved from house to house.
Reasons for missed vaccinations were noted using the second questionnaire, administered to caregivers of children with missed vaccinations. Following a participant's informed consent for audio recording, the interview was recorded and captured in writing to ensure validity. The two teams met at the end of each day to consolidate their daily records, which were then entered into a spreadsheet by one of the team leaders and shared with the supervisor. The supervisor facilitated a daily debriefing session, followed by planning for the next day's field work.
Data were collected over 30 days (July 2017), as per the WHO protocol,[12] and captured in an Excel spreadsheet (Microsoft Corp., USA) independently by the respective team leaders. Data validity was ensured by comparing the spreadsheet data with the photographs of the RtHCs and interview recordings. Summary fields with relevant formulae were added. For example, for calculating the FIC figure, the following immunisations had to be recorded: one dose of bacille Calmette-Guérin (BCG) vaccine; two doses of oral poliovirus vaccine (OPV); three doses of the pentavalent vaccine against diphtheria, tetanus, acellular pertussis, inactivated poliovirus and Haemophilus influenzae type b (DTaP-IPV-Hib; also known as Penta vaccine); three doses of the hepatitis B vaccine (HepB); two doses of rotavirus vaccine (RV); three doses of pneumococcal conjugate vaccine (PCV); and one dose of the measles vaccine (MV).[2] Once the data points had been validated, summary fields had been added and the data sets had been cleaned and coded, they were imported to Epi Info 7 (Centers for Disease Control and Prevention, USA) for preliminary descriptive statistical analysis. Further data cleaning was conducted after identifying inconsistencies (e.g. subsequent dose recorded without the previous dose being recorded) and discrepancies (e.g. frequency of a variable differing between data sets) revealed by the preliminary analysis of the two data sets. Descriptive statistical analysis was then performed using Epi Info 7 (CDC; USA), which included calculating the proportion of children who had received each vaccine and also the cumulative combinations of vaccines from birth to 9 months of age as an indication of FIC. The drop-out rate associated with each vaccine (i.e. the proportion of children who received the previous vaccination combination but not the next in the series) was calculated using the number of children who received the previous vaccine series in the schedule as the denominator, and the number of children who received the subsequent vaccine as the numerator.
Ethical considerations
The protocol was approved by the Sefako Makgatho University Research Ethics Committee (ref. no. SMUREC/P/69/2017:PG) and permission to conduct the study was granted by the Tshwane Research Committee (ref. no. GP_2017RP13_814).
Results
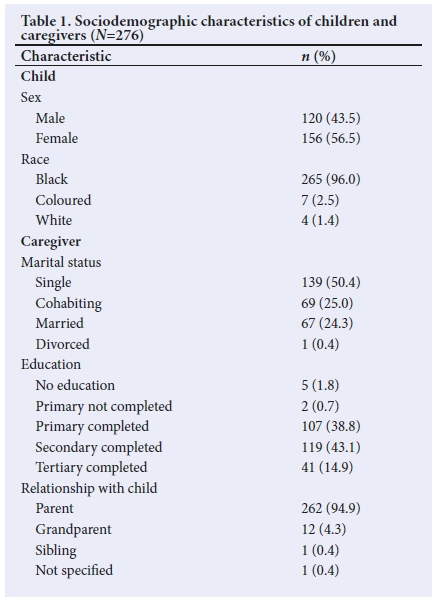
The number of houses listed in the municipal records (13 793) included vacant or undeveloped numbered stands (1 403 'houses') and inaccessible gated communities (including security complexes) (1 318 houses), discovered only during data collection. Hence only 24 clusters, comprising 11 072 houses, were surveyed. Of these, 72.8% (n=8 060/11 072) were visited; this included 245 houses where entry was refused. Of the houses visited, someone was found at home in 87.2% of cases (n=7 032/8 060). A child aged 12 - 23 months was found to have spent the previous night in these homes in 5.6% of cases (n=394/7 032). RtHCs were available for 83.0% of these children (n=327/394). Of caregivers of eligible children, 84.4% (n=276/327) consented to participate (see supplementary Table 1: http://www.sajch.org.za/public/files/1798.pdf). Caregivers were aged between 17 and 68 years (mean 30.2; median 29). Children's ages ranged from 12.03 to 23.97 months (mean 17.73; median 17.75). Table 1 summarises other sociodemographic characteristics.
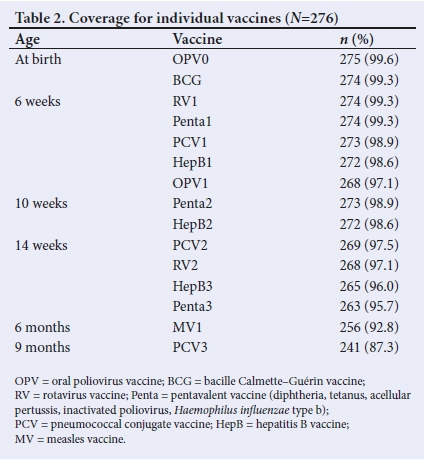
FIC was calculated as 78.6% (n=217/276), with 59 children being partially immunised (missed at least one scheduled EPI-SA vaccine). These 59 children had missed 123 vaccinations, of which 6 children accounted for 39.0% (n=48/123). Table 2 shows individual vaccine coverage. Records showed that 24 children received PCV3 without having received all vaccines scheduled at earlier ages, with nine having missed vaccinations when a subsequent dose of a vaccine series was recorded without the previous dose being administered (e.g. HepB3 administered at 18.6 weeks without HepB2 being recorded). These missed vaccinations were never caught up at subsequent visits (Table 3). The overall drop-out rate (i.e. proportion of children who received OPV0 but not all the other scheduled vaccines) was 21.1% (n=58/275) (see supplementary Table 2: http://www.sajch.org.za/public/files/1798.pdf). More than three-quarters of the missed vaccinations (76.4%; n=94/123) were those scheduled for administration between the age of 14 weeks and 9 months.
Missed vaccinations were mostly ascribed to health facility obstacles (34.1%; n=42/123), followed by lack of information (26.8%; n=33/123), personal obstacles (23.6%; 29/123) and lack of motivation (15.4%; n=19/123). In 15 cases, children whose caregivers were unaware of missed vaccinations had received Penta2 without missed vaccinations having been caught up; in 14 cases, children had received PCV3 without missed vaccinations having been caught up (Supplementary Table 3; http://www.sajch.org.za/public/files/1798.pdf).
Discussion
This study is the first household immunisation coverage survey to be conducted in Tshwane Region 5 since the incorporation of Metsweding into the Tshwane district in 2011. The FIC figure of 78.6% is very similar to that reflected by the DHIS (80.7%) for this region in 2017 (National Department of Health, personal communication), and just below the WHO target of 80%.[1] Failure to achieve immunisation coverage at the herd immunity threshold for highly infectious diseases such as measles is a major cause of outbreaks of VPDs.[5,6] Investigating individual vaccine coverage, and reasons for missed vaccinations, is important for identifying and addressing gaps at subdistrict level. Individual vaccine coverage ranged from 99.6% (OPV0) to 87.3% (PCV3), therefore FIC of 87.3% was expected. However, PCV3 coverage was higher than the overall FIC because of missed vaccination opportunities affecting 24 children. Of particular concern is that nine children had subsequent doses in a specific vaccination series recorded on their RtHC without having received a prior dose. Most of these missed vaccination opportunities could have been avoided if RtHC had been thoroughly checked, as previously suggested by other SA studies.[4,5,7]
The finding that vaccination drop-out rates increase with age, with 76.4% of missed vaccinations being those scheduled for the period between 14 weeks and 9 months, agrees with results from earlier SA studies.[4,5,7] The authors of a study on immunisation coverage among under-fives in Ga-Rankuwa (Tshwane Region 1) suggested that caregivers might perceive taking healthy older children to the clinic as unnecessary.[6] However, in this study, caregivers of partially vaccinated children were too busy (21.2%), unaware of PCV3 being needed at 9 months (16.7%) or found the clinic hours inconvenient (12.1%) (Supplementary Table 3; http://www.sajch.org.za/public/files/1798.pdf). These three reasons were unique to these later-stage vaccines, and constituted the majority of reasons for later vaccines being missed. Caregivers being too busy and inconvenient clinic hours are closely related, as although mothers are legally entitled to 4 months' unpaid maternity leave in SA, they are also legally allowed to return to work 6 weeks after giving birth.[14] Mothers who take only 6 weeks' postnatal leave may have difficulty taking leave during working hours, the only time that SA public sector clinics are open. Thus, although being too busy is included under personal obstacles (see Supplementary Table 3: http://www.sajch.org.za/public/files/1798.pdf), a strong case can also be made for including this reason as a health facility obstacle, resulting in over half of missed vaccinations being caused by health facility obstacles. The turnout of 1 081 children at a community-based vaccination catch-up campaign over six weekends in 2017 shows that many more caregivers will have their children vaccinated if clinics are open over weekends.[15]
EPI-SA managers previously reported vaccine stock-outs as one of the key challenges of running an effective immunisation programme,[16] a finding supported by several other surveys.[5,7,17] This was also found to apply in the current study, with stock-outs of the BCG, HepB, Penta, PVC and MV affecting 16.7% of partially vaccinated children. One caregiver reported becoming so demotivated after repeatedly being told that the required vaccines were unavailable, that she stopped taking her child for vaccination. The only vaccine shortage that may not have been caused by poor stock control at district or facility level was for the BCG vaccine, as there had been a global shortage in 2014/15.[18] This may have affected one child who missed a BCG vaccination because of unavailability. However, this child was born in November 2015 and catch-up therefore should have been possible at a subsequent visit, as the BCG vaccine can be given up to the age of 12 months in the SA public sector.[19] No global or national shortages of any of the other vaccines were reported. The cases of missed HepB and Penta vaccinations at 10 weeks (two children) and 14 weeks (four children) therefore cannot be attributed to the global 2017 shortage of the hexavalent vaccine (DTaP-IPV-Hib-HepB),[20] as all six children (born between November 2015 and January 2016) were eligible for this vaccine in 2016. Although the hexavalent vaccine was introduced into the EPI-SA programme in August 2015, Penta and HepB vaccinations were captured as two separate events in this study because this is how they were captured on the RtHCs and many clinics still had Penta and HepB stock available several months after the hexavalent vaccine was introduced (National Department of Health, personal communication).
Lack of information, accounting for 26.8% of missed vaccinations, points to the importance of effective communication between vaccinators and caregivers. This includes both verbal communication (with the vaccinator discussing the next scheduled visit with the caregiver at the end of each vaccination visit) and written communication (with the vaccinator writing the date for the next scheduled visit on the RtHC).[20,21] It can therefore be argued that the lack of information also qualifies as a healthcare facility obstacle, as it is the duty of vaccinators to ensure that caregivers are fully informed of vaccination visits. Effective communication could have prevented 11 cases of missed PCV3 doses owing to caregivers' being unaware of the need for a follow-up vaccination at 9 months. This affected 16.7% of partially vaccinated children. Although effective communication should also have alerted caregivers to their child not having received certain vaccines (affecting 22.7% of partially vaccinated children), it is clear that the vaccinators were not aware of these missed vaccinations either, as none of the missed vaccinations was caught up at subsequent visits. If these vaccines were available in the clinic at the time of subsequent visits, this again implies healthcare facility obstacles, owing to vaccinator negligence.
Study limitations
The vast majority of participants were willing to vaccinate their children, with only one caregiver having no faith in vaccination and another ceasing vaccination efforts after 10 weeks because she had lost faith in the healthcare system. However, this survey has important limitations resulting in it not being representative across the full socioeconomic spectrum in Tshwane Region 5.
First, field workers could not gain access to households in gated communities, where a higher rate of internet access is more likely. As the internet is the major source of vaccination misinformation,[22] higher rates of vaccine hesitancy and lower FIC rates would be expected in these communities.[22] This is a major limitation of the study, and since the majority of people living in these communities are likely to use private-sector vaccination services, their children's coverage would not be included in the DHIS coverage figures. This might explain why the FIC rate found in this survey is so similar to that reflected by the DHIS for Tshwane Region 5. For future surveys, the risk of unavoidable bias when conducting face-to-face household surveys in populations with pockets of gated communities must be considered, and more innovative ways of reaching these communities must be found.[2]
Second, no one was found at home or entry was refused at 1 028 houses. Apart from the 245 houses where entry was refused, follow-up visits were attempted after hours and on weekends, but without success. As this study was conducted during the school holidays, it is likely that these residents were on vacation. Those who take vacations during school holidays are more likely to have young children, hence a substantial number of eligible children may have been missed by this survey. Also, people who can afford to take vacations are more likely to be employed. As employed residents in a similar study in Tshwane Region 1 were found to have more knowledge and awareness about vaccination,[23] the FIC rate may have been higher among children in these households.
Third, of the 118 eligible caregivers who did not participate in the study, 67 were excluded because they did not have a RtHC. A previous study from elsewhere in SA reported that children without RtHCs were less likely to be fully immunised,[4] and therefore it is possible that the FIC rate may have been lower among these children. The remaining 51 caregivers in this group refused to participate after hearing the purpose of this study, which may suggest that they were not interested in vaccination. The FIC rate could consequently have been lower among these children.
These limitations resulted in the target sample size of 780 not being reached. However, it is important to note that the entire Region 5 had been divided into 30 clusters, which included six that consisted of gated communities and vacant or undeveloped numbered stands and so were not surveyed. Thus, of the 13 793 households listed by the City of Tshwane municipal records, only 8 188 were theoretically accessible. Of these, 98.4% were visited during the survey. Also, if a 50% FIC rate is assumed across 30 clusters (50% gives the largest possible sample size at every level of precision) and a desired precision of ±10% (80% power) at a 95% confidence level and a design effect of 2, a sample size of only 210 was needed, which translates to only seven eligible participants in each cluster. Thus, despite the limitation introduced by the reduced number of surveyed households, the study is still powered at >80%, thus satisfying the statistical power requirement for a subdistrict survey.[12]
Conclusion
The 78.6% FIC rate reported in this study is slightly below the WHO district target of 80%, and can be improved by addressing reasons for missed vaccinations, mostly related to modifiable healthcare facility obstacles. Possible solutions include: providing accredited programmes to empower vaccinators and their supervisors to effectively manage vaccination logistics and administration, and to communicate effectively with their clients about vaccination; extending clinic hours to early evenings and Saturdays and offering immunisations daily instead of only on specific days; advocating MomConnect service utilisation to remind caregivers about the date for the next immunisation visit. MomConnect, a National Department of Health initiative, which involves registering pregnant women on an SMS database to receive weekly health messages during pregnancy and their child's first year of life. Participants can also send messages to ask questions free of charge.[21]
There is also a need for increased vaccine advocacy among communities and education on the importance of always having the RtHC available. The Department of Health recently launched a digital Road to Health (RtH) booklet (https://www.jembi.org/Project/The-Digital-Road-to-Health-Project), which is a free application available for Android-operated smartphones. This is similar to the paper version of the RtH booklet that was introduced in November 2017 to replace the previous RtHC.[24] Although not all caregivers can afford smartphones, these digital records are highly likely to improve the validity of future household coverage surveys. Also, if used together with MomConnect messaging, this application can potentially increase FIC as well.
The Department of Health recently embarked on the first national immunisation coverage survey since 1994, with data on more than 15 000 children aged 2 - 3 years being collected.[2,25] National surveys are invaluable tools for monitoring and evaluating vaccination programmes, but are costly and therefore conducted infrequently in low- and middle-income countries.[2,25] It was recently highlighted that once the gaps identified by the national survey have been addressed, smaller-scale surveys will be needed in districts where corrective interventions have been implemented.[2] The current study is an example of how high-validity smaller-scale studies can be conducted, without the huge financial implications of a national survey.[2] In addition, online surveys are recommended to reach caregivers living in gated communities, who may be more affluent and educated or have higher rates of vaccine hesitancy.[22]
Declaration. The manuscript was submitted in partial fulfilment of the requirements for the MPharm degree at Sefako Makgatho Health Sciences University.
Acknowledgements. The authors thank S Mahori, RN Montwedi and RT Motha for assisting with data collection, and T Ndlovu for assisting with data collection training. We thank all the caregivers who participated in the study and appreciate the support received from the municipality and community members in Tshwane Region 5.
Author contributions. JCM and RJB conceptualised the study. DNM developed the protocol under the supervision of JCM and RJB. DNM and VVN led the data collection teams, and contributed to data capture validation. RJB and JCM trained the data collectors and supervised the field work. RJB performed the statistical analysis. All authors contributed to interpretation of data and critically reviewed the manuscript prior to submission.
Funding. The National Research Foundation of South Africa funded the study and conference attendance where the results of the study were reported.
Conflicts of interest. None.
References
1. World Health Organization. Global Vaccine Action Plan 2011-2020. Geneva: WHO, 2013. https://www.who.int/teams/immunization-vaccines-and-biologicals/strategies/global-vaccine-action-plan (accessed 13 April 2020). [ Links ]
2. Burnett RJ, Dlamini NR, Meyer JC, et al. Progress towards obtaining valid vaccination coverage data in South Africa. S Afr J Sci 2019;115(5/6). https://doi.org/10.17159/sajs.2019/6060 [ Links ]
3. National Department of Health, Statistics South Africa, South African Medical Research Council, ICF. South Africa Demographic and Health Survey 2016: Key Indicators. Pretoria: StatsSA, 2017. http://www.statssa.gov.za/publications/Report%2003-00-09/Report%2003-00-092016.pdf [ Links ]
4. Corrigall J, Coetzee D, Cameron N. Is the Western Cape at risk of an outbreak of preventable childhood diseases? Lessons from an evaluation of routine immunisation coverage. S Afr Med J 2008;98(1):41-45. [ Links ]
5. Le Roux K, Akin-Olugbade O, Katzen LS, et al. Immunisation coverage in the rural Eastern Cape - are we getting the basics of primary care right? Results from a longitudinal prospective cohort study. S Afr Med J 2017;107(1):52-55. https://doi.org/10.7196/samj.2016.v107.i1.11242 [ Links ]
6. Wright SCD, Maja TMM, Furaha SA. The impact of mothers' knowledge on the immunisation of children younger than five in Ga-Rankuwa, South Africa. Afr J Nurs Midwifery 2011;13(2):29-42. [ Links ]
7. Burnett RJ, Mmoledi G, Ngcobo NJ, et al. Impact of vaccine stock-outs on infant vaccination coverage: A hospital-based survey from South Africa. Int Health 2018;10(5):376-381. https://doi.org/10.1093/inthealth/ihy036 [ Links ]
8. Barron P, Day C, Loveday M, Monticelli F. The District Health Barometer Year 1. January-December 2004. Durban: Health Systems Trust, 2005. http://www.hst.org.za/publications/District%20Health%20Barometers/DHB_Year1.pdf [ Links ]
9. Barron P, Day C, Monticelli F, et al. The District Health Barometer 2005/06. Durban: Health Systems Trust, 2006. http://www.hst.org.za/publications/District%20Health%20Barometers/dhb0506.pdf [ Links ]
10. Monticelli F. Output indicators. In: Barron P, Day C, Monticelli F, eds. District Health Barometer 2006/07. Durban: Health Systems Trust, 2007:47-56. http://www.hst.org.za/publications/District%20Health%20Barometers/DHB_2006_07.pdf [ Links ]
11. Jassat W. Output indicators. In: Day C, Barron P, Massyn N, et al, eds. District Health Barometer 2010/11. Durban: Health Systems Trust, 2012:40-50. http://www.hst.org.za/publications/District%20Health%20Barometers/DHB%202010-11lowres.pdf. [ Links ]
12. World Health Organization. Immunisation coverage cluster survey - Reference manual. Geneva: WHO, 2005. https://apps.who.int/iris/handle/10665/(accessed 1 June 2020). [ Links ]
13. City of Tshwane. Region 5: Regional Integrated Development Plan 2014 - 15, 2014. http://www.tshwane.gov.za/sites/Council/Ofiice-Of-The-Executive-Mayor/20162017%20IDP/Annexure%20F%20Region%205%20RIDPv9_090514.pdf (accessed 13 April 2020). [ Links ]
14. Bosch A, ed. The SABPP Women's Report 2016: Pregnancy in the workplace, 2016. https://sabpp.co.za/wp-content/uploads/2016/12/ujsabppwomensreport2016.pdf (accessed 13 April 2020). [ Links ]
15. Meyer H, Moila T. Vaccination catch-up campaign: Multidisciplinary teams led by public health pharmacists. S Afr Pharm J 2018;85(1):16-17. [ Links ]
16. Wiysonge CS, Ngcobo NJ, Jeena PM, et al. Advances in childhood immunisation in South Africa: Where to now? Programme managers' views and evidence from systematic reviews. BMC Public Health 2012;12(1):578-586. https://doi.org/10.1186/1471-2458-12-578 [ Links ]
17. Ngcobo NJ, Kamupira MG. The status of vaccine availability and associated factors in Tshwane government clinics. S Afr Med J 2017;107(6):535-538. https://doi.org/10.7196/samj.2017.v107i6.12149 [ Links ]
18. Du Preez K, Seddon JA, Schaaf HS, et al. Global shortages of BCG vaccine and tuberculosis meningitis in children. Lancet 2019;7:e28-e29. https://doi.org/10.1016/s2214-109x(18)30474-1 [ Links ]
19. National Department of Health. Standard treatment guidelines and essential medicines list. 2018 edition. Online version 3.0. http://www.health.gov.za/index.php/standard-treatment-guidelines-and-essential-medicines-list/ category/285-phc (accessed 13 April 2020). [ Links ]
20. Aung Y, Dlamini RN. Immunisation. In: Massyn N, Padarath A, Peer N, Day C, eds. District Health Barometer 2016/17. Durban: Health Systems Trust, 2017:118-129. http://www.hst.org.za/publications/District%20Health%20Barometers/District%20Health %20Barometer%202016-2017.pdf [ Links ]
21. Barron P, Peter J, LeFevre AE, et al. Mobile health messaging service and helpdesk for South African mothers (MomConnect): History, successes and challenges. BMJ Glob Health 2018;3(Suppl 2):e000559. https://doi.org/10.1136/bmjgh-2017-000559 [ Links ]
22. Burnett R, Von Gogh L, Moloi M, François G. A profile of anti-vaccination lobbying on the South African internet, 2011 - 2013. S Afr Med J 2015;105(11):922-926. https://doi.org/10.7196/samj.2015.v105i11.9654 [ Links ]
23. Furaha SA. Immunisation coverage of children less than 5 years in Ga-Rankuwa. MTech dissertation. Pretoria: Tshwane University of Technology, 2009:1-172. [ Links ]
24. Slemming W, Bamford L. The new Road to Health Booklet demands a paradigm shift. S Afr J Child Health 2018;12(3):86-87. https://doi.org/10.7196%2FSAJCH.2018.v12i3.1595 [ Links ]
25. Burnett RJ, Dlamini NR, Meyer JC, et al. South Africa's first national vaccination coverage survey since 1994. S Afr Med J 2019;109(5):289. https://doi.org/10.7196/samj.2019.v109i5.14020 [ Links ]
 Correspondence:
Correspondence:
J C Meyer
hannelie.meyer@smu.ac.za
Accepted 11 January 2021














