Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.15 no.3 Pretoria sep. 2021
http://dx.doi.org/10.7196/SAJCH.2021.v15.i3.1752
RESEARCH
A study reflecting the demographics and comorbidities of children diagnosed with autism spectrum disorder at initial presentation to the KwaZulu-Natal Children's Hospital
S PillaiI; M MakhethaII; C AldousIII
IMB ChB, DCH; Department of Clinical Medicine, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIMMedSc; Department of Clinical Medicine, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
IIIPhD; Department of Clinical Medicine, Nelson R Mandela School of Medicine, University of KwaZulu-Natal, Durban, South Africa
ABSTRACT
BACKGROUND. Autism spectrum disorder (ASD) retards the holistic development of a child owing to both inherent and comorbid medical pathology. Despite the profound effect of ASD on a child's life, information regarding this neurodevelopmental disorder is limited. In South Africa (SA), there is a dearth of knowledge regarding ASD. In addition, the resources available to accommodate the needs of autistic children are largely insufficient in quantity and quality.
OBJECTIVES. To determine demographics and comorbidities in autistic children at the KwaZulu-Natal Children's Hospital (KZNCH).
METHODS. This study was a retrospective chart review conducted at the neurodevelopmental and neuropsychiatric clinics at the KZNCH in Durban, SA. Medical records of autistic children at their initial presentation to KZNCH from 1 January 2017 - 31 December 2017 were obtained and analysed.
RESULTS. The study sample comprised 114 study participants. Most participants (87%) presented above 36 months of age to the KZNCH. A 24-month delay was noted between onset of symptoms suggestive of ASD and presentation to a healthcare facility or KZNCH. Almost 50% of participants were awaiting placement in a special school. Attention deficit hyperactivity disorder (ADHD) was the most common comorbidity, affecting 43% of participants.
CONCLUSION. The study illustrated the demographic profiles and comorbidities of autistic children presenting to the KZNCH. However, the medical and social shortcomings in KZN elucidated in this study reinforce the necessity for further research to be conducted and resources to be invested to address the plight of children with ASD.
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterised by deficits in verbal and non-verbal communication, social interaction and demonstration of stereotyped repetitive and restrictive behaviour.[1-7] Research suggests that the pathophysiology of ASD is linked to altered brain connectivity and modification of neuronal organisation in early brain development.[4,7] The aetiology of ASD is largely unknown but likely to be multifactorial.[3] Genetic, immunological, perinatal and neuroanatomical factors have been suggested to be contributing factors.[3,6-8]
Studies exploring demographics of children with ASD showed varying ages at which the diagnosis of ASD could be made. The median age of diagnosis ranged from 18 to 42 months, depending on the countries in which the studies had been conducted.[3,9,10] A definitive diagnosis of ASD can be made during 24 - 36 months of age, based on symptoms; however, it has been suggested that caregivers may notice developmental or behavioural aberrations in children as young as 12 months of age.[11]
According to the World Health Organization (WHO), the prevalence of ASD is 1 in 160 children globally, and continues to increase.[5,12-17] The reported prevalence varies between countries owing to erratic notification and the disparity of research conducted in the developed v. developing world.[18] In the USA, the prevalence is ~1 in 45 (2%).[13] In Africa, and more specifically South Africa (SA), the prevalence is unknown owing to a lack of data and research.[9,13,18-20]
Early diagnosis and intervention are necessary to significantly improve long-term functionality involving cognition, communication, social skills and adaptive behaviours.[21-23] Many of the interventions which mitigate the effects of ASD are targeted at addressing common comorbidities associated with ASD. These include medical, psychological and social comorbidities. Medical comorbidities include epilepsy, sleep disorders and gastrointestinal problems[3,4,8,10-12,14,24,25] while psychiatric comorbidities include attention deficit hyperactivity disorder (ADHD), anxiety disorders, intellectual impairment or learning disorders, and mood or behavioural disorders.[2-4,10,12,14,24-26] Social comorbidities include increased levels of family stress and school refusal behaviour[9,19,25,26]
Although the diagnosis of ASD cannot be affirmed at a very young age, the American Academy of Pediatrics (AAP) recommends that all children should be screened for features ofASD as early as 18 - 24 months of age.[12,22] Furthermore, despite the absence of comorbidities in some children with ASD,[24] an awareness of pathologies that may coexist with ASD is essential in order to provide holistic patient management and optimise outcomes.[23] Studies have shown that early intervention resulted in 15 - 20% of affected children becoming self-sufficient adults while 20 - 30% were able to function adequately in adulthood with minimal support, effectively decreasing the burden of disease.[9] By addressing specific distresses, management of a child with ASD may be directed and subsequently more effective, but failure to diagnose early impacts negatively on the long-term quality of life of patients and their families.
According to the Bill of Rights, Section 27 of the Constitution, healthcare is a basic human right and its fulfilment is the objective of the healthcare system of SA. Embedded in this right is effective and timeous intervention. Internationally, a dearth of services for children with ASD has been documented. These include limitations in expertise as well as infrastructure or accessibility of services.[27] In Africa, the number of paediatricians available per 100 000 people ranges between 0.03 and 0.8; and in particular, sub-Saharan Africa has the poorest public health infrastructure worldwide.[28] Delays in diagnosing ASD have also been documented for SA.[9,19] For instance, the average waiting time following referral from a primary healthcare facility to a tertiary healthcare facility to ascertain the diagnosis of ASD was 18 months.[9] In addition, the estimated waiting time for allied health services ranged from 1 to 6 months for a 30-minute session. Furthermore, the waiting time for enrolment in a school catering for the needs of autistic children was ~3 years.[9] This successive delay in accessing appropriate healthcare and services for children with ASD denies them the benefits of early diagnosis and timeous intervention.
The SA public healthcare sector has a tiered system whereby the initial point of entry is at primary healthcare level; usually a local clinic. If deemed necessary, the patient is thereafter referred to a district or regional hospital for further assessment or management. If the patient requires interventions that surpass the scope of practice at these hospitals, the patient is referred to a tertiary healthcare centre where specialist or sub-specialist care is available. This referral pathway is dependent on the ability of healthcare workers to identify aberrations from normality or recognise pathology that exceeds the knowledge of the healthcare worker or facilities at a healthcare institution. A study conducted in KZN revealed that parents of children with ASD thought that healthcare practitioners possessed minimal knowledge regarding ASD. As a result, parents felt that their concerns were dismissed or resulted in them being misinformed about their child's condition.[12,19] Hence, for children with suspected ASD to receive a comprehensive assessment and appropriate management from the specialised KZNCH, a fundamental knowledge needs to be present at all levels of healthcare.[17,21-23,29-
Community awareness of ASD is lacking[12] but is as important as awareness within the healthcare fraternity. Parents raising a child with ASD experience multiple challenges related to family or community perceptions. Challenges from the family dynamic include neglect of the child by family members or friends as well as social segregation based on the misconstrued beliefs that autistic children are a result of 'God's curse.[1] The stressors experienced by parents of children with ASD affect their physical, mental and socioeconomic wellbeing.[12,19] Stressors include diagnostic and prognostic uncertainty, increased financial burden, social isolation, limited access to essential services, and psychological distress regarding the acceptance of and dealing with the challenges of having a child with ASD.[6,12,19] These concerns should be addressed in order to empower parents to fight social stigma and develop necessary coping skills as ASD has been identified as one of the most stressful neurodevelopmental disorders for parents to deal with.[19]
In KZN, there is a need to understand the burden of ASD as well as the health and social needs of patients and their families so as to address services for improved care. Hence, the purpose of this descriptive study was to identify demographics, define comorbidities, social challenges and delays in accessing specialised healthcare endured by children diagnosed with ASD presenting to the neurodevelopmental or neuropsychiatric clinics at the KZNCH in Durban for the period January to December 2017. We aimed to elucidate the difficulties experienced by children and families of children with ASD in KZN that could lead to addressing these shortfalls. Ethics approval was obtained on 30 May 2018 from the UKZN Biomedical Ethics Committee.
Methods
Clinic attendance registers for the year 2017 were used to obtain medical records satisfying the inclusion criteria. The inclusion criteria encompassed the children having attended either the neurodevelopmental or neuropsychiatric clinics, being diagnosed initially at KZNCH using the DSM-5 criteria and the modified Autism Diagnostic Observation Schedule (ADOS) and diagnosed with ASD between 1 January 2017 and 31 December 2017. Participants were excluded from the study if the diagnosis of ASD was not initially made at the KZNCH or confirmed by diagnostic assessments used at the KZNCH, and if children were previously diagnosed as having Asperger's disorder or pervasive developmental disorder not otherwise specified (PDD NOS) as per DSM-4 criteria and not re-classified to ASD as per DSM-5 criteria. Medical records for those children who fulfilled the inclusion criteria were subjected to retrospective review.
Variables assessed in this study were recorded on data collection tools. Measurements included (i) demographics which were: age of onset of symptoms, age at presentation to a healthcare facility, age at presentation to the KZNCH, gender, race, nutritional status and severity of ASD; (ii) social characteristics, namely attending mainstream school, attending a special school, awaiting placement at a special school, primary caregiver and the presence of both or one parent in the child's life; (iii) comorbidities of epilepsy or seizures, sleep disorders, gastrointestinal symptoms, ADHD, intellectual impairment, mood disorders and behavioural disorders.
Results
Demographics
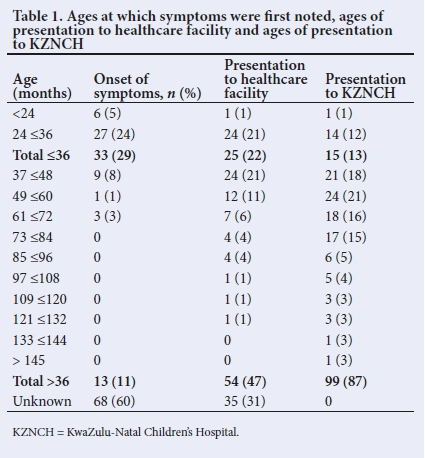
There was a total of 114 study participants, 76% of whom were boys. Racial demographics comprised 69% black, 20% Indian, 6% coloured, 4% white and 1% unknown. Participants were aged between 18 months and 13 years. As there is no definitive age at which ASD is diagnosed, ages were analysed using a benchmark of 24 - 36 months which is an approximation based on available literature.[3,8,9,10,17] Ages were further subdivided into 12-month intervals from 24 months to 144 months as shown in Table 1.
Clinical signs
Most of the children (99%) had a normal nutritional status. Severity corresponded to the levels of functionality documented in DSM-5 criteria, i.e. Level 1, Level 2 and Level 3 correlated with mild, moderate and severe ASD respectively. The range of ASD severity assessed in this study showed a predominance of moderate and/or mild ASD where 18% of children displayed moderate ASD while mild and mild-to-moderate categories were present in 17% of the children. Children with severe or moderate-to-severe ASD were least frequent with 11% and 12% of children being affected accordingly.
Social characteristics
The primary caregiver for 83% of the children was the mother, except for 4% of the children who were abandoned. The occurrence of households headed by a single caregiver was 6% higher than those with both parents. Regarding school attendance, 42% of children were attending school, with 29% enrolled in mainstream and 15% in special schools. A total of 49% of the children were still awaiting placement at special schools.
Comorbidities
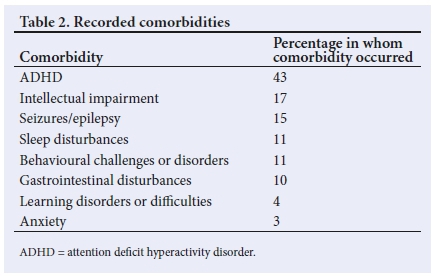
Table 2 shows a range of comorbidities which occurred in study participants. According to the literature, these comorbidities commonly occur in children with ASD.[2-4,8,10-12,19,24-26]
Discussion
Demographics
The male predominance exhibited in this study (76% of the participant population) replicated the findings in other studies where ASD was more common in boys than girls.[1,7,17,22,29-32] The racial distribution of the study participants showed a majority (69%) of black children with ASD. This figure is contrary to international studies where white children are most commonly diagnosed with ASD[14,22] however, it is reflective of the demographics of KZN; the second most highly populated province in SA which has a black population of 87%.[33]
The most frequent age at which symptoms suggestive of ASD were first noted by caregivers or educators was 36 months or below, and this was timeous as 18 - 36 months is the range of approximate earliest ages at which ASD can be diagnosed.[3,21,22,31] This figure accounted for 29% of the study sample. These results inferred that a portion of the caregivers or educators in KZN were able to recognise abnormalities in behavioural, cognitive, communicative and/or social functioning. In 60% of participants, the ages at which symptoms were first detected were unknown. This may have been attributed to either inadequate documentation in medical records or recall bias. Consequently, the results for age of onset of symptoms reflect only 40% of the study sample, which may influence the accuracy of the waiting period.
Although symptoms, in some cases, were timeously identified, 47% of children presented above 36 months of age to a healthcare facility for assessment of their symptoms. Of the 47%, 21% revealed up to 12 months, while 11% exhibited up to 24 months' delay from recognition of symptoms to initial presentation to any healthcare facility. A delayed initial presentation to the SA healthcare system subsequently contributes to belated confirmation of the diagnosis and institution of appropriate management. As a result, patient functionality and behaviour following appropriate interventions may bear the risk of being suboptimal or redundant. [21,23].
An 87% segment of study participants who presented at KZNCH was above 36 months' of age, most of whom fell into the 49- to -60 months age group. A timeline encompassing the ages at which most patients manifested symptoms or presented at each point in the healthcare system revealed the following: (i) the difference between the age of recognition of symptoms and first presentation to a healthcare facility was ~0 to 24 months; (ii) the difference between presentation to a healthcare facility and presentation to the KZNCH ranged from 0 - 24 months; and (iii) the difference between age at which symptoms were initially noted and presentation to the KZNCH was also a range of 0 - 24 months. The two-year delay noted restricts the benefit of neural plasticity of the young brain which may be the reason for the decreased severity and marked long-term improvements associated with the early intervention.[9]
Social characteristics
More than 50% of the participant population was not attending school for reasons such as some children being too young to enrol; some were unable to cope academically and/or socially in a mainstream or special school; and others were expelled from school owing to their aggressive behaviour or repetitive running away from school, often because they were bullied by other children. Of the 42% of school-going children, only 15% were attending a special school while 49% of the total participant population was awaiting placement at a special school. The 29% of the total study participants were attending a mainstream school largely owing to the necessity of receiving an education regardless of whether the school accommodated their academic or social needs. These results are evidence of the dire shortage of educational facilities available to children with ASD. There are only 35 special schools in KZN that have the capacity to accept children with ASD.[34
Although there was not a marked difference between the number of caregivers in a household, the mother was most commonly identified as the primary caregiver. This was not true for 4% of the households comprising children who had been abandoned by one or both of their biological parents and were subsequently cared for by the remaining parent or grandmother. Reasons for abandonment were not specified in all cases but some alluded to the inability of a mother to cope with the challenges associated with raising a child with ASD, which echoes the well-established comorbidity of increased family stress. A former study illustrated other factors that hindered the ability of a family to meet the healthcare requirements of their children; this study identified estranged, separated or deceased parents as contributory factors.[21]
Clinical characteristics
The majority of children in the present study exhibited moderate and/or mild ASD. Owing to changes of the diagnostic criteria for ASD and limited availability of literature regarding ASD, the severity profiles of these study participants were novel. The documentation of the current burden of ASD, in terms of severity, in this study may be used as a comparison in other studies that also explore the degree of severity of ASD in children.
Comorbidities
The comorbidities highlighted in the present paper are those known to occur in children with ASD as per national and international literature. These were medical comorbidities which included seizures or epilepsy, sleep disturbances, gastrointestinal disturbances, and psychological comorbidities which encompassed ADHD, concomitant anxiety, intellectual impairment, learning difficulties and other behavioural disorders (Table 2). The most common comorbidity was ADHD (43%) which was diagnosed using Conners Comprehensive Behaviour Rating Scales (Conners CBRS). Because Conners CBRS is only available in English, communication barriers were overcome by using a translator. As evidenced by other studies, ADHD is a behavioural disorder with a familiar association with ASD.[15,25,30] It tends to occur in children with ASD who do not display intellectual deficits and poses an additional challenge to social and academic limitations that are inherent in children with ASD.[2,14]
Children with ASD are often termed mentally retarded[1] owing to community ignorance. However, ~50% of children with ASD have no cognitive impairment.[32] In the present study, 17% of participants exhibited intellectual impairment which was most likely a rudimentary assessment as the level of intellectual impairment was not quantified using the intelligence quotient (IQ). As a result, the varying degrees of severity could not be assessed and compared with findings in other studies where ~30% of children with ASD have mild to moderate impairment and 45 - 50% have severe to profound impairment.[3]
Concomitant epilepsy or seizures were present in 15% of study participants. This parallels findings that show that epilepsy and epileptiform activity on electroencephalographys occur more commonly in children with ASD than in children without ASD.[4,8,13] In addition, epilepsy in autistic children is often refractory to pharmacological therapy and poses an increased mortality risk.[14,18,35]
Sleep disturbances and behavioural disorders were present in 11% of study participants, respectively. It has been suggested that sleep disorders may be a primary contributor to behavioural difficulties in children with or without ASD but occur more commonly in children with ASD.[23] Behavioural disorders encompassed undesirable nonspecific presentations as opposed to definitive disorders. These disorders included aggression, tantrums and disruptive and self-injurious behaviour. The behaviours identified echoed findings in other studies which illustrated the occurrence of such behaviours in children with ASD.[15]
Gastrointestinal disturbances occurring in this cohort encompassed a range of symptoms, yet the only two symptoms noted in the participants of the present study were constipation and food selectivity. Constipation is a recognised independent comorbidity in children with ASD but may be compounded by food selectivity.[23] Gastrointestinal manifestations may be debilitating; for example, food selectivity may lead to obesity or failure to thrive.[13,23]
Learning difficulties and anxiety disorders were the least identified comorbidities in the present study. Evidence suggested that 75% of children with ASD have learning difficulties; high-functioning autistic children have an increased occurrence of concomitant learning disorders, especially concerning written expression and dysgraphia.[11,35] However, the only learning difficulties identified were difficulties with letter identification and mathematics. These findings may be accounted for by misidentifying or misclassifying the specific learning difficulty as intellectual impairment or by insufficient documentation in the patient's medical record. The anxiety disorders noted in this study included two specific phobias and one unspecified anxiety disorder. It was unclear whether these comorbidities were diagnosed as per DSM-5 criteria or were a rudimentary assessment. Specific phobias occur more commonly in younger children with ASD as opposed to social phobias and obsessive compulsive disorder (OCD) which occur predominantly in adolescents.[36]
Conclusion
In conclusion, the present study vividly illustrates the challenges faced by children with ASD in KZN. These challenges supersede the limitations inherent in their medical pathology and affect their ability to function holistically as children in society. This study also echoes affirmations illustrated in other literature regarding the burden that ASD places on the healthcare system.[4] The 24-month delay identified in this study from the recognition of symptoms to obtaining appropriate healthcare clearly demonstrates the chasm of awareness and services available to assist children with ASD. We hope this study helps healthcare professionals and the community at large to hear the voices of those children who are so frequently misheard or sometimes not heard at all.
Declaration. None.
Acknowledgements. Dr V Govender and staff at the KZNCH.
Author contributions. SP conceived and developed the study and wrote the manuscript. MM and CA supervised the study.
Funding. None.
Conflicts of interest. None.
References
1. Preity S, Hawlader MDH, Akhter S, Abdullah A-S, Biswas A. Views of the parents of autistic children about autism and schools for autistic children: A qualitative study in urban Bangladesh. Int J Pub Health Res 2017;5(5):56-61. [ Links ]
2. Romero M, Aguilar JM, Del-Rey-Mejías A, et al. Psychiatric comorbidities in autism spectrum disorder: A comparative study between DSM-IV-TR and DSM-5 diagnosis. Int J Clin Health Psychol 2016;16(3):266-275. https://doi.org/10.1016/j.ijchp.2016.03.001 [ Links ]
3. Talukdar B, Deka N. Autism spectrum disorder - an overview. Eastern J Psychiatry 2016;20(2):42-48. [ Links ]
4. Buckley AW, Holes GL. Epilepsy and autism. Cold Spring Harb Perspect Med 2016;6(4):a022749. [ Links ]
5. Bowker A, DAngelo, Hicks R, Wells K. Treatments for autism: Parental choices and perceptions of change. J Aut Dev Disord 2011;41:1373-1382. https://doi.org/10.1007/s10803-010-1164-y [ Links ]
6. Neely J, Amatea ES, Echevarria-Doan S, Tannen T. Working with families living with autism: Potential contributions of marriage and family therapists. J Marital Fam Trier 2012;38:211-226. https://doi.org/10.1111/j.1752-0606.2011.00265.x [ Links ]
7. Abrahams BS, Geschwind DH. Advances in autism genetics: On the threshold of a new neurobiology. Nat Rev Genet 2008;9(5):341-355. https://doi.org/10.1038/nrg2346 [ Links ]
8. Brignell A, Albein-Urios N, Woolfenden S, Hayen A, Iorio A, Williams K. Overall prognosis of preschool autism spectrum disorder diagnoses (Protocol). Cochrane Datab Syst Rev 2017;(8):117-121. https://doi.org/10.1002/14651858.CD012749 [ Links ]
9. Guler J, de Vries PJ, Seris N, Shabalala N, Franz L. The importance of context in early autism intervention: A qualitative South African study. Autism 2018;22(8):1005-1017. https://doi.org/10.1177/1362361317716604 [ Links ]
10. Kuhlthau KA, McDonnel E, Coury DL, Payakachat N, Macklin E. Associations of quality of life with health-related characteristics among children with autism. Autism 2017;22(7):804-813. https://doi.org/10.1177/136236131770442 [ Links ]
11. Baird G, Cass H, Slonims V. Diagnosis of autism. BMJ 2003;327:488-493. [ Links ]
12. Glazzard J, Overall K. Living with autistic spectrum disorder: Parental experiences of raising a child with autistic spectrum disorder (ASD). Support Learn 2012;27(1):37-45. [ Links ]
13. Frye RE, Rossignol DA. Identification and treatment of pathophysiological comorbidities of autism spectrum disorder to achieve optimal outcomes. Clin Med Insights: Pediatrics 2017;10(4):43-56. https://doi.org/10.4137/CMPed.S38337 [ Links ]
14. Esler AN, Hall-Lande J, Hewitt A. Phenotypic characteristics of autism spectrum disorder in a diverse sample of Somali and other children. J Aut Dev Disord 2017;47(10):3150-3165. https://doi.org/10.1007/s10803-017-3232-z [ Links ]
15. Springer PE, van Toorn R, Laughton B, Kidd M. Characteristics of children with pervasive developmental disorders attending a developmental clinic in the Western Cape Province, South Africa. S Afr J Child Health 2013;7(3):95-99. https://doi.org/10.7196/SAJCH.530 [ Links ]
16. Zablotsky B, Colpe LJ, Pringle BA, Kogan MD, Rice C, Blumberg SJ. Age of parental concern, diagnosis, and service initiation among children with autism spectrum disorder. Am J Intellect Dev Disabil 2017;122(1):49-61. https://doi.org/10.1352/1944-7558-122.1.49 [ Links ]
17. Mubaiwa L. Autism: Understanding basic concepts. S Afr J Child Health 2008;2(1):6-7. [ Links ]
18. Van Biljon S, Kritzinger A, Geertsema S. A retrospective case report on demographic changes of learners at a school for children with autism spectrum disorder in the Gauteng Province. S Afr J Childhood Education 2015;5(1):42-61. [ Links ]
19. Fewster DL, Gurayah T. First port of call: Facing the parents of autism spectrum disorder. S Afr Fam Pract 2015;57(1):31-34. https://doi.org/10.1080/20786190.2014.995917 [ Links ]
20. Mankoski RE, Collins M, Ndosi NK, Mgalla EH, Sarwatt VV, Folstein SE. Etiologies of autism in a case-series from Tanzania. J Aut Dev Disord 2006;36:1039-1051. https://doi.org/10.1007/s10803-006-0143-9 [ Links ]
21. Berg KL, Acharya K, Shiu CS, Msall ME. Delayed diagnosis and treatment among children with autism who experience adversity. J Aut Dev Disord 2018;48(1):45-54. https://doi.org/10.1007/s10803-017-3294-y [ Links ]
22. Christensen DL, Maenner MJ, Bilder D, et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 4 Years - Early Autism and Developmental Disabilities Monitoring Network, Seven Sites, United States, 2010, 2012, and 2014. Atlanta: Centers for Disease Control and Prevention; 12 April 2019. Contract No. 2. [ Links ]
23. Mannix M. Medical comorbidities in autism spectrum disorder. Brown University Child and Adolescent Behavior Letter 2016;32:5-7. https://doi.org/10.1002/cbl.30100 [ Links ]
24. Wetherston V, Gangat S, Shange N, Wheeler K, Sayed Karrim SB, Pahl J. The views and knowledge of parents of children with autism spectrum disorder on a range of treatments. S Afr J Child Health 2017;11(3):117-121. https://doi.org/10.7196/SAJCH.2017.v11i3.1274 [ Links ]
25. Sanz-Cervera P, Pastor-Cerezuela G, González-Sala F, Tárraga-Mínguez R, Fernández-Andrés MI. Sensory processing in children with autism spectrum disorder and/or attention deficit hyperactivity disorder in the home and classroom contexts. Front Psychol 2017;8:1-12. https://doi.org/10.3389/fpsyg.2017.01772 [ Links ]
26. Munkhaugen EK, Gjevik E, Pripp AH, Sponheim E, Diseth TH. School refusal behaviour: Are children and adolescents with autism spectrum disorder at a higher risk? Resin Aut Spectrum Disord 2017;41-42:31-38. https://doi.org/10.1016/j.rasd.2017.07.001 [ Links ]
27. Dymond SK, Gilson CL, Myran SP. Services for children with autism spectrum disorders. J Disabil Policy Studies 2007;18(3):133-147. [ Links ]
28. Wilmshurst JM. Threats to the child's brain in resource-poor countries. J Int Child Neurol Assoc 2017:1-10. [ Links ]
29. Johnson CP, Myers SM, Council on Children With Disabilities. Identification and evaluation of children with autism spectrum disorders. Am Acad Pediatr 2007;120(5):1183-1225. www.pediatrics.org/cgi/doi/10.1542/peds.2007-2361 [ Links ]
30. Kamio Y, Moriwaki A, Inokuchi E. Neuropsychiatric comorbidities in autism spectrum disorders without intellectual disability. Neurology Asia 2013;18(1):43-45. [ Links ]
31. Venketramen J, Petersen R, Donald KA. Neurodevelopmental profile of first time attenders at a tertiary developmental paediatrics service in South Africa during 1 January 2016 to 31 December 2016. Eur J Paed Neurol 2016;21:69. https://doi.org/10.1016/j.ejpn.2017.04.1167 [ Links ]
32. Hallerod SLH, Larson T, Stahlberg O, et al. The autism-tics, AD/HD and other comorbidities (A-TAC) telephone interview: Convergence with the Child Behavior Checklist (CBCL). Nord J Psychiatry 2010;64(3):218-224. https://doi.org/10.3109/08039480903514443 [ Links ]
33. Statistics South Africa. Mid-year population estimates. Pretoria: StasSA, 2017. https://www.statssa.gov.za/publications/P0302/P03022017.pdf [ Links ]
34. Special Needs in Education Services. Pinetown: Department of Education. (accessed 1 June 2020) [ Links ]
35. Mayes SD, Calhoun SL. Learning, attention, writing, and processing speed in typical children and children with ADHD, autism, anxiety, depression, and oppositional-defiant disorder. Child Neuropsychol 2007;13:469-493. https://doi.org/10.1080/09297040601112773 [ Links ]
36. White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev 2009;29:216-229. https://doi.org/10.1016/j.cpr.2009.01.003 [ Links ]
 Correspondence:
Correspondence:
S Pillai
sa.jal@hotmail.com
Accepted 15 December 2020














