Servicios Personalizados
Articulo
Indicadores
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en Google
Similares en Google
Compartir
South African Journal of Child Health
versión On-line ISSN 1999-7671
versión impresa ISSN 1994-3032
S. Afr. j. child health vol.14 no.3 Pretoria sep. 2020
http://dx.doi.org/10.7196/sajch.2020.v14i3.1712
RESEARCH
'It's like making your own alcohol at home': Factors influencing adolescent use of over-the-counter cough syrup
Z EssackI, II; C J GroenewaldI; A van HeerdenI, III
IPhD; Centre for Community-Based Research, Human Sciences Research Council, Pietermaritzburg, South Africa
IIPhD; School of Law, University of KwaZulu-Natal, Pietermaritzburg, South Africa
IIIPhD; MRC/WITS Developmental Pathways for Health Research Unit, Department of Paediatrics, Faculty of Health Science, University of the Witwatersrand, Johannesburg, South Africa
ABSTRACT
BACKGROUND. Adolescents are increasingly experimenting with new 'craze drugs, including over-the-counter cough medicine (OTCCM). However, there is limited empirical evidence regarding South African (SA) adolescents' use of codeine-containing medicines, especially OTCCMs.
OBJECTIVE. To describe SA adolescents' views of OTCCM misuse, and the factors that may promote its use.
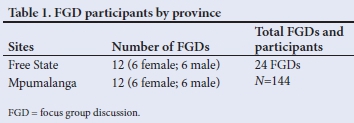
METHODS. The research adopted an exploratory qualitative design. Focus group discussions (N=24) were conducted with 144 learners between 14 and 17 years old in two township communities in SA. Data were analysed thematically supported by Atlas.ti.
RESULTS. Three core themes emerged from the analysis, namely knowledge of OTCCM use; factors that influence OTCCM use; and effects of OTCCM use. Participants reported that young people use OTCCM recreationally. Four main factors were noted to influence OTCCM misuse in their communities, namely accessibility, affordability, social influences and the clandestine appeal of cough medicine. Adolescents also said that OTCCM had similar euphoric effects to alcohol or marijuana, but could not readily describe any negative impact.
CONCLUSION. This exploratory study with adolescent participants provides contextualised empirical evidence about OTCCM. The findings call for the South African Health Products Regulatory Authority (SAHPRA) to promptly consider pending regulations on OTC codeine-containing medication and demands increased awareness of codeine misuse in communities.
Over the past decade, adolescent interest in recreational substances has expanded beyond the use of alcohol and/or cannabis. Rather, adolescents are increasingly using substances that offer alternative modes of usage, such as whoonga (a low-grade form of heroin that is smoked in conjunction with cannabis)[1] and, more recently, over-the-counter cough medicine (OTCCM) that contains codeine[2] or high levels of alcohol (hereafter referred to as 'cough syrup').
In South Africa (SA), the use of cough syrup as a recreational drug is a relatively new but rapidly growing phenomenon. Through the broader research study on which the current paper is based, we found that one-quarter (n=52) of our sample (N=205) reported having used cough syrup recreationally. Among this sub-group of recreational users, most (n=31) indicated that they first used this substance at 15 -17 years of age.
Cough syrups are generally consumed as a cocktail mixed with fizzy sodas or fruit juices, and this concoction is globally referred to as 'lean, 'sizzurp, 'purple drank, 'dirty sprite'[3] or 'double cupping,'[4] among others. 'Lean' has been popularised in rap and hip-hop music since the 1990s,[3] and is increasingly referenced in SA hip-hop. Anecdotal evidence, presented in print, television and social media, suggests that young people prefer cough syrups that contain alcohol or codeine, given the euphoric effects associated with their usage.[4,5]
Excessive use of products containing codeine may lead to withdrawal symptoms, including cravings and a preoccupation with using codeine products,[6] and 'lean' use has also been associated with serious brain damage,[7] illicit drug abuse, and heightened risk of polydrug addiction.[8] Similarly, the abuse of alcohol is associated with adverse health and behavioural consequences, and may lead to adulthood dependence.[9,10] Research has documented cough syrup abuse in China and Hong Kong,[11-13] India[14,15] and the USA.[3,16-18] However, research on cough syrup misuse in SA is limited, although some research has explored adult use of codeine-based OTC tablets.[6] There is therefore a paucity of SA research pertaining to adolescents' misuse of cough syrups. The current paper addresses this gap by describing SA adolescents' views of cough syrup misuse, and the factors that may promote misuse.
Methods
The present paper is based on results from a larger mixed-methods study that explored underage drinking in two low-resourced townships in Mpumalanga and Free State provinces, SA. The paper presents qualitative findings on adolescents' knowledge and perceptions of recreational cough syrup use.
Participants in Grades 10 - 12 were recruited at four schools in two townships. Participants were eligible if they were <18 years old, volunteered to participate and provided consent (parental consent and adolescent assent).
All eligible participants' names were compiled and 72 learners per township were randomly selected (N=144) to participate in focus group discussions (FGDs). The study received ethics approval from the Human Sciences Research Council Research Ethics Committee (ref. no. REC2/22/11/17c). Twenty-four FGDs were completed with purposively selected learners between 15 and 17 years old (Table 1). All FGDs were audio-recorded with consent, transcribed verbatim and, where relevant, translated. Data were analysed thematically[19] using an inductive-deductive approach and managed in Atlas.ti (ATLAS.ti Scientific Software Development GmbH, USA).
Results
Recreational cough syrup use was discussed in 14 of the 24 FGDs. These discussions generally focused on the following three themes: (i) knowledge of recreational cough syrup use; (ii) factors that influence recreational cough syrup use; and (iii) perceived effects of recreational cough syrup use.
Knowledge of recreational cough syrup usage: 'they call it codeine'
Participants revealed that recreational cough syrup use is commonly practised by young people in their communities, especially boys. Five different types of cough syrup which contained either alcohol or codeine were identified by the adolescents. These were Stillpain, DPH, Benelyn, Alcopholyx and Allergex - with Stillpain and DPH most frequently referenced.
Most participants referred to these cough syrups as 'codeine, with no participants making reference to commonly used street names (e.g., lean or sizzurp); for example:
Participants (collectively): 'They call it codeine. Yes.' [...] Interviewer: 'Oh... they call it codeine (.) So, can you please tell me more about it? What do they mix there specifically?' Participant 4: 'They buy a medicine called Stillpain at pharmacies and they mix it with Sprite. That medicine is strong, so they get drunk after that!' (female participant, Grade, 12, T2).
Participants generally explained that 'codeine' was a cocktail of cough syrup mixed with fizzy drinks, mostly Sprite, '... that can drug you' (female participant, T1). They were able to provide detail on how it is mixed and its 'purple' colour:
'You go to the chemist to buy a medication for flu and you will then go buy... sparkling water. Then you can drink half of the fizzy drink before pouring all the medication so that it can drug you.' (female participant, Grade 10, S2).
A few participants reported that this cocktail may also be laced with other OTC tablets such as Panado or Disprin where adolescents '. put Panado and mix it with Sprite and Benelyn' (female participant, Grade 10, T1).
Factors influencing adolescents 'codeine misuse'
Participants described four main factors that influence codeine misuse among young people in their community. These were accessibility, affordability, social influences, and the clandestine appeal of cough medicine.
Accessibility: 'You just go to the pharmacy and buy'
Although none of the participants in our study mentioned accessing 'codeine' through illegal vendors in their communities, it was evident that 'codeine' was easily accessible in their communities through local pharmacies and clinics: '[t]hey are there [in the community] and others say they are sold at the shops' (female participants, Grade 12, S1). Participants reported that cough syrups were readily available because adolescents were able to legitimately procure it from pharmacies and clinics where '[you] don't need a prescription or birth certificate or nothing' (female participant, Grade 10, T1). This easy access may further contribute to their increasing popularity and misuse by young people. It was mentioned, however, that pharmacies were exercising increasing supervision over OTC cough medicine (OTCCM) procurement; for example:
'But these days they are refusing because they have noticed that people are using it wrongly.' (male participants, Grade 11, T1).
Additionally, household medicine cabinets were identified as spaces where 'codeine' could be accessed: '. the cough mixture is usually readily available in most households.' (female participant, T2) and 'they are there at home' (female participant, Grade 11, T2).
Affordability
The cost of the types of OTCCM mentioned by the participants normally ranged between R20 and R80, with one cough syrup bottle used to make up as much as 2 L of 'lean':
Interviewer: 'Do you buy that codeine?'
Participant: 'Yes.'
Interviewer: 'How much is it?'
Participant: 'R25, if I remember.'
Interviewer: 'So, that small bottle of R25, how much codeine can you make?'
Participant: 'Two litre.' (male, Grade 11, T1).
For those participants who are able to access 'codeine' through their primary healthcare clinic, this cost may be negligible. Therefore, in addition to its accessibility, 'codeine' was a preferred substance as it is an affordable recreational drug:
'They would mix and mix... they go and buy [it] because Coke is very cheap and the cough mixture is usually readily available in most households, so they would then mix [it together].' (female participant, T2).
Relative to other substances such as alcohol, adolescents can legally access cough syrups at a nominal cost, which may encourage its use; for example 'when they don't have money to buy alcohol, they do like that [use 'codeine']. (female participant Grade 11, T1).
Social influences: 'So, anything that is trending on Instagram is the one that we'd like'
'Codeine' was described as not only socially consumed with friends but also its use was socially constructed via social media popularity. Apart from having observed peers using 'codeine, several participants indicated that they were introduced to 'codeine' through music, television and social media platforms such as Instagram, Facebook and YouTube:'They show us by making a video on Instagram and it is done online. The person will make a video shoot of it, holding it and showing how it is done. So when we are watching those people, we want to fit in. So, anything that is trending on Instagram is the one that we'd like. So, it seems like some 'swag' [trend] that is good!' (male participant, Grade 11, T2).
Adolescents also made specific reference to the influence of Hip Hop artists, mentioning Migos and 21 Savage. They referenced specifically the lyrics of the song 'I feel it' by 21 Savage:
'Everywhere we go we clean.
She want me to quit that lean.
Baby, I can't quit that lean.
Put a ring around codeine.'
The profound impact of social media on adolescents' behaviour is evident in the above extract. Many adolescents have access to social media platforms with the intention of monitoring and enacting trends to promote their own popularity. As indicated in the adolescent's narrative, young people feel pressured to behave accordingly in order to be popular or 'fit in', even when trends are negative. The increasing popularity of codeine is especially apparent in another participant's description that 'Oh! And now it's the fashion.' (male participant, Grade 11, T1). Given this growing trend, many people on social media were said to post pictures of their 'codeine' use, so perpetuating the perception that codeine use is 'on trend'.
Clandestine use: 'They will think it is juice'
Participants reported that 'codeine' use often occurs in concealed ways but in public spaces such as homes, house parties or at parks. This concealment was often ensured by masking the drug with darker-coloured sodas. Alarmingly, in one of the study sites (T2), participants cited schools as a common place where 'codeine' is consumed:
'...right here at school'...there was this child who used to come carrying a squeeze bottle.' (female participant, Grade 10, T2). 'They come with it mixed already in a bottle and the teachers won't be able to notice what is in there. They will think it is just juice.' (female participant, Grade 12, T2).
The ability to use OTCCM and other medications in a clandestine way thus perpetuates its open use and may further promote its increasing popularity.
Effects of codeine use: 'You get drunk'
When asked about the potential effects of 'codeine' use, the participants generally focused on its euphoric effects rather than harmful consequences:
Participant: 'Oh, side-effects? We don't even know; we just drink it! We know it gets one drunk! Codeine is the most dangerous alcohol.'
Interviewer: 'Why?'
Participant: 'Because Eish! The things that they mix inside there!'
Interviewer: 'So do you drink it?'
Participant: 'Yes! It tastes nice and it tastes like strawberry!'
It was noted that while there might be negative side-effects, participants had not personally experienced these: 'Yes, there is this guy that drank it, he overdose it. So, he was actually sick. So, obviously the side-effects are there. So, in our case we have never overdosed and that's why we don't know the side-effects.' (male participant, Grade 11, T1).
'Codeine' was considered to contribute to stress relief, promoting meditation and used as an escape from reality. The social benefits acquired from fitting in and being perceived as having 'swag' may have positive appeal for adolescents.
Furthermore, participants considered 'cough syrups' to have similar intoxicating effects as alcohol. This was apparent in their use of the word 'drunk' and also evident in the following extracts where codeine was likened to alcohol spirits:
'... the same as when you have drank alcohol; you get drunk the same way. It's like making your own alcohol at home!' (female participant, Grade 11, T1).
Others noted that 'it is just like dagga [cannabis] with its effects.' (female participant, Grade 12, T2) in that it makes one 'just laugh, 'feel sleepy, 'act funny', 'high' or 'become crazy'.
Discussion
This paper aimed to describe adolescents' perceptions and knowledge of cough syrup misuse in two low-resourced townships in SA. In the larger study, approximately one-quarter of survey participants reported having used cough syrups recreationally, and the popularity of this 'craze drug' seems to be increasing. The qualitative findings showed that adolescents generally used cough syrups that contain codeine or alcohol, which they colloquially referred to as 'codeine'. Recreational 'codeine' use was facilitated by the potential to easily obtain it from numerous sources including pharmacies, clinics and medicine cabinets at home, as shown in research from the USA[20] and an internet study.[21] 'Codeine' was also considered a cheaper alternative to alcohol that provides similar euphoric effects and can be used in a clandestine way. The drug's popularity and 'glamorising' on social media[22] and in peer groups, along with the low cost, appears to further enhance its acceptability and 'trendiness.
A critical factor reported to promote codeine use was its ease of accessibility. The Children's Act[23] enables adolescent access to medical treatments and prescribed drugs independently, if certain capacity requirements are satisfied.[24] Adolescents from 12 years old can access medical treatment without parental consent, granted that they have 'sufficient maturity and the mental capacity to understand the benefits, risks, social and other implications of the treatment.'[24] Ensuring an enabling legal and policy environment is critical for adolescents to access youth-friendly services. The increasing misuse of codeine-based medications, however, underscores the value of age and capacity considerations as well as regulation of OTC sales more broadly.
In line with the Codeine Care initiative, some pharmacies request proof of identity before the sale of codeine-based medication, while others record identifying information in a register. However, the impact of this monitoring system is currently unknown.[25] Given the reports of increasing codeine misuse, particularly among adolescents,[4,5] supported by data from the present study, it remains imperative that careful consideration be given to the regulatory framework for OTC medication in SA, improved surveillance, and monitoring of sales.[6] A narrative review of codeine misuse and mitigation strategies has made similar recommendations.[26]
Given the relatively recent onset of cough syrup misuse by adolescents in SA communities, further research is required to document the kind of cough syrups that the youth misuse in different contexts, the kinds of 'cocktails' or combinations that are created, and factors associated with recreational codeine use among adolescents. In this way, the epidemiology of adolescent cough syrup usage in SA can be understood and targeted responses to interrupt patterns of consumption be developed. It is evident that there is a lack of knowledge and awareness of the adverse health effects and addictive properties of cough syrup misuse among our sample - contrary to findings among Chinese adolescents, which emphasised the negative effects relative to the benefits.[13] Research has associated long-term misuse of the drug codeine, specifically, with various harmful outcomes including gastric ulcers, inflammatory bowel conditions, gastrointestinal bleeding, potential addiction[6,27] and mental health problems.[28] Similarly, the health and behavioural consequences of adolescent alcohol misuse (including alcohol-based cough syrups) include increased likelihood of mental health and neurocognitive challenges,[28] learning disabilities,[29] risky sexual behaviour[30] and increased risk of alcohol dependence during adulthood.[31] Because discussions on the potential harm of cough syrup misuse were limited in our dataset, it is important to raise awareness about the harmful health outcomes associated with cough syrup misuse and dependence with adolescents, their parents, teachers and wider communities.
Our research was exploratory in nature and limited to two townships in two SA provinces. Therefore, the results presented here may not reflect those of all adolescents in SA. Nevertheless, the study provides important insights on codeine use and misuse, and is one of the first to focus on adolescent use in SA.
Conclusion
This exploratory study of adolescent participants provides contextualised empirical evidence about OTCCM, how it is used, and the factors that promote its use. Findings of this research underline the importance of pending regulations by the South African Health Products Regulatory Authority (SAHPRA), the consideration of capacity requirements for adolescents' access to such medications and how best to operationalise these, and the value of awareness and care initiatives that ensure robust monitoring and surveillance of OTC purchases to flag misuse early.
Declaration. Opinions expressed and conclusions are those of the authors and are not to be attributed to the DST-NRF Centre of Excellence (CoE) in Human Development at the University of the Witwatersrand.
Acknowledgements. The authors acknowledge their data collection and processing team, including Sinankekelwe Khumalo, Akhona Nkwanyana, Mafanato Gladys Maluleka, Thabo Gerald Keetsi, Xolani Ntinga and Khanya Vilakazi. We also thank all stakeholders for allowing access to participants, and the latter who participated in focus group discussions. CG acknowledges the support of the DST-NRF CoE.
Author contributions. ZE and CR conceptualised the paper and analysed the data. All authors contributed to the final draft of the manuscript.
Funding. The findings are based on results from a larger study on underage drinking. Funding for the larger study was provided by Aware.org.
Conflicts of interest. None.
References
1. Groenewald C, Essack Z. "I started that day and continued for 2 years": A case report on adolescent 'whoonga' addiction. J Substance Use 2019;24(6):578-580. http://hdl.handle.net/20.500.11910/14261 [ Links ]
2. Kulak JA, Griswold KS. Adolescent substance use and misuse: Recognition and management. Am Fam Phys 2019;99(11):689-696. [ Links ]
3. Hart M, Agnich LE, Stogner J, Miller BL. 'Me and My Drank:' Exploring the relationship between musical preferences and purple drank experimentation. Am J Crim Just 2014;39(1):172-186. https://doi.org/10.1007/s12103-013-9213-7 [ Links ]
4. Ngubane S. KZN's home-made drug fear. IOL News .https://www.iol.co.za/news/kzns-home-made-drug-fear-2005344 (accessed 5 April 2016). [ Links ]
5. ShoziP. SA's new addiction. News 24.https://www.news24.com/SouthAfrica/Local/Hillcrest-Fever/sas-new-addiction-20181120 (accessed 27 November 2018). [ Links ]
6. Van Hout MC, Rich E, Dada S, Bergin M. "Codeine Is My Helper." Misuse of and dependence on codeine-containing medicines in South Africa. Qual Health Res 2017;27(3):341-350. https://doi.org/10.1177/1049732315613764 [ Links ]
7. Hou H, Yin S, Jia S, et al. Decreased striatal dopamine transporters in codeine-containing cough syrup abusers. Drug Alc Depend 2011;118(2-3):148-151. https://doi.org/10.1016/j.drugalcdep.2011.03.011 [ Links ]
8. Jones CM. Heroin use and heroin use risk behaviors among nonmedical users of prescription opioid pain relievers-United States, 2002-2004 and 2008-2010. Drug Alc Depend 2013;132(1-2):95-100. [ Links ]
9. Olawole-Isaac A, Ogundipe O, Amoo EO, Adeloye D. Substance use among adolescents in sub-Saharan Africa: A systematic review and meta-analysis. S Afr J Child Health 2018;12(2b):79-83. https://doi.org/10.7196%2FSAJCH.2018.v12i2b.1524 [ Links ]
10. Marshall EJ. Adolescent alcohol use: Risks and consequences. Alc Alcohol 2014;49(2):160-164. https://doi.org/10.1093/alcalc/agt180 [ Links ]
11. Lam LC, Lee DT, Shum PP, Chen CN. Cough mixture misuse in Hong Kong-an emerging psychiatric problem? Addiction 1996;91(9):1375-1378. [ Links ]
12. Wu Q, Yu J, Yang C, et al. Nonmedical use of cough syrup among secondary vocational school students: A national survey in China. Medicine 2016;95(10):e2969. https://doi.org/10.1097/md.0000000000002969 [ Links ]
13. Shek DT, Lam CM. Beliefs about cough medicine abuse among Chinese young people in Hong Kong. Social Behavior and Personality: An International Journal 2008;36(1):135-144. https://doi.org/10.2224/sbp.2008.36.L135 [ Links ]
14. Mattoo SK, Basu D, Sharma A, Balaji M, Malhotra A. Abuse of codeine-containing cough syrups: A report from India. Addiction 1997 Dec;92(12):1783-1787. [ Links ]
15. Wairagkar NS, Das J, Kumar S,et al. Codeine containing cough syrup addiction in Assam and Nagaland. Indian J Psychiatry 1994;36(3):129-132. [ Links ]
16. Agnich LE, Stogner JM, Miller BL, Marcum CD. Purple drank prevalence and characteristics of misusers of codeine cough syrup mixtures. Addict Behav 2013;38(9):2445-2449. https://doi.org/10.1016/j.addbeh.2013.03.020 [ Links ]
17. Palamar JJ, Le A, Cleland CM. Nonmedical opioid use among electronic dance music party attendees in New York City. Drug Alc Depend 2018;186:226-232. https://doi.org/10.1016%2Fj.drugalcdep.2018.03.001 [ Links ]
18. Palamar JJ. Use of 'lean' among electronic dance music party attendees. Am J Addict 2019;28(5):347-352. https://doi.org/10.1111/ajad.12897 [ Links ]
19. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3(2):77-101. https://doi.org/10.1191/1478088706qp063oa [ Links ]
20. Elwood WN. Sticky business: Patterns of procurement and misuse of prescription cough syrup in Houston. J Psychoactive Drugs 2001;33(2):121-133. https://doi.org/10.1080/02791072.2001.10400477 [ Links ]
21. Van Hout MC. Nod and wave: An Internet study of the codeine intoxication phenomenon. Inter J Drug Policy 2015;26(1):67-77. https://doi.org/10.1016/j.drugpo.2014.06.016 [ Links ]
22. Cherian R, Westbrook M, Ramo D, Sarkar U. Representations of codeine misuse on instagram: Content analysis. JMIR Pub Health Surveill 2018;4(1):e22. https://doi.org/10.2196/publichealth.8144 [ Links ]
23. South Africa. Children's Act No. 38 of 2005. Pretoria: Government Printer; June 2006. [ Links ]
24. Strode A, Essack Z. Facilitating access to adolescent sexual and reproductive health services through legislative reform: Lessons from the South African experience. S Afr Med J 2017;107(9):741-744. https://doi.org/10.7196/samj.2017.v107i9.12525 [ Links ]
25. Parry CD, Rich E, Van Hout MC, Deluca P. Codeine misuse and dependence in South Africa: Perspectives of addiction treatment providers. S Afr Med J 2017;107(5):451-456. https://doi.org/10.7196/samj.2017.v107i5.12242 [ Links ]
26. Olasunkanmi AR, Isreal AO. A narrative review of codeine and preventive measures in mitigating against the widespread of its abuse and misuse. J Alcohol Drug Depend 2019;7(323):2. http://doi.org/10.4172/2329-6488.1000323 [ Links ]
27. Foley M, Carney T, Rich E, Dada S, Mburu C, Parry C. A study of medical professionals' perspectives on medicines containing codeine in South Africa. S Afr J Psychiatry 2018;24(1): a1162. https://doi.org/10.4102/sajpsychiatry.v24.i0.1162. [ Links ]
28. Inchley JC, Currie DB, Vieno A, et al. Adolescent alcohol-related behaviours: Trends and inequalities in the WHO European Region, 2002-2014. Geneva: WHO; 2018. [ Links ]
29. Clark DB, Thatcher DL, Tapert SF. Alcohol, psychological dysregulation, and adolescent brain development. Alcohol Clin Exp Res 2008;32(3):375. https://doi.org/10.1111/j.1530-0277.2007.00601.x [ Links ]
30. Groenewald C, Essack Z, Khumalo S. Speaking through pictures: Canvassing wadolescent risk behaviours in a semi-rural community in KwaZulu-Natal Province, South Africa. S Afr J Child Health 2018;12(2b):s57-s62. https://doi.org/10.7196%2FSAJCH.2018.v12i2b.1514 [ Links ]
31. McCambridge J, McAlaney J, Rowe R. Adult consequences of late adolescent alcohol consumption: A systematic review of cohort studies. PLoSMed 2011;8(2):e1000413. https://doi.org/10.1371/journal.pmed.1000413 [ Links ]
 Correspondence:
Correspondence:
Z Essack
zessack@hsrc.ac.za
Accepted 9 March 2020














