Serviços Personalizados
Artigo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em Google
Similares em Google
Compartilhar
South African Journal of Child Health
versão On-line ISSN 1999-7671
versão impressa ISSN 1994-3032
S. Afr. j. child health vol.15 no.1 Pretoria Abr. 2021
http://dx.doi.org/10.7196/sajch.2021.v15i1.1705
SHORT REPORT
https://doi.org/10.7196/sajch.2021.v15i1.1705
Association of attention deficit and hyperactivity disorder symptoms with visual functioning difficulties in Grade 1 learners
M de MilanderI; R SchallI; V van der VyverII; E J HattinghII
IPhD; Department of Exercise and Sport Sciences, Faculty of Health Sciences, University of the Free State, Bloemfontein, South Africa
IIBA Hons; Department of Mathematical Statistics and Actuarial Science, Faculty of Natural and Agricultural Sciences, University of the Free State, Bloemfontein, South Africa
ABSTRACT
BACKGROUND: Children with attention deficit and hyperactivity disorder (ADHD) can experience visual motor control difficulties. Therefore, early identification of such difficulties is important
OBJECTIVE: To determine whether ADHD symptoms are associated with visual motor control difficulties in Grade 1 learners
METHOD: In total, 382 children participated in the study. To determine the presence of ADHD symptoms, the educators completed the Strength and Weaknesses of ADHD symptoms Normal behaviour scale (SWAN) for each learner after six months of observing their class behaviour. Two kinderkineticists applied two tests, namely the Pyfer Sensory Input Systems Screening test and one subtest of the Quick Neurological Screening Test-II (QNST-II). Fisher's exact test was used to determine if ADHD symptoms were associated with visual functioning difficulties
RESULTS: ADHD symptoms were found to be significantly associated with 10 out of 21 visual functioning difficulties. These skills included fixation with both eyes (p=0.0491), fixation with the right eye (p=0.0003), fixation with the left eye (p=0.0042), ocular alignment of the right eye (p=0.0029), visual tracking with both eyes on X shape (p=0.0284), visual tracking with the right eye (p=0.0301), and visual tacking with the left eye on a circle (p=0.0032). Furthermore, ADHD symptoms were significantly associated with the QNST-II tracking test normal range (p=0.0028), moderate discrepancy (p=0.0028) and severe discrepancy (p=0.0075
CONCLUSION: ADHD symptoms are significantly associated with approximately half of the tested visual functioning of Grade 1 learners. Appropriate interventions should be implemented by professionals to assist these learners
Collectively, neurological disorders such as difficulties associated with vision,[1] in addition to attention deficit and hyperactivity disorder (ADHD),[2] are commonly seen in children. A variety of these visual difficulties (visual acuity, fixation and visual tracking) are often overlooked, causing children to be labelled as ADHD. This statement is in fact contradictory because these children essentially have learning-related visual difficulties.[3] However, the literature also indicates that these learning-related visual difficulties are associated with ADHD.[3] From an educational and movement perspective, it is expected from school-age children to excel both in academics (reading, spelling, writing, arithmetic)[3] and on the sportsfield (playing sports including stability, locomotor and object manipulation tasks).[4] However, owing to visual difficulties and ADHD simultaneously, children might find it challenging to perform well in the classroom or take part in sports, leading to a low self-image.[3] Consequently, the overall wellbeing of the child should be developed.
Vision is the ability to understand what is seen by means of light entering the eye to form an image on the retina. Vision may be affected by the integrity of visual impulses in the eye or the optic nerve, and even in the visual cortex.[5-7] According to Cheatum and Hammond,[3] and also Payne and Isaacs,[7] depth perception, eye-hand co-ordination, visual form perception, visual memory and visual development have an important impact on motor performance. Most of the information that learners gain from their environment is through vision.[2-4] Furthermore, Cheatum and Hammond[3] stated that 20% of school-age children experience visual problems that are generally undetected ('hidden disabilities'). Children with visual problems will struggle with activities such as reading, spelling, handwriting and arithmetic, which are visual skills fundamental for success in the school setting.[5-9] Visual problems can be associated with symptoms of ADHD.[3]
Learners with ADHD struggle with visual functioning difficulties, suggesting that learners with ADHD may have trouble in completing certain tasks owing to poor visual functioning.[10-12] The American Psychiatric Association (APA) defines ADHD as a neurodevelopmental disorder that is one of the most commonly diagnosed disorders in children.[2] According to Roth et al.,[5] ADHD can be divided into three major symptom clusters, namely inattentive, hyperactive-impulsive, and combined subtypes. Children with ADHD may not give attention to detail; not sustain attention during free play; apparently do not listen when someone speaks to them; do not follow instructions; lose things they need for an activity; are distracted by other stimuli; and have difficulty in organising a variety of tasks.[5]
Previous studies have stated that ADHD may be associated with various dysfunctions of the eye such as fixation.[8-10] A study of 32 girls with ADHD aged 6 - 13 years showed difficulties concerning their saccadic eye movements compared with the control group, although the researchers did not find any significant differences in eye movement performance during smooth pursuit.[10] Gould et al.'111found similar results with 29 girls with ADHD using a 21-second fixation test. Saccadic eye movements interfered with their ability to fixate. Munoz et al.[12] tested 114 people with ADHD between the ages of 6 and 59 years and concluded that the participants had a reduced ability to control their fixation behaviour voluntarily. Furthermore, researchers found a high percentage (57%) of children had convergence difficulties, and this was attributed to comorbidity factors, one of which was ADHD.[13] Deans et al.[15] studied 27 children in the age range 6 - 12 years. The children had to read, thus fixating on a word and by means of saccadic movements move from one word to another. It was found that the ADHD group had much slower reading times than the typically developmental group. Accordingly, previous research clearly suggests that children with ADHD can experience visual functioning difficulties, and early identification is therefore important to support learners to excel in the school setting.[13-14]
Information specifically about the association of ADHD symptoms with visual functioning difficulties in children with reference to fixation, ocular alignment, convergence-divergence and visual tracking, is limited. Furthermore, the data available are outdated. Therefore, the aim of the present study was to determine if ADHD symptoms are associated with visual functioning difficulties among Grade 1 learners.
Methods
Participants
Initially, 13 former model C primary schools were requested to participate, but only five of the mainstream schools took part in the study. Consequently, the participating schools were all from suburbs with a high socio-economic status. The five schools were located within a 30 km radius of the University of the Free State in Bloemfontein, South Africa (SA).
All Grade 1 children attending the five participating schools were considered for inclusion in the study. The following exclusion criteria were applied: a child in the age group was outside the expected range (either younger than 5 or older than 8 years); informed consent was not obtained from a parent or guardian; and the informed consent form was not fully completed. Children who were absent during the testing procedure were also excluded because the testing procedure had not been completed.
Scores on the Strength and Weaknesses of ADHD Symptoms Normal Behaviour rating scale (SWAN),[15] the Pyfer Sensory Input Systems Screening test (Pyfer),[16] and the Quick Neurological Screening Test-II (QNST-II) according to Mutti et al.[1] were obtained for a total of 382 learners in Grade 1, of whom 160 (41.9%) were boys. The mean (standard deviation (SD)) age of the children was 6 years and 8 months (0.4 years, range 6 - 7 years and 9 months).
Ethical considerations
Permission to conduct the research at the various schools was obtained from the Department of Education of Free State Province. In addition, the principal of each school gave permission for the research to be conducted on the school premises during the physical education periods, so that no academic learning time was lost. Approval for the study was obtained from the Ethics Committee of the Faculty of Health Sciences, University of the Free State (ref. no. ECUFS57/2012). Parents or legal guardians of all participants provided informed consent. Finally, each child participating in the study signed an assent form.
Procedure
The SWAN rating scale was applied as described previously.[15] The lead investigator explained the procedure for completion of the SWAN rating scale to each head of department (HOD), who in turn explained the procedure in detail to Grade 1 teachers at each school, as not all teachers involved could attend instruction sessions. Teachers observed children in their classrooms for six months to ensure that they were familiar with each child. According to the APA,[2] symptoms of ADHD should be present for at least six months before a diagnosis can be made.
At each of the five schools, Grade 1 teachers had to observe their own class and assess each child. The number of children per class ranged between 25 and 32. Teachers had to assess children in their own time over a period of one month. They were informed in advance that they could withdraw from the study at any time and that there was no compensation for completing the SWAN. The SWAN rating scale was used to determine which children exhibited symptoms of inattentive, hyperactive or combined clusters of ADHD. In addition, two Kinderkinetics postgraduate students, who had been trained to use the Pyfer and QNST-II tests, administered the tests to participants at their schools during physical education periods. Each Kinderkineticist was responsible for performing either one of the instruments to ensure consistency across the study. The results of the SWAN were used to determine the association of ADHD symptoms with visual functional difficulties as determined by the Pyfer and QNST-II in Grade 1 learners.
Measuring instruments
SWAN
The SWAN rating scale was developed by Swanson et al.[16]and consists of 18 questions/statements on which the participant is rated by the educator or a parent. The questionnaire needs to be completed after a period of six months of formal schooling to ensure that educators are familiar with each child in the classroom.[5] This recommendation was applied in our study. When completing the scale, a value of 1 is allocated if the response to the statement is 'not at all' or 'just a little', and 0 if the response is 'quite a bit' or 'very much'. The values allocated to the statements are then added, and when the sum is >6 for questions 1 - 9, the participant is likely to have inattentive subtype ADHD. When the sum is >6 for statements 10 - 18, the participant is likely to have hyperactive/impulsive subtype ADHD. When the sums of both groups of statements (1 - 9 and 10 - 18) are >6, the participant is likely to have combined subtype ADHD. If neither adds up to >6, the participant is unlikely to have ADHD symptoms.[15]
Pyfer
The Pyfer test consists of seven skills that include (i) reflex items (tonic labyrinthine supine, tonic labyrinthine prone, positive support reaction and equilibrium reactions); (ii) vestibular test items; (iii) fixation; (iv) ocular alignment; (v) convergence-divergence ocular control; (vi) visual tracing; and (vii) kinesthesis. For the purpose of this study, only fixation, ocular alignment, convergence-divergence ocular control and visual tracing were used, as these are all the visual motor skills. The Pyfer test is scored only according to pass or fail criteria. If the participant could perform the activity requested, a pass is allocated.[16]
QNST-II
According to Mutti et al.,[1]the QNST-II is designed to determine whether a child has learning problems or has symptoms of ADHD. The test consists of 15 skills, of which only subtest 4 (eye tracking) was used for the purpose of this study, as this is the only subtest to measure visual functioning. A mark of either 1 or 3 is allocated for the various aspects observed during the execution of the subtest. The participant scores 1 if the head is moved while performing the test and 3 if any jerkiness of the eyes occurs on vertical or horizontal movements. Inability to focus on an object or distractibility is also scored as 3. If the participant scored between 0 and 3, they will fall within the normal range, indicating no learning problems. However, scores between 4 and 6 are indicative of falling within the mild discrepancy range, and by implication they might find it difficult to learn in a normal environment. If a score > 6 is obtained, the participant falls into the severe discrepancy range, indicating ADHD associated with learning difficulties.[17]
Data analysis
The principal researcher used a Microsoft Excel (Microsoft Corp., USA) spreadsheet to capture data from the Pyfer screening test and the QNST-II test electronically. The data were analysed by means of SAS statistical software.[17] Fisher's exact test was performed to assess the association between ADHD symptoms and visual functioning difficulties. Odds ratios (OR) and associated exact mid-p 95% confidence intervals (CI) were calculated[17] (i.e. the odds of failing the visual test in question when ADHD symptoms were present, divided by the odds of failing the visual test when ADHD symptoms were absent). The association of ADHD symptoms with the results of the QNST-II test (normal, moderate or severe problems) was assessed using the Mantel-Haenszel correlation test.[17]
Results
Of the 382 study participants, 95 (24.9%) had ADHD symptoms; because the group with ADHD symptoms was relatively small, it was not divided into a hyperactive, inattentive or combined group. The remaining 287 (75.1%) participants showed no symptoms of ADHD.
Table 1 presents the cross-tabulations of participants by the result of the various visual functioning tests (fail v. pass) and the presence or absence of ADHD symptoms. For each visual functioning test, Table 2 presents the inferential statistics for assessing the association of ADHD with visual functioning difficulties, namely OR and associated exact 95% CI. Only the seven visual function difficulties with a significant association are discussed further on. Similarly to Table 1, Table 3 presents the cross-tabulation of participants by the result of the QNST-II and the presence or absence of ADHD symptoms.

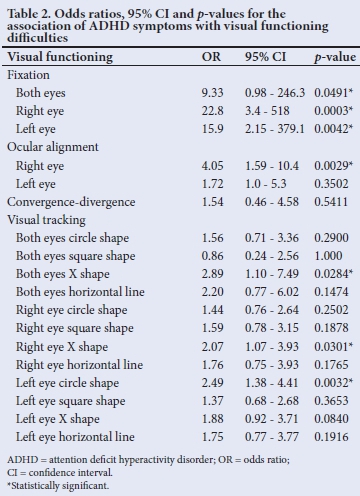

Table 1 shows that 7.4% of participants with ADHD symptoms failed the fixation right eye test, but only 0.4% of participants without ADHD symptoms failed this test. The OR was 22.8 (95% CI 3.42 - 518; p=0.0003; Table 3), which means that the odds of failing the fixation right eye test among participants with ADHD symptoms were 22.8 times higher than the odds of failing the fixation right eye test among participants without ADHD symptoms. Similarly, 5.3% of participants with ADHD symptoms failed the fixation left eye test, but only 0.4% of participants without ADHD symptoms failed this test. The OR was 15.9 (95% CI 2.15 - 379; p=0.0042). Additionally, fixation both eyes also indicated an odds ratio of 9.3 (95% CI 0.98 -246.3; p=0.0491).
Furthermore, ADHD symptoms were found to be a statistically significant risk factor for four other visual functioning tests. As shown in Table 1, 11.6% of participants with ADHD symptoms also failed ocular alignment for the right eye, and only 3.1% of learners with ADHD symptoms, although no significant difference was found for the left eye between learners with ADHD symptoms and those without ADHD symptoms. The OR was 4.1 (95% CI 2.15 - 379; p=0.0029). Visual tracking with both eyes on X shape showed that 9.5% of participants with ADHD symptoms failed the test, compared with 3.5% of those without ADHD symptoms. The odds of failing were only 2.9 times higher (95% CI 1.10 - 7.49; p=0.0284). Similar results for visual tracking with the right eye on X showed that 19.0% failed the skill, compared with 10.1% of learners without ADHD symptoms. The OR was 2.1 (95% CI 1.07 - 3.93; p=0.0301). In addition, visual tracking with the left eye on a circle indicated that 26.3% of learners with ADHD symptoms failed the test, and only 12.5% of learners without symptoms of ADHD. Accordingly, the OR was 2.5 (95% CI 1.38 - 4.41; p=0.0032).
Finally, ADHD symptoms were significantly associated with the results of the QNST-II tracking test (p=0.0028), such that presence of ADHD symptoms was associated with the risk of moderate or severe problems with visual functioning. Of the participants with ADHD symptoms, 23.2% had an abnormal result (moderate or severe problem), whereas only 9.5% of participants without ADHD symptoms had an abnormal result (Table 1).
The strongest association of ADHD symptoms with visual motor skill problems (highest odds ratios) was for fixation right eye and fixation left eye.
Discussion
The study aimed to determine whether the presence of ADHD symptoms was associated with visual functioning difficulties among learners aged 6 - 8 years. However, a causal relationship between ADHD symptoms and visual functioning difficulties cannot strictly be established using data from a cross-sectional study alone, as we did here.
In fact, it could be argued that ADHD symptoms might be a risk factor for impaired visual functioning, as indicated by Gronlund et al.,[18] who made use of detailed ophthalmologic evaluations when conducting a study on 42 children with a mean age of 12 years in Sweden. The researchers came to the conclusion that children on medication for ADHD did significantly better compared with children without medication on the visual acuity test for distance. In contrast, Fabian et al.[19] conducted a study on 56 participants (mean age 9.5 years) diagnosed with ADHD and 66 (mean age 9 years) without ADHD. All participants were tested by a professional optometrist to determine their visual abilities at the Sheba Medical Institution in Israel. The results for both groups were similar for visual acuity, binocular vision as well as accommodation, and therefore not attributed to ADHD.
It is a common characteristic that children diagnosed with ADHD often avoid tasks demanding sustained mental effort,[5] which may influence both fixation and visual tracking. Therefore, according to Cheatum and Hammond,[3] a child with fixation problems can experience difficulties in the classroom when they have to focus on an object such as a block, word or picture or even the teacher. With regard to fixation, the current study indicated that ADHD is significantly associated with difficulties both in the right and left eye.
This observation is in agreement with Munoz et al.,[12] who tested children and adults. The researchers made use of a pro-saccade task and an anti-saccade task. The difference between the two tasks was that for the pro-saccade task, participants were asked to focus on a central fixation point and then they had to move towards a visual target that was located unconventionally. For the anti-saccade task, stimulus appearance was similar; however, the participants now had to look at a central fixation point which was located on the opposite sides of the target, while they had to try and suppress saccade to the stimulus. There were 76 children with ADHD and 75 children in the control group. There was a significant difference between the two groups, especially to supress their saccadic eye movement when they had to fixate on an object for some time.[12] Gould et al.[11] tested 53 children with the combined type of ADHD and 44 children in the control group between the ages of 7 and 13 on a 21-second fixation test. The conclusion from this study indicated that the ADHD children, both the girls and boys, struggled more with the fixation test.[8] In contrast, Karatekin and Asarnow[20] studied 30 ADHD children and 26 children without ADHD in Los Angeles, USA. The children had to do a fixation test using a picture out of a children's book and to answer three questions about the picture. Although the ADHD group had shorter fixation times, these were not significantly different from children without ADHD.
Visual tracking is the ability to follow an object.[3] In this regard, Cheatum and Hammond[3] are of the opinion that the learner with visual tracking problems might struggle to read as the eyes move from one word to another. Furthermore, difficulties can be experienced in the physical education class or on the sportsfield, as the learner might not be able to take part in activities such as throwing and catching because they struggle to track the object.[3] Observing slower smooth-pursuit eye movements, the current study indicated that only three of the 12 visual tracking functions had been implicated in significant associations with ADHD, namely both eyes X shape, right eye X shape and left eye circle shape. Similarly to the current study, Ross et al.[21] tested 17 adults with ADHD and 37 without ADHD. The slow pursuit eye movements were recorded during a constant velocity task at 16.7° per second. The researchers came to the conclusion that although the participants showed slower tracking movements of the eyes, these still fell into a normal range similar to participants without ADHD. In contrast, Jacobsen et al., [22] found that the participants (18 ADHD and 22 without ADHD) in their study could not continuously track an object even at a constant speed, using an infrared photoelectric limbus detection eye-tracking device.
In contrast to the current study, Borsting et al.[23] performed a study on 24 children between the age of 8 and 15 years. The researchers determined the association between convergence insufficiency and ADHD and concluded that the association does exist.[23] A similar but retrospective study was conducted by Granet et al.,[24] who reviewed the charts of 266 participants from the USA. The researchers indicated a threefold greater association between convergence insufficiency and ADHD. However, the current study did not find such an association (p=0.5411). The reason for the contradicting results might be due to the fact that Borsting et al.[23] as well as Granet et al.[24] used samples where the participants were previously diagnosed with visual difficulties in their respective visual faculties. The current study only made used of the Pyfer[17] and the QNST-II,[18] which are both only screening instruments to determine if a child might have visual difficulties. According to Cheatum and Hammond,[3] convergence is an important aspect in the classroom, especially when the learner completes work on his/her desk, such as playing with clay, writing and beadwork.
Implications
The literature clearly indicates that ADHD and visual function difficulties can lead to learning difficulties in an educational setting such as the classroom, in addition to activities on the sports field. The current study indicated that children find it hard to fixate because they cannott supress their saccadic eye movements. This will influence the child's academic performance as they will not be able to fixate on the teacher explaining the work, reading activities or being able to build with blocks. On the sports field, for example with cricket, a batsman will find it hard to fixate on the oncoming bowler and ball. The result will be an inability to hit the ball. Furthermore, the inability to visually track words in a book will lead to poor reading performance. On the sports field, these children will especially struggle with object manipulation skills where they have to track an object, such as catching a ball in rugby and netball, striking activities such as hockey and cricket, or kicking a ball in soccer. Regarding sports skills, visual functioning difficulties can restrict a learner's physical activity, causing further motor and physical developmental delays. Although the current study did not indicate problems with convergence, other literature indicates that these children might also experience problems which will affect their ability to perform tasks at close range, for example on a table, and includes activities such as playing with clay or writing in their books. Therefore, early detection and prevention of visual function difficulties is important to initiate appropriate interventions to prevent failure in the school environment and sports field that can lead to low self-image. Furthermore, visual studies can aid in categorising ADHD.
Study limitations
The current study only recruited children from the Bloemfontein metropolitan area, while no children from rural regions of the province were included. Therefore, the study is not representative of the SA population. Hence, a replication of this study in different provinces and regions in SA is recommended to provide more robust results. Furthermore, ADHD symptoms were identified based on the SWAN completed by a teacher, rather than a clinician. In future studies, the parents of the participants could be asked to complete the SWAN in order to compare its results with the findings of teachers.
Conclusion
The objective of the present study was to determine if the presence of ADHD symptoms was associated with visual functioning difficulties in Grade 1 learners (fixation, ocular alignment, convergence-divergence ocular control, visual tracking, QNST-2 eye tracking). These tests were conducted on learners 6 - 8 years of age. The results of this study show that the presence of ADHD symptoms is significantly associated (p<0.05) with visual functioning difficulties where both eyes are fixating, as well as where individual eyes are fixating, respectively. Furthermore, significant associations of ADHD symptoms have also been noted in problems with the right eye regarding ocular alignment, both eyes in visual tracking for the X shape, and the right eye for visual tracking X shape, left eye visual tracking in a circle, and lastly for QNST-II tracking.
Declaration. VvdV and EJH were independent researchers.
Acknowledgements. We thank the principals, staff members and children at the primary schools where the study was conducted.
Author contributions. MDM planned the research and wrote the article.
RS did the data analysis and helped with discussion of results. VvdV and EJH collected the data.
Funding. None.
Conflicts of interest. None.
References
1. Mutti MC, Sterling HM, Martin NA, Spalding NV. QNST-II. Quick Neurological Screening Test. 2nd ed. Novato: Academic Therapy Publications, 1998. [ Links ]
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington: American Psychiatric Publishing, 2013. [ Links ]
3. Cheatum BA, Hammond AA. Physical Activities for Improving Children's Learning and Behaviour: A Guide to Sensory Motor Development. Champaign: Human Kinetics, 2000. pp 263, 267, 285. [ Links ]
4. Gallahue DL, Ozmun JC. Understanding Motor Development: Infants, Children, Adolescent, Adults. 6th ed. New York: McGraw-Hill, 2006. [ Links ]
5. Roth K, Zittel L, Pyfer J, Auxter D. Principles and Methods of Adapted Physical Education and Recreation. 12th ed. Boston: McGraw Hill, 2017. pp 588, 608609. [ Links ]
6. VanPutte C, Regan J, Russo A. Seeley's Essentials of Anatomy and Physiology. 8th ed. Boston: McGraw-Hill, 2013. [ Links ]
7. Payne VG, Isaacs LD. Human Motor Development: A Lifespan Approach. 7th ed. New York: McGraw Hill, 2008. [ Links ]
8. Barkley RA. Major life activity and health outcomes associated with attention-deficit/hyperactivity disorder. J Clin Psychiatry 2002;63(Suppl 12):10-15. [ Links ]
9. Wender PH. ADHD: Attention-Deficit Hyperactivity Disorder in Children, Adolescents and Adults. Oxford: Oxford University Press, 2002. [ Links ]
10. Castellanos FX, Marvasti FF, Ducharme JI, et al. Executive function oculomotor tasks in girls with ADHD. J Am Acad Child Adolesc Psychiatry 2000;39(5):644-650. https://doi.org/10.1097/00004583-200005000-00019 [ Links ]
11. Gould TD, Bastain TM, Israel ME, Hommer DW, Castellanos FX. Altered performance on an ocular fixation task in attention-deficit/hyperactivity disorder. Biol Psychiatry 2001;50(8):633-635. https://doi.org/10.1016/s0006-3223(01)01095-2 [ Links ]
12. Munoz DP, Armstrong IT, Hampton KA, Moore KD. Altered control of visual fixation and saccadic eye movements in attention-deficit hyperactivity disorder. J Neurophysiol 2003:90(1):503-514. https://doi.org/10.1152/jn.00192.2003 [ Links ]
13. Pauc R. The occurrence, identification and treatment of convergence failure in children with dyslexia, dyspraxia, attention deficit disorder (ADD), attention deficit hyperactive disorder (AD/HD), obsessive compulsive disorder (OCD) and Tourette's syndrome. Clin Chiropractic 2008:11(3):130-137. https://doi.org/10.1016/j.clch.2008.10.006 [ Links ]
14. Deans P, O'Laughlin L, Brubaker B, Gay N, Krug D. Use of eye movement tracking in the differential diagnosis of attention deficit hyperactivity disorder (ADHD) and reading disability. Psychology 2010;1:238-246. https://doi.org/10.4236/psych.2010.14032 [ Links ]
15. Swanson J, Schuck S, Mann M, et al. The SWAN rating scale 2001. http://www.adhd.net (accessed 11 September 2012). [ Links ]
16. Pyfer JL. Sensory Input Systems Screening Test. Texas: Texas Woman's University. 1987. In: Auxter D, Pyfer J, Roth K, Zittel L, editors. Principles and Methods of Adapted Physical Education and Recreation. 10th ed. New York: McGraw Hill, 2005. [ Links ]
17. SAS Institute Inc. SAS/STAT 14.3 User's Guide. Cary: SAS Institute, 2017. [ Links ]
18. Gronlund MA, Aring E, Landgren M, Hellstrom A. Visual function and ocular features in children and adolescents with attention deficit hyperactivity disorder, with and without treatment with stimulants. Eye 2007;21:494-502. https://doi.org/10.1038/sj.eye.6702240 [ Links ]
19. Fabian ID, Kinori M, Ancri O, Spierer A, Tsinman A, Ben Simon GJ. The possible association of attention deficit hyperactivity disorder with undiagnosed refractive errors. J Am Assoc Pediatr Ophthalmol Strabismus 2013;17(5):507-511. https://doi.org/10.1016/j.jaapos.2013.06.005 [ Links ]
20. Karatekin C, Asarnow RF. Exploratory eye movements to pictures in childhood-onset schizophrenia and attention-deficit/hyperactivity disorder (ADHD). J Abnorm Child Psychol 1999:27:35-49. https://doi.org/10.1023/a:1022662323823 [ Links ]
21. Ross RG, Olincy A, Harris JG, Sullivan B, Radant A. Smooth pursuit eye movements in schizophrenia and attentional dysfunction: Adults with schizophrenia, ADHD, and a normal comparison group. Biol Psychiatry 2000:48(3):197-203. https://doi.org/10.1016/s0006-3223(00)00825-8 [ Links ]
22. Jacobsen LK, Hong WL, Hommer DW, Hamburger S, Castellanos FX, Frazier JA. Smooth pursuit eye movements in childhood onset schizophrenia: Comparison of attention deficit disorder and normals. Biol Psychiatry 1996;40(11):1144-1154. https://doi.org/10.1016/s0006-3223(95)00630-3 [ Links ]
23. Borsting E, Rouse M, Chu R. Measuring ADHD behaviors in children with symptomatic accommodative dysfunction or convergence insufficiency: A preliminary study. Optometry 2005;76(10):588-592. https://doi.org/10.1016/j.optm.2005.07.007 [ Links ]
24. Granet DB, Gomi CF, Ventura R, Miller-Scholte AM. The relationship between convergence insufficiency and ADHD. Strabismus 2005;13(4):163-186. https://doi.org/10.1080/09273970500455436 [ Links ]
 Correspondence:
Correspondence:
M de Milander
demilanderm@ufs.ac.za
Accepted 13 November 2020














